Abstract
Background
Washington State experienced the first major outbreak of COVID-19 in the US and despite a significant number of cases, has seen a relatively low death rate per million population compared with other states with major outbreaks, and has seen a substantial decrease in the projections for healthcare use, that is, “flattening the curve.” This consensus report seeks to identify the key factors contributing to the effective health system disaster response in western WA.
Methods
A multidisciplinary, expert panel including individuals and organizations who were integral to managing the public health and emergency healthcare system response were engaged in a consensus process to identify the key themes and lessons learned and develop recommendations for ongoing management of the COVID-19 pandemic.
Results
Six key themes were identified, including early communication and coordination among stakeholders; regional coordination of the healthcare system response; rapid development and access to viral testing; proactive management of long-term care and skilled nursing facilities; proactive management of vulnerable populations; and effective physical distancing in the community.
Conclusions
Based on the lessons learned in each of the areas identified by the panel, 11 recommendations are provided to support the healthcare system disaster response in managing future outbreaks.
Abbreviations and Acronyms: DMCC, Disaster Medical Control Center; EMS, emergency medical services; HMC, Harborview Medical Center; I&O, isolation and quarantine; LTCF, long-term care facility; NWHRN, Northwest Healthcare Response Network; PHSKC, Public Health Seattle & King County; PPE, personal protective equipment; UW, University of Washington; WRC, Western Washington Regional COVID Coordinating Center
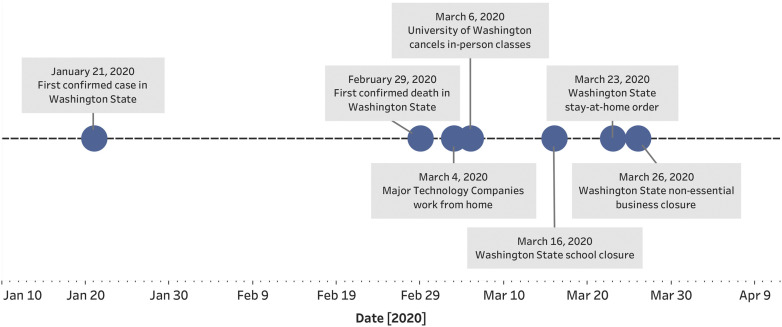
As of June 5, 2020, more than 6.7 million people worldwide have been infected with COVID-19, with more than 1.9 million (28%) cases in the US. Managing this pandemic has put considerable strain on healthcare systems, with many regions experiencing a surge in critically ill patients that exceeds the capacity of the system. The first confirmed case of COVID-19 in the US was identified in Washington state on January 21, 2020, the first COVID-19 outbreak in a long-term care facility (LTCF) in King County, WA identified on February 28, 2020, and the first confirmed death in King County on February 29, 2020. Ultimately, 167 cases were identified in the LTCF outbreak, involving 101 residents, 50 staff, and 16 visitors.1 In response, Public Health Seattle & King County (PHSKC) and the Disaster Medical Control Center (DMCC) at Harborview Medical Center (HMC) mounted a response to stabilize the facility and support regional distribution of patients with assistance from the Northwest Healthcare Response Network (NWHRN) and CDC. In addition, state and local governments began to implement a series of widespread community mitigation measures, including physical distancing, closure of nonessential businesses, closure of schools, and suspension of elective surgical procedures by hospitals (Fig. 1 ).
Figure 1.
Timeline of COVID-19 events in Washington state. This timeline represents the progression from the initial case and first death from COVID-19 in Washington state to the series of events leading to effective physical distancing in the community.
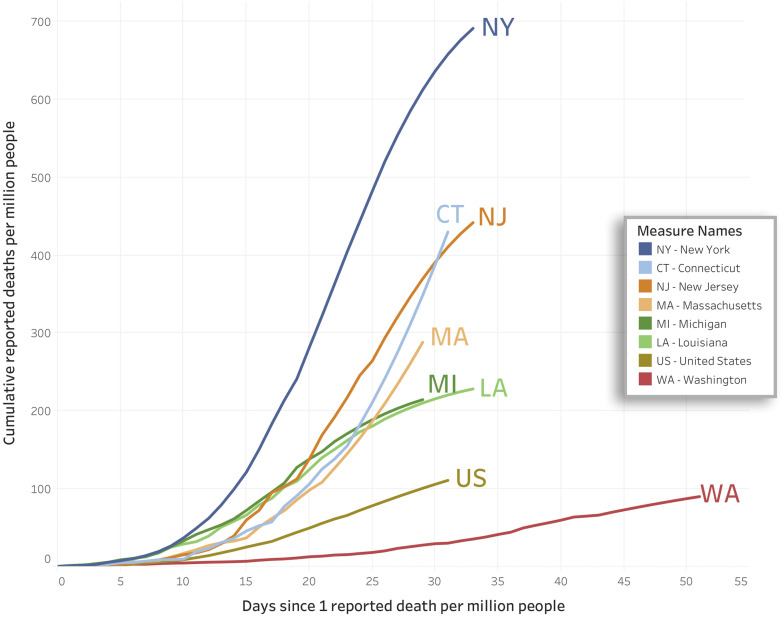
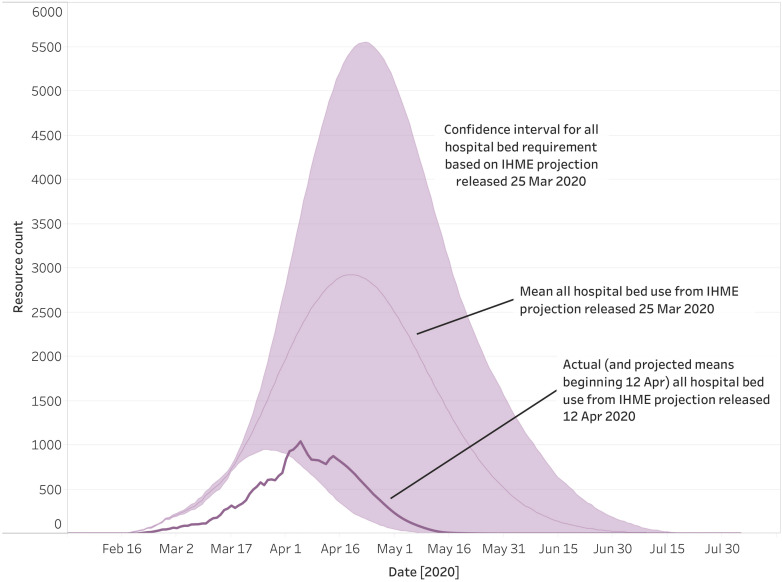
As of June 5, 2020, Washington State has tested 383,587 patients for severe acute respiratory syndrome coronavirus 2 (5.9%% positive) with 22,729 confirmed cases of COVID-19 and 1,138 reported deaths among a statewide population of 7.6 million people. This reflects the lowest death rate per million people among all states that have experienced a major outbreak so far (Fig. 2 ).2 The Institute of Health Metrics and Evaluation has been instrumental in forecasting the projected need for medical resources across the US, which has been critical for surge planning. As shown in Fig. 2, initial estimates on March 25, 2020 were that Washington state would need a mean of 3,000 hospital beds for COVID-19 patients at the peak of the outbreak. These projections were revised on April 12, 2020, suggesting the state had already peaked, with fewer than 1,000 beds required. This is dramatic evidence of “flattening the curve” (Fig. 3 ). As a result, the healthcare systems in western Washington, where the largest number of cases were concentrated, have been able to function without compromising patient care or access to emergency care.
Figure 2.
Institute for Health Metrics and Evaluation (IHME) projections for cumulative deaths per million people by state.2 This figure was based on the IHME model as of April 12, 2020 with projections to April 20, 2020 by state for the 7 states most effected by COVID-19. Cumulative deaths per million population are shown over the days since 1 reported death per million was documented.2
Figure 3.
Institute for Health Metrics and Evaluation (IHME) projections for Washington State: All hospital bed requirement.2 The IHME published an initial estimate of total hospital beds required for COVID-19 patients in Washington State on March 25,2020 (light pink line, shaded pink area represents CIs). New projections were published on April 12, 2020, which incorporated all hospital bed use up to that date (dark pink line) showing a significant reduction compared with initial projections.
Despite this success, until there is an effective vaccine, there are likely to be intermittent outbreaks, especially among vulnerable populations. There is also risk of a second peak of infections as physical distancing orders are relaxed and with seasonal changes later in the year. The objective of this study was to identify the key factors that contributed to the flattening of the curve and an effective healthcare system disaster response in western Washington. This report seeks to capture the lessons learned, but also provide guidance to governmental leaders and healthcare systems in managing the pandemic over time. Our goal is to support the ability of the healthcare systems to meet the needs of patients with COVID-19, maintain access for common medical emergencies, and support the care of patients with chronic health conditions, including those requiring surgical intervention.
Methods
This is a consensus statement based on engagement of a panel of 26 experts who were selected based on their experience and key roles in the response to the COVID-19 outbreak in western Washington. The panel members included representatives from University of Washington (UW) Emergency Medicine leadership for population health and disaster preparedness, PHSKC, HMC Infection Prevention and Control, UW Virology Laboratory and Laboratory Medicine, King County DMCC leadership, NWHRN, UW Trauma system leadership, UW Medicine system leadership, UW post-acute care leadership, and HMC Ambulatory care for vulnerable populations (eAppendix 1). HMC is the safety-net hospital for King County and is managed under contract by UW Medicine. HMC serves as the regions Level I trauma center and as the DMCC. Each of the panel members were contacted and asked to provide a detailed description of the response in their area and asked to identify the key factors that they believe contributed to an effective healthcare system response in western WA.
These responses were collected and reviewed by 3 members of the panel (SM, EB, JL) who formed a steering committee. Qualitative analysis revealed 6 overarching themes that reflected the topics reported by the panel. A White Paper was then drafted organizing the input received into 6 key elements and was sent back to all panelists for review and feedback. There was uniform consensus on the key elements and additional detail was provided to the steering committee as needed.
The lessons learned in each of the 6 domains were then organized by the steering committee into a set of 11 consensus recommendations that are designed to provide guidance for the ongoing response to manage future outbreaks in a community. All panel members approved these recommendations.
Results
The 6 themes identified as key factors in supporting the healthcare system response to the COVID-19 pandemic in western WA were early communication and coordination among all stakeholders, including public health, academia, hospital systems, emergency medical services (EMS), and long-term care facilities; regional coordination and situational awareness of the healthcare system response; rapid development and access to viral testing; proactive management of long-term care and skilled nursing facilities; proactive management of vulnerable populations; and effective physical distancing in the community. A summary of each of these factors will be described.
Overview of factors supporting the healthcare system response
Early communication and coordination among stakeholders
NWHRN is the healthcare coalition for western Washington. In the days after the identification of the state's first case, NWHRN coordinated with PHSKC, HMC Infection Prevention and Control, and the WA Department of Health to support the public health and healthcare response. NWHRN and the Washington State Hospital Association have established networks of communication across individual health systems, which normally function in a competitive healthcare landscape. Daily regional calls and an established electronic platform for communication (WA TRAC) have worked to reinforce interdependent relationships and improve situational awareness across the region.
Although many regions have established practices to manage isolated surge incidents, additional surge strategies are necessary for a protracted event with periods of high resource use. In 2012, the NWHRN developed the Disaster Clinical Advisory Committee, which consists of 45 clinicians representing 18 different specialties and all major healthcare systems in the region. NWHRN also administers the state Disaster Medical Advisory Committee on behalf of the Washington Department of Health, which includes a multidisciplinary group of subject matter experts covering the range of medical care needed for major events, including crisis standards of care. Both committees have brought a strong clinical lens to the response in this pandemic.
Regional coordination and situational awareness
The early cluster of patients at the Kirkland LTCF provided immediate evidence of the need for a regional approach to surveillance and coordination of care. The cluster led to a crisis at the LTCF in which large numbers of staff and residents had become symptomatic and the local hospital had difficulty locating sufficient ventilators.3 This occurred as large amounts of capacity remained within other local healthcare systems.
Regional medical operations center
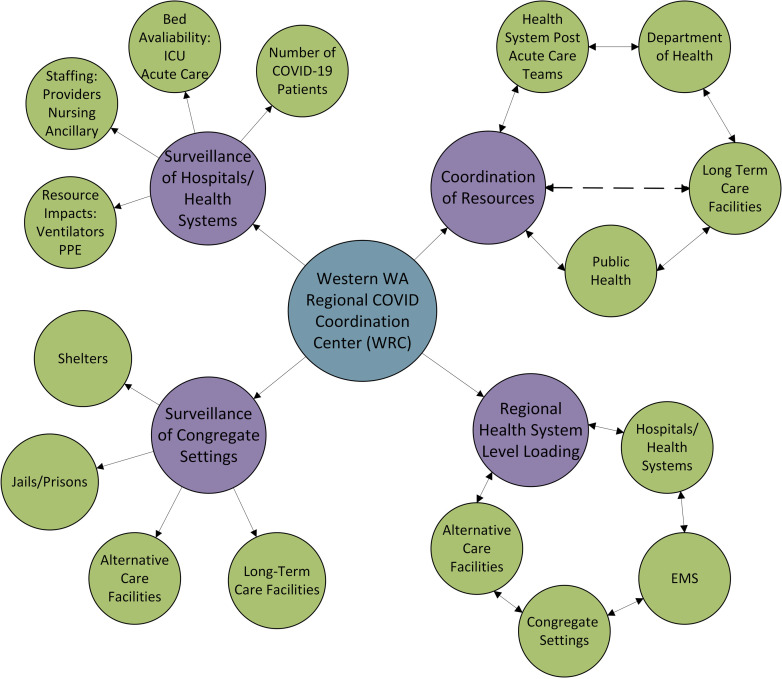
The King County DMCC has served to coordinate and distribute patients across the healthcare system since the initial outbreak. However, the DMCC was designed to manage patient distribution in discrete mass casualty events and had to adapt to meet the ongoing needs of this pandemic. This led to the creation of the Western Washington Regional COVID Coordinating Center (WRC), which functions as a Medical Operations Coordinating Cell4 , 5 (Fig. 4 ).
Figure 4.
Western Washington Regional COVID Coordination Center (WRC). The WRC has 4 pillars of activity including 2 surveillance pillars that provide situational awareness of hospital resources and COVID-19 status in congregate settings and 2 coordination pillars that include coordination of resources and support for long-term care facilities and distribution of patients across area hospitals to level-load the system. EMS, emergency medical services; PPE, personal protective equipment.
COVID-19 outbreaks spread effectively in congregate settings.1 , 6 Spread from a single case can lead to a crisis within the facility and nearby local hospitals. To facilitate this work, the WRC is establishing relationships across the spectrum of congregate living settings, including jails and prisons, homeless shelters, alternate care facilities, and LTCFs. Meetings are conducted with stakeholders to establish points of contact and a shared procedural understanding for functioning and conducting surveillance.
The WRC monitors EMS and public health data to identify outbreaks within the LTCFS, and when clusters of patients are identified, the WRC coordinates with EMS and regional hospitals to balance patient placement. The WRC also assists hospitals at maximum capacity to decompress by transferring groups of COVID-19 or non-COVID-19 patients to other hospitals. The WRC has the capabilities to coordinate this distribution statewide and across states if needed. The primary goal of the WRC is to ensure that any single hospital is not overburdened and to maintain community standards of care and capacity for both COVID-19 and non-COVID-19 patients requiring acute care. Although existing relationships between the DMCC, NWHRN, and the Washington Hospital Association were leveraged to create the coordination for the WRC, the NWHRN is now initiating routine regional and statewide exercises, primarily in the form of virtual tabletop drills to mature this coordination.
NWHRN and the WRC also partnered with Microsoft to build the emergency response platform for improved surveillance of health system variables prone to constraint in the pandemic. The Washington Department of Health has recently adopted the platform and launched it as WAHealth. This solution allows the WRC to visualize resource impacts, including beds, staffing, ventilators, personal protective equipment (PPE), and number of COVID-19 patients across all hospitals. The WRC is working to extend this platform to include LTCFs and EMS.
Rapid development and access to viral testing
Early diagnostic testing is critical to identify COVID-19 cases and slow transmission. As the initial outbreak was unfolding in China and the first viral sequence was published, the UW Virology laboratory quickly designed and obtained reverse transcriptase polymerase chain reaction primers and probes and moved rapidly into initial test validation. State public health laboratories will almost always have the first validated assay in the state and receive early, confirmed positive specimens for a novel pathogen. Close partnering with state laboratories for early validation helps amplify regional testing capacity.
As early CDC testing criteria were restrictive, communities with early clusters had difficulty obtaining testing for the virus. Having established communication between laboratory directors and infectious disease physicians was critical to support early-stage coordination of testing criteria. The ability of reference laboratories to scale and invest resources was also critical. UW Laboratory Medicine supported this rapid investment and expansion of resources to provide 24/7 testing operations, including additional quantitative polymerase chain reaction machines, additional instrumentation, couriers to facilitate transport, and volunteers from research and clinical laboratories across the UW campus. Development of diverse, redundant supply chains and validation techniques was necessary to support continued availability of laboratory consumables. Purchase agreements, financial arrangements (leases, hiring, and contracts), and approval processes were modified to meet the need. The result for UW Virology was an initial testing capacity of 1,000 samples per day, which increased steadily in 6 weeks to a capacity of 7,500 samples per day.
Moving forward it will be essential that the worlds of academia and public health laboratories collaborate and leverage their respective roles to accomplish population-based testing and surveillance. In King County, the Seattle Flu Study and PHSKC have recently announced the initiation of the Seattle Coronavirus Assessment Network, an innovative disease surveillance platform that will allow cross-sectional community surveillance.7
Proactive management of long-term care facilities
LTCFs, such as skilled nursing facilities, are high-risk settings for severe outbreaks. Many lack the infrastructure and supplies necessary to respond to a pandemic. An effective response starts with creation of a centralized disease reporting and outbreak monitoring program, establishment of staffing surge capacity, and collaborations with public health and local healthcare systems to provide on-site support and infection control assistance.
A centralized reporting system is critical for an effective response. Focus must be given to identify distressed LTCFs, identify PPE supply chain challenges, infection prevention education, managing staffing shortages, and support for diagnostic and clinical assistance. A central coordination system must match the urgent needs of an LTCF with predetermined local, county, and state resources identified as the support network. This includes work to monitor safe staffing levels and to coordinate augmentation of staffing from a regional resource pool when staffing ratios become unsafe. Existing public health data and active surveillance activities, such as phone calls to LTCFs experiencing increased EMS use, were used to facilitate this coordination early in the pandemic. However, LTCFs are now required to report these data to the Washington State Department of Health.
Our region's response in support of the LTCFs has included major health systems, the NWHRN and PHSKC. Health systems and PHSKC have developed strike teams that provide on-site support for infection prevention, triage, containment, testing, and clinical management of patients not requiring hospitalization. Their work includes conservation guidelines for PPE, training for testing of residents and staff, and protocols for increased surveillance and outbreak management. To support these efforts, PHSKC facilitates weekly calls between agencies and statewide webinars are conducted in conjunction with skilled nursing facility associations in the state. This provides a forum for local experts to educate, train, and provide real-time situational awareness.
Proactive management of vulnerable populations
In addition to residents of skilled nursing facilities, the COVID-19 pandemic presents challenges for other vulnerable communities.
Minority, immigrant, and non-English language communities
Many diseases including COVID-19, disproportionately impact those who are socially and economically disadvantaged.8 Data from US health departments reveal a disturbing, disproportionate impact of COVID-19 on racial and ethnic minorities, including Latinos and Black Americans.9 Preliminary analyses within the UW Medicine system comparing COVID-19 rates across race, ethnicity, and language demonstrate higher positive results among tests performed for COVID-19 among racial/ethnic minorities and populations with limited English proficiency. PHSKC surveillance data mirror these findings. There are likely multiple factors responsible for these findings, including lack of culturally relevant messaging and education, living in multigenerational households, and more likely to work in essential jobs resulting in inability to physically distance. PHSKC has worked to engage racially and linguistically diverse communities and has convened 9 taskforces and a community advisory group to collaborate across sectors and provide tools and resources to support physical distancing and reduce the risk of disease transmission.
People living homeless
Seattle has the third largest homeless population of any large city in the US, with a recent estimate of more than 11,000 people experiencing homelessness in King County.10 This population experiences a high rate of comorbid physical and mental health conditions. As such, shelters and other congregate settings must consider opportunities for physical distancing and prevention in settings that are normally crowded.11 , 12 To address this, King County has rapidly added shelter locations by using empty public spaces, some of which were closed because of the pandemic. The result was substantial decompression of existing shelter spaces and greater physical distancing.
Individuals living in tents and recreational vehicles can be considered differently than those living in shelters when it comes to isolation and quarantine (I&Q). In cases where a person has COVID-19 and is amenable to outpatient treatment, self-isolation might be attainable; however, with the closure of most public spaces, resources for hygiene are limited. Strategies include opening public restrooms in parks and deploying hand-washing stations.
In King County, people living homeless have been designated a priority population for COVID-19 testing. Discharging patients to a congregate setting without appropriate testing can lead to a rapid outbreak. Developing a robust system for I&Q is critical. This requires a close relationship and open communication with community partners. PHSKC has developed a number of locations and a call center to facilitate access to I&Q services.
Jail and prison populations
During outbreaks, jails and prisons must work quickly to establish I&Q units and consider methods to decrease inmate population density. Jail and prison leaders need to work with arresting agencies and correctional partners to decrease arrests and provide physical distancing within facilities. This can include work with courts and judges to pursue alternatives to secure detention.13, 14, 15
Jails also face challenges pertaining to the release of inmates. Because release from jail is a criminal justice and not a healthcare process, there is no mandatory health evaluation at release. Release from jail can occur any time of day or night, making the release of individuals with pending test results problematic. The King County jail has used an I&Q call center to obtain housing for individuals released and unable to self-isolate.
Effective physical distancing in the community
It has become evident worldwide that effective physical distancing at the community level can result in substantial reductions in disease transmission.16 The Seattle Mayor, King County Executive and Health Officer, and the Governor of WA have been proactive in enacting city, county, and statewide measures to achieve this goal. A timeline of the implementation is shown in Figure 1. Before the governor's statewide policies, physical distancing in King County had already begun, including the closure of the UW campus and other schools and work-from-home policies by large technology employers. As a result, effective physical distancing was established early in this region's outbreak.
A recent analysis of mobility data by Unacast found that between February 26 and April 14, King County had seen a > 70% reduction in nonessential visits and a 40% to 55% reduction in average mobility.17 An analysis of cell phone mobility reported in the New York Times revealed a > 60% reduction in mobility across western Washington.18 Automobile traffic in the Seattle area has also seen substantial reductions. Continued emphasis on physical distancing will be critical in preventing a resurgence of disease activity.19
Discussion
As Washington state and the nation contemplate the next phase of our pandemic response, many questions remain unanswered. We still do not know the true burden of infection, the level or duration of immunity post infection, or the extent of immunity in the community. Supply chains remain fragile and inconsistent, leading to the need for continuous reassessment of new PPE and COVID-19 sample collection capacity. Due to the work of the UW Virology laboratory, western Washington state has achieved good access to testing, but needs to continue to scale and maintain an adequate supply chain to ensure widespread testing availability and access for vulnerable populations in congregate settings. Ongoing work is needed to ensure comprehensive COVID-19 preparedness and response capacity in LTCFs.
The aggressive physical distancing practices put into place were aimed at reducing the incidence of new infections so that hospitals, emergency departments, and clinics could provide care in a safe and effective way. This has been successful, and this time has allowed us to transform the way care is delivered. Surge capacity was rapidly built, clinic visits moved to telehealth, and nonurgent care for many has been delayed, especially for those awaiting surgical procedures. How long many of these changes will continue remains unknown, but it is clear that healthcare systems can change rapidly when needed.
When the number of new cases in Washington state declines sufficiently and relaxing distancing measures and back-to-work policies are considered, it will be critical to have widespread access to COVID-19 testing, healthcare system capacity to manage a future surge in patients, adequate supplies of PPE, and robust public health capacity to conduct rapid case and contact tracing and effective isolation and quarantine of ill and exposed persons. The vast majority of the population remains susceptible, making a resurgence likely if these conditions are not adequately met.
Conclusions
The 6 key themes identified in this report provide a road map for navigating future outbreaks. A strength of this report is that the lessons learned were identified by a multidisciplinary group of experts on the front lines of the healthcare disaster response. Limitations include the lack of literature available to guide these recommendations and uncertainty regarding the long-term trajectory for this disease. Although we believe these recommendations will be applicable in communities across the US, they might not all be generalizable to healthcare settings with more limited resources. It is our hope that the key factors and recommendations identified in this report will help other states and nations in supporting their healthcare system disaster response.
Key recommendations
-
1.
A robust healthcare coalition with engagement of stakeholders and active regional disaster preparedness establishes relationships that facilitate communication and rapid response to a crisis in the healthcare system.
-
2.
Regional medical operations centers are vital for ensuring early identification of outbreaks, coordination of regional care, and ensuring healthcare assets are level-loaded.
-
3.
Establishing lines of communication and sharing of data with local public health, healthcare coalitions, healthcare systems, and EMS are essential for optimal coordination of regional assets and identification of disease clusters.
-
4.
State-level adoption of a data platform that tracks (at a minimum) bed capacity, staffing impacts, and equipment (PPE and ventilators) is essential.
-
5.
Early preparation is key for laboratories with the capability of establishing their own tests for emerging pathogens; at a minimum, obtaining primers and probes early can save valuable time.
-
6.
Collaboration between academic, state, county, and public health laboratory resources is critical for initiating and scaling clinical pathogen testing.
-
7.
Academic laboratories capable of rapidly developing their own tests are a valuable resource for the US healthcare system and should be encouraged to participate in the early stages of an emerging pandemic.
-
8.
A centralized, local coordination center to aid LTCFs and congregate living environments should be established to identify distressed facilities and coordinate resources, education, and training.
-
9.
Public health, local healthcare systems, and coalitions should coordinate to identify strategies that support local LTCFs in times of disaster by providing support, consultation, and resources.
-
10.
Public health, local healthcare systems, and coalitions must make targeted efforts to reach out and provide resources for vulnerable populations, including non-English-speaking residents, homeless residents, and jail inmates. These include plans for surveillance and testing, resources to support physical distancing, and safe isolation and quarantine.
-
11.
When rates of COVID-19 transmission increase, community-wide physical distancing is necessary to decrease the number of ill people and prevent the healthcare system from being overwhelmed.
Appendix
Members of the Western WA COVID-19 Expert Panel: James Lewis, MD, Public Health, Seattle & King County, Seattle, WA; Jeffrey S Duchin, MD, Public Health, Seattle & King County, Seattle, WA; Keith R Jerome, MD, PhD, Virology Division, Department of Laboratory Medicine, University of Washington, Seattle, WA, Vaccine and Infectious Disease Division, Fred Hutchinson Cancer Research Center, Seattle, WA; Geoffrey S Baird, MD, PhD, Clinical Laboratories, Department of Laboratory Medicine, University of Washington, Seattle, WA; Susan A Stern, MD, Department of Emergency Medicine, University of Washington, Seattle, WA; Timothy H Dellit, MD, Division of Allergy & Infectious Diseases Department of Medicine, University of Washington Seattle, WA; Louise Simpson, MHA, Post-Acute Care, UW Medicine, Seattle, WA; Onora Lien, MA, Northwest Healthcare Response Network, Tukwilla, WA; Nancy K Sugg, MD, Division of General Internal Medicine, Department of Medicine, University of Washington, Seattle, WA; Meagan Kay, DVM, Public Health, Seattle & King County, Seattle, WA; Benjamin Sanders, MD, MPH, Public Health, Seattle & King County, Seattle, WA; Margaret D Lukoff, MD, Public Health, Seattle & King County, Seattle, WA; Sabine von Preyss-Friedman, MD, Division of Gerontology and Geriatric Medicine, Department of Medicine, University of Washington, Seattle, WA; Matias Valenzuela, PhD, Public Health, Seattle & King County, Seattle, WA; Chloe Bryson-Cahn, MD, Division of Allergy & Infectious Diseases Department of Medicine, University of Washington Seattle, WA; Vanessa A Makarewicz, MN; Hanh Pan, MHA, Post-Acute Care, UW Medicine, Seattle, WA.
Author Contributions
Study conception and design: Mitchell, Bulger, Lynch
Acquisition of data: Mitchell, Bulger, Duber, Greninger, Ong, Morris, Chew
Analysis and acquisition of data: Mitchell, Bulger, Duber, Greninger, Ong, Morris, Chew, Haffner, Sakada, Lynch
Drafting of manuscript: Mitchell, Bulger, Duber, Greninger, Ong, Morris, Chew, Haffner, Sakata
Critical revision: Mitchell, Bulger, Duber, Greninger, Ong, Morris, Chew, Haffner, Sakata, Lynch
Footnotes
Members of the Western WA COVID-19 Expert Panel are listed in the Appendix.
Disclosure Information: Nothing to disclose.
Contributor Information
Eileen M. Bulger, Email: ebulger@uw.edu.
Western WA COVID-19 Expert Panel:
James Lewis, Jeffrey S. Duchin, Keith R. Jerome, Geoffrey S. Baird, Susan A. Stern, Timothy H. Dellit, Louise Simpson, Onora Lien, Nancy K. Sugg, Meagan Kay, Benjamin Sanders, Margaret D. Lukoff, Sabine von Preyss-Friedman, Matias Valenzuela, Chloe Bryson-Cahn, and Hanh Pan
Appendix
eAppendix: Panel of 26 experts selected based on their experience and key roles in the response to the COVID-19 outbreak in western Washington
Steering Committee Members
Steven H Mitchell, MD, Medical Director, Western Washington COVID-19 Coordination Center; Medical Director, Emergency Department, Harborview Medical Center; Department of Emergency Medicine, University of Washington, Seattle, WA. Eileen M Bulger, MD, FACS, Chief of Trauma, Harborview Medical Center, Department of Surgery, University of Washington, Seattle, WA. John B Lynch, MD, MPH, Medical Director, Infection Prevention & Control, Harborview Medical Center; Division of Allergy & Infectious Diseases, Department of Medicine, University of Washington Seattle, WA
Expert Panel
Herbert C Duber, MD, MPH, Section Chief, Population Health, Department of Emergency Medicine, University of Washington, Seattle, WA; Institute for Health Metrics and Evaluation, University of Washington, Seattle, WA. Alexander L Greninger, MD, PhD, MS, MPhil, Assistant Director, Clinical Virology Lab, UW Medicine, Virology Division, Department of Laboratory Medicine, University of Washington, Seattle, WA. Thuan D Ong, MD, MPH, Section Chief, Post-Acute Care Service, UW Medicine, Division of Gerontology and Geriatric Medicine, Department of Medicine, University of Washington, Seattle, WA. Stephen C Morris, MD, MPH, Acting Medical Staff Supervisor, Incident Command COVID-19 Response, Department of Emergency Medicine, University of Washington, Seattle, WA. Lisa D Chew, MD, MPH, Associate Medical Director, Ambulatory Care, Harborview Medical Center, Division of General Internal Medicine, Department of Medicine, University of Washington, Seattle, WA. Vicki L Sakata, MD, Senior Medical Advisor, Northwest Healthcare Response Network, Tukwilla, WA. James Lewis, MD, COVID-19 Acute Healthcare System Support Lead, Public Health, Seattle & King County, Seattle, WA. Jeffrey S Duchin, MD, Health Officer and Chief, Communicable Disease Epidemiology & Immunization Section, Public Health, Seattle and King County, Seattle, WA. Keith R Jerome, MD, PhD, Head, Virology Division, Department of Laboratory Medicine, University of Washington, Seattle, WA; Member, Vaccine and Infectious Disease Division, Fred Hutchinson Cancer Research Center, Seattle, WA. Geoffrey S Baird, MD, PhD, Interim Chair, Department of Laboratory Medicine, University of Washington, Seattle, WA. Susan A Stern, MD, Chair, Department of Emergency Medicine, University of Washington, Seattle, WA. Timothy H Dellit, MD, Chief Medical Officer, UW Medicine, Division of Allergy & Infectious Diseases, Department of Medicine, University of Washington, Seattle, WA. Louise Simpson, MHA, Administrator, UW Medicine Post-Acute Care, Seattle, WA. Onora Lien, MA, Executive Director, Northwest Healthcare Response Network, Tukwila, WA. Nancy K Sugg, MD, Medical Director, Pioneer Square Clinic and Downtown Homeless Programs, Harborview Medical Center, Department of Medicine, University of Washington, Seattle, WA. Meagan Kay, DVM, Regional Health Administrator, Public Health Seattle King County, Seattle, WA. Benjamin Sanders, MD, MPH, Medical Director, Jail Health Services Division, Public Health-Seattle & King County, Seattle, WA. Margaret D Lukoff, MD, Communicable Disease Epidemiology and Immunization Section, Public Health-Seattle & King County, Seattle, WA. Sabine von Preyss-Friedman, MD, Post-Acute Care Service, Division of Gerontology & Geriatric Medicine, Department of Medicine, University of Washington, Seattle, WA. Matías Valenzuela, PhD, Director, Office of Equity and Social Justice, Public Health - Seattle & King County, Seattle, WA. Chloe Bryson-Cahn, MD, Associate Medical Director, Infection Prevention & Control, Harborview Medical Center, Division of Allergy & Infectious Diseases, Department of Medicine, University of Washington, Seattle, WA. Vanessa A Makarewicz, MN, RN, Manager, Infection Prevention & Control Harborview Medical Center, Seattle, WA. Hanh Pan, MHA, Program Director, Post-Acute Care UW Medicine, Seattle, WA.
References
- 1.McMichael TM, Currie DW, Clark S et al. Epidemiology of covid-19 in a long-term care facility in King County, Washington. N Engl J Med 382:2005–2011. [DOI] [PMC free article] [PubMed]
- 2.COVID-19 estimate downloads Institute for Health Metrics and Evaluation. http://www.healthdata.org/covid/data-downloads Available at:
- 3.Arentz M., Yim E., Klaff L. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA. 2020;323:1612–1614. doi: 10.1001/jama.2020.4326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stewart R.M., Bulger E.M., Epley E., Mitchell S.H. How to set up a regional medical operations center to manage the COVID-19 pandemic. http://preview.acs.siteworx.com/covid-19/clinical-guidance/rmoc-setup Available at:
- 5.Establishing medical operations coordination cells (MOCCs) for COVID-19 Assistant Secretary for Preparedness and Response TRACIE. https://files.asprtracie.hhs.gov/documents/aspr-tracie-mocc-webinar--4-24-20-final-slides.pdf Available at:
- 6.McMichael T.M., Clark S., Pogosjans S. COVID-19 in a long-term care facility—King County, Washington, February 27-March 9, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:339–342. doi: 10.15585/mmwr.mm6912e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Introducing SCAN: The Greater Seattle Coronavirus Assessment Network Public Health Insider. https://publichealthinsider.com/2020/03/23/introducing-scan-the-greater-seattle-coronavirus-assessment-network/ Available at:
- 8.Laurencin C.T., McClinton A. The COVID-19 pandemic: a call to action to identify and address racial and ethnic disparities. J Racial Ethn Health Disparities. 2020;7:398–402. doi: 10.1007/s40615-020-00756-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yancy C.W. COVID-19 and African Americans. JAMA. 2020 Apr 15 doi: 10.1001/jama.2020.6548. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 10.Seattle/King County point-in-time count of persons experiencing homelessness 2019 Applied Survey Research. http://allhomekc.org/wp-content/uploads/2019/09/KING-9.5-v2.pdf Available at:
- 11.Farrell A, Gonzales E, Self JL, et al. COVID-19 outbreak among three affiliated homeless service sites—King County, Washington, 2020. MMWR Morb Mortal Wkly Rep 69:523–526. [DOI] [PMC free article] [PubMed]
- 12.Mosites E., Parker E.M., Clarke K.E. Assessment of SARS-CoV-2 infection prevalence in homeless shelters — Four U.S. Cities, March 27–April 15, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:521–522. doi: 10.15585/mmwr.mm6917e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Akiyama M.F., Spaulding A.C., Rich J.D. Flattening the curve for incarcerated populations—COVID-19 in jails and prisons. N Engl J Med. 2020;382:2075–2077. doi: 10.1056/NEJMp2005687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Simpson P.L., Butler T.G. Covid-19, prison crowding, and release policies. BMJ. 2020;369:m1551. doi: 10.1136/bmj.m1551. [DOI] [PubMed] [Google Scholar]
- 15.Kinner S.A., Young J.T., Snow K. Prisons and custodial settings are part of a comprehensive response to COVID-19. Lancet Public Health. 2020;5:e188–e189. doi: 10.1016/S2468-2667(20)30058-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thakkar N., Burstein R., Hu H. Social distancing and mobility reductions have reduced COVID-19 transmission in King County, WA. Institute for Disease Modeling, Bellevue, WA. https://covid.idmod.org/data/Social_distancing_mobility_reductions_reduced_COVID_Seattle.pdf Available at:
- 17.Unacast Social Distancing Scoreboard. https://www.unacast.com/covid19/social-distancing-scoreboard Available at:
- 18.Thompson S.A., Serkez Y., Kelley L. How has your state reacted to social distancing. New York Times. https://www.nytimes.com/interactive/2020/03/23/opinion/coronavirus-economy-recession.html Available at:
- 19.Thakkar N., Burstein R., Klein D. Physical distancing is working and still needed to prevent COVID-19 resurgence in King, Snohomish, and Pierce counties. Institute for Disease Modeling, Bellevue, Washington. https://covid.idmod.org/data/Physical_distancing_working_and_still_needed_to_prevent_COVID-19_resurgence.pdf Available at: