BACKGROUND
The Covid-19 pandemic has affected all aspects of nursing care including wound care. In an effort to minimize unnecessary contact with patients and decrease the spread of the virus, wound providers need to consider alternative strategies to evaluate wounds using telehealth or telemedicine. Wound consultations (either in person or remotely) can be managed using principles of basic wound assessment and photography (eg, may be digital or video-based dependent on facility-approved methods) described as follows:
Follow facility guidelines for handwashing and donning and doffing personal protective equipment (PPE).
Gather all supplies necessary for the wound assessment and treatment before entering the isolation room; limit supplies taken in that need to be removed from the room.
-
Wound assessment:
Location: Describe the site of each wound specifically (eg, not just “leg” or “buttocks”).
Wound measurements: Use a clock face mentally imagined over the surface of the wound bed (12 o'clock is toward the head); measure length and width using a disposable measuring tape or stick noting clock positions (eg, 10-4 greatest length, perpendicular 7-1 is width). Use a measuring stick or sterile cotton-tipped applicator to probe depth, measure at the greatest depth perpendicular to the wound edge (if able).
Wound drainage amount: None, scant, minimal, moderate, heavy (dripping).
Wound drainage consistency and color: Thin or thick, opaque or clear, white, yellow, tan, brown, red, or other.
Wound edges: Flat, elevated, edematous, rolled.
Skin around wound: Normal and warm, red (<5 cm) and warm, red (extending >5cm) and hot to touch, pale and cool to touch (may not be able to discern temperature through the PPE, do NOT remove PPE to feel for warmth/coolness).
-
Photograph (eg, phone, tablet, camera, video; based on facility guidelines and patient consent):
Maximize lighting by turning on all exam lights in the room.
Obtain image using an approved source of photography at the facility (eg, phone, tablet, camera, video screenshot).
-
Obtain the first photograph (if possible) of the entire body surface where the wound is located and the second photograph of the wound within 6 to 12 inches (about 10-15 cm) from the wound surface (distance will vary based on the device used for photography).
Transfer images to the electronic medical record (EMR) per facility guidelines; if the facility does not use an EMR, follow facility guidelines for photo storage.
Make sure images are in focus.
Maintain camera lens perpendicular to the body surface, not at an angle.
-
Place measuring guide in the photograph for size reference; follow facility guidelines for information to include in the photograph/image (eg, medical record number, wound location, date).
Dispose of measuring tape/guide per facility infection prevention policy.
Wipe the device (eg, phone, tablet, camera) according to facility guidelines, set aside on clean surface away from direct patient care area, and let it dry as recommended based on solution used prior to removal from the patient's room.
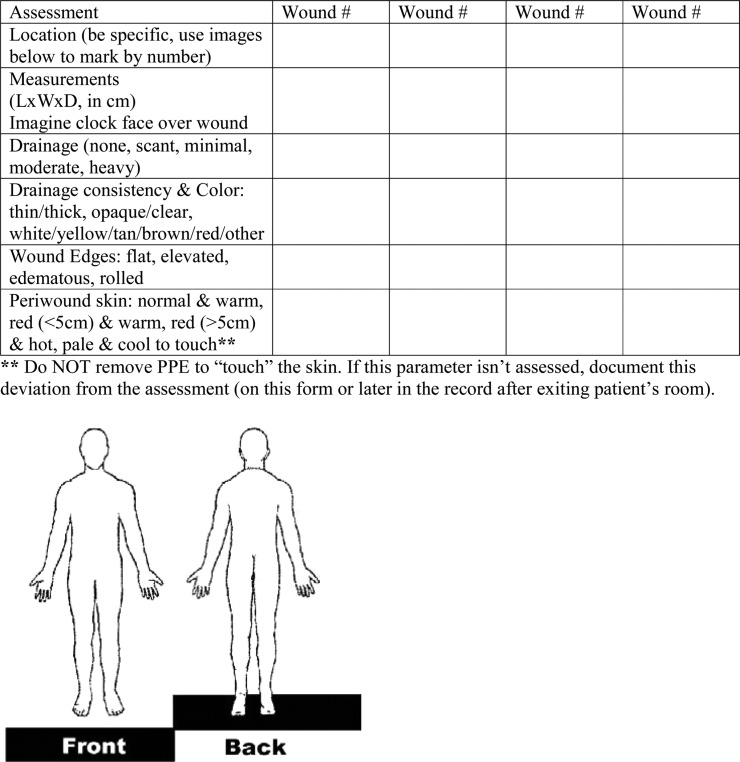
The form (Figure) can be photocopied on paper to take into the isolation room for bedside wound documentation. The form can be photographed and submitted to an EMR for documentation similar to a photograph (if allowed by facility guidelines) and then the paper is discarded in the isolation room. Additional documentation can be completed outside the isolation room and photographs (wound and/or documentation sheet) can be referenced per facility guidelines.
Figure.
Table & figure for wound documentation in isolation. Copyright© 2020 by the Wound, Ostomy and Continence Nurses Society (WOCN). Date of publication: April 2020. No part of this publication may be reproduced, photocopied, or republished in any form, in whole or in part, without written permission of the WOCN Society.
CONTRIBUTORS
Originated by: Board of Directors, WOCN Society
Original Publication Date: April 2020
The Wound, Ostomy and Continence Nurses Society would like to thank many members who have provided comments and guidance for this document. Especially integral are Task Force members:
Derik Alexander, MSN, RN, FNP-BC, CWOCN, CFCN
Christine Berke, MSN, APRN-NP, CWOCN-AP, AGPCNP-BC
Vittoria (Vicky) Pontieri-Lewis, MS, RN, ACNS-BC, CWOCN
Footnotes
The authors declare no conflicts of interest.
Contributor Information
Collaborators: WOCN Board of Directors Task Force