Abstract
This essay examines the implications of the COVID-19 pandemic for health inequalities. It outlines historical and contemporary evidence of inequalities in pandemics—drawing on international research into the Spanish influenza pandemic of 1918, the H1N1 outbreak of 2009 and the emerging international estimates of socio-economic, ethnic and geographical inequalities in COVID-19 infection and mortality rates. It then examines how these inequalities in COVID-19 are related to existing inequalities in chronic diseases and the social determinants of health, arguing that we are experiencing a syndemic pandemic. It then explores the potential consequences for health inequalities of the lockdown measures implemented internationally as a response to the COVID-19 pandemic, focusing on the likely unequal impacts of the economic crisis. The essay concludes by reflecting on the longer-term public health policy responses needed to ensure that the COVID-19 pandemic does not increase health inequalities for future generations.
Keywords: DEPRIVATION, Health inequalities, EMPLOYMENT, GENDER, GEOGRAPHY
INTRODUCTION
In 1931, Edgar Sydenstricker outlined inequalities by socio-economic class in the 1918 Spanish influenza epidemic in America, reporting a significantly higher incidence among the working classes.1 This challenged the widely held popular and scientific consensus of the time which held that ‘the flu hit the rich and the poor alike’.2 In the COVID-19 pandemic, there have been similar claims made by politicians and the media - that we are ‘all in it together’ and that the COVID-19 virus ‘does not discriminate’.3 This essay aims to dispel this myth of COVID-19 as a socially neutral disease, by discussing how, just as 100 years ago, there are inequalities in COVID-19 morbidity and mortality rates—reflecting existing unequal experiences of chronic diseases and the social determinants of health. The essay is structured in three main parts. Part 1 examines historical and contemporary evidence of inequalities in pandemics—drawing on international research into the Spanish influenza pandemic of 1918, the H1N1 outbreak of 2009 and the emerging international estimates of socio-economic, ethnic and geographical inequalities in COVID-19 infection and mortality rates. Part 2 examines how these inequalities in COVID-19 are related to existing inequalities in chronic diseases and the social determinants of health, arguing that we are experiencing a syndemic pandemic. In Part 3, we explore the potential consequences for health inequalities of the lockdown measures implemented internationally as a response to the COVID-19 pandemic, focusing on the likely unequal impacts of the economic crisis. The essay concludes by reflecting on the longer-term public health policy responses needed to ensure that the COVID-19 pandemic does not increase health inequalities for future generations.
PART 1. HISTORICAL AND CONTEMPORARY EVIDENCE OF INEQUALITIES IN PANDEMICS
More recent studies have confirmed Sydenstricker’s early findings: there were significant inequalities in the 1918 Spanish influenza pandemic. The international literature demonstrates that there were inequalities in prevalence and mortality rates: between high-income and low-income countries, more and less affluent neighbourhoods, higher and lower socio-economic groups, and urban and rural areas. For example, India had a mortality rate 40 times higher than Denmark and the mortality rate was 20 times higher in some South American countries than in Europe.4 In Norway, mortality rates were highest among the working-class districts of Oslo5; in the USA, they were highest among the unemployed and the urban poor in Chicago,6 and across Sweden, there were inequalities in mortality between the highest and lowest occupational classes—particularly among men.7 In contrast, countries with smaller pre-existing social and economic inequalities, such as New Zealand, did not experience any socio-economic inequalities in mortality.8 9 An urban–rural effect was also observed in the 1918 influenza pandemic whereby, for example, in England and Wales, the mortality was 30%–40% higher in urban areas.10 There is also some evidence from the USA that the pandemic had long-term impacts on inequalities in child health and development.11
Several studies have also demonstrated inequalities in the 2009 H1N1 influenza pandemic. For example, globally, Mexico experienced a higher mortality rate than that in higher-income countries.12 In terms of socio-economic inequalities, themortality rate from H1N1 in the most deprived neighbourhoods of England was three times higher than in the least deprived.13 It was also higher in urban compared to rural areas.13 Similarly, a Canadian study in Ontario found that hospitalisation rates for H1N1 were associated with lower educational attainment and living in a high deprivation neighbourhood.14 Another study found positive associations between people with financial issues (eg, financial barriers to healthcare access) and influenza-like illnesses during the 2009 H1N1 pandemic in the USA.15 Various studies on cyclical winter influenza in North America have also found associations between mortality, morbidity and symptom severity and socio-economic status among adults and children.16 17
Just as in 1918 and 2009, evidence of social inequalities is already emerging in relation to COVID-19 from Spain, the USA and the UK. Intermediate data published by the Catalonian government in Spain suggest that the rate of COVID-19 infection is six or seven times higher in the most deprived areas of the region compared to the least deprived.18 Similarly, in preliminary USA analysis, Chen and Krieger (2020) found area-level socio-spatial gradients in confirmed cases in Illinois and positive test results in New York City, with dramatically increased risk of death observed among residents of the most disadvantaged counties.19 With regard to ethnic inequalities in COVID-19, data from England and Wales have found that people who are black, Asian and minority ethnic (BAME) accounted for 34.5% of 4873 critically ill COVID-19 patients (in the period ending April 16, 2020) and much higher than the 11.5% seen for viral pneumonia between 2017 and 2019.20 Only 14% of the population of England and Wales are from BAME backgrounds. Even more stark is the data on racial inequalities in COVID-19 infections and deaths that are being released by various states and municipalities in the USA. For example, in Chicago (in the period ending April 17, 2020), 59.2% of COVID-19 deaths were among black residents and the COVID-19 mortality rate for black Chicagoans was 34.8 per 100 000 population compared to 8.2 per 100 000 population among white residents.21 There will likely be an interaction of race and socio-economic inequalities, demonstrating the intersectionality of multiple aspects of disadvantage coalescing to further compound illness and increase the risk of mortality.22
PART 2. THE SYNDEMIC OF COVID-19, CHRONIC DISEASE AND THE SOCIAL DETERMINANTS OF HEALTH
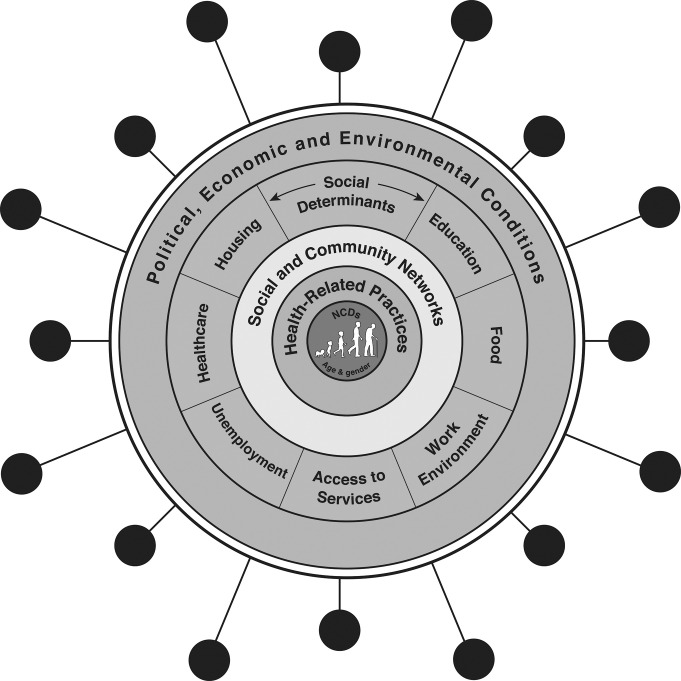
The COVID-19 pandemic is occurring against a backdrop of social and economic inequalities in existing non-communicable diseases (NCDs) as well as inequalities in the social determinants of health. Inequalities in COVID-19 infection and mortality rates are therefore arising as a result of a syndemic of COVID-19, inequalities in chronic diseases and the social determinants of health. The prevalence and severity of the COVID-19 pandemic is magnified because of the pre-existing epidemics of chronic disease—which are themselves socially patterned and associated with the social determinants of health. The concept of a syndemic was originally developed by Merrill Singer to help understand the relationships between HIV/AIDS, substance use and violence in the USA in the 1990s.23 A syndemic exists when risk factors or comorbidities are intertwined, interactive and cumulative—adversely exacerbating the disease burden and additively increasing its negative effects: ‘A syndemic is a set of closely intertwined and mutual enhancing health problems that significantly affect the overall health status of a population within the context of a perpetuating configuration of noxious social conditions’ [24 p13]. We argue that for the most disadvantaged communities, COVID-19 is experienced as a syndemic—a co-occurring, synergistic pandemic that interacts with and exacerbates their existing NCDs and social conditions (figure 1).
Figure 1.
The syndemic of COVID-19, non-communicable diseases (NCDs) and the social determinants of health (adapted from Singer23 and Dahlgren and Whitehead25).
Minority ethnic groups, people living in areas of higher socio-economic deprivation, those in poverty and other marginalised groups (such as homeless people, prisoners and street-based sex workers) generally have a greater number of coexisting NCDs, which are more severe and experienced at at a younger age. For example, people living in more socio-economically disadvantaged neighbourhoods and minority ethnic groups have higher rates of almost all of the known underlying clinical risk factors that increase the severity and mortality of COVID-19, including hypertension, diabetes, asthma, chronic obstructive pulmonary disease (COPD), heart disease, liver disease, renal disease, cancer, cardiovascular disease, obesity and smoking.26–29 Likewise, minority ethnic groups in Europe, the USA and other high-income countries experience higher rates of the key COVID-19 risk factors, including coronary heart disease and diabetes.28 Similarly, the Gypsy/Roma community—one of the most marginalised minority groups in Europe—has a smoking rate that is two to three times the European average and increased rates of respiratory diseases (such as COPD) and other COVID-19 risk factors.29
These inequalities in chronic conditions arise as a result of inequalities in exposure to the social determinants of health: the conditions in which people ‘live, work, grow and age’ including working conditions, unemployment, access to essential goods and services (eg, water, sanitation and food), housing and access to healthcare.25 30 By way of example, there are considerable occupational inequalities in exposure to adverse working conditions (eg, ergonomic hazards, repetitive work, long hours, shift work, low wages, job insecurity)—they are concentrated in lower-skill jobs. These working conditions are associated with increased risks of respiratory diseases, certain cancers, musculoskeletal disease, hypertension, stress and anxiety.31 In addition to these long-term exposures, inequalities in working conditions may well be impacting the unequal distribution of the COVID-19 disease burden. For example, lower-paid workers (where BAME groups are disproportionately represented)—particularly in the service sector (eg, food, cleaning or delivery services)—are much more likely to be designated as key workers and thereby are still required to go to work and rely on public transport for doing so. All these increase their exposure to the virus.
Similarly, access to healthcare is lower in disadvantaged and marginalised communities—even in universal healthcare systems.32 In England, the number of patients per general practitioner is 15% higher in the most deprived areas than that in the least deprived areas.33 Medical care is even more unequally distributed in countries such as the USA where around 33 million Americans—from the most disadvantaged and marginalised groups—have insufficient or no healthcare insurance.27 This reduced access to healthcare—before and during the outbreak—contributes to inequalities in chronic disease and is also likely to lead to worse outcomes from COVID-19 in more disadvantaged areas and marginalised communities. People with existing chronic conditions (eg, cancer or cardiovascular disease (CVD)) are less likely to receive treatment and diagnosis as health services are overwhelmed by dealing with the pandemic.
Housing is also an important factor in driving health inequalities.34 For example, exposure to poor quality housing is associated with certain health outcomes, for example, damp housing can lead to respiratory diseases such as asthma while overcrowding can result in higher infection rates and increased risk of injury from household accidents.34 Housing also impacts health inequalities materially through costs (eg, as a result of high rents) and psychosocially through insecurity (eg, short-term leases).34 Lower socio-economic groups have a higher exposure to poor quality or unaffordable, insecure housing and therefore have a higher rate of negative health consequences.35 These inequalities in housing conditions may also be contributing to inequalities in COVID-19. For example, deprived neighbourhoods are more likely to contain houses of multiple occupation and smaller houses with a lack of outside space, as well as have higher population densities (particularly in deprived urban areas) and lower access to communal green space.27 These will likely increase COVID-19 transmission rates—as was the case with H1N1 where strong associations were found with urbanity.13
The social determinants of health also work to make people from marginalised communities more vulnerable to infection from COVID-19—even when they have no underlying health conditions. Decades of research into the psychosocial determinants of health have found that the chronic stress of material and psychological deprivation is associated with immunosuppression.36 Psychosocial feelings of subordination or inferiority as a result of occupying a low position on the social hierarchy stimulate physiological stress responses (eg, raised cortisol levels), which, when prolonged (chronic), can have long-term adverse consequences for physical and mental health.37 By way of example, studies have found consistent associations between low job status (eg, low control and high demands), stress-related morbidity and various chronic conditions including coronary heart disease, hypertension, obesity, musculoskeletal conditions, and psychological ill health.38 Likewise, there is increasing evidence that living in disadvantaged environments may produce a sense of powerlessness and collective threat among residents, leading to chronic stressors that, in time, damage health.39 Studies have also confirmed that adverse psychosocial circumstances increase susceptibility—influencing the onset, course and outcome of infectious diseases—including respiratory diseases like COVID-19.40
PART 3. THE GREAT LOCKDOWN: THE COVID-19 ECONOMIC CRISIS AND HEALTH INEQUALITIES
The impact of COVID-19 on health inequalities will not just be in terms of virus-related infection and mortality, but also in terms of the health consequences of the policy responses undertaken in most countries. While traditional public health surveillance measures of contact tracing and individual quarantine were successfully pursued by some countries (most notably by South Korea and Germany) as a way of tackling the virus in the early stages, most other countries failed to do so, and governments worldwide were eventually forced to implement mass quarantine measures—in the form of lockdowns. These state-imposed restrictions—usually requiring the government to take on emergency powers—have been implemented to varying levels of severity, but all have in common a significant increase in social isolation and confinement within the home and immediate neighbourhood. The aims of these unprecedented measures are to increase social and physical distancing and thereby reduce the effective reproduction number (eR0) of the virus to less than 1. For example, in the UK, individuals were only allowed to leave the home for one of four reasons (shopping for basic necessities, exercise, medical needs, travelling for work purposes). Following Wuhan province in China, most of the lockdowns have been implemented for 8 to 12 weeks.
The immediate pathways through which the COVID-19 emergency lockdowns are likely to have unequal health impacts are multiple—ranging from unequal experiences of lockdown (eg, due to job and income loss, overcrowding, urbanity, access to green space, key worker roles), how the lockdown itself is shaping the social determinants of health (eg, reduced access to healthcare services for non-COVID-19 reasons as the system is overwhelmed by the pandemic) and inequalities in the immediate health impacts of the lockdown (eg, in mental health and gender-based violence). However, arguably, the longer-term and largest consequences of the ‘great lockdown’ for health inequalities will be through political and economic pathways (figure 1). The world economy has been severely impacted by COVID-19—with almost daily record stock market falls, oil prices have crashed and there are record levels of unemployment (eg, 5.2 million people filed for unemployment benefit in just 1 week in April 2020 in the USA), despite the unprecedented interventionist measures undertaken by some governments and central banks—such as the £300 billion injection by the UK government to support workers and businesses. The pandemic has slowed China’s economy with a predicted loss of $65 billion as a minimum in the first quarter of 2020. Economists fear that the economic impact will be far greater than the financial crisis of 2007/2008, and they say that it is likely to be worse in depth than the Great Depression of the 1930s. Just like the 1918 influenza pandemic (which had severe impacts on economic performance and increased poverty rates), the COVID-19 crisis will have huge economic, social and—ultimately—health consequences.
Previous research has found that sudden economic shocks (like the collapse of communism in the early 1990s and the global financial crisis (GFC) of 200841) lead to increases in morbidity, mental ill health, suicide and death from alcohol and substance use. For example, following the GFC, worldwide an excess of suicides were observed in the USA, England, Spain and Ireland.42 There is also evidence of other increases in poor mental health after the GFC including self-harm and psychiatric morbidity.41 42 These health impacts were not shared equally though—areas of the UK with higher unemployment rates had greater increases in suicide rates and inequalities in mental health increased with people living in the most deprived areas experiencing the largest increases in psychiatric morbidity and self-harm.43 Further, unemployment (and its well-established negative health impacts in terms of morbidity and mortality38) is disproportionately experienced by those with lower skills or who live in less buoyant local labour markets.27 So, the health consequences of the COVID-19 economic crisis are likely to be similarly unequally distributed—exacerbating heath inequalities.
However, the effects of recessions on health inequalities also vary by public policy response with countries such as the UK, Greece, Italy and Spain who imposed austerity (significant cuts in health and social protection budgets) after the GFC experiencing worse population health effects than those countries such as Germany, Iceland and Sweden who opted to maintain public spending and social safety nets.41 Indeed, research has found that countries with higher rates of social protection (such as Sweden) did not experience increases in health inequalities during the 1990s economic recession.44 Similarly, old-age pensions in the UK were protected from austerity cuts after the GFC and research has suggested that this prevented health inequalities increasing amongst the older population.45 These findings are in keeping with previous studies of the effects of public sector and welfare state contractions and expansions on trends in health inequalities in the UK, USA and New Zealand.27 46–49 For example, inequalities in premature mortality and infant mortality by income and ethnicity in the USA decreased during the period of welfare expansion in the USA (‘war on poverty’ era 1966 to 1980), but they increased again during the Reagan–Bush period (1980–2002) when welfare services and healthcare coverage were cut.46 Similarly, in England, inequalities in infant mortality rates reduced as child poverty decreased in a period of public sector and welfare state expansion (from 2000 to 2010),47 but increased again when austerity was implemented and child poverty rates increased (from 2010 to 2017).48
CONCLUSION
So this essay makes for grim reading for researchers, practitioners and policymakers concerned with health inequalities. Historically, pandemics have been experienced unequally with higher rates of infection and mortality among the most disadvantaged communities—particularly in more socially unequal countries.8 9 Emerging evidence from a variety of countries suggests that these inequalities are being mirrored today in the COVID-19 pandemic. Both then and now, these inequalities have emerged through the syndemic nature of COVID-19—as it interacts with and exacerbates existing social inequalities in chronic disease and the social determinants of health. COVID-19 has laid bare our longstanding social, economic and political inequalities - even before the COVID-19 pandemic, life expectancy amongst the poorest groups was already declining in the UK and the USA and health inequalities in some European countries have been increasing over the last decade.50 It seems likely that there will be a post-COVID-19 global economic slump—which could make the health equity situation even worse, particularly if health-damaging policies of austerity are implemented again. It is vital that this time, the right public policy responses (such as expanding social protection and public services and pursuing green inclusive growth strategies) are undertaken so that the COVID-19 pandemic does not increase health inequalities for future generations. Public health must ‘win the peace’ as well as the ‘war’.
Acknowledgments
We would like to thank Chris Orton from the Cartographic Unit, Department of Geography, Durham University, for his assistance with the graphics for figure 1.
Twitter: Clare Bambra @ProfBambra.
Funding: CB is a senior investigator in the National Institute for Health Research (NIHR) ARC North East and North Cumbria, NIHR Policy Research Unit in Behavioural Science, NIHR School of Public Health Research, the UK Prevention Research Partnership SIPHER: Systems science in Public Health and Health Economics Research consortium, and the Norwegian Research Council Centre for Global Health Inequalities Research. JF is a senior investigator in the NIHR ARC East of England. FM is a senior investigator in the NIHR Policy Research Unit in Ageing and Frailty. The views expressed in this publication are those of the authors and not necessarily those of the funders.
Competing interests: We have read and understood the BMJ Group policy on declaration of interests and declare the following interests: none.
Patient consent for publication: Not required.
Data sharing statement: Data sharing not applicable as no datasets generated and/or analysed for this study.
Provenance and peer review: Not commissioned; internally peer reviewed.
REFERENCES
- 1.Sydenstricker E. The incidence of influenza among persons of different economic status during the epidemic of 1918. Public Health Rep 2006[1931];121:191–204. [PubMed] [Google Scholar]
- 2.Lawrence AJ. The incidence of influenza among persons of different economic status during the epidemic of 1918 (1931): commentary. Public Health Rep 2006;121:190 10.1177/00333549061210S122 [DOI] [PubMed] [Google Scholar]
- 3.SkyNews (27/03/20) ‘virus does not discriminate claims Gove [Conservative government Minister for the Cabinet Office, UK]. Available https://news.sky.com/video/coronavirus-virus-does-not-discriminate-gove-11964771 (accessed 22 04 2020).
- 4.Murray CJ, Lopez AD, Chin B, et al. Estimation of potential global pandemic influenza mortality on the basis of vital registry data from the 1918-20 pandemic: a quantitative analysis. Lancet 2006;368:2211–8. 10.1016/S0140-6736(06)69895-4 [DOI] [PubMed] [Google Scholar]
- 5.Mamelund SE. A socially neutral disease? Individual social class, household wealth and mortality from Spanish influenza in two socially contrasting parishes in Kristiania 1918-19. Soc Sci Med 2006;62:923–40. 10.1016/j.socscimed.2005.06.051 [DOI] [PubMed] [Google Scholar]
- 6.Grantz KH, Rane MS, Salje H, et al. Disparities in influenza mortality and transmission related to sociodemographic factors within Chicago in the pandemic of 1918. PNAS 2016. 10.1073/pnas.1612838113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bengtsson T, Dribe M, Eriksson B. social class and excess mortality in sweden during the 1918 influenza pandemic. Am J Epidemiol. 2018;187:2568–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rice G, Bryder L. Black november: the 1918 influenza pandemic in New Zealand. Christchurch: Canterbury University Press, 2005. [Google Scholar]
- 9.Summers JA, Stanley J, Baker MG, et al. Risk factors for death from pandemic influenza in 1918: 1919: a case–control study. Influenza Other Respir Viruses 2014;8:329–38. 10.1111/irv.12228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chowell G, Bettencourt LMA, Johnson N, et al. The 1918–1919 influenza pandemic in England and Wales: spatial patterns in transmissibility and mortality impact. Proc R Soc B 2008;275:501–9. 10.1098/rspb.2007.1477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Almond D. Is the 1918 influenza pandemic over? Long‐term effects of in utero influenza exposure in the post‐1940 U.S. population. J Polit Econ 2006;114:672–712. 10.1086/507154 [DOI] [Google Scholar]
- 12.Charu V, Chowell G, Majia LSF, et al. Mortality burden of the H1N1 pandemic in Mexico: a comparison of deaths and years of life lost to seasonal influenza. Clin Infect Dis 2011;53:985–93. 10.1093/cid/cir644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rutter PD, Mytton OT, Mak M, et al. Socio-economic disparities in mortality due to pandemic influenza in England. Int J Public Health 2012;57:745–50. 10.1007/s00038-012-0337-1 [DOI] [PubMed] [Google Scholar]
- 14.Lowcock EC, Rosella LC, Foisy J, et al. The social determinants of health and pandemic H1N1 2009 influenza severity. Am J Public Health 2012;102:51–8. 10.2105/AJPH.2012.300814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Biggerstaff M, Jhung MA, Reed C, et al. Impact of medical and behavioural factors on influenza-like Illness, healthcare-seeking, and antiviral treatment during the 2009 H1N1 pandemic: United States, 2009–2010. Epidemiol Infect 2014;142:114–25. 10.1017/S0950268813000654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tam K, Yousey-hindes K, Hadler L. Influenza-related hospitalization of adults associated with low census tract socioeconomic status and female sex in New Haven County, Connecticut, 2007-2011. Influenza Other Respir Viruses 2014;8:274–81. 10.1111/irv.12231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Crighton EJ, Elliott SJ, Moineddin R, et al. A spatial analysis of the determinants of pneumonia and influenza hospitalizations in Ontario (1992-2001). Soc Sci Med 2007;64:1636–50. 10.1016/j.socscimed.2006.12.001 [DOI] [PubMed] [Google Scholar]
- 18.Catalan Agency for Health Quality and Assessment (AQuAS) Coronavirus SARS-Cov-2 interactive map. Available http://aquas.gencat.cat/.content/IntegradorServeis/mapa_covid/atlas.html (accessed 22 Apr 2020).
- 19.Chen JT, Krieger N. Revealing the unequal burden of COVID-19 by income, race/ ethnicity,and household crowding: US county vs ZIP code analyses. Harvard Center for Population and Development Studies Working Paper Series 21 Apr 2020. Volume 19, Number 1. Available https://tinyurl.com/ya44we2r [DOI] [PubMed]
- 20.Intensive Care National Audit and Research Centre Report on COVID-19 in critical care 17 April 2020. London: Intensive Care National Audit and Research Centre, 2020. [Google Scholar]
- 21.Chicago Department of Public Health COVID-19 death characteristics for Chicago residents. 2020. Available https://www.chicago.gov/city/en/sites/covid-19/home/latest-data.html (accessed 18 Apr 2020).
- 22.Gkiouleka A, Huijts T, Beckfield J, et al. Understanding the micro and macro politics of health: inequalities, intersectionality and institutions - a research agenda. Soc Sci Med 2018;200:92–8. 10.1016/j.socscimed.2018.01.025 [DOI] [PubMed] [Google Scholar]
- 23.Singer M. Introduction to syndemics: a systems approach to public and community health. San Francisco, CA: Jossey-Bass, 2009. [Google Scholar]
- 24.Singer M. A dose of drugs, a touch of violence, a case of AIDS: conceptualizing the SAVA syndemic. Free Inq Creat Sociol 2000;28:13–24. [Google Scholar]
- 25.Dahlgren G, Whitehead M. Policies and strategies to promote social 9. Equity in health. Stockholm: Institute for Future Studies, 1991. [Google Scholar]
- 26.Guo L, Wei D, Zhang X, et al. Clinical features predicting mortality risk in patients with viral pneumonia: the MuLBSTA score. Front Microbiol 2019;10:2752 10.3389/fmicb.2019.02752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bambra C. Health divides: where you live can kill you. Bristol: Policy Press, 2016. [Google Scholar]
- 28.Public health England Local action on health inequalities understanding and reducing ethnic inequalities in health. London: Public Health England, 2018. [Google Scholar]
- 29.European commission Roma health report: health status of the Roma population in the member states of the European union. Brussels: European Commission, 2014. [Google Scholar]
- 30.WHO - World Health. Organisation Commission on the social determinants of health: closing the gap in a generation. Geneva, 2008. [Google Scholar]
- 31.Bambra C. Work, worklessness and the political economy of health inequalities. J Epidemiol Community Health 2011;65:746–50. 10.1136/jech.2009.102103 [DOI] [PubMed] [Google Scholar]
- 32.Todd A, Copeland A, Kasim A, et al. Access all areas? An area-level analysis of the relationship between community pharmacy and primary care distribution, urbanity and social deprivation in England. BMJ Open 2015;5:e007328 10.1136/bmjopen-2014-007328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lacobucci G. GPs in deprived areas face severest pressures. BMJ. 2019;365:l2104. [DOI] [PubMed] [Google Scholar]
- 34.Gibson M, Petticrew M, Bambra C, et al. Housing and health inequalities: a synthesis of systematic reviews of interventions aimed at different pathways linking housing and health. Health Place 2011;17:175–84. 10.1016/j.healthplace.2010.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McNamara CL, Balaj M, Thomson KH, et al. The contribution of housing and neighborhood conditions to educational inequalities in non-communicable diseases in Europe: findings from the European social survey (2014) special module on the social determinants of health. Eur J Public Health 2017;27:102–6. 10.1093/eurpub/ckw224 [DOI] [PubMed] [Google Scholar]
- 36.Segerstrom SC, Miller GE. Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychol Bull 2004;130:601–30. 10.1037/0033-2909.130.4.601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bartley M. Health inequality: an introduction to concepts, theories and methods. 2nd edn. London: Polity, 2016. [Google Scholar]
- 38.Bambra C. Work, worklessness and the political economy of health. Oxford: Oxford University Press, 2011. [DOI] [PubMed] [Google Scholar]
- 39.Whitehead M, Pennington A, Orton L, et al. How could differences in “control over destiny” lead to socio-economic inequalities in health? A synthesis of theories and pathways in the living environment. Health Place 2016;39:51–61. 10.1016/j.healthplace.2016.02.002 [DOI] [PubMed] [Google Scholar]
- 40.Biondi M, Zannino L . Psychological stress, neuroimmunomodulation, and susceptibility to infectious diseases in animals and man: a review. Psychother Psychosom 1997;66:3–26. 10.1159/000289101 [DOI] [PubMed] [Google Scholar]
- 41.Stuckler D, Basu S. The body economic. why austerity kills. London: Thomas Allen, 2013. [Google Scholar]
- 42.Corcoran P, Griffin E, Arensman E, et al. Impact of the economic recession and subsequent austerity on suicide and self-harm in Ireland: an interrupted time series analysis. Int J Epidemiol 2015;44:969–77. 10.1093/ije/dyv058 [DOI] [PubMed] [Google Scholar]
- 43.Barr B, Kinderman P, Whitehead P. Trends in mental health inequalities in England during a period of recession, austerity and welfare reform 2004-2013. Soc Sci Med 2015;147:324–31. 10.1016/j.socscimed.2015.11.009 [DOI] [PubMed] [Google Scholar]
- 44.Copeland A, Bambra C, Nylen L, et al. All in it together? The effects of recession on population health and health inequalities in England and Sweden, 1991 to 2010. Int J Health Serv 2015; 45: 45 3–24. [DOI] [PubMed] [Google Scholar]
- 45.Akhter N, Bambra C, Mattheys K, et al. Inequalities in mental health and well-being in a time of austerity: longitudinal findings from the Stockton-on-Tees cohort study. SSM Pop Health 2018;6:75–84. 10.1016/j.ssmph.2018.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Krieger N, Rehkopf DH, Chen JT, et al. The fall and rise of US inequities in premature mortality: 1960-2002. PLoS Med 2008;5:227–41. 10.1371/journal.pmed.0050046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Robinson T, Brown H, Norman P, et al. Investigating the impact of New Labour’s English health inequalities strategy on geographical inequalities in infant mortality: a time trend analysis. J Epidemiol Community Health 2019;73:564–8. 10.1136/jech-2018-211679 [DOI] [PubMed] [Google Scholar]
- 48.Taylor-Robinson D, Lai E, Wickham S, et al. (2019) Assessing the impact of rising child poverty on the unprecedented rise in infant mortality in England, 2000–2017: time trend analysis. BMJ Open 2019;9:e029424 10.1136/bmjopen-2019-029424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Beckfield J, Bambra C. Shorter lives in stingier states: social policy shortcomings help explain the US mortality disadvantage. Soc Sci Med. 2016;171:30–8. [DOI] [PubMed] [Google Scholar]
- 50.Forster T, Kentikelenis A, Bambra C. Health inequalities in Europe: setting the stage for progressive policy action, Foundation for European Progressive Studies and the Think Tank for Action on Social Change (TASC). 2018. Available https://www.feps-europe.eu/component/attachments/attachments.html?task=attachment&id=168