ABSTRACT
Extrahepatic bile duct duplication is a rare biliary anomaly often associated with conditions like cholecysto-choledocholithiasis, choledochal cyst and malignancy. Precise preoperative diagnosis using conventional radiologic imaging still remains a challenge and use of existing classification system is equally confusing. A female patient diagnosed with choledochal cyst by magnetic resonance cholangiopancreatography was found to have an associated new variant of double common bile duct during surgery. The variant discovered could not be classified by existing classification systems and was missed by preoperative imaging. Recognition of existence of this anomaly that warrants careful dissection during biliary surgery is necessary to avoid inadvertent biliary injury as preoperative diagnosis still remains a challenge. Review of existing classification systems is required to include newly discovered variants.
INTRODUCTION
Choledochal cysts (CC) are rare biliary anomalies predominantly encountered in children, but increasingly being diagnosed in adults [1]. It is less common in Western population (1 in 100 000 to 1 in 150 000 individuals) compared with Asian population (1 in 13 000 individuals) and affects more females than males [female to male ratio of 4:1] [2]. Similarly, duplicated extrahepatic bile duct, also called double common bile duct (DCBD) and first reported by Vesalius in 1543 [3], is an extremely rare form of biliary anomaly with an unknown prevalence. Both CC and DCBD are known to co-exist and are also associated with other conditions such as cholecysto-choledocholithiasis, pancreatobiliary maljunction (PBM) and malignancy [4]. An unclassified variant of DCBD associated with CC is presented here-in.
CASE PRESENTATION
A 35-year-old female presented to a local hospital with a 3-month history of intermittent abdominal pain. Initial abdominal ultrasonography revealed cystic dilatation of the extrahepatic bile duct. A suspicion of choledochal cyst was made and was referred for surgical management. Her past medical history was unremarkable. She weighed 83 kg and was 164 cm tall, with body mass index of 30.9 kg/m2. Apart from mild right upper quadrant tenderness, her physical examination was unremarkable. Laboratory tests including liver and renal function tests, serum and urine amylase levels were normal. A magnetic resonance cholangio-pancreatography (MRCP) done showed a cystic fusiform dilatation of the common bile duct (CBD) extending into the right and left hepatic ducts (Fig. 1). No PBM was observed. The MRCP findings suggested type Ic CC. Without any further imaging, patient was scheduled for complete cyst excision with cholecystectomy and hepaticoenterostomy surgery. At laparotomy, the CBD was found to be fusiformly dilated. Bile samples were taken from the cyst and the gallbladder (GB) for amylase level essays. The GB was dissected from the liver bed and the cystic duct opened into the midportion of the cyst. After careful dissected of the cyst from surrounding vascular structures, the distal part entering the head of pancreas was noticed to be unaffected (Fig. 2). The distal part was transected just at the level of the head of pancreas and samples were taken for frozen section. Dissection at the hepatic hilum revealed two separate dilated ducts originating from the confluence of the left and right hepatic ducts and both entering into the cyst (Fig. 3). The two ducts were transected just distal to their origin from hepatic confluence to avoid confusing them as true right and left hepatic ducts (Fig. 4). The hepatic confluence was then opened to expose the true left and right hepatic ducts (Fig. 5). The dilated portions of the both hepatic ducts were transected and samples were taken for frozen section. A right and left hepaticojejunostomy reconstruction was done. No intraoperative cholangiogram was performed. Frozen section results of both the distal and proximal surgical margins were negative for malignancy. The amylase levels of both the cyst and GB were 47 031 and 44 770 U/L, respectively (normal serum amylase level: 25–110 U/L). Patient was discharged on postoperative Day 6. She is well with no evidence of malignancy after 23 months of follow-up.
Figure 1.

(A) MRI and (B) MRCP showing cystic dilatation of the common bile duct with intrahepatic extension (type Ic).
Figure 2.
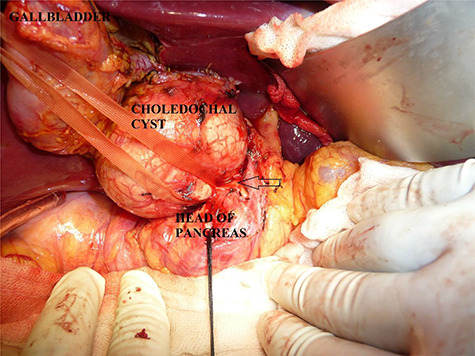
Open view of the choledochal cyst after removal of gallbladder from liver bed. Distal part of cyst noted to be normal as it enters the head of pancreas (arrow).
Figure 3.
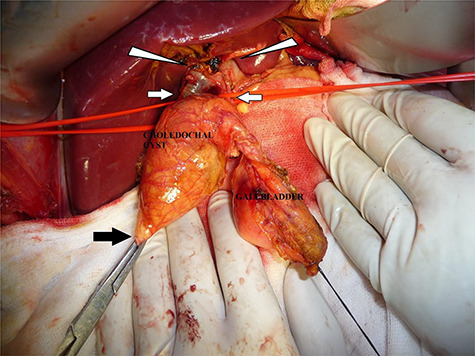
Proximal hilar dissection showing double ducts (white arrows) originating from the hilar confluence of left and right hepatic ducts (arrow head). Distal part of cyst transected from head of pancreas (black arrow).
Figure 4.
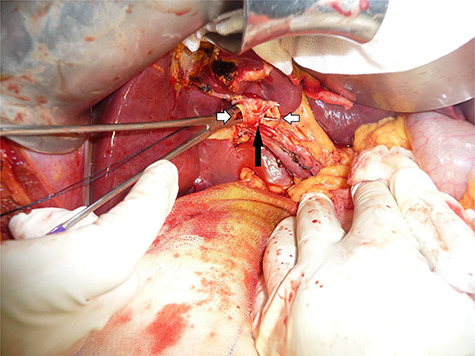
Orifice of the left- and right-sided double ducts after transection distal to the hepatic confluence.
Figure 5.
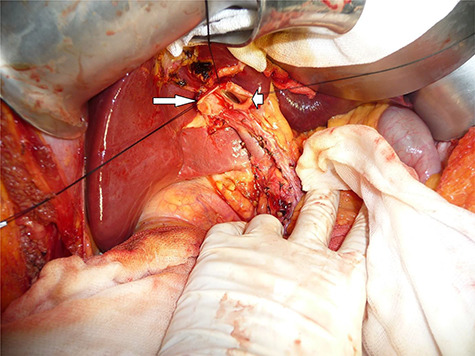
Opened hepatic confluence showing left (short arrow) and right hepatic (long arrow) duct orifices.
DISCUSSION
Co-existence of CC and DCBD and their association with other conditions such as cholecysto-choledocholithiasis, PBM and malignant transformation have been well documented [1]. Abdominal pain is the most common presenting complaint although significant number of cases are asymptomatic for both conditions. Cholangitis, pancreatitis, recurrent gallstone formation and malignancy are among the frequently reported clinical presentations in the literature [2, 4]. Unlike CC, preoperative diagnosis of DCBD remains a challenge with most cases diagnosed surprisingly during surgery or after inadvertent biliary injury [5]. Although MRCP is the preferred choice of imaging for both anomalies, other imaging modalities including computed tomography, esophagogastroduodenoscopy, endoscopic retrograde cholangio-pancreatography and intraoperative cholangiography have been used to diagnose these anomalies successfully [4, 6]. The Todani and Choi classification systems based on morphology are widely used to classify CC and DCBD, respectively [7, 8]. In the current case, the patient was diagnosed with type Ic (fusiform dilatation of extrahepatic bile duct) choledochal cyst using MRCP. However, the MRCP failed to identify the presence of DCBD which was found during surgery. The variant discovered appears to be similar to the type previously reported by Nuamah et al. [5], with the cyst affecting the distal common channel. It differs from Choi’s type Vb in that the cystic duct opens into the distal common channel instead of the right sided duct (Fig. 6). A review of the Japanese and Chinese literature revealed CC and DCBD co-existed in 10.6 and 33.3% of the reported cases of DCBD, respectively [4, 6]. None of these reports, however, commented on the types of CC (per the Tadoni classification) identified We have inserted the running head. In the cases. In the review by Tahara et al. [9] of pediatric cases of DCBD, seven out of the total eight cases had type I [four fusiform and three saccular] choledochal cyst. Another characteristic of both CC and DBCD is their association with PBM, considered a risk factor for biliary cancer [10]. Although the MRCP done in the current case could not confirm the presence of PBM, the extremely high levels of amylase in both bile samples from the CC and GB strongly suggest reflux of pancreatic secretions into the cyst. The preferred management option for both conditions is excision of the extrahepatic biliary ducts and bilioenteric anastomosis, although close monitoring could be suitable for certain subtypes of both anomalies. Although the risk of malignancy is reported to be significantly reduced after surgical excision of CC (from 23–28% to 0–6%), long-term follow-up is recommended [10].
Figure 6.
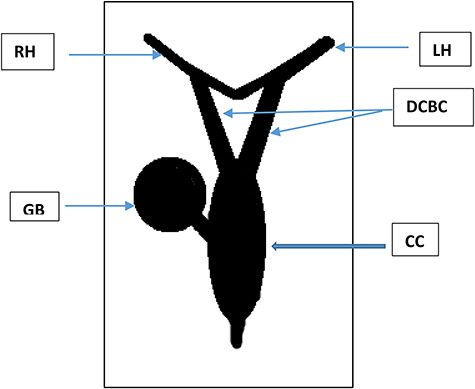
Schematic illustration of the variant described. LH: left hepatic duct, RH: right hepatic duct, DCBD: double bile duct originating from the hepatic duct confluence, CC: fusiform cyst formed at the distal unified portion of the DCBC, GB: gallbladder emptying into the CC.
CONCLUSION
Both choledochal cyst and DCBD are rare forms of biliary anomalies co-existing in some individuals. Preoperative diagnosis of DCBD still remain a challenge, hence careful dissection with high index of suspicion is required to avoid inadvertent biliary injury. Both conditions can lead to malignancy, hence surgical excision and long-term follow-up is recommended in most cases. A comprehensive study of all reported variants and review of existing classification systems is required.
CONFLICT OF INTEREST
All authors have no conflict of interest relating to this article and no financial disclosure.
CONSENT FOR PUBLICATION
Informed consent was obtained for this case report.
REFERENCE
- 1. Edil BH, Cameron JL, Reddy S, Lum Y, Lipsett PA, Nathan H, et al. Choledochal cyst disease in children and adults: a 30-year single-institution experience. J Am Coll Surg 2008;206:1000–5. [DOI] [PubMed] [Google Scholar]
- 2. Soares KC, Arnaoutakis DJ, Kamel I, Rastegar N, Anders R, Maithel S, et al. Choledochal cysts: presentation, clinical differentiation, and management. J Am Coll Surg 2014;219:1167–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Vesalius A. De humani corporis fabrica libri septem. Lib 5, Cap 8, Lc1543;624 (from Boyden EA).
- 4. Yamashita K, Oka Y, Urakami A, Iwamoto S, Tsunoda T, Eto T. Double common bile duct: a case report and a review of the Japanese literature. Surgery 2002;131:676–81. [DOI] [PubMed] [Google Scholar]
- 5. Nuamah NM, Ibis C, Gok AFK, Ekiz F, Acunas B. Duplicated common bile duct: a recipe for biliary injury. Report of a new variant. J Surg Case Rep 2017;4:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chen G, Wang H, Zhang L, Li Z, Bie P. Double common bile duct with choledochal cyst and cholelithiasis: report of a case. Surg Today 2014;44:778–82. [DOI] [PubMed] [Google Scholar]
- 7. Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K. Congenital bile duct cysts: classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg 1977;134:263–9. [DOI] [PubMed] [Google Scholar]
- 8. Choi E, Byun JH, Park BJ, Lee MG. Duplication of the extrahepatic bile duct with anomalous union of the pancreaticobiliary ductal system revealed by MR cholangiopancreatography. Br J Radiol 2007;80:150–4. [DOI] [PubMed] [Google Scholar]
- 9. Tahara K, Ishimaru Y, Fujino J, Suzuki M, Hatanaka M, Igarashi A, et al. Association of extrahepatic bile duct duplication with pancreati cobiliary maljunction and congenital biliary dilatation in children: a case report and literature review. Surg Today 2013;43:800–5. [DOI] [PubMed] [Google Scholar]
- 10. Jabłońska B. Biliary cysts: etiology, diagnosis and management. World J Gastroenterol 2012;18:4801–10. [DOI] [PMC free article] [PubMed] [Google Scholar]


