Abstract
Background
Percutaneous endoscopic lumbar discectomy (PELD) has become one of the most popular minimally invasive surgeries for lumbar disc herniation (LDH), however, very highly migrated LDH is still a tricky issue for PELD. This study reported a new endoscopic discectomy strategy for the treatment of very highly migrated LDH between the L4/5 and L5/S1 level.
Material/Methods
The current study retrospectively analyzed 12 patients who accepted PELD for very highly migrated LDH between the L4/5 and L5/S1 level. Under local anesthesia, the transforaminal approach was chosen for the L4/5 level and the interlaminar approach was chosen for the L5/S1 level. The 10-point visual analogue scale (VAS) was used to assess back pain (VAS-Back) and leg pain (VAS-Leg). Oswestry disability index (ODI) and Modified Mac Nab Criteria were adopted as the functional evaluation methods. All patients were followed in the outpatient department for at least 12 months after their operation.
Results
Our study showed that very highly migrated disc between L4/5 and L5/S1 level could be removed completely by this strategy. Except for 1 case of postoperative dysesthesia and 1 case of dural tear, no severe complication occurred. At the last follow-up, the average VAS-Back score of the study patients was reduced from 5.17±2.12 to 2.08±1.08 (P<0.05) and the average VAS-Leg score was reduced from 7.25±1.48 to 1.33±0.89 (P<0.05). The average ODI scores improved from 48.50±10.59 to 13.00±2.76 (P<0.05). According to the Modified Mac Nab Criteria, 83.33% of patients (10 out of 12 patients) received an excellent or good recovery and no poor result was reported. No recurrence was observed during follow up.
Conclusions
PELD via a transforaminal and interlaminar combined approach provides an alternative option for select patients with very highly migrated LDH between the L4/5 and L5/S1 level.
MeSH Keywords: Diskectomy, Percutaneous; Intervertebral Disc Degeneration; Lumbar Vertebrae; Osteoarthritis, Spine; Spinal Cord Compression
Background
Nowadays, percutaneous endoscopic lumbar discectomy (PELD) has become one of the most popular minimally invasive surgeries for lumbar disc herniation (LDH) [1]. The indication spectrum of PELD has been expanded extensively due to the introduction of techniques like foraminoplasty and corresponding instruments like high-speed burrs [2].
Generally, disc migration is classified into 4 zones (Zone 1–4) depending on the direction and distance from the disc space [3]. Once the herniated fragments migrate beyond these zones (Zone 5–6), it is considered to be a very highly migrated disc herniation (Figure 1). Normally, PELD could be used to remove nearly all types of migrated intervertebral disc herniation. However, very highly migrated disc herniation is still a great challenge for PELD through single level transforaminal or interlaminar approach because the endoscopic instruments are straight and rigid [4]. Despite the limitation of endoscopic instruments, several modified techniques of PELD have been proposed to deal with the highly or even very highly migrated LDH, such as the foraminoplasty, contralateral transforaminal approach, transpedicle approach, and translaminar approach [5–8]. However, several shortcomings of these modified techniques should be noted, such as the high rate of failure, massive bone resection, increased operating difficulty, and great demand of equipment.
Figure 1.
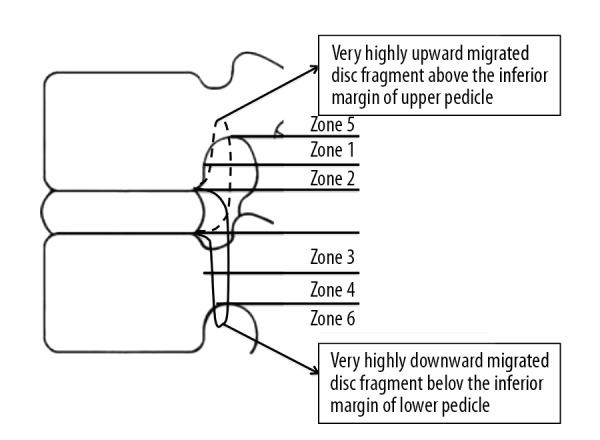
Schematic of highly migrated disc. Zone 1, far upward; Zone 2, near upward; Zone 3, near downward; Zone 4, far downward; Zone 5, very highly upward; Zone 6, very highly downward.
SD – standard deviation.
The interlaminar approach, which bypasses the blockade of iliac crest, reduces the difficulty of puncture and radiation exposure [9,10]. It is believed that interlaminar approach has advantage over transforaminal approach in treating migrated LDH [11]. But this approach reaches herniated disc tissue via the spinal canal, which might increase the risk of epidural fibrosis and scar tissue formation [12,13]. In addition, because the interlaminar window is limited, the range of adjustment of one level interlaminar approach is restricted and it might not be able to remove all far migrated disc tissue. As for the transforaminal approach, it is challenging to achieve an ideal position of endoscope to herniated tissue between the L4/5 and L5/S1 level because of the limited range of endoscope’s adjustment on the sagittal plane, as a result, massive bone resection has to be performed to reach the migrated fragment [14]. Open surgery often has to been chosen due to the scarce capacity of current PELD techniques in the management of highly migrated LDH.
In order to provide an alternative option for select cases with very highly migrated LDH, we performed PELD via a transforaminal and interlaminar combined approach for very highly LDH between the L4/5 and L5/S1 level. In the current study, we introduced our early experience with this strategy and evaluated its safety and efficacy.
Material and Methods
General information
This study was approved by Institutional Review Board of our hospital and informed consent was obtained from all individual participants. The current study retrospectively reviewed all patients who accepted PELD in our department because of L4/5 or L5/S1 disc herniation from January 2015 to October 2016. The inclusion criteria were as follows: 1) low back pain and sciatica history; 2) computed tomography and magnetic resonance imaging confirmed very highly migrated LDH, including downward migrated L4/5 disc fragment below the inferior margin of lower pedicle and upward migrated L5/S1 disc fragment over the inferior margin of upper pedicle; and 3) failure of standard conservative treatment for at least 3 months. The exclusion criteria were as follows: 1) radiographic findings were not consistent with patients’ symptoms or signs; 2) multiple level disc herniation; 3) lumbar instability, severe spinal canal stenosis, cauda equina syndrome, or other spinal diseases; 4) previous surgery history for herniated level; and 5) other severe underlying diseases. There were 12 patients included in this study.
Surgical procedure
Patients were placed on a radiolucent operating table in a prone position. Local anesthesia and intravenous sedation were chosen for this strategy. Under the guidance of x-ray, the puncture trajectory was designed and marked on the surface [15].
Transforaminal approach was performed for the L4/5 level. Following the designed puncture trajectory, a puncture needle was inserted, and skin incision and soft tissue dilatation were performed. Then, foraminoplasty was performed by bone dills to enlarge the intervertebral foramina. The working cannula was then introduced, and the endoscope was inserted through working cannula. The visible herniated mass should be first grabbed at the proximal end and removed as a whole. Then, debridement of the intervertebral space was performed. Leaving the working cannula in position, the endoscope could be retrieved.
The interlaminar approach was adopted for the L5/S1 level. A puncture needle was inserted into the lesion side of the L5/S1 laminar interspace. A working annular was rotated along the dilator and confirmed by x-ray for an ideal position. The endoscope was then introduced through the working cannula. The working cannula was rotated forward into the spinal canal, which was opened by partial resection of ligamentum flavum. The working cannula and endoscope were introduced over the shoulder of the nerve root to reach the upper space of this level. After the identification of herniated mass, the oblique opening of working cannula was used to tract the nerve root and dural sac by rotation. Curved disc forceps were used to probe upward to find any migrated fragment. And debridement of the intervertebral space was performed. Because the free nucleus might migrate upwards during the operation at the L5/S1 level, the endoscope was reinserted into the working cannula at the L4/5 level to detect any possible migrated tissues.
Data collection
The demographic data, operation time, fluoroscopy times, hospital stay, and complications were collected from medical records. The 10-point visual analogue scale (VAS) was used to assess back pain (VAS-Back) and leg pain (VAS-Leg) at the following time points: pre-operation, 1st postoperative day, 3rd postoperative month, 12th postoperative month and the last follow-up. The Oswestry disability index (ODI) was adopted to evaluate patient’s function status at the following time points: pre-operation, 12th postoperative month, and last follow-up. Modified Mac Nab Criteria was used to analyze patient’s satisfaction at 12th postoperative month and last follow-up.
Statistical analysis
All statistical analyses were performed using SPSS (version 21.0, IBM Corp., Chicago, IL, USA). Continuous variables were presented as mean±standard deviation. Student’s t-test was used to compare the continuous variables such as VAS-Back, VAS-Leg, and ODI scores between different time points. All P values were 2-sided and P<0.05 was regarded as statistically significant.
Results
Characteristics and operation-related data of included patients
Characteristics are listed in Table 1; there were 7 males and 5 females who accepted PELD for very highly migrated LDH between the L4/5 and L5/S1 level. The median age of these patients was 42 years old (range, 18–67 years). There were 10 cases of far-downward migrated L4/5 LDH and 2 cases of far-upward migrated L5/S1 LDH. The mean operation time and fluoroscopy times were 87.50 minutes and 37.50 times, respectively. The mean hospital stay was 3.42 days and the average follow-up time was 17.50 months.
Table 1.
Characteristics and operation-related data of included patients (n=12).
| Variables | Results |
|---|---|
| Gender (male: female) (n) | 7: 5 |
| Age (median, range) (year) | 42 (18–67) |
| Herniated segment (L4/5: L5/S1) (n) | 10: 2 |
| Operation time (mean±SD) (minute) | 87.50±15.00 |
| Fluoroscopy times (mean±SD) (n) | 37.50±8.26 |
| L4/5 level | 26.00±7.77 |
| L5/S1 level | 11.50±3.09 |
| Hospital stay (mean±SD) (day) | 3.42±1.00 |
| Follow-up time (mean±SD) (month) | 17.50±4.76 |
| Complications (n) | |
| Postoperative dysesthesia | 1 |
| Dural tear | 1 |
Clinical outcomes
The very highly migrated disc between the L4/5 and L5/S1 level was removed completely in all patients. All patients received significant pain relief after the surgery. The average VAS-Back score was reduced from 5.17±2.12 to 3.67±0.98 (P<0.05) at the 1st postoperative day and reduced to 2.08±1.08 (P<0.05) at the last follow-up. The average VAS-Leg score was reduced from 7.25±1.48 to 3.50±1.00 (P<0.05) at the 1st postoperative day and reduced to 1.33±0.89 (P<0.05) at the last follow-up. As for function improvement, the average ODI scores improved from 48.50±10.59 to 13.00±2.76 (P<0.05) at the last follow up (Table 2). According to the Modified Mac Nab Criteria, 83.33% of patients (10 out of 12 patients) received an excellent or good recovery and no poor result was reported (Table 3).
Table 2.
Pain relief and functional improvement.
| Variables | Pre-operation | 1st postoperative day | 3rd postoperative month | 12th postoperative month | Last follow up |
|---|---|---|---|---|---|
| VAS-Back | 5.17±2.12 | 3.67±0.98* | 2.58±1.16* | 2.42±0.90* | 2.08±1.08* |
| VAS-Leg | 7.25±1.48 | 3.50±1.00* | 2.00±1.04* | 1.58±1.08* | 1.33±0.89* |
| ODI scores | 48.50±10.59 | – | – | 18.00±6.49 | 13.00±2.76* |
P<0.05 represents a statistical difference from preoperative data.
VAS – visual analogue scale, ODI – Oswestry disability index.
Table 3.
Modified Mac Nab criteria.
| Excellent | Good | Fair | Poor | |
|---|---|---|---|---|
| Patients (n) | 3 | 7 | 2 | 0 |
| Percentage (%) | 25.00% | 58.33% | 16.67% | 0% |
With respect to complications, 1 patient suffered from postoperative dysesthesia and the symptom disappeared in 11 days after the application of dexamethasone and neurotrophic drugs. Dural tear at L5/S1 level occurred in 1 patient, however, the dural laceration was very small and the patient received a good recovery. No recurrence was observed during the follow-up (Table 1).
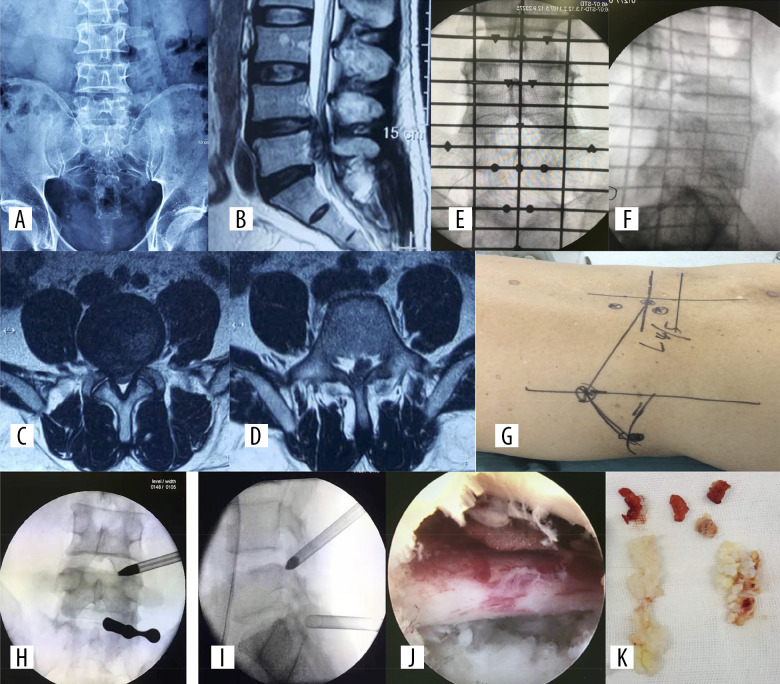
Case presentation
A 63-year-old male admitted to our department for severe left leg radicular pain of nearly 10 months. This patient was diagnosed with very highly downward migrated L4/5 LDH in consideration of the physical examination and imaging findings. The herniated mass was completely removed during the surgery. This patient received immediate pain relief and was discharged from hospital on the 3rd postoperative day. During the follow-up, the functional improvement was satisfactory (Figure 2).
Figure 2.
Case presentation. (A) Pelvis anterior-posterior x-ray image. (B) Magnetic resonance imaging (MRI) sagittal view of herniated level. (C) MRI cross-section view of L4/5. (D) MRI cross-section view of L5/S1. (E) Anterior-posterior x-ray image with surface locator. (F) Lateral x-ray image with surface locator. (G) The rough shape of anatomical structures like pedicles and iliac crest was drawn on skin, and puncture targets and trajectories were marked on skin. (H) Anteroposterior x-ray view of the working cannulas at L4/5 and L5/S1. (I) Lateral x-ray view of the working cannulas at L4/5 and L5/S1. (J) The decompressed nerve root under endoscopic view. (K) Two huge migrated fragments were removed).
Discussion
PELD has been widely used in the management of LDH with the satisfactory efficacy and less iatrogenic injury [10]. Normally, disc migration can be classified into 4 degrees: far upward, near upward, near downward and far downward [3]. Once the disc fragment migrates beyond this range, we define it as very highly migrated disc herniation. In the current study, we introduced the PELD via a transforaminal and interlaminar combined approach to manage very highly migrated LDH. All patients received significant pain reduction and function improvement after surgery, no severe complication occurred during the surgery, and most of the patients (83%) obtained an excellent or good recovery at the last follow-up. Therefore, our study showed PELD via a transforaminal and interlaminar combined approach could manage a case of very highly migrated disc herniation efficiently and safely; and as a result, this technique might be a feasible alternative to deal with the very highly migrated LDH.
For the strategy described in the current study, the transforaminal approach was routinely performed at the L4/5 level. An ideal position of the puncture needle could be achieved with low-dose radiation exposure and the working cannula could be smoothly placed without massive osseous resection. Normally, the herniated disc tissue could be easily visualized, and we could remove part of the migrated disc tissues through this approach. For very highly downward migrated the L4/5 disc herniation, the transforaminal approach at this level could identify the proximal end of herniated disc and remove most of it. The interlaminar approach was routinely performed at the L5/S1 level to avoid problems caused by high iliac, thick transverse process, and narrowed foramina. Since the puncture for the interlaminar approach is less demanding, the puncture needle and working cannula could be easily placed without much radiation exposure. The posterior space of the L5 vertebra body could be reached by slight traction of the nerve root and dural sac. Migrated disc tissues could be detected and removed by probing to the upper space with curved disc forceps. The reintroduce of endoscope for the L4/5 level at the end of the surgery would make sure that all herniated tissues were removed.
Several endoscopic techniques have been reported to treat the highly migrated LDH. Choi et al. used the foraminoplasty in a transforaminal approach to treat highly migrated LDH, and 91.4% of patients (54 out of 59 patients) obtained satisfactory results. However, removal of the part of superior facet and inferior pedicle may lead to instability of lumbar segment [5]. Wang et al. used the transpedicle approach to treat highly migrated LDH of 2 patients by making a bone hole on the pedicle [7]. And migrated disc mass was completely removed in both patients. However, regardless of the bone resection, bleeding, and limited endoscope’s adjustment, there was a high demand in accurate surface locating when adopting this technique [7]. Kim et al. introduced the transforaminal contralateral approach for far migrated LDH in 5 patients, and all patients received the significant pain relief after the surgery [16]. Nevertheless, the disadvantages of this technique should not be ignored, including the risk of contralateral leg dysesthesia, steep learning curve, and narrow indication [16]. Du et al. introduced a translaminar approach for 7 cases with highly down-migrated LDH by opening a bone hole on the vertebral lamina [8]. All patients obtained the significant pain reduction and function improvement after the surgery, and no recurrence was observed during the follow-up period. However, the high demand of precise surface location, difficulty to treat calcified tissue and increased bleeding from the edge of the hold might limit the promotion of this method [8].
Some limitations should be considered when interpreting our data. The retrospective design might lead to selection bias and the small sample size might reduce the stringency of our results. Besides, there was no comparison with other surgical techniques in this study. However, it should be noted that we aimed to introduce a new endoscopic discectomy strategy for the treatment of very highly migrated disc between the L4/5 and L5/S1 level, and our results demonstrated this strategy was effective and safe.
Conclusions
Percutaneous endoscopic discectomy via a transforaminal and interlaminar combined approach can treat very highly migrated LDH between the L4/5 and L5/S1 level safely and effectively, and this technique could provide an alternative option for select patients with very highly migrated LDH.
Abbreviation
- PELD
percutaneous endoscopic lumbar discectomy
- LDH
lumbar disc herniation
- VAS
visual analogue scale
- VAS-Back
VAS for back pain
- VAS-Leg
VAS for leg pain
- ODI
Oswestry disability index
Footnotes
Conflict of interest
None.
Source of support: This work was supported by the Research Project of Shanghai Tenth People’s Hospital (grant numbers 04.01.18054)
References
- 1.Ahn Y. Endoscopic spine discectomy: Indications and outcomes. Int Orthop. 2019;43(4):909–16. doi: 10.1007/s00264-018-04283-w. [DOI] [PubMed] [Google Scholar]
- 2.Kim HS, Paudel B, Jang JS, et al. Percutaneous endoscopic lumbar discectomy for all types of lumbar disc herniations (LDH) including severely difficult and extremely difficult LDH cases. Pain Physician. 2018;21(4):E401–8. [PubMed] [Google Scholar]
- 3.Lee S, Kim SK, Lee SH, et al. Percutaneous endoscopic lumbar discectomy for migrated disc herniation: Classification of disc migration and surgical approaches. Eur Spine J. 2007;16(3):431–37. doi: 10.1007/s00586-006-0219-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Choi KC, Lee JH, Kim JS, et al. Unsuccessful percutaneous endoscopic lumbar discectomy: A single-center experience of 10,228 cases. Neurosurgery. 2015;76(4):372–80. doi: 10.1227/NEU.0000000000000628. discussion 380–81; quiz 381. [DOI] [PubMed] [Google Scholar]
- 5.Choi G, Lee SH, Lokhande P, et al. Percutaneous endoscopic approach for highly migrated intracanal disc herniations by foraminoplastic technique using rigid working channel endoscope. Spine (Phila Pa 1976) 2008;33(15):E508–15. doi: 10.1097/BRS.0b013e31817bfa1a. [DOI] [PubMed] [Google Scholar]
- 6.Liu C, Chu L, Yong HC, et al. Percutaneous endoscopic lumbar discectomy for highly migrated lumbar disc herniation. Pain Physician. 2017;20(1):E75–84. [PubMed] [Google Scholar]
- 7.Wang D, Pan H, Hu Q, et al. Percutaneous endoscopic transpedicle approach for herniated nucleus pulposus in the lumbar hidden zone. Asian J Endosc Surg. 2017;10(1):87–91. doi: 10.1111/ases.12320. [DOI] [PubMed] [Google Scholar]
- 8.Du J, Tang X, Jing X, et al. Outcomes of percutaneous endoscopic lumbar discectomy via a translaminar approach, especially for soft, highly down-migrated lumbar disc herniation. Int Orthop. 2016;40(6):1247–52. doi: 10.1007/s00264-016-3177-4. [DOI] [PubMed] [Google Scholar]
- 9.Nie H, Zeng J, Song Y, et al. Percutaneous endoscopic lumbar discectomy for L5-S1 disc herniation via an interlaminar approach versus a transforaminal approach: A prospective randomized controlled study with 2-year follow up. Spine (Phila Pa 1976) 2016;(41 Suppl 19):B30–37. doi: 10.1097/BRS.0000000000001810. [DOI] [PubMed] [Google Scholar]
- 10.Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: A prospective, randomized, controlled study. Spine (Phila Pa 1976) 2008;33(9):931–39. doi: 10.1097/BRS.0b013e31816c8af7. [DOI] [PubMed] [Google Scholar]
- 11.Choi KC, Kim JS, Ryu KS, et al. Percutaneous endoscopic lumbar discectomy for L5–S1 disc herniation: transforaminal versus interlaminar approach. Pain Physician. 2013;16(6):547–56. [PubMed] [Google Scholar]
- 12.Aydin Y, Ziyal IM, Duman H, et al. Clinical and radiological results of lumbar microdiskectomy technique with preserving of ligamentum flavum comparing to the standard microdiskectomy technique. Surg Neurol. 2002;57(1):5–13. doi: 10.1016/s0090-3019(01)00677-2. discussion 13–14. [DOI] [PubMed] [Google Scholar]
- 13.Ozer AF, Oktenoglu T, Sasani M, et al. Preserving the ligamentum flavum in lumbar discectomy: A new technique that prevents scar tissue formation in the first 6 months postsurgery. Neurosurgery. 2006;59(Suppl 1):ONS126–33. doi: 10.1227/01.NEU.0000220078.90175.E6. discussion ONS126-33. [DOI] [PubMed] [Google Scholar]
- 14.Gadjradj PS, van Tulder MW, Dirven CM, et al. Clinical outcomes after percutaneous transforaminal endoscopic discectomy for lumbar disc herniation: A prospective case series. Neurosurg Focus. 2016;40(2):E3. doi: 10.3171/2015.10.FOCUS15484. [DOI] [PubMed] [Google Scholar]
- 15.Fan G, Wang C, Gu X, et al. Trajectory planning and guided punctures with isocentric navigation in posterolateral endoscopic lumbar discectomy. World Neurosurg. 2017;103:899–905.e4. doi: 10.1016/j.wneu.2017.04.034. [DOI] [PubMed] [Google Scholar]
- 16.Kim JS, Choi G, Lee SH. Percutaneous endoscopic lumbar discectomy via contralateral approach: A technical case report. Spine (Phila Pa 1976) 2011;36(17):E1173–78. doi: 10.1097/BRS.0b013e3182264458. [DOI] [PubMed] [Google Scholar]