Abstract
Knee injuries such as ACL tears commonly occur and there is a high re-injury rate after primary ACL reconstruction with figures estimated at 25%-33%. Clinicians often use hip strengthening as a key component of knee rehabilitation. Evidence suggests that adopting a “regional” or “proximal” approach to rehabilitation can increase hip strength, but motor control often remains unchanged, particularly during more complex tasks such as running and jumping. It has been previously suggested that the current approach to “regional/proximal” rehabilitation is too basic and is constrained by a reductionist philosophy. This clinical commentary provides the clinician a framework for optimizing knee rehabilitation, underpinned by a more global approach. Although this approach remains hip-focused, it can be easily adapted to modify exercise complexity and key loading variables (speed, direction, flight), which will help the clinician to better replicate the sport specific demands on the knee.
Level of Evidence
5
Keywords: ACL, dynamic knee valgus, hip exercise, movement system, proximal rehabilitation
THE PROBLEM
The annual incidence of anterior cruciate ligament injuries is approximately 120,000 in the United States, and slowly increasing, especially amongst female athletes.1 Primary ACL reconstruction is the predominant surgical treatment of choice,2 but only two thirds of individuals return to their preinjury level of sports participation.3 Furthermore, re-injury rates following primary ACL reconstruction are estimated at 25%-33%;4 with the return-to-play rate reducing to 50% after revision surgery. Despite an exponential increase in research over the past 20 years, ACL injury rates remain unchanged, placing a significant burden on public health with annual costs averaging $1billion.1 This begs the question – Are current ACL prevention and rehabilitation programs sufficient for the athletic patient?
Authors have previously suggested that the current approach to “regional / proximal” knee rehabilitation is constrained by a reductionist philosophy, which overlooks the “global complexity” of movement patterns throughout the entire kinetic chain.5 In effect, most contemporary knee rehabilitation and prevention programs incorporate regional or “proximal” exercises that target the hip region.6 While these exercises increase local hip strength,6 hip focused exercise programs do not meaningfully change regional lower limb kinematics, particularly during higher speed dynamic tasks such as running7 and landing.8 Recently researchers have reported that greater medial knee displacement during landing is a primary risk factor for ACL injury.9 Consequently, the best therapeutic exercise approach for controlling aberrant kinematics, such as uncontrolled dynamic knee valgus, remains unclear.
The clinical suggestion offered in this commentary is a framework for improving knee rehabilitation and reducing ACL injury incidence and reinjury rates. It uses a global approach to highlight key principles and exercise variables, currently missing from popular ACL prevention and rehabilitation programs. The framework is underpinned by the following principles: 1) hip arthrokinematics must be addressed; 2) use of the trunk as a lever for resistance; 3) the incorporation of a flight phase to replicate ground reaction forces. Although the primary focus is on the knee, it is anticipated that this framework is relevant to end stage rehabilitation and return to sport exercise prescription for other lower extremity injuries.
THE SOLUTION
Hip Arthrokinematics
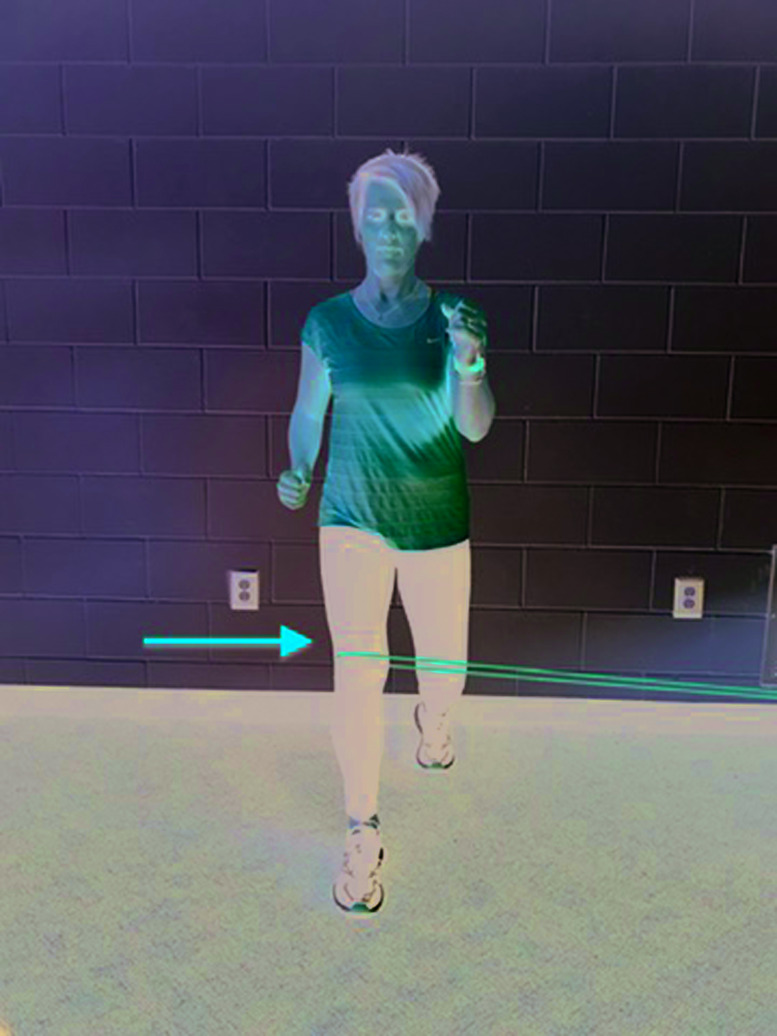
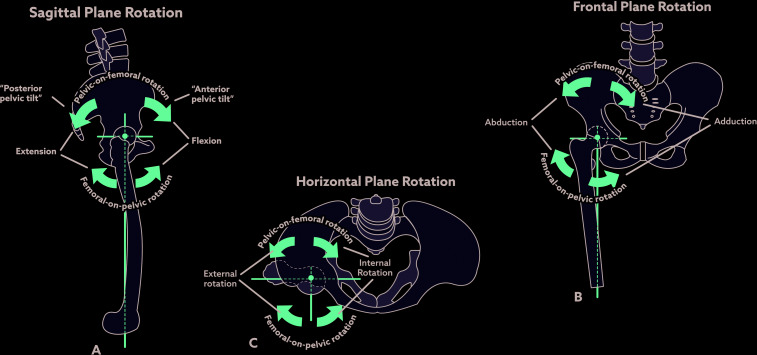
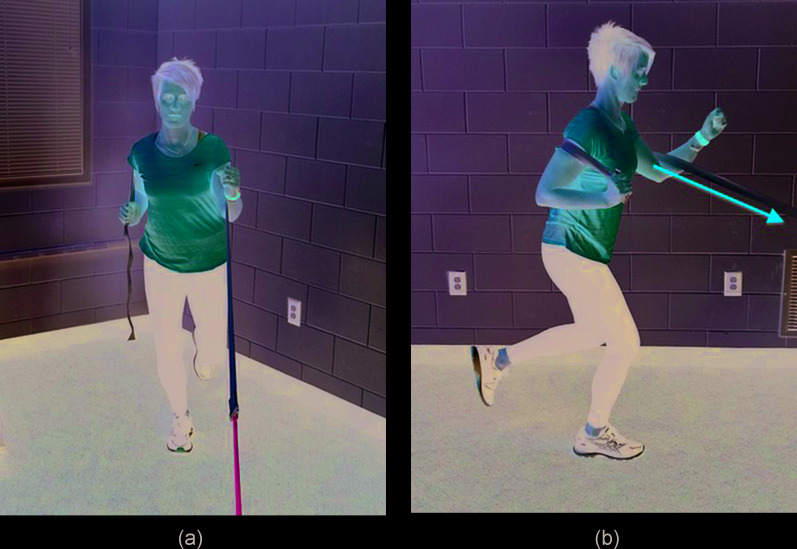
The exercise shown in Figure 1 is commonly prescribed to address dynamic knee valgus.7,10,11 This exercise is an example of a basic ‘ball under socket’ exercise, where the femur is the moving lever, and resistive forces are delivered at the knee, along the frontal plane. However, when athletes undertake multi-directional loading in a weight-bearing position, hip arthrokinematics are ‘socket over ball’, as it is the pelvic acetabulum moving over the femur. ‘Socket over ball’ movements have a distinct arthrokinematic pattern,12,13 whereby the pelvis moves in a triplanar motion (anterior tilt, contralateral pelvic drop and a forward rotation) over a fixed femur (Figure 2).14 This coordinated interplay between the pelvis and femur, is similar to the scapulohumeral rhythm noted in the shoulder.15 Therefore, the ‘socket over ball’ exercises shown in Figures 3a and 3b represent an important progression from Figure 1, as they recreate the distinct hip arthrokinematics that occur during single leg loading, and maximally challenge pelvifemoral coordination. There is evidence that altering the position of the pelvis during exercise, influences trunk muscle activation16,17 and that trunk muscle activation increases EMG activity of the hip musculature.18 This demonstrates the intimate relationship between the trunk, pelvis and hip musculature, but future EMG studies of the specific exercises presented in this paper are warranted.
Figure 1.
Dynamic knee valgus control exercise utilizing a bottom-up approach. The band tethered around the knee restricts the athlete's ability to leave the ground and delivers the resistance in one specific plane only.
Figure 2.
Schematic representation of acetabulo-femoral movements in red (“socket over ball”) whereas the pelvis is moving on a fixed femur and femoral-acetabular movements in yellow (“ball under socket”) illustrating how the femur is moving under a fixed or stable pelvis.
Figure 3.
Single leg squat progression utilizing the trunk as the lever for triaxial resistance. The resistance is on a downward angle moving across three planes of motion specifically targeting the hip.
The ‘Proximal’ Trunk
Many existing ACL prevention and rehabilitation programs broadly define ‘proximal’ control as any movement above the knee.19 This interpretation of ‘proximal’ is too vague and often overlooks the meaningful relationship between the hip and the trunk. Knee rehabilitation programs must progress to incorporate proprioceptive challenges and perturbations involving the trunk,20 while specifically integrating the hip. Recent evidence supports the hypothesis that impaired trunk control contributes to injuries of the spine, and to segments of the kinetic chain, such as the knee.20 Primarily, increasing trunk stability enhances stiffness throughout the kinetic linkage and therefore plays a key role in controlling dynamic knee valgus. Prospective research shows that female collegiate athletes with poor neuromuscular control of the trunk (based on active proprioceptive repositioning) are at greater risk of knee injury.21
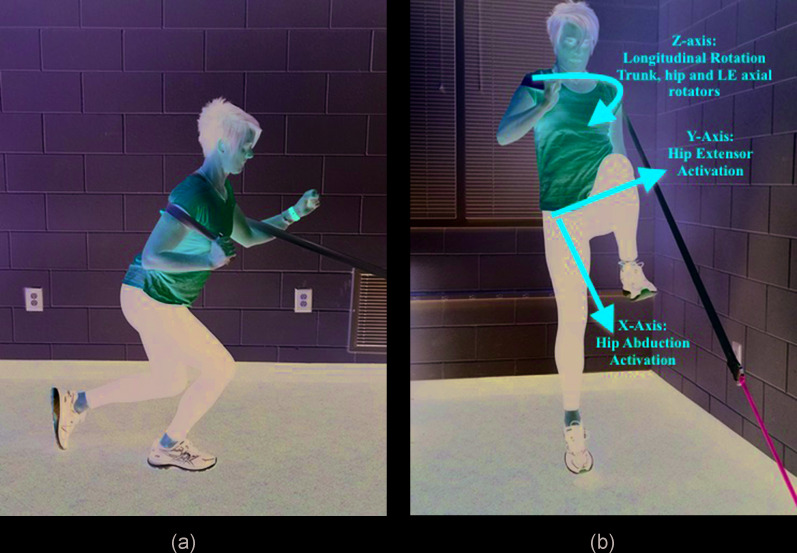
In effect, the trunk is a key proximal lever, and its triplanar position directly affects lower extremity function and potentially the acetabular pelvic position on the femur. For example, counter rotation of the trunk on the pelvis (the trunk rotating about the vertical z-axis, as seen in Figures 4a and 4b), increases tension in the entire musculoskeletal system (analogous to wringing out a wet towel) ultimately limiting end range motion at the hip joint.22,23 Similar concepts have been extrapolated to common active movements such as the throwing mechanics with pitchers,24 and recent fascial research,22,25 further supports the concept that “kinetic chains” are not just conceptual pathways, but are physical entities dictating viscoelastic tension in the body.14,23,26,27
Figure 4.
ingle leg jumps with triaxial resistance at the proximal trunk. The resistance is moved proximally allowing the trunk to become the lever for the exercise. The resistance induces a spin about the longitudinal z-axis which makes the athlete accommodate for these spiraling forces as she lands.
These findings suggest ‘proximal’ control should combine the movements of the trunk and hip to create a blended program offering both hip strengthening and proximal trunk control simultaneously,5 this would be supported by evidence that reported ACL prevention programs that included both strength and proximal control exercises demonstrated the greatest prophylactic effects.28 Interestingly, it has also been reported that utilizing a multimodal approach and a varied combination of exercises may protect the knee during athletic movements.28
Many of these concepts are applied in Figures 3a and 3b, where external resistance is applied around the proximal trunk creating a longer lever and allowing forces to be applied over multiple joints. As noncontact ACL injury typically involves multiplanar mechanisms,29 it is important that the direction of external resistance is such that it creates a spiral force (about the vertical longitudinal axis /Z-axis), which further challenges the athlete to control medial lower extremity collapse in this position. The nature and direction of the external forces also helps to maximize the contribution from the posterior chain, particularly engaging the gluteus maximus. The fiber orientation of the gluteus maximus coupled with its expansive tendinous attachments across the pelvic crest and sacrum, proximally to the humerus (via the thoracolumbar fascia) and distally to the tibia (via the iliotibial tract),30 mean that this posterior muscular chain is optimally placed to eccentrically control internal rotation and adduction of the femur, anterior pelvic rotation and contralateral pelvic drop (relative hip adduction of the stance limb) at ground contact, highlighting the mechanical contributions of the gluteus medius and maximus and their role in the prevention of ACL injuries.31
Flight, Speed and Endurance
A recent meta-analysis reported that the impact phase of a ballistic task has been correlated to hip weakness and increased dynamic knee valgus32 and medial knee displacement,9 both of which have been reported as risk factors for ACL injury.33,34 Thus, it is imperative that lower extremity prevention and rehabilitation programs include task specific exercises including the repetitive attenuation of ground reaction forces while landing from a flight phase. Knee rehabilitation or prevention exercises that anchor the resistance at the lower extremity (e.g. Figure 1), will limit the athlete's ability to leave the ground and enter a flight phase. In contrast, Figures 4a and 4b anchor the external resistance at the shoulders facilitating a more global collaborative response between the femur, pelvis, and trunk. Utilizing the trunk as a lever also allows the clinician to apply varying angles of resistance throughout the movement. For example, once the subject has left the ground, the band can be used to apply a rotatory force, directed around the longitudinal Z-axis (Fig. 4b). Upon landing, the hip musculature is challenged to activate immediately in order to control triaxial rotary collapse.35,36 There is further evidence that athletes recovering from ACL injury commonly suffer prolonged deficits in their rate of force development, despite demonstrating near normal strength.37 Training the flight phase in this triplanar manner repetitively can address the endurance component of the program. As neuromuscular fatigue is also responsible for biomechanical alterations that may increase the risk of a noncontact ACL injury during landing,38 clinicians need to be sensitive of both peripheral and central mechanisms of fatigue and integrate endurance based sport specific landing tasks.39,40
The diagram in Figure 5 conceptualizes and presents a summary of key subcomponents of therapeutic knee exercise inclusive of the components described above. The relevance (size) of each subcomponent (circle) depends on the specific needs of an athlete and the demands of their sport. The framework is predicated on the philosophy that the subcomponents in Fig. 5 can eventually be integrated into a singular training method. By allowing all these variables to interact simultaneously (i.e. the center of the Venn), in an attempt to recreate the athletic demands involved with single limb loading, providing the greatest potential to optimize higher speed athletic movements. The authors acknowledge that other more distal factors, such as foot biomechanics, can contribute to lower limb injury.41,42 While this commentary is not meant to minimize the distal contributions to the kinetic chain, there is evidence to support the role of the trunk and hip in dynamic knee valgus, which provides a rationale for the mechanism being considered a “proximal to distal process.”31,43 It should also be acknowledged the importance of using local (knee) and regional (hip) based exercise in the early stages of rehabilitation, with recovery progressing through the integration of and increasing number of exercise components.44,45 It is important to note, transitions from local to regional to global exercise have precautions secondary to the increase in rotational forces at the knee. Clinical judgement is necessary and introducing rotary forces during a post-operative ACL rehabilitation must follow appropriate healing parameters. Typically these type of rotary based exercises should be initiated after the athlete has already returned to sport specific running, cutting and jumping activities.
Figure 5.
Venn Diagram: Multifactorial representation of the modifiable components of a hip focused therapeutic exercise program.
CONCLUSION
The ultimate goal for clinicians is to design exercises that are replicating, as closely as possible, the complex demands of higher-level functional activities prior to the end of rehabilitation and return to sport. Many of the current ‘proximal’ exercise programs have questionable transference to sport as they are confined to non-weight-bearing exercise, ball under socket weight-bearing exercises, performed in a single plane, often at a single speed. This framework will help to incorporate exercises which replicate sporting challenges and recreates ‘socket over ball’ kinematics. The framework encourages a global approach, whereby ‘proximal’ is not be confined to the hip; but rather incorporates proprioceptive challenges and perturbations involving the trunk. It highlights the importance of implementing a triplanar flight phase that challenges trunk counter rotation, to recreate the relevant sequencing of coupled joint movements and neuromotor patterns unique to ballistic single leg athletic movements. The proposed approach to rehabilitation and prevention programs may have the potential to address continued high rates of ACL injury through the implementation of advanced exercise prescription, although future studies will be needed to assess this approach to injury prevention.
References
- 1.Kaeding CC Leger-St-Jean B Magnussen RA. Epidemiology and diagnosis of anterior cruciate ligament injuries. Clin Sports Med. 2017;36(1):1-8. [DOI] [PubMed] [Google Scholar]
- 2.Gans I Retzky JS Jones LC Tanaka MJ. Epidemiology of recurrent anterior cruciate Ligament Injuries in National Collegiate Athletic Association Sports: The Injury surveillance program, 2004-2014. Orthop J Sports Med. 2018;6(6):2325967118777823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ardern CL Taylor NF Feller JA Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48(21):1543-1552. [DOI] [PubMed] [Google Scholar]
- 4.Schilaty ND Nagelli C Bates NA, et al. Incidence of second anterior cruciate ligament tears and identification of associated risk factors from 2001 to 2010 using a geographic database. Orthop J Sports Med. 2017;5(8):2325967117724196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dischiavi SL Wright AA Hegedus EJ Ford KR Bleakley C. Does ‘proximal control’ need a new definition or a paradigm shift in exercise prescription? A clinical commentary. Br J Sports Med. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ford KR Nguyen AD Dischiavi SL Hegedus EJ Zuk EF Taylor JB. An evidence-based review of hip-focused neuromuscular exercise interventions to address dynamic lower extremity valgus. Open Access J Sports Med. 2015;6:291-303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Willy RW Davis IS. The effect of a hip-strengthening program on mechanics during running and during a single-leg squat. J Orthop Sports Phys Ther. 2011;41(9):625-632. [DOI] [PubMed] [Google Scholar]
- 8.Palmer K Hebron C Williams JM. A randomised trial into the effect of an isolated hip abductor strengthening programme and a functional motor control programme on knee kinematics and hip muscle strength. BMC Musculoskelet Disord. 2015;16:105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Krosshaug T Steffen K Kristianslund E, et al. The vertical drop jump is a poor screening test for ACL injuries in female elite soccer and handball players: a prospective cohort study of 710 athletes. Am J Sports Med. 2016;44(4):874-883. [DOI] [PubMed] [Google Scholar]
- 10.Esculier JF Bouyer LJ Dubois B et al. Is combining gait retraining or an exercise programme with education better than education alone in treating runners with patellofemoral pain?A randomised clinical trial. Br J Sports Med. 2018;52(10):659-666. [DOI] [PubMed] [Google Scholar]
- 11.Passigli S Capacci P Volpi E. The effects of a multimodal rehabilitation program on pain, kinesiophobia and function in a runner with patellofemoral pain. Int J Sports Phys Ther. 2017;12(4):670-682. [PMC free article] [PubMed] [Google Scholar]
- 12.Neumann DA. Kinesiology of the hip: a focus on muscular actions. J Orthop Sports Phys Ther. 2010;40(2):82-94. [DOI] [PubMed] [Google Scholar]
- 13.Murray R Bohannon R Tiberio D Dewberry M Zannotti C. Pelvifemoral rhythm during unilateral hip flexion in standing. Clin Biomech. 2002;17(2):147-151. [DOI] [PubMed] [Google Scholar]
- 14.Dischiavi SL Wright AA Hegedus EJ Bleakley CM. Rethinking dynamic knee valgus and its relation to knee injury: normal movement requiring control, not avoidance. J Orthop Sports Phys Ther. 2019;49(4):216-218. [DOI] [PubMed] [Google Scholar]
- 15.Levangie PK Norkin CC Levangie PK. Joint structure and function : a comprehensive analysis. 5th ed. Philadelphia: F.A. Davis Co.; 2011. [Google Scholar]
- 16.Filho Rde F de Brito Silva P Ito MA Alves N Padovan CR, Micolis de Azevedo F. Stabilization of lumbo-pelvic region and electromyography of the abdominal muscles. Electromyogr Clin Neurophysiol. 2006;46(1):51-57. [PubMed] [Google Scholar]
- 17.Schoenfeld BJ Contreras B Tiryaki-Sonmez G Willardson JM Fontana F. An electromyographic comparison of a modified version of the plank with a long lever and posterior tilt versus the traditional plank exercise. Sports Biomech. 2014;13(3):296-306. [DOI] [PubMed] [Google Scholar]
- 18.Chan MK Chow KW Lai AY Mak NK Sze JC Tsang SM. The effects of therapeutic hip exercise with abdominal core activation on recruitment of the hip muscles. BMC Musculoskelet Disord. 2017;18(1):313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sugimoto D Myer GD Foss KD Hewett TE. Specific exercise effects of preventive neuromuscular training intervention on anterior cruciate ligament injury risk reduction in young females: meta-analysis and subgroup analysis. Br J Sports Med. 2015;49(5):282-289. [DOI] [PubMed] [Google Scholar]
- 20.Zazulak B Cholewicki J Reeves NP. Neuromuscular control of trunk stability: clinical implications for sports injury prevention. J Am Acad Orthop Surg. 2008;16(9):497-505. [PubMed] [Google Scholar]
- 21.Zazulak BT Hewett TE Reeves NP Goldberg B Cholewicki J. The effects of core proprioception on knee injury: a prospective biomechanical-epidemiological study. Am J Sports Med. 2007;35(3):368-373. [DOI] [PubMed] [Google Scholar]
- 22.Tak IJR. Hip and groin pain in athletes: morphology, function and injury from a clinical perspective. Br J Sports Med. 2018. [DOI] [PubMed] [Google Scholar]
- 23.Zugel M Maganaris CN Wilke J, et al. Fascial tissue research in sports medicine: from molecules to tissue adaptation, injury and diagnostics. Br J Sports Med. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chu SK Jayabalan P Kibler WB Press J. The kinetic chain revisited: new concepts on throwing mechanics and injury. PM R. 2016;8(3 Suppl):S69-77. [DOI] [PubMed] [Google Scholar]
- 25.Carvalhais VO Ocarino Jde M Araujo VL Souza TR Silva PL Fonseca ST. Myofascial force transmission between the latissimus dorsi and gluteus maximus muscles: an in vivo experiment. J Biomech. 2013;46(5):1003-1007. [DOI] [PubMed] [Google Scholar]
- 26.Wilke J Krause F Vogt L Banzer W. What is evidence-based about myofascial chains: a systematic review. Arch Phys Med Rehabil. 2016;97(3):454-461. [DOI] [PubMed] [Google Scholar]
- 27.Dischiavi SL Wright AA Hegedus EJ Bleakley CM. Biotensegrity and myofascial chains: A global approach to an integrated kinetic chain. Med Hypotheses. 2018;110:90-96. [DOI] [PubMed] [Google Scholar]
- 28.Sugimoto D Mattacola CG Bush HM, et al. Preventive neuromuscular training for young female athletes: comparison of coach and athlete compliance rates. J Athl Train. 2017;52(1):58-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Anderson MJ Browning WM, 3rd Urband CE Kluczynski MA Bisson LJ. A systematic summary of systematic reviews on the topic of the anterior cruciate ligament. Orthop J Sports Med. 2016;4(3):2325967116634074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stecco A Gilliar W Hill R Fullerton B Stecco C. The anatomical and functional relation between gluteus maximus and fascia lata. J Bodyw Mov Ther. 2013;17(4):512-517. [DOI] [PubMed] [Google Scholar]
- 31.Cannon J Cambridge EDJ McGill SM. Anterior cruciate ligament injury mechanisms and the kinetic chain linkage: the effect of proximal joint stiffness on distal knee control during bilateral landings. J Orthop Sports Phys Ther. 2019:1-45. [DOI] [PubMed] [Google Scholar]
- 32.Dix J Marsh S Dingenen B Malliaras P. The relationship between hip muscle strength and dynamic knee valgus in asymptomatic females: A systematic review. Phys Ther Sport. 2019;37:197-209. [DOI] [PubMed] [Google Scholar]
- 33.Hewett TE Myer GD Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492-501. [DOI] [PubMed] [Google Scholar]
- 34.Padua DA Bell DR Clark MA. Neuromuscular characteristics of individuals displaying excessive medial knee displacement. J Athl Train. 2012;47(5):525-536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Allison GT Morris SL Lay B. Feedforward responses of transversus abdominis are directionally specific and act asymmetrically: implications for core stability theories. J Orthop Sports Phys Ther. 2008;38(5):228-237. [DOI] [PubMed] [Google Scholar]
- 36.Aruin AS Latash ML. Directional specificity of postural muscles in feed-forward postural reactions during fast voluntary arm movements. Exp Brain Res. 1995;103(2):323-332. [DOI] [PubMed] [Google Scholar]
- 37.Angelozzi M Madama M Corsica C, et al. Rate of force development as an adjunctive outcome measure for return-to-sport decisions after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2012;42(9):772-780. [DOI] [PubMed] [Google Scholar]
- 38.Santamaria LJ Webster KE. The effect of fatigue on lower-limb biomechanics during single-limb landings: a systematic review. J Orthop Sports Phys Ther. 2010;40(8):464-473. [DOI] [PubMed] [Google Scholar]
- 39.Frank BS Gilsdorf CM Goerger BM Prentice WE Padua DA. Neuromuscular fatigue alters postural control and sagittal plane hip biomechanics in active females with anterior cruciate ligament reconstruction. Sports Health. 2014;6(4):301-308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Webster KE Santamaria LJ McClelland JA Feller JA. Effect of fatigue on landing biomechanics after anterior cruciate ligament reconstruction surgery. Med Sci Sports Exerc. 2012;44(5):910-916. [DOI] [PubMed] [Google Scholar]
- 41.Smith HC Vacek P Johnson RJ, et al. Risk factors for anterior cruciate ligament injury: a review of the literature - part 1: neuromuscular and anatomic risk. Sports Health. 2012;4(1):69-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Loudon JK Jenkins W Loudon KL. The relationship between static posture and ACL injury in female athletes. J Orthop Sports Phys Ther. 1996;24(2):91-97. [DOI] [PubMed] [Google Scholar]
- 43.Hewett TE Myer GD. The mechanistic connection between the trunk, hip, knee, and anterior cruciate ligament injury. Exerc Sport Sci Rev. 2011;39(4):161-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Blanchard S Glasgow P. A theoretical model to describe progressions and regressions for exercise rehabilitation. Phys Ther Sport. 2014;15(3):131-135. [DOI] [PubMed] [Google Scholar]
- 45.Blanchard S Glasgow P. A theoretical model for exercise progressions as part of a complex rehabilitation programme design. Br J Sports Med. 2019;53(3):139-140. [DOI] [PubMed] [Google Scholar]