ABSTRACT
Introduction
Differentiation between sepsis and systemic inflammation response syndrome (SIRS) remains a diagnostic challenge for clinicians as both may have similar clinical presentation. A quick and accurate diagnostic tool that can discriminate between these two conditions would aid in appropriate therapeutic decision-making. This prospective study was conducted to evaluate the diagnostic and prognostic utility of soluble urokinase-type plasminogen activator receptor (suPAR) and procalcitonin (PCT) in sepsis and SIRS patients.
Materials and methods
Eighty-eight patients were enrolled, of which 29 were SIRS and 59 were sepsis patients. The levels of suPAR and PCT were measured on the day of admission (day 1), day 3, and day 7.
Results
The levels of suPAR and PCT were significantly higher (p = 0.05 and p < 0.001, respectively) in sepsis group as compared to the SIRS group. The soluble urokinase-type plasminogen activator receptor was a better diagnostic tool in predicting sepsis over PCT [area under curve (AUC) 0.89 vs 0.82] on day 1. The best cutoff for suPAR was 5.58 pg/mL [96% sensitivity and 90% negative predictive value (NPV)] and the best cut-off for PCT was 1.96 ng/mL (93.1% sensitivity and 80% NPV). However, PCT had better prognostic trends (p = 0.006) to identify nonsurvivors in sepsis group.
Conclusion
Our findings suggest that both suPAR and PCT can be used as potential test tools to differentiate between SIRS and sepsis. Procalcitonin showed significant prognostic trends to identify nonsurvivors. The soluble urokinase-type plasminogen activator receptor showed better diagnostic potential than PCT on day 1.
Clinical significance
Both suPAR and PCT can be used as surrogate biomarkers to distinguish sepsis from SIRS. Procalcitonin showing a significant prognostic trend to identify nonsurvivors can help the clinicians to take relevant clinical decisions. Also, the use of biomarkers like PCT and suPAR could reduce the inappropriate use of antibiotics in noninfective SIRS.
How to cite this article
Sharma A, Ray S, Mamidipalli R, Kakar A, Chugh P, Jain R, et al. A Comparative Study of the Diagnostic and Prognostic Utility of Soluble Urokinase-type Plasminogen Activator Receptor and Procalcitonin in Patients with Sepsis and Systemic Inflammation Response Syndrome. Indian J Crit Care Med 2020;24(4):245–251.
Keywords: Procalcitonin, Sepsis, Soluble urokinase-type plasminogen activator receptor, Systemic inflammation response syndrome
INTRODUCTION
During the last decade, there has been a worldwide increase in the incidence of sepsis.1,2 This has led to a twofold increase in hospitalization rate (11.6 to 24.0 per 10,000 population).3 Although in recent years management of sepsis has improved survival, the overall mortality is still rising as the number of sepsis cases has been increasing.4,5 According to the consensus definition of the American College of Chest Physicians (ACCP) and the Society of Critical Care Medicine (SCCM), sepsis is defined as a systemic inflammatory host response (SIRS) to infection and characterized by alterations in physiologic parameters such as temperature, heart rate, respiratory rate, mentation, etc.6 These changes in physiologic parameters are nonspecific in the clinical context and may manifest in many other non-infectious causes of SIRS such as trauma, burns, pancreatitis, etc. Recently, the Third International Consensus Definitions for Sepsis and Septic Shock (2017) has redefined sepsis as life-threatening organ dysfunction caused by a dysregulated host response to infection, as it has been now observed that the immune response in sepsis is more complex than just an inflammatory cytokine response.7 It has been observed that a subset of patients shows a predominant surge of anti-inflammatory cytokines but the initial clinical response is still guided by SIRS criteria.7
Differentiating between SIRS due to noninfectious causes and infection is a challenge, since both these conditions may have similar clinical features.8,9 The gold standard is a positive bacterial culture, which has a sensitivity of less than 50%.10 Hence, there is a need to identify biomarkers that not only are more sensitive and specific but can also be performed quickly and cost-effectively. Review of published literature suggests procalcitonin (PCT) as a good biomarker which can differentiate patients with SIRS and sepsis and has been evaluated extensively.11–13 Procalcitonin is a precursor of the hormone calcitonin and is produced by parafollicular cells of thyroid and neuroendocrine cells of lungs and intestine. The levels of PCT rises in response to an inflammatory stimulus, especially of bacterial origin.12
A new biomarker, soluble urokinase-type plasminogen activator receptor (suPAR), demonstrated to have the ability to predict disease severity in bacteremia, ventilator-associated pneumonia, SIRS, and sepsis.14–16 The urokinase-type plasminogen activator receptor (uPAR) is a three-domain glycosylated protein (D1–D3) which binds to glycosylphosphatidylinositol (GPI) anchor on cell surface to release its soluble form, i.e., suPAR.17 Immunologically active cells, including neutrophils, lymphocytes, monocytes, and macrophages, all have roles in the pathogenesis of inflammation expressing uPAR.17 The soluble urokinase-type plasminogen activator receptor has chemotactic properties and is present in most biological fluids such as serum, plasma, and urine.14 Thus, systemic suPAR levels have been suggested as a novel prognostic marker of inflammation.18,19 Multiple studies have documented the clinical relevance of systemic suPAR levels to predict outcome in patients with SIRS, sepsis, and septic shock.14
The aim of the present study was to determine the diagnostic and prognostic utility of suPAR in comparison to PCT in adult patients diagnosed with SIRS and sepsis admitted to the intensive care unit (ICU) at Sir Ganga Ram Hospital, New Delhi. This was a single-center study conducted over a period of 2.6 years.
MATERIALS AND METHODS
The study protocol was approved by institutional ethics committee (EC/02/15/788); and the prospective, observational, single-center study was conducted at Sir Ganga Ram Hospital, New Delhi (India), over a period of 2.6 years (September 2015 to March 2018).
Patients aged >18 years suspected of having SIRS or sepsis (ACCP/SCCM definition) were enrolled in this study.6
Patients transferred from other ICUs, patients treated with antibiotics in the preceding 3 months; patients having any malignancy, immunocompromised patients, those with conditions that could prove lethal in the next 24 hours, and postoperative patients were not included in the study. Patients suffering from tropical diseases such as malaria, dengue, leptospira, and rickettsia or having bilateral pneumonia were also excluded.
Patient demographics, principal diagnosis, and related clinical parameters were recorded at the time of inclusion in the study. Acute physiology and chronic health evaluation score (APACHE II) at 24 hours were recorded for all the enrolled patients. Patient's sample was collected at three time points, i.e., day 1, day 3, and day 7. Patients were followed up for 30 days to document survival/mortality.
Sample Collection and Processing
Blood samples for culture were taken in both aerobic and anaerobic BacT/Alert bottles and performed by BacT/Alert method (BioMerieux, Marcy l'Etiole, France) on day 1 of admission to the ICU. Blood sample of 1 mL was collected in non-EDTA/plain vial for biomarker evaluation at three time points as described above. Samples were centrifuged at 2,000g for 10 minutes. After centrifugation, the serum samples were stored at −80°C until analysis. The soluble urokinase-type plasminogen activator receptor was measured using commercial solid-phase enzyme-linked immunosorbent assay (suPAR; ViroGates, Denmark). For PCT levels, signals emitted from an immune complex with time delay is measured using time-resolved amplified cryptate emission technology (Kryptor PCT; BRAHMS, Henningsdorf, Germany).
Classification of Patient Groups
Based on the criteria of SIRS and sepsis, patients were classified as:
Group I (noninfectious SIRS): Patients with two or more signs of SIRS without any evidence of infection and diagnosed with recent onset of pancreatitis and trauma (within 24 hours) were included in this group.
Group II (sepsis group): Patients with two or more signs of SIRS and clinical suspicion of infection or culture-proven infections.
The diagnosis of bacterial infection in culture-negative patients was done based on the findings of a clinical focus of infection.7
Intra-abdominal infection was diagnosed in case of exudative ascitic tap with increased polymorphonuclear cell count.
Bacterial pneumonia was confirmed by X-ray showing lobar infiltrate.
Urosepsis was suspected with signs of urinary tract infection and with a raised leukocyte count in the urine (>10 pus cells/high-power field) and signs of pyelonephritis by ultrasonography.
Cellulitis was diagnosed by the skin signs, i.e., lesions.
Puerperal sepsis was suspected in peripartum patients with signs of pelvic pain and abnormal or foul smelling vaginal discharge (presence of pus).7
Statistical Analysis
Statistical Package for the Social Science (SPSS) version 17.0 was used to perform statistical testing. Continuous variables were presented as mean ± standard deviation (SD) or median (interquartile range, IQR) for nonnormally distributed data. Student's t test was done to compare normally distributed continuous variables between the groups. Mann–Whitney U test was performed for nonnormal distribution continuous variables. For categorical variables, Chi-square test or Fisher's exact test was used, and the results were expressed as frequencies and percentages as appropriate. A receiver–operating characteristic (ROC) analysis was calculated to determine the optimal cutoff value for suPAR and PCT. To analyze the diagnostic accuracy of the markers, AUC, sensitivity, specificity, positive predictive value (PPV), and NPV were calculated. For all statistical tests, a p value of <0.05 is indicative of significant difference.
RESULTS
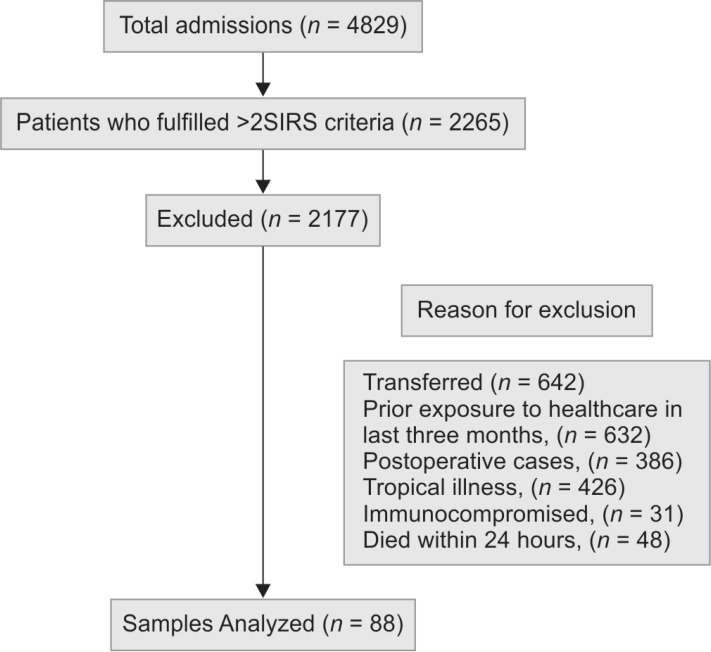
The study was conducted in 88 patients prospectively. As explained in the methodology, enrolled patients were classified into two groups, namely, noninfectious SIRS (n = 29) and sepsis (n = 59) (Flowchart 1). Of the total patients enrolled, nearly 33% patients were noninfectious SIRS and 67% were sepsis. The demographic characteristics of the patients enrolled are shown in Table 1.
Flowchart 1.
Patients enrolled in the study
Table 1.
Demographics and outcome of the study patient groups
| Characteristics | Group I (SIRS) | Group II (Sepsis) | p value |
|---|---|---|---|
| No. of patients | 29 | 59 | – |
| Sex, M/F | 20/9 | 40/19 | – |
| Mean age (years/min–max) | 37 (20–64) | 58 (38–84) | NS |
| Mortality, n (%) | 4 (13.8%) | 24 (40.7%) | 0.001 |
| APACHE II, mean (range) | 15.8 (5–48) | 25.3 (9–47) | <0.001 |
Characteristics of Patients Enrolled
No significant age or gender difference was observed between the study groups (Table 1). Mean APACHE II score was significantly (p < 0.001) higher in sepsis group (25.3) as compared to SIRS group (15.8). Also, the mortality in sepsis group (40.7%) was significantly higher as compared to SIRS group (13.8%; p = 0.001).
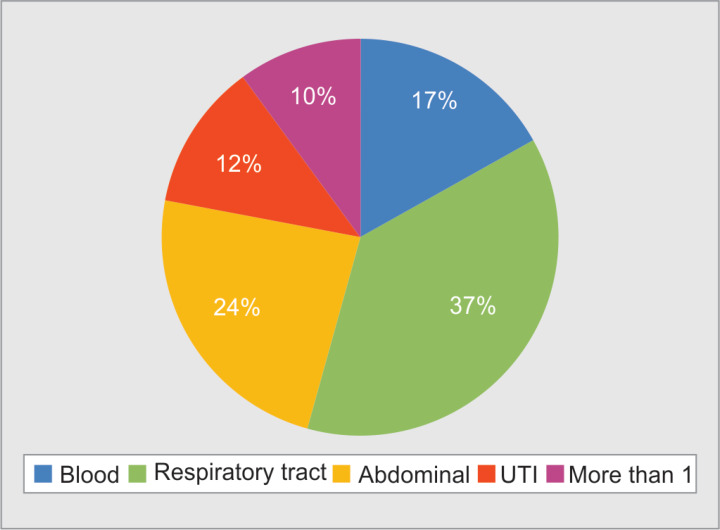
Source of Infection
The major sources of infection were respiratory tract (37.3%), abdominal (23.7%), bloodstream (17.9%), and urinary tract (11.9%) (Fig. 1). Ten percent of the patients had more than one source of infection.
Fig. 1.
Median values of soluble urokinase-type plasminogen activator receptor and procalcitonin
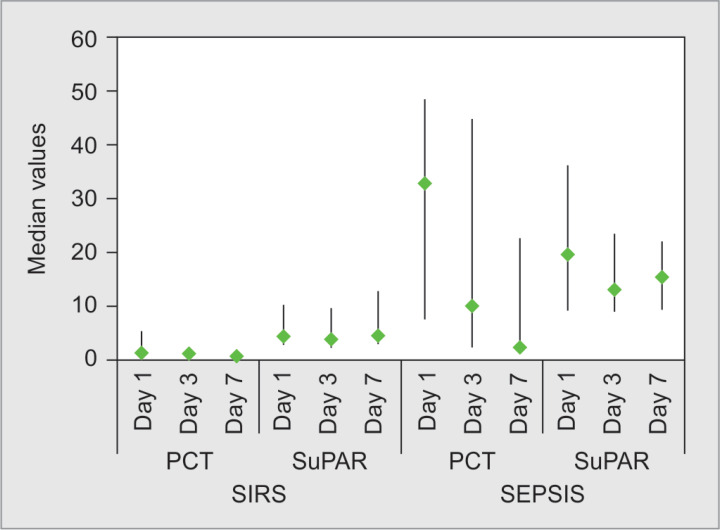
Serum Levels of suPAR and PCT in Study Groups
The levels of suPAR and PCT were measured in all the enrolled patients on the day of admission (day 1), day 3, and day 7. The median PCT value on day 1 was significantly higher (p < 0.001) in the sepsis group (32.78 ng/mL) as compared to SIRS group (1.17 ng/mL). Similarly, day 1 median suPAR values were significantly higher in sepsis group (19.54 pg/mL) as compared to SIRS (4.2 pg/mL) (p = 0.05) (Fig. 2). Thus, both PCT and suPAR were able to distinguish between sepsis and SIRS on day 1.
Fig. 2.
Receiver–operating characteristic curve for soluble urokinase-type plasminogen activator receptor and procalcitonin to differentiate sepsis from systemic inflammation response syndrome
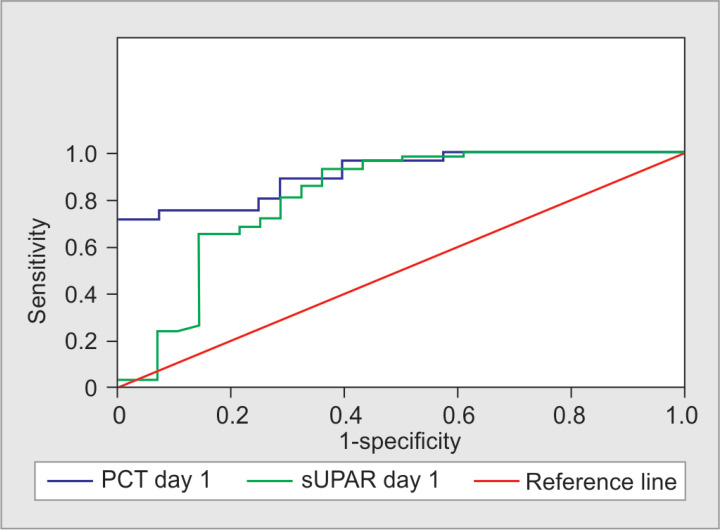
Discriminative Performance of suPAR and PCT to Diagnose Sepsis
The ROC curve analysis was performed for suPAR and PCT for prediction of sepsis (Fig. 3). The AUC for suPAR (day 1) and PCT (day 1) were 0.89 and 0.82, respectively. For suPAR, the optimal cutoff point was 5.58 with a sensitivity of 96%, NPV of 90%, and accuracy of 82.05%. The best cutoff for PCT was 1.96 with a sensitivity of 93.1%, NPV of 73.4%, and accuracy of 79.4%. Both the markers were sensitive enough to predict sepsis; however, suPAR was statistically a more accurate marker for the diagnosis of sepsis. Similar trends were observed in the levels of suPAR and PCT collected on day 3 (Table 2). On day 3, suPAR was statistically slightly better at differentiating sepsis from SIRS (Table 2).
Fig. 3.
Source of infection in the enrolled patients
Table 2.
Diagnostic performance of soluble urokinase-type plasminogen activator receptor and procalcitonin in differentiating sepsis and systemic inflammation response syndrome
| Variable | Cutoff | AUC | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Accuracy (%) |
|---|---|---|---|---|---|---|---|
| PCT @ day 1 | 1.96 | 0.82 | 93.1 | 53.33 | 79.41 | 80.0 | 79.55 |
| suPAR @ day 1 | 5.58 | 0.89 | 96 | 60.00 | 79.31 | 90.00 | 82.05 |
Prognostic Values of suPAR and PCT to Predict Mortality in SIRS
On analyzing the suPAR values, we observed no difference in median values from day 1 to day 7 in both survivors (p = 0.276) and nonsurvivors (p = 0.607) (Table 3). A significant decrease in the median PCT levels was observed in survivors (p = 0.001) from day 1 (1.18 ng/mL, IQR = 0.2 to 4.46) to day 7 (0.5 ng/mL; IQR = 0.2 to 0.68) and a sharp increase (p = 0.05) in the median PCT values from day 1 (3.11 ng/mL (IQR = 0.31 to 5.99) to day 7 (36.86 ng/mL; IQR = 3.45 to 70.07) in nonsurvivors of SIRS group (p = 0.05). The trends of median values for both suPAR and PCT suggest that PCT had a better prognostic value for predicting nonsurvivors in SIRS group. On day 7, a significant increase in the median suPAR (p = 0.009) and PCT (p = 0.003) levels was observed in nonsurvivors as compared to survivors.
Table 3.
Prognostic values of soluble urokinase-type plasminogen activator receptor and procalcitonin in systemic inflammation response syndrome group
| SIRS | Survivors | Nonsurvivors | p value |
|---|---|---|---|
| Median (IQR) | Median (IQR) | ||
| PCT D1 | 1.18 (0.2–4.46) | 3.11 (0.31–5.99) | 0.793 |
| PCT D3 | 0.80 (0.40–3.02) | 1.21 (0.09–2.38) | 0.431 |
| PCT D7 | 0.5 (0.2–0.68) | 36.86 (3.45–70.07) | 0.003* |
| p value | <0.001* | 0.050 | |
| suPAR D1 | 4.20 (2.69–9.56) | 19.20 (2.48–36.15) | 0.470 |
| suPAR D3 | 3.73 (2.28–8.89) | 12.55 (2.42–21.22) | 0.280 |
| suPAR D7 | 4.21 (3.11–8.70) | 24.83 (15.65–25.90) | 0.009* |
| p value | 0.276 | 0.607 |
Highly significant
Prognostic Values of suPAR and PCT to Predict Mortality in Sepsis
In the case of sepsis, no significant difference (p = 0.45) was observed in the median suPAR values from day 1 (12.2 pg/mL; IQR = 7.12 to 23.03) to day 7 (13.19 pg/mL, IQR = 7.39 to 18.2) among survivors, whereas a decrease was observed in the median values of suPAR from 28.66 pg/mL (IQR = 14.84 to 38.55) on day 1 to 19.13 pg/mL (IQR = 10.19 to 28.83) on day 7 in nonsurvivors, though it did not reach statistical significance (Table 4). It was observed that the suPAR values were significantly higher at all three time points (day 1, p = 0.003; day 3, p < 0.001; and day 7, p = 0.022) in nonsurvivors as compared to survivors.
Table 4.
Prognostic values of soluble urokinase-type plasminogen activator receptor and procalcitonin in sepsis group
| Sepsis | Survivors | Nonsurvivors | p value |
|---|---|---|---|
| Median (IQR) | Median (IQR) | ||
| PCT D1 | 22.93 (7.11–47.56) | 36.24 (9.48–104.64) | 0.210 |
| PCT D3 | 6.24 (2.23–20.96) | 33.45 (4.03–109.88) | 0.004** |
| PCT D7 | 1.20 (0.65–3.68) | 28.04 (12.04–53.45) | <0.001** |
| p value | <0.001** | 0.006** | |
| suPAR D1 | 12.20 (7.12–23.03) | 28.66 (14.84–38.55) | 0.003** |
| suPAR D3 | 9.55 (6.98–15.38) | 22.08 (13.24–21.94) | <0.001** |
| suPAR D7 | 13.19 (7.39–18.20) | 19.13 (10.19–28.83) | 0.022* |
| p value | 0.452 | 0.104 |
Highly significant
Similar trends in the median PCT values were observed in survivors and nonsurvivors. The median PCT levels decreased significantly from day 1 to day 7 in both survivors (p < 0.001) and nonsurvivors (p = 0.006), but the PCT levels remained significantly higher in nonsurvivors as compared to survivors on day 3 (p = 0.004) and day 7 (<0.001).
Median values of suPAR at all the time points (day 1, day 3, and day 7) were significant in distinguishing the nonsurvivors from the survivors. The accuracy of suPAR at day 1 (p = 0.002), day 3 (p < 0.001), and day 7 (p = 0.008) was 73.7%, 69.6%, and 70.9%, respectively. The NPV of suPAR was 73.8%, 100%, and 75.7% on day 1, day 3, and day 7, respectively (Table 5).
Table 5.
Prognostic ability of soluble urokinase-type plasminogen activator receptor to distinguish between survivors and nonsurvivors in sepsis group
| Sepsis | AUC | suPAR Cut off | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Accuracy (%) | p value |
|---|---|---|---|---|---|---|---|---|
| Day 1 | 0.741 | 30.2 | 50.0 | 88.6 | 73.3 | 73.8 | 73.7 | 0.002 |
| Day 3 | 0.805 | 9.77 | 100.0 | 52.80 | 54.05 | 100.0 | 69.6 | <0.001 |
| Day 7 | 0.684 | 18.36 | 55.0 | 80.0 | 61.1 | 75.7 | 70.9 | 0.008 |
The median values of PCT on day 3 and day 7 were highly significant in identifying nonsurvivors in the sepsis groups. For PCT, a cutoff value of 16.93 ng/mL on day 3 (p = 0.001) had a specificity and NPV of 72.2% and 81.3%, respectively, to predict mortality. On day 7, at a cutoff value of 11.62 ng/mL, PCT (p < 0.001) had a specificity and NPV of 97.2% and 89.7%, respectively, to predict mortality (Table 6). Although there was a difference in the median values of PCT on day 1 to differentiate survivors from nonsurvivors among sepsis patients, it did not reach statistical significance.
Table 6.
Prognostic ability of procalcitonin to distinguish between survivors and nonsurvivors in sepsis group
| Sepsis | AUC | PCT cutoff | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Accuracy (%) | p value |
|---|---|---|---|---|---|---|---|---|
| Day 1 | 0.597 | 23.25 | 70.8 | 52.8 | 50.0 | 73.1 | 60.0 | 0.071 |
| Day 3 | 0.728 | 16.93 | 72.7 | 72.20 | 61.54 | 81.3 | 72.4 | 0.001 |
| Day 7 | 0.895 | 11.62 | 81.8 | 97.2 | 94.7 | 89.7 | 91.4 | <0.001 |
DISCUSSION
Sepsis is a life-threatening clinical syndrome characterized by a dysregulated host response to infections with nonspecific clinical symptoms.5 The dysregulated inflammatory responses involve the activation of proinflammatory and anti-inflammatory cellular and humoral responses affecting organ function in sepsis. Early diagnosis of sepsis is important to rapidly implement appropriate therapy, which is directly associated with clinical outcomes.
The gold standard to diagnose infection is bacterial culture, which is positive in less than 50% of cases of sepsis (8) and it takes 24 to 48 hours. Despite adequate improvements in diagnostic techniques, it is still a challenge to differentiate between sepsis and SIRS early. These patients are primarily diagnosed by clinical acumen based on very subjective criteria. Thus, identifying a marker that can differentiate between sepsis, particularly culture-negative sepsis, and noninfectious SIRS is the need of the hour. Early and better diagnostic and prognostic markers will aid the clinicians in taking appropriate clinical decisions. As evidence has shown, giving early antibiotics (within 1 hour) in sepsis patients improves outcome significantly.20 Recently, many new biomarkers such as PCT, suPAR, interleukin (IL)-27, macrophage migration inhibitory factor (MIF), and galectin-3 have been evaluated for their diagnostic and prognostic ability in management of sepsis either as independent diagnostic/prognostic biomarkers or as a combination of biomarkers.9,21–23
Procalcitonin is a peptide precursor of hormone calcitonin consisting of 116 amino acids (molecular weight, 13 kD).24 It is synthesized by the C-cells of thyroid gland and remains undetectable in healthy individuals. Assicot et al. were the first to report abnormally raised PCT levels in patients with bacterial infections.25 In healthy volunteers, high PCT levels were detected in plasma 2 to 3 hours after endotoxin injection. The half-life of PCT in serum is 25 to 30 hours.26
The suPAR is the soluble form of the uPAR, a three-domain receptor mainly expressed on immune cells, including neutrophils, activated T-cells, and macrophages.14 The levels of suPAR were found to be elevated in several pathological conditions such as sepsis, bacteremia, malaria, tuberculosis, HIV infection, central nervous system infections, etc.15–18 Published literature has acknowledged suPAR as a marker to predict sepsis; however, it is also known to be relatively nonspecific. Our study evaluates the diagnostic and prognostic ability of serum PCT and suPAR in identifying sepsis patients and their value in prognostication.
The APACHE II score is an indicator of severity of illness and the risk of mortality in critically ill patients. In the current study, we observed that APACHE II scores were significantly higher in sepsis (p < 0.001) group as compared with SIRS. The mortality rate was also significantly higher in the sepsis group. This was similar to the results of Phua et al. and Kumar et al. who reported higher mortality in sepsis patients as compared to noninfective SIRS.20,27
We observed a significant increase in both suPAR and PCT in the sepsis group. Several immune cells are activated in sepsis, thereby resulting in a highly inflammatory condition. These activated immune cells release both suPAR and PCT which is reflected in our study. Our study results were in agreement with those reported by Mölkänen et al.28 and Sehestedt et al.29
The ROC analysis between sepsis and SIRS patients demonstrated a slightly superior AUC for suPAR in diagnosing sepsis than PCT on day 1. The sensitivity of suPAR at an optimum cutoff value of 5.58 pg/mL was 96% with an NPV of 90%. For PCT at a cutoff value of 1.96 ng/mL, the sensitivity and NPV were comparatively lower (93% and 80%, respectively). Kofoed et al. and Sehestedt et al. found similar results, wherein suPAR showed higher sensitivity in patients with sepsis and SIRS.29,30
A clinical trial TRIAGE III was carried out to assess the prognostic value of suPAR. The trial did not find any significant correlation between increased level of suPAR and mortality.31 Our study correlates the declining trends in PCT (p < 0.001) with better prognostication than the trends in suPAR to predict survivors in SIRS (p = 0.276) and sepsis (p = 0.452).
Our data suggest suPAR to have a statistically better diagnostic ability in predicting sepsis over PCT. On the contrary, the PCT trend showed a better prognostic value to predict mortality in patients with sepsis and SIRS.
Hence, both suPAR and PCT can be used in addition to culture reports to improve outcome in sepsis by early initiation of antibiotics and resuscitation. On the contrary, both these biomarkers could reduce the inappropriate use of antibiotics in noninfective SIRS. Further, suPAR and PCT assays are simple to perform, provide quick results, and can be carried out in most modern healthcare establishments. The sensitivity and NPV of both suPAR and PCT suggest that they can be useful markers that can guide early, accurate, and rapid differentiation of sepsis from noninfective SIRS, much before the availability of culture reports. Further, a sequential analysis of PCT levels at various time points in sepsis can aid in understanding the severity and outcome of the disease.
The strength of our study was the stringent inclusion and exclusion criteria to enroll patients that clearly delineated the two groups under study. For sepsis, only those patients with fresh episodes having no history of previous hospital stay or antibiotic therapy in the last 3 months; and for SIRS, patients with trauma or pancreatitis in the last 24 hours were enrolled. The limitation of this study is that it is a single-center study without a very large number of patients. A multicenter study will enable validation of our findings.
CONCLUSION
Our findings suggest that both suPAR and PCT can be used as potential test tools to differentiate between SIRS and sepsis. Both suPAR and PCT can help in the clinical setting by accurately and sensitively differentiating sepsis from SIRS, thereby improving outcomes in sepsis by early initiation of antibiotics and resuscitation. It would also help in reducing inappropriate antibiotic use in noninfective SIRS. Their ability to predict disease progression would help the clinicians to prognosticate outcomes. Larger multicenter trials are required to corroborate our findings.
CLINICAL SIGNIFICANCES
Surrogate biomarkers such as suPAR and PCT may aid in better distinction of sepsis from SIRS. Our study showed PCT to have a significant prognostic trend to identify nonsurvivors. This can help clinicians to identify the patients at greater risk. Also, the use of biomarkers such as PCT and suPAR could reduce the inappropriate use of antibiotics in noninfective SIRS.
ACKNOWLEDGMENTS
We thank Mr Devinder Soni from ViroGates for providing us with the kits to perform suPAR. He had no role in planning, conducting and analyzing this study. We are grateful to Dr Seema Bhargava, Department of Biochemistry, Sir Ganga Ram Hospital, New Delhi, for helping us with the PCT results. A heartfelt thanks to the patients and the families of the enrolled patients for cooperating with the clinical and the research team.
Footnotes
Source of support: ViroGates
Conflict of interest: None
REFERENCES
- 1.Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United states from 1979 through 2000. N Engl J Med. 2003;348(16):1546–1554. doi: 10.1056/NEJMoa022139. DOI: [DOI] [PubMed] [Google Scholar]
- 2.Engel C, Brunkhorst FM, Bone HG, Brunkhorst R, Gerlach H, Grond S, et al. Epidemiology of sepsis in Germany: results from a national prospective multicenter study. Intensive Care Med. 2007;33(4):606–618. doi: 10.1007/s00134-006-0517-7. DOI: [DOI] [PubMed] [Google Scholar]
- 3.Dombrovskiy VY, Martin AA, Sunderram J, Paz HL. Rapid increase in hospitalization and mortality rates for severe sepsis in the United States: a trend analysis from 1993 to 2003. Crit Care Med. 2007;35(5):1244–1250. doi: 10.1097/01.CCM.0000261890.41311.E9. DOI: [DOI] [PubMed] [Google Scholar]
- 4.Hall MJ, Williams SN, DeFrances CJ, Golosinskiy A. Inpatient care for septicemia or sepsis: a challenge for patients and hospitals. NCHS Data Brief. 2011;(62):1–8. [PubMed] [Google Scholar]
- 5.Vincent JL, Rello J, Marshall J, Silva E, Anzueto A, Martin CD, et al. EPIC II group of investigators. International study of the prevalence and outcomes of infection in intensive care units. J Am Med Assoc. 2009;302(21):2323–2329. doi: 10.1001/jama.2009.1754. DOI: [DOI] [PubMed] [Google Scholar]
- 6.Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM consensus conference committee. American college of chest physicians/society of critical care medicine. Chest. 1992;101(6):1644–1655. doi: 10.1378/chest.101.6.1644. DOI: [DOI] [PubMed] [Google Scholar]
- 7.Anand D, Das S, Bhargava S, Srivastava LM, Garg A, Tyagi N, et al. Procalcitonin as a rapid diagnostic biomarker to differentiate between culture-negative bacterial sepsis and systemic inflammatory response syndrome: a prospective, observational, cohort study. J Crit Care. 2015;30(1):218.e7–12. doi: 10.1016/j.jcrc.2014.08.017. DOI: [DOI] [PubMed] [Google Scholar]
- 8.Høyer-Hansen G, Rønne E, Solberg H, Behrendt N, Ploug M, Lund LR, et al. Urokinase plasminogen activator cleaves its cell surface receptor releasing the ligand-binding domain. J Biol Chem. 1992;267(25):18224–18229. [PubMed] [Google Scholar]
- 9.Wilhelm OG, Wilhelm S, Escott GM, Lutz V, Magdolen V, Schmitt M, et al. Cellular glycosylphosphatidylinositol-specific phospholipase D regulates urokinase receptor shedding and cell surface expression. J Cell Physiol. 1999;180(2):225–235. doi: 10.1002/(SICI)1097-4652(199908)180:23.0.CO;2-2. DOI: [DOI] [PubMed] [Google Scholar]
- 10.Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). J Am Med Assoc. 2016;315(8):801–810. doi: 10.1001/jama.2016.0287. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tsalik EL, Jaggers LB, Glickman SW, Langley RJ, van Velkinburgh JC, Park LP, et al. Discriminative value of inflammatory biomarkers for suspected sepsis. J Emerg Med. 2012;43(1):97–106. doi: 10.1016/j.jemermed.2011.05.072. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liaudat S, Dayer E, Praz G, Bille J, Troillet N. Usefulness of procalcitonin serum level for the diagnosis of bacteremia. Eur J Clin Microbiol Infect Dis. 2001;20(8):524–527. doi: 10.1007/s100960100548. DOI: [DOI] [PubMed] [Google Scholar]
- 13.Chirouze C, Schuhmacher H, Rabaud C, Gil H, Khayat N, Estavoyer JM, et al. Low serum procalcitonin level accurately predicts the absence of bacteremia in adult patients with acute fever. Clin Infect Dis. 2002;35(2):156–161. doi: 10.1086/341023. DOI: [DOI] [PubMed] [Google Scholar]
- 14.Wittenhagen P, Kronborg G, Weis N, Nielsen H, Obel N, Pedersen SS, et al. The plasma level of soluble urokinase receptor is elevated in patients with streptococcus pneumoniae bacteraemia and predicts mortality. Clin Microbiol Infect. 2004;10(5):409–415. doi: 10.1111/j.1469-0691.2004.00850.x. DOI: [DOI] [PubMed] [Google Scholar]
- 15.Huttunen R, Syrjänen J, Vuento R, Hurme M, Huhtala H, Laine J, et al. Plasma level of soluble urokinase-type plasminogen activator receptor as a predictor of disease severity and case fatality in patients with bacteraemia: a prospective cohort study. J Intern Med. 2011;270(1):32–40. doi: 10.1111/j.1365-2796.2011.02363.x. DOI: [DOI] [PubMed] [Google Scholar]
- 16.Langkilde A, Hansen TW, Ladelund S, Linneberg A, Andersen O, Haugaard SB. Increased plasma soluble uPAR level is a risk marker of respiratory cancer in initially cancer-free individuals. Cancer Epidemiol Biomarkers Prev. 2011;20(4):609–618. doi: 10.1158/1055-9965.EPI-10-1009. DOI: [DOI] [PubMed] [Google Scholar]
- 17.Eugen-Olsen J, Gustafson P, Sidenius N, Fischer TK, Parner J, Aaby P, et al. The serum level of soluble urokinase receptor is elevated in tuberculosis patients and predicts mortality during treatment: a community study from guinea-Bissau. Int J Tuberc Lung Dis. 2002;6(8):686–692. [PubMed] [Google Scholar]
- 18.Savva A, Raftogiannis M, Baziaka F, Antonopoulou A, Koutaukas P, Tsaganos T, et al. Soluble urokinase plasminogen activator receptor (suPAR) for assessment of disease severity in ventilator-associated pneumonia and sepsis. J Infect. 2011;63(5):344–350. doi: 10.1016/j.jinf.2011.07.016. DOI: [DOI] [PubMed] [Google Scholar]
- 19.Koch A, Voigt S, Kruschinski C, Sanson E, Duckers H, Horn A, et al. Circulating soluble urokinase plasminogen activator receptor is stably elevated during the first week of treatment in the intensive care unit and predicts mortality in critically ill patients. Crit Care. 2011;15(1):R63. doi: 10.1186/cc10037. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, Sharma S, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006;34(6):1589–1596. doi: 10.1097/01.CCM.0000217961.75225.E9. DOI: [DOI] [PubMed] [Google Scholar]
- 21.Backes Y, van der Sluijs KF, Mackie DP, Tacke F, Koch A, Tenhunen JJ, et al. Usefulness of suPAR as a biological marker in patients with systemic inflammation or infection: a systematic review. Intensive Care Med. 2012;38(9):1418–1428. doi: 10.1007/s00134-012-2613-1. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sidenius N, Sier CF, Blasi F. Shedding and cleavage of the urokinase receptor (uPAR): identification andcharacterisation of uPAR fragments in vitro and in vivo. FEBS Lett. 2000;475(1):52–56. doi: 10.1016/s0014-5793(00)01624-0. DOI: [DOI] [PubMed] [Google Scholar]
- 23.Jevdjic J, Surbatovic M, Milosavljevic S, Rondovic G, Stanojevic I, Eric S, et al. Galectin-3 in critically ill patients with sepsis and/or trauma: a good predictor of outcome or not? Ser J Exp Clin Res. 2017 [Google Scholar]
- 24.Le Moullec JM, Jullienne A, Chenais J, Lasmoles F, Guliana JM, Milhaud G, et al. The complete sequence of human preprocalcitonin. FEBS Lett. 1984;167(1):93–97. doi: 10.1016/0014-5793(84)80839-x. DOI: [DOI] [PubMed] [Google Scholar]
- 25.Assicot M, Gendrel D, Carsin H, Raymond J, Guilbaud J, Bohuon C. High serum procalcitonin concentrations in patients with sepsis and infection. Lancet. 1993;341(8844):515–518. doi: 10.1016/0140-6736(93)90277-n. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dandona P, Nix D, Wilson MF, Aljada A, Love J, Assicot M, et al. Procalcitonin increase after endotoxin injection in normal subjects. J Clin Endocrinol Metab. 1994;79(6):16058. doi: 10.1210/jcem.79.6.7989463. DOI: [DOI] [PubMed] [Google Scholar]
- 27.Phua J, Koh Y, Du B, Tang YQ, Divatia JV, Tan CC, et al. Management of severe sepsis in patients admitted to Asian intensive care units: prospective cohort study. BMJ. 2011;342:d3245. doi: 10.1136/bmj.d3245. (jun13 1): DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mölkänen T, Ruotsalainen E, Thorball CW, Järvinen A. Elevated soluble urokinase plasminogen activator receptor (suPAR) predictsmortality in staphylococcus aureus bacteremia. Eur J Clin Microbiol Infect Dis. 2011;30(11):1417–1424. doi: 10.1007/s10096-011-1236-8. DOI: [DOI] [PubMed] [Google Scholar]
- 29.Sehestedt T, Lyngbæk S, Eugen-Olsen J, Jeppesen J, Andersen O, Hansen TW, et al. Soluble urokinase plasminogen activator receptor is associated with subclinical organ damage and cardiovascular events. Atherosclerosis. 2011;216(1):237–243. doi: 10.1016/j.atherosclerosis.2011.01.049. DOI: [DOI] [PubMed] [Google Scholar]
- 30.Kofoed K, Eugen-Olsen J, Petersen J, Larsen K, Andersen O. Predicting mortality in patients with systemic inflammatory response syndrome: an evaluation of two prognostic models, two soluble receptors, and a macrophage migration inhibitory factor. Eur J Clin Microbiol Infect Dis. 2008;27(5):375–383. doi: 10.1007/s10096-007-0447-5. DOI: [DOI] [PubMed] [Google Scholar]
- 31.Schultz M, Rasmussen L, Andersen M, Stefansson J, Falkentoft A, Alstrup M, et al. Use of the prognostic biomarker suPAR in the emergency department improves risk stratification but has no effect on mortality: a cluster-randomized clinical trial (TRIAGE III). Scand J Trauma Resusc Emerg Med. 2018;26(1):69. doi: 10.1186/s13049-018-0539-5. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]