Abstract
Introduction
Smoking cessation treatments currently succeed at a rate of approximately 20%–30%, underscoring the importance of exploring factors that might increase intervention effectiveness. Although negative affect has been studied extensively in relation to smoking cessation, psychological well-being (PWB; eg, life satisfaction, optimism, positive affect, purpose in life) has received little attention. This study tested longitudinal and reciprocal relationships between PWB and smoking status in older adults.
Methods
Panel data were obtained from the biennial, longitudinal Health and Retirement Study. Using structural equation modeling, we developed cross-lagged models to examine the relationships of PWB in 2006 with smoking status in 2010 and of smoking status in 2006 with PWB in 2010 while controlling for covariates (Ns = 2939–4230, 55% women, 89% white, mean age = 64 years, mean years of education = 13, 25% smokers in 2006 and 21% smokers in 2010). Separate cross-lagged models were developed for each of the PWB variables: life satisfaction, optimism, positive affect, and purpose in life.
Results
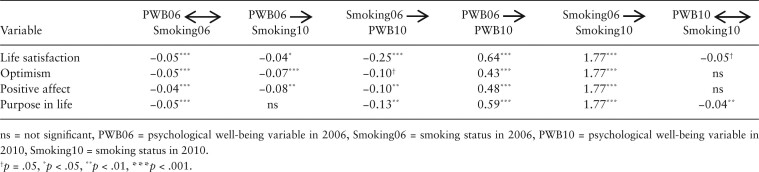
Greater life satisfaction (standardized path coefficient = −0.04), optimism (standardized path coefficient = −0.07), and positive affect (standardized path coefficient = −0.08) in 2006 predicted a reduced likelihood of smoking in 2010. Being a smoker in 2006 predicted lower life satisfaction (standardized path coefficient = −0.25), optimism (standardized path coefficient = −0.10), positive affect (standardized path coefficient = −0.10), and purpose in life (standardized path coefficient = −0.13) in 2010.
Conclusions
Findings warrant further exploration of the relationships between PWB and smoking, and support the incorporation of PWB-boosting components into existing treatments.
Implications
Given the relatively low success rate of current smoking cessation treatments, the present results suggest that increasing PWB might promote abstinence and therefore warrant consideration as a focus of future cessation treatment research. Moreover, these results suggest that smoking might inhibit PWB, illuminating a negative consequence of smoking not previously identified. Helping smokers increase their PWB may benefit them beyond promoting cessation and contribute to a flourishing society. These results warrant further investigation of PWB and smoking, and support the continued evaluation of PWB-boosting components in smoking cessation treatments.
Introduction
The role of negative affect in the development and maintenance of addiction has been well established. Indeed, negative affect withdrawal symptoms are considered pathognomonic of addiction in several time-honored theories of drug use1–3 and conceptualized as the leading motivational catalysts of compulsive drug use in present-day models.4 With regard to cigarette use, negative affect manifestations predict the onset and progression of dependence,5 negative affect manipulations in the laboratory reliably elicit cravings to smoke,6 and negative affect symptomatology is a consistent predictor of smoking cessation treatment failure.7,8 Though contemporary smoking cessation treatments incorporate elements that target negative affect, the most intensive of these treatments typically yield long-term abstinence rates of approximately 20%–30%9 despite nearly universal desire to quit smoking among cigarette users (eg, Fong et al.10). Given these low success rates, the pursuit of smoking cessation strategies that extend beyond the scope of negative affect is imperative. This expanded scope could elucidate additional mechanisms that promote long-term abstinence.
The previous focus on relieving negative affect is justified in that negative information and affect exert more influence on cognitive evaluations than positive information and affect.11 However, psychological well-being (PWB; eg, life satisfaction, optimism, positive affect, purpose in life) does have a measurable impact on life outcomes12,13 including health,14 but has been largely ignored in the etiology of tobacco and other substance dependence. This is relevant because whereas negative affect narrows response options—“fight” and “flight” are motivated by anger and fear, respectively15—PWB promotes creative problem-solving and strengthens social support networks,16,17 attributes that would be expected to increase the likelihood of tobacco and other substance abstinence. PWB is associated with a number of improved medical and psychiatric outcomes, including management of osteoarthritis symptoms,18 reduced likelihood of stroke and better cardiac health,19,20 a greater decrease in cancer antigen among patients with ovarian cancer,21 lower levels of plasma triglycerides and better lung function,22 a decreased odds of postpartum depression,23 reduced craving among those seeking treatment for alcohol dependence,24 and others.25 With regard to smoking, a large cross-sectional survey of older Lithuanians found that being a former or never-smoker was associated with a greater quality of life as compared to being a current smoker,26 and a small survey conducted in Brazil found that nonsmokers reported greater levels of mindfulness and subjective well-being than smokers.27 Furthermore, a cross-sectional study of black and Puerto Rican young adults found that greater restrictions on smoking in the home were associated with less smoking, which was in turn associated with greater subjective well-being and psychological adjustment.28 Finally, a recent pilot randomized controlled trial of positive psychotherapy for smoking cessation found that positive psychotherapy was associated with a higher odds of abstinence as compared to standard smoking cessation treatment,29 adducing that greater PWB may foster abstinence. The prospective relationships of PWB to cigarette use have otherwise not been explored, and thus the potential causal role that PWB might play in the cessation process is not entirely clear.
PWB may also be particularly worthwhile to target in smoking cessation because, as suggested by Tiffany et al.,30 substance use treatments should address more than abstinence alone and focus on additional outcomes such as quality of life. PWB is integral to quality of life as health is more than the absence of ill-being.31 Indeed, PWB itself is an important public health concern (eg, Kobau et al.32). To the best of our knowledge, the prospective relationships of cigarette use to PWB have not previously been evaluated. Whether smoking cessation might potentially play a causal role in augmenting PWB is therefore not known.
The aim of this study was to evaluate the relationships between PWB and smoking. Using a large, representative sample of older US adults who responded to a survey in 2006 and 2010, we evaluated the longitudinal and reciprocal relationships between PWB and cigarette use via cross-lagged analysis. Although the current research was not conceived with the intention to test the associations between PWB and cigarette use among older adults in particular, there is nonetheless a dearth of information regarding older smokers.33 This is significant because the number of older individuals in the United States is projected to more than double between 2010 and 2050, smoking is a leading risk factor in the major causes of death in older people, older smokers may be especially dependent on nicotine yet motivated to quit, and age-related cognitive and physiological changes may present unique challenges to quitting smoking.33–35
Given that greater PWB is associated with improved health outcomes and those with greater PWB may be more likely to protect their health because they find their lives worth living,31 we hypothesized that greater PWB in 2006 would be associated with a decreased likelihood of smoking in 2010. In addition, we hypothesized that smoking in 2006 would predict lower PWB in 2010 because a persistent, recurring focus on the short-term hedonistic pleasure of smoking may preclude smokers from engaging in meaningful behaviors that result in long-term PWB.36,37
Method
Sample
The biennial Health and Retirement Study (HRS) has longitudinally surveyed a representative sample of Americans aged 50 years and older since 1992 to describe the health, psychological, financial, work, insurance, and retirement planning conditions of these adults. The HRS began collecting PWB data in full in 2006 from half of the sample and collected PWB data from alternating halves at each subsequent assessment period. Thus, our analyses used the 2006 and 2010 data38,39 because these assessment periods included the same individuals and represent the first available longitudinal PWB data from the HRS. Interviewers collected data via face-to-face interviews and leave-behind questionnaires, with an 87.7% response rate in 2006 and 73.1% response rate in 2010. The University of Michigan Institute for Social Research provides extensive documentation about the survey methodology, psychosocial measures, and sampling strategy40 (see http://hrsonline.isr.umich.edu/index.php?p=dbook).
Measures
We followed the instructions included in the HRS documentation on coding and index creation for each analyzed variable. To report smoking status, respondents answered yes or no to the question, “Do you smoke cigarettes now?” This question was adapted from the National Health Interview Survey, which has been conducted by the National Center for Health Statistics of the Centers for Disease Control and Prevention since 1960 (see https://www.cdc.gov/nchs/nhis/about_nhis.htm).
Life satisfaction was measured using the Satisfaction with Life Scale.41,42 An example item is, “In most ways my life is close to ideal.” Responses across five items were averaged with higher scores indicating greater satisfaction with life. Scores ranged from one to six in 2006 and one to seven in 2010. In multiple studies, the Satisfaction with Life Scale has a Cronbach’s alpha ranging from .79 to .89 and test-retest reliability ranging from .83 after two weeks and .54 after four years.
Optimism was measured using three items from the Life Orientation Test—Revised43 with items such as, “In uncertain times, I usually expect the best.” Scores ranged from one to six and were the result of averaging responses across items, with higher scores representing greater optimism. The LOT-R has a Cronbach’s alpha of .78 and a test-retest reliability of .68 after four months and .79 after 28 months.
Positive affect was measured in 2006 using the positive affect measure from the National Survey of Midlife Development in the United States (MIDUS II).44 Participants responded to questions such as, “During the last 30 days, how often did you feel in good spirits?” Responses from the six items were averaged with scores ranging from one to five. Higher scores indicated that respondents experienced positive emotions with greater frequency. Cronbach’s alpha for this measure is .88 and test–retest reliability is .68 over 8 weeks.
In 2010, positive affect was assessed with the Positive and Negative Affect Schedule.45 The 10 items of the positive mood scale were averaged with scores ranging from one to five. Higher values represent higher levels of positive affect. Cronbach’s alpha for this measure is .92 and test–retest reliability is .70 after 2 months.
Purpose in life was measured using a scale of the Ryff Measures of Psychological Well-being.46–48 One example item is, “I enjoy making plans for the future and working to make them a reality.” Responses were averaged across seven items and ranged from one to six. Higher scores represent greater purpose in life. Cronbach’s alpha for this scale is 0.90 with a test–retest reliability of .82 after 6 weeks.
Statistical Analysis
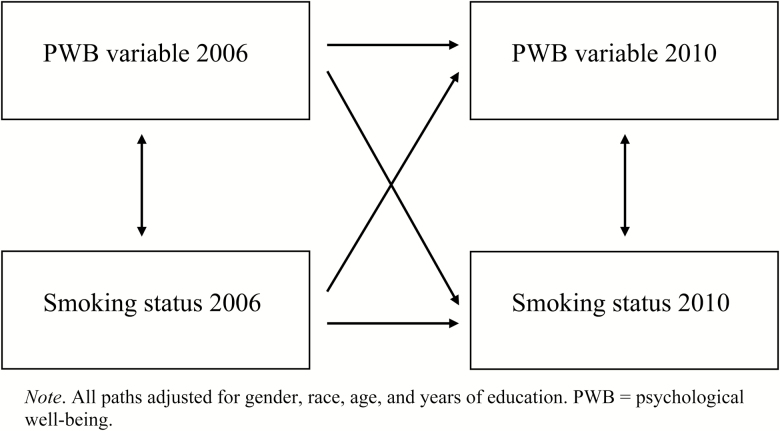
We conducted a cross-lagged analysis of panel data from the HRS assessment periods in 2006 and 2010. Our primary analyses were structural equation models developed using Mplus49 Version 7 software. To examine the reciprocal relations between the PWB variables and smoking status, cross-lagged models were estimated for each of the PWB variables. The reciprocal relationships between PWB and smoking status at 2006 and 2010 were modeled as lag-1 relationships (Figure 1). Path coefficients are reported as standardized estimates that express the proportion of a standard deviation change in one variable due to a one standard deviation change in a second variable.
Figure 1.
Cross-lagged models. All paths adjusted for gender, race, age, and years of education. PWB = psychological well-being.
The sociodemographic covariates of gender, race, age, and years of education were included in each model. All the covariates were included in the model statement and allowed to covary with each other and to serve as potential predictors of PWB and smoking. Thus, each path of each model was adjusted for each covariate. We attempted to maximize the number of respondents available for our analyses (ie, those with complete data on all variables included in the models), thus the number of respondents available for each model varied slightly depending on missing data for each PWB variable. For life satisfaction, 4145 respondents provided complete data in 2006 whereas 2990 respondents provided completed data in 2010. For optimism, 4200 respondents provided complete data in 2006 whereas 2968 respondents provided complete data in 2010. For positive affect, 4230 respondents provided complete data in 2006 whereas 2975 respondents provided complete data in 2010. For purpose in life, 4174 respondents provided complete data in 2006 whereas 2939 respondents provided complete data in 2010. Therefore, for each of the four models, approximately 70% of those who provided complete data in 2006 also provided complete data in 2010. All models were estimated using the weighted least squares parameter estimator implemented in Mplus. The weighted least squares parameter estimator uses a “diagonal weight matrix accompanied by standard errors and mean- and variance- adjusted chi-square test statistics that use a full weight matrix.”49(p533) All models were weighted using calibrated HRS sampling weights to account for the complex survey design and nonresponse in 2010.50,51
Results
Participants were 55% women and 89% white with a mean age of 64 years and a mean of 13 years of education in 2006. In 2006 and 2010, 25% and 21% of the sample reported smoking, respectively. Descriptive statistics for the PWB variables in 2006 and 2010 are presented in Table 1. Figure 1 depicts the cross-lagged models and Table 2 presents the standardized path coefficients for each model.
Table 1.
Psychological Well-Being Variables by Smoking Status per Year
| Life satisfaction | Optimism | Positive affect | Purpose in life | |
|---|---|---|---|---|
| 2006 | ||||
| Smoker, M (SEM) | 4.01 (0.06) | 4.31 (0.06) | 3.34 (0.04) | 4.37 (0.05) |
| Nonsmoker, M (SEM) | 4.40 (0.03) | 4.58 (0.03) | 3.59 (0.02) | 4.61 (0.02) |
| 2010 | ||||
| Smoker, M (SEM) | 4.35 (0.09) | 4.21 (0.07) | 3.32 (0.05) | 4.33 (0.05) |
| Nonsmoker, M (SEM) | 4.93 (0.04) | 4.47 (0.03) | 3.58 (0.02) | 4.63 (0.02) |
Table 2.
Standardized Path Coefficients
The analysis tested the hypothesis that greater PWB in 2006 would be associated with not smoking in 2010 and that smoking in 2006 would be associated with lower PWB in 2010. The models supported this hypothesis for all but one path. Specifically, though there was no association between purpose in life in 2006 and smoking status in 2010, greater life satisfaction, optimism, and positive affect measured in 2006 were each predictive of a reduced likelihood of smoking in 2010. In all models, smoking in 2006 was associated with less PWB in 2010. Specifically, smoking in 2006 was related to lower life satisfaction, optimism, positive affect, and purpose in life in 2010.
Discussion
The purpose of this study was to probe longitudinal and reciprocal associations between PWB and smoking status using a large, representative sample of older US adults. We hypothesized that greater life satisfaction, optimism, positive affect, and purpose in life in 2006 would correspond to not smoking in 2010 and that smoking in 2006 would correspond to less life satisfaction, optimism, positive affect, and purpose in life in 2010. With only one exception these hypotheses were supported by our findings.
Analyses revealed that greater life satisfaction, optimism, and positive affect measured in 2006 predicted a reduced likelihood of smoking in 2010 above and beyond smoking status in 2006. In addition, results showed that smoking in 2006 predicted less life satisfaction, optimism, positive affect, and purpose in life in 2010 above and beyond these PWB constructs measured in 2006. These findings suggest that greater PWB may promote abstinence, and consistent with results from a pilot test of a positive psychology intervention for smoking cessation,29 components designed to boost PWB may increase success rates of current smoking cessation treatments. In addition, the findings suggest that smoking may inhibit PWB. Although effects were modest in size, it is noted that even the most effective smoking cessation interventions produce modest rates of abstinence,9 and even modest effects can have meaningful impacts, especially at the population level. For instance, if all of the approximately 38 million adult smokers in the United States52 were provided a new treatment that increased abstinence rates by only 2%, as many as 760 000 lives could be saved.
We suggest several putative mechanisms for how greater PWB might reduce smoking. First, smokers with greater life satisfaction may feel their lives are worth living and therefore they may be more motivated to protect their health.31 Second, smokers with greater positive affect may find more effective cessation strategies through more creative problem-solving and may have stronger social support networks that encourage their cessation efforts.15 Further, positive affect boosts resilience,53 suggesting that smokers with more positive affect may be more resilient to setbacks (eg, cravings, lapses, negative affect) when attempting to quit smoking. Third, optimism may promote successful cessation by fostering persistence in a quit attempt. Consistent with this notion, greater optimism fosters greater persistence generally,13 and specifically predicted greater productivity and employment longevity in insurance sales agents.54
Regarding the finding that smoking is associated with PWB, we speculate that the short-term reward of smoking may be so salient as to preclude smokers from engaging in other behaviors (eg, socializing, career enhancement) that would promote PWB. Furthermore, given that smokers experience chronic withdrawal symptoms such as craving, irritability, anxiety, and difficulty concentrating,4 these chronic symptoms may reduce life satisfaction, inhibit efforts toward problem-solving and building support networks, and limit persistence.
One implication that follows from these results is that cessation therapies designed to boost PWB should continue to be developed and tested either as supplements to existing smoking cessation treatments, or as standalone treatments themselves. Such interventions could include those that target optimism and positive affect by prescribing, for 20 min/d for 2 weeks, writing about one’s best possible future self that has achieved all desired goals,55 as well as those that foster gratitude.56 Another implication of the current findings is that smoking might exact an even greater toll on society than previously considered. In addition to the numerous known smoking-related health consequences, smoking may also reduce PWB. If this is the case, smokers as well as society at large lose out on PWB-related benefits, including enhanced creative problem-solving, larger and more collaborative social networks, and persistence in goal pursuit.12 Incorporating PWB into smoking cessation, therefore, might have a multiplicative effect in that it may reduce the burden smoking places on society and promote a thriving society independent of effects on smoking per se.
Strengths of the study include using a large sample representative of older US adults and a longitudinal 4-year follow-up. Addiction is a chronic, relapsing disorder, yet many current studies of smoking cessation focus on cessation outcomes of 1 year or less.9 Although outcomes of such duration are meaningful and practical for research purposes, it is also worthwhile to consider longer-term outcomes such as the 4-year timeframe offered by the HRS. One limitation is that the panel data analyzed in this study may only reflect a one-time “snapshot” of PWB and smoking status, and may not reflect fluctuations in both PWB and smoking status (ie, multiple quit attempts) during the intervening 4 years. Though the present findings are consistent with the view that increasing PWB might promote smoking abstinence, more persuasive findings would demonstrate an association between PWB and smoking status during an actual quit attempt. PWB variables, however, are considered relatively stable though modifiable. These analyses were further limited by the self-report nature of PWB constructs, and smoking status was not confirmed using biochemical assays. However, these data were collected in a naturalistic setting from many respondents and therefore merit inclusion in the larger body of smoking cessation data. Finally, as the sample was composed of older adults, these results may not generalize to younger smokers. However, older smokers are a special population that warrants unique consideration, and as such the current findings suggest potential avenues for treatment.
In conclusion, given the low success rate of current smoking cessation treatments, the present results suggest that increasing PWB may promote abstinence and therefore warrant consideration as a focus of future interventions. Moreover, these results suggest that smoking might inhibit PWB, illuminating a negative consequence of smoking not previously identified. Helping smokers increase their PWB may help them quit smoking, and is a worthwhile goal in itself because it may benefit smokers beyond promoting cessation and contributes to a flourishing society. Future research should expand on the current findings through continued experimental manipulation of PWB in cessation therapies.
Funding
The Health and Retirement Study (HRS) was sponsored by the National Institute on Aging (NIA U01AG009740) and was conducted by the University of Michigan.
Declaration of Interests
The authors have no conflicts of interest to declare.
References
- 1. Siegel S. Classical conditioning, drug tolerance, and drug dependence. In: Smart RG, Glaser FB, Israel Y, Kalant H, Popham RE, Schmidt W, eds. Research Advances in Alcohol and Drug Problems. Boston, MA: Springer; 1983:207–246. [Google Scholar]
- 2. Solomon RL. The opponent-process theory of acquired motivation: The costs of pleasure and the benefits of pain. Am Psychol. 1980;35(8):691–712. [DOI] [PubMed] [Google Scholar]
- 3. Wikler A. Dynamics of drug dependence. Implications of a conditioning theory for research and treatment. Arch Gen Psychiatry. 1973;28(5):611–616. [DOI] [PubMed] [Google Scholar]
- 4. Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychol Rev. 2004;111(1):33–51. [DOI] [PubMed] [Google Scholar]
- 5. Goodwin RD, Pagura J, Spiwak R, Lemeshow AR, Sareen J. Predictors of persistent nicotine dependence among adults in the United States. Drug Alcohol Depend. 2011;118(2-3):127–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Heckman BW, Kovacs MA, Marquinez NS, et al. . Influence of affective manipulations on cigarette craving: A meta-analysis. Addiction. 2013;108(12):2068–2078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Leventhal AM, Piper ME, Japuntich SJ, Baker TB, Cook JW. Anhedonia, depressed mood, and smoking cessation outcome. J Consult Clin Psychol. 2014;82(1):122–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Piper ME, Cook JW, Schlam TR, Jorenby DE, Baker TB. Anxiety diagnoses in smokers seeking cessation treatment: Relations with tobacco dependence, withdrawal, outcome and response to treatment. Addiction. 2011;106(2):418–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Schlam TR, Baker TB. Interventions for tobacco smoking. Annu Rev Clin Psychol. 2013;9(1):675–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fong GT, Hammond D, Laux FL, et al. . The near-universal experience of regret among smokers in four countries: Findings from the International Tobacco Control Policy Evaluation Survey. Nicotine Tob Res. 2004;6(suppl 3):S341–S351. [DOI] [PubMed] [Google Scholar]
- 11. Ito TA, Larsen JT, Smith NK, Cacioppo JT. Negative information weighs more heavily on the brain: The negativity bias in evaluative categorizations. J Pers Soc Psychol. 1998;75(4):887–900. [DOI] [PubMed] [Google Scholar]
- 12. Lyubomirsky S, King L, Diener E. The benefits of frequent positive affect: Does happiness lead to success?Psychol Bull. 2005;131(6):803–855. [DOI] [PubMed] [Google Scholar]
- 13. Carver CS, Scheier MF. Dispositional optimism. Trends Cogn Sci. 2014;18(6):293–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pressman SD, Cohen S. Does positive affect influence health?Psychol Bull. 2005;131(6):925–971. [DOI] [PubMed] [Google Scholar]
- 15. Fredrickson BL. The role of positive emotions in positive psychology. The broaden-and-build theory of positive emotions. Am Psychol. 2001;56(3):218–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fredrickson BL, Joiner T. Positive emotions trigger upward spirals toward emotional well-being. Psychol Sci. 2002;13(2):172–175. [DOI] [PubMed] [Google Scholar]
- 17. Fredrickson BL, Branigan C. Positive emotions broaden the scope of attention and thought-action repertoires. Cogn Emot. 2005;19(3):313–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Benyamini Y. Can high optimism and high pessimism co-exist? Findings from arthritis patients coping with pain. Pers Individ Dif. 2005;38(6):1463–1473. [Google Scholar]
- 19. Dubois CM, Beach SR, Kashdan TB, et al. . Positive psychological attributes and cardiac outcomes: Associations, mechanisms, and interventions. Psychosomatics. 2012;53(4):303–318. [DOI] [PubMed] [Google Scholar]
- 20. Kim ES, Park N, Peterson C. Dispositional optimism protects older adults from stroke: The Health and Retirement Study. Stroke. 2011;42(10):2855–2859. [DOI] [PubMed] [Google Scholar]
- 21. de Moor JS, de Moor CA, Basen-Engquist K, Kudelka A, Bevers MW, Cohen L. Optimism, distress, health-related quality of life, and change in cancer antigen 125 among patients with ovarian cancer undergoing chemotherapy. Psychosom Med. 2006;68(4):555–562. [DOI] [PubMed] [Google Scholar]
- 22. Steptoe A, Demakakos P, de Oliveira C, Wardle J. Distinctive biological correlates of positive psychological well-being in older men and women. Psychosom Med. 2012;74(5):501–508. [DOI] [PubMed] [Google Scholar]
- 23. Grote NK, Bledsoe SE. Predicting postpartum depressive symptoms in new mothers: The role of optimism and stress frequency during pregnancy. Health Soc Work. 2007;32(2):107–118. [DOI] [PubMed] [Google Scholar]
- 24. McHugh RK, Kaufman JS, Frost KH, Fitzmaurice GM, Weiss RD. Positive affect and stress reactivity in alcohol-dependent outpatients. J Stud Alcohol Drugs. 2013;74(1):152–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rasmussen HN, Scheier MF, Greenhouse JB. Optimism and physical health: A meta-analytic review. Ann Behav Med. 2009;37(3):239–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sapranaviciute-Zabazlajeva L, Luksiene D, Virviciute D, Bobak M, Tamosiunas A. Link between healthy lifestyle and psychological well-being in Lithuanian adults aged 45-72: A cross-sectional study. BMJ Open. 2017;7(4):e014240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Barros VV, Kozasa EH, Formagini TD, Pereira LH, Ronzani TM. Smokers show lower levels of psychological well-being and mindfulness than non-smokers. PLoS One. 2015;10(8):e0135377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Pahl K, Brook JS, Koppel J, Lee JY. Unexpected benefits: Pathways from smoking restrictions in the home to psychological well-being and distress among urban Black and Puerto Rican Americans. Nicotine Tob Res. 2011;13(8):706–713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kahler CW, Spillane NS, Day AM, et al. . Positive psychotherapy for smoking cessation: A pilot randomized controlled trial. Nicotine Tob Res. 2015;17(11):1385–1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Tiffany ST, Friedman L, Greenfield SF, Hasin DS, Jackson R. Beyond drug use: A systematic consideration of other outcomes in evaluations of treatments for substance use disorders. Addiction. 2012;107(4):709–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ryff CD, Singer B. The contours of positive human health. Psychol Inq. 1998;9(1):1–28. [Google Scholar]
- 32. Kobau R, Seligman ME, Peterson C, et al. . Mental health promotion in public health: Perspectives and strategies from positive psychology. Am J Public Health. 2011;101(8):e1–e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Sachs-Ericsson N, Collins N, Schmidt B, Zvolensky M. Older adults and smoking: Characteristics, nicotine dependence and prevalence of DSM-IV 12-month disorders. Aging Ment Health. 2011;15(1):132–141. [DOI] [PubMed] [Google Scholar]
- 34. Kleykamp BA, Heishman SJ. The older smoker. JAMA. 2011;306(8):876–877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hall SM, Humfleet GL, Muñoz RF, Reus VI, Robbins JA, Prochaska JJ. Extended treatment of older cigarette smokers. Addiction. 2009;104(6):1043–1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Diener E, Fujita F, Tay L, Biswas-Diener R. Purpose, mood, and pleasure in predicting satisfaction judgments. Social Indicators Research. 2012;105(3):333–341. [Google Scholar]
- 37. Steger MF, Kashdan TB, Oishi S. Being good by doing good: Daily eudaimonic activity and well-being. J Rese Pers. 2008;42(1):22–42. [Google Scholar]
- 38. Health and Retirement Study. HRS 2006 Core (Final V3.0). In: Michigan Uo, ed. U01AG009740) NIoAgnN, trans. Ann Arbor, MI: University of Michigan; 2014. [Google Scholar]
- 39. Health and Retirement Study. HRS 2010 Core (Final V5.0). In: Michigan Uo, ed. U01AG009740) NIoAgnN, trans. Ann Arbor, MI: University of Michigan; 2014. [Google Scholar]
- 40. Wallace RB, Herzog AR. Overview of the health measures in the health and retirement study. J Hum Resour. 1995;30:S84–S107. [Google Scholar]
- 41. Diener E, Emmons RA, Larsen RJ, Griffin S. The Satisfaction With Life Scale. J Pers Assess. 1985;49(1):71–75. [DOI] [PubMed] [Google Scholar]
- 42. Pavot W, Diener E. Review of the satisfaction with life scale. Psychol Assess. 1993;5(2):164–172. [Google Scholar]
- 43. Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A reevaluation of the Life Orientation Test. J Pers Soc Psychol. 1994;67(6):1063–1078. [DOI] [PubMed] [Google Scholar]
- 44. Ryff C, Almeida DM, Ayanian J, et al. . National Survey of Midlife Development in the United States (MIDUS II), 2004–2006. Inter-university Consortium for Political and Social Research (ICPSR) Ann Arbor, MI; 2012. 10.3886/ICPSR04652.v7 [DOI] [Google Scholar]
- 45. Watson D, Clark LA.. The PANAS-X: Manual for the Positive and Negative Affect Schedule—Expanded form. Iowa City, IA: University of Iowa; 1994. [Google Scholar]
- 46. Ryff CD, Keyes CL. The structure of psychological well-being revisited. J Pers Soc Psychol. 1995;69(4):719–727. [DOI] [PubMed] [Google Scholar]
- 47. Keyes CL, Shmotkin D, Ryff CD. Optimizing well-being: The empirical encounter of two traditions. J Pers Soc Psychol. 2002;82(6):1007–1022. [PubMed] [Google Scholar]
- 48. Ryff CD. Happiness is everything, or is it?J Pers Soc Psychol. 1989;57(6):1069–1081. [Google Scholar]
- 49. Muthén LK, Muthén BO.. Mplus User’s Guide. 7th ed Los Angeles, CA: Muthén & Muthén; 1998–2012. [Google Scholar]
- 50. Haziza D, Lesage É. A discussion of weighting procedures for unit nonresponse. J Off Stat. 2016;32(1):129–145. [Google Scholar]
- 51. Kott PS, Liao D. Calibration weighting for nonresponse that is not missing at random: Allowing more calibration than response-model variables. J Surv Stat Methodol. 2017;5(2): 159–174. [Google Scholar]
- 52. Jamal A, Phillips E, Gentzke AS, et al. . Current cigarette smoking among adults - United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(2):53–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Tugade MM, Fredrickson BL. Resilient individuals use positive emotions to bounce back from negative emotional experiences. J Pers Soc Psychol. 2004;86(2):320–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Seligman MEP, Schulman P. Explanatory style as a predictor of productivity and quitting among life insurance sales agents. J Pers Soc Psychol. 1986;50(4):832. [Google Scholar]
- 55. Meevissen YM, Peters ML, Alberts HJ. Become more optimistic by imagining a best possible self: Effects of a two week intervention. J Behav Ther Exp Psychiatry. 2011;42(3):371–378. [DOI] [PubMed] [Google Scholar]
- 56. Wood AM, Froh JJ, Geraghty AW. Gratitude and well-being: A review and theoretical integration. Clin Psychol Rev. 2010;30(7):890–905. [DOI] [PubMed] [Google Scholar]