Abstract
Purpose
To evaluate the safety and efficacy of intra corneal ring segment (ICRS) implantation combined with crosslinking (CXL) using a Small Incision Lenticule Extraction (SMILE) lenticule for intraoperative stromal augmentation in thin corneas.
Observations
The procedure was performed in three eyes of progressive keratoconus or post refractive surgery corneal ectasia, with a preoperative mean thinnest pachymetry of 389.34 ± 5.5 μm. Keratometry flattening (preoperative mean maximum keratometry of 63.17 ± 9.31D to postoperative mean maximum keratometry of 54.77 ± 9.47D) and improvement in spectacle corrected distance visual acuity (mean preoperative LogMAR 0.43 ± 0.19 to mean postoperative LogMAR 0.71 ± 0.26) was noted at three months, with stability at one-year postoperative visit. Demarcation line was demonstrated at a depth of 220.67 ± 8.32 μm. No significant endothelial cell loss was noted.
Conclusions and importance
Intraoperative stromal thickness augmentation using a lenticule obtained from SMILE allows safe and effective CXL in combination with ICRS in ultrathin corneas. This allows an alternative to lamellar keratoplasty for visual rehabilitation in such eyes.
Keywords: Corneal collagen cross-linking, Intra corneal ring segment, Keratoconus, Post refractive surgery ectasia, Thin corneas
1. Introduction
Corneal ectatic disorders, including keratoconus and post refractive surgery ectasia are associated with progressive thinning, protrusion and increased aberrations. Corneal collagen crosslinking (CXL) increases the mechanical and biochemical strength of the tissue, thereby halting the ectatic process.1 In advanced stages of the disease, a combination with Intra Corneal Ring Segments (ICRS) affords global tissue remodeling with improvement in the anterior and posterior corneal profile.2 Although the corneal pachymetry might be adequate at the site of ICRS placement, the thinnest pachymetry may well be below the threshold of that considered safe for traditional CXL.3 The authors have described the use of a stromal lenticule obtained from patients undergoing Small Incision Lenticule Extraction (SMILE) for intraoperative stromal augmentation in thin corneas undergoing CXL.4 We describe the clinical outcomes of the above technique with concomitant ICRS implantation in three eyes over a one-year follow-up period.
1.1. Findings
The study adhered to the tenets of declaration of Helsinki, Ethics committee clearance was obtained and an informed consent was taken from the patients. Eyes with progressive keratoconus or post refractive surgery ectasia with a thinnest pachymetry lower than 400 μm, central clear cornea with no scarring, pachymetry greater than 400 μm at the site of ICRS placement, contact lens intolerance and mesopic pupil not greater than 5mm were included in the study.
Clinical examination preoperatively and at one, three and twelve months’ postoperative visit included: uncorrected distance visual acuity (UDVA), manifest refraction, corrected spectacle distance visual acuity (CSDVA), slit lamp bio microscopy, dilated fundus evaluation, corneal tomography (Pentacam HR, Oculus Optikgerate GmbH, Wetzlar, Germany), anterior segment optical coherence tomography (Optovue, CA, USA) and specular microscopy (Topcon SP-1P).
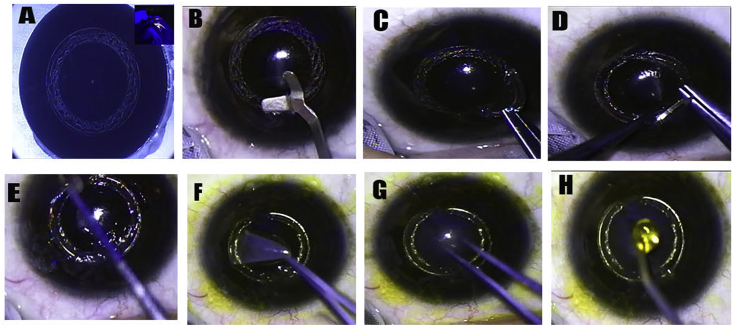
The procedure was performed under topical anesthesia with Proparacaine 0.5% (Alcaine) drops. The pupil or geometric center of the cornea was marked to localize the center of intrastromal dissection. The channels for placement of segments were fashioned at 80% stromal depth using the VisuMax femtosecond laser system (Carl Zeiss, Meditec) with the incision along steepest meridian (Fig. 1a). Selection of number, arc length and thickness of segment(s) was made using the nomogram defined by the manufactures. Segments were inserted into the channels using special forceps (Fig. 1b and c) and a 10–0 nylon suture was placed at the incision site (Fig. 1d). De-epithelialization (Fig. 1e) was followed by intraoperative pachymetry to determine the required thickness of the refractive lenticule. The lenticule was obtained from patients undergoing Small Incision Lenticule Extraction (SMILE) for myopic correction (Fig. 1f). All patients underwent serological investigation for Human Immunodeficiency Virus and hepatitis. The central area of the lenticule was placed over the apex of the cone (Fig. 1g) and an augmented stromal thickness greater than 400 μm was confirmed by intraoperative ultrasonic pachymetry, allowing CXL to be performed within the required safety protocol guidelines. One drop of riboflavin (0.1% solution of 10 mg riboflavin-5-phosphate) was instilled every 5 minutes for 30 minutes (Fig. 1h) and drop every 5 minutes under UVA irradiation for the next 30 minutes. Ultraviolet-A radiation of 365 nm with desired irradiance of 3 mW/cm2 was delivered at a distance of 5 cm (UV-X, IROC Innocross AG). On completion of the procedure, the refractive lenticule was peeled off the stromal bed, the surface was irrigated with normal saline and a bandage contact lens was placed.
Fig. 1.
Steps of Intracorneal Ring Segments with lenticule assisted cross-linking. (1a) Femtosecond laser assisted creation of channels and corneal incision. (1b) Opening of channels. (1c) Insertion of intra corneal ring segments. (1d) 10–0 nylon suture placed at corneal incision. (1e) Epithelial debridement with blunt spatula. (1f) Stromal thickness augmentation using lenticule obtained from Small Incision Lenticule Extraction. (1g) Placement of thickest center of lenticule over thinnest area of cone. (1h) Riboflavin instillation and remaining CXL carried out as per standard guidelines.
Postoperative medications included gatifloxacin 0.3% eye drops 4 times daily for one week, loteprednol etabonate 0.5% eye drops (L-Pred) 3 times daily for 3 weeks, and polyethylene glycol 0.4% and propylene glycol 0.3% (Systane Ultra, Alcon Laboratories) for 2 months.
The procedure was performed in three eyes with a minimal follow-up of one year (Table 1). Keratometry flattening (preoperative mean maximum keratometry of 63.17 ± 9.31D to postoperative mean maximum keratometry of 54.77 ± 9.47D) with an associated improvement in corrected spectacle visual acuity (mean preoperative LogMAR 0.43 ± 0.19 to mean postoperative LogMAR 0.71 ± 0.26) was noted. No significant endothelial cell loss was observed. All eyes demonstrated stability at one-year follow-up visit. No persistent haze or scarring was noted in any of the eyes at final postoperative visit.
Table 1.
Treatment outcomes in three eyes.
| Case | 1 | 2 | 3 | |
|---|---|---|---|---|
| Age/Sex | 33/M | 25/F | 28/M | |
| Indication | Post LASIK ectasia | Keratoconus | Post LASIK ectasia | |
| Corrected spectacle visual acuity (LogMAR) | Preoperative | 0.4 | 0.63 | 0.25 |
| Postoperative | 0.63 | 1.0 | 0.50 | |
| Manifest refraction | Preoperative | −15.0 D sphere with −4.0 D cylinder @ 170 | −1.75 D sphere with −3.50 D cylinder @ 140 | −6.0 D sphere with −4.0 D cylinder @ 60 |
| Postoperative | −9.0 D sphere with −2.5 D cylinder @ 135 | −1.25 D sphere with −1.50 D cylinder @ 110 | −2.50 D sphere with −2.25 D cylinder @ 70 | |
| Simulated Keratometry (D) | Preoperative | 57.5/63.6 | 43.5/47.4 | 45.8/47.8 |
| Postoperative | 53.5/56.9 | 41.5/41.9 | 41.6/43.7 | |
| Maximum Keratometry (D) | Preoperative | 73.5 | 55.4 | 60.6 |
| Postoperative | 65.7 | 49.1 | 49.5 | |
| Thinnest Pachymetry (microns) | Preoperative | 384 | 395 | 389 |
| Postoperative | 374 | 366 | 403 | |
| Endothelial Cell Count (cells/mm2) | Preoperative | 2460 | 2674 | 2298 |
| Postoperative | 2428 | 2666 | 2301 | |
| Demarcation line (microns) | 214 | 230 | 218 |
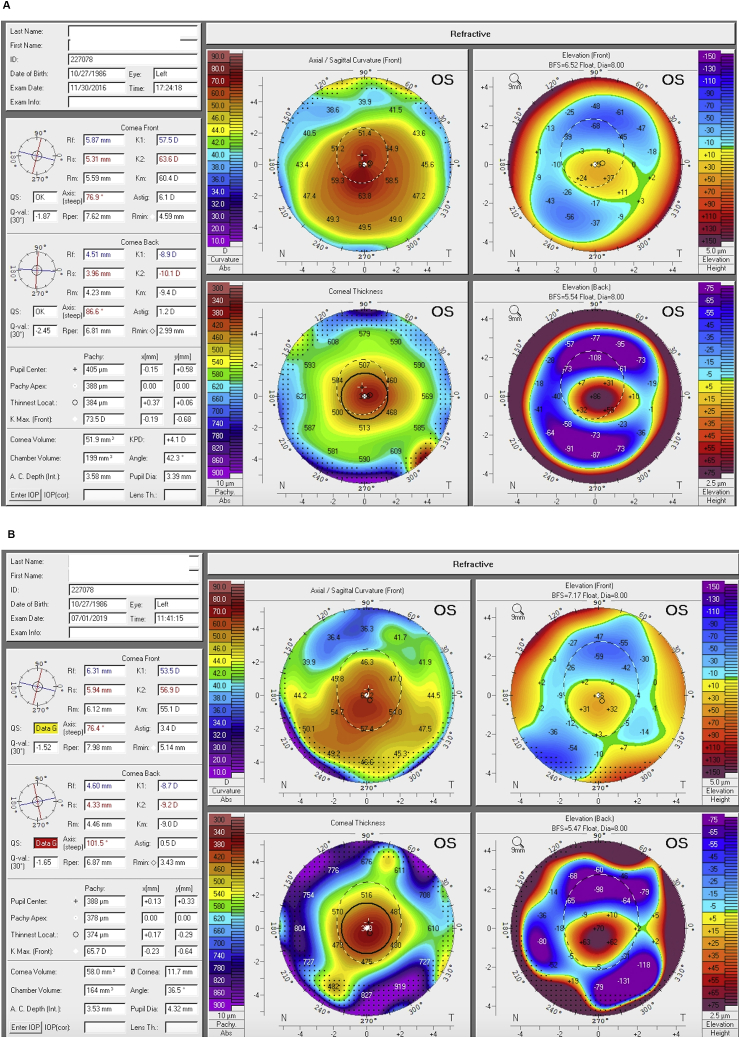
Fig. 2 demonstrates the preoperative (Fig. 2a) and three-year postoperative (Fig. 2b) tomography of one patient.
Fig. 2.
Preoperative (2a) and three-year postoperative (2b) corneal tomography following Intracorneal Ring Segments with lenticule assisted crosslinking in post LASIK ectasia.
2. Discussion
Keratectasia, either idiopathic or iatrogenic is associated with progressive corneal thinning and protrusion. Corneal collagen crosslinking (CXL) increases the mechanical and biochemical strength of the tissue, thereby halting the ectatic process. Standard Dresden protocol mandates a minimal stromal thickness of 400 μm, to limit ultraviolet A radiation at the endothelial level below damage threshold. Unfortunately, a number of patients with advanced keratoconus or post refractive surgery ectasia have thinner corneas, making the disease not amenable to traditional CXL.5
Treatment options in such cases would include lamellar keratoplasty with associated limitations including delayed visual recovery, risk of graft rejection and glaucomatous damage. Our technique allows cross-linking in eyes with stromal pachymetry below 400 μm by utilizing a lenticule obtained from patients undergoing SMILE for myopic correction. The thickness of the lenticule obtained depends on the refractive error corrected and affords tailored stromal expansion. Moreover, the biomechanical and absorptive properties of the lenticule are similar to the underlying stroma, unlike other methods of stromal augmentation including contact lens assisted CXL.6 Additionally, the lenticule remains firmly adherent to the underlying stromal surface and no intraoperative buckling is seen.
Other techniques for crosslinking in thin corneas including transepithelial CXL and topoguided epithelial debridement CXL,7,8 entail an intact epithelium over the cone thereby limiting the efficacy. Our technique involves epithelial debridement overcoming the limitations of epithelium on approaches.
3. Conclusions
To summarize, we describe a technique of tailored stromal expansion for performing CXL in thin and ultrathin corneas by adding a myopic lenticule. The technique was found to be safe and effective in our initial few cases. Long-term studies are required to further establish the efficacy and feasibility of this procedure.
Patient consent: Consent to publish the case report was not obtained. This report does not contain any personal information that could lead to the identification of the patient.
Funding
No funding or grant support
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
CRediT authorship contribution statement
Gitansha Shreyas Sachdev: Conceptualization, Methodology, Data curation, Writing - original draft, Writing - review & editing. Ritika Sachdev: Investigation, Writing - review & editing. Mahipal S. Sachdev: Investigation, Writing - review & editing, Supervision.
Declaration of competing interest
The following authors have no financial disclosure: GS, RS, MSS.
Acknowledgements
None.
Contributor Information
Gitansha Shreyas Sachdev, Email: sachdevgitansha@gmail.com.
Ritika Sachdev, Email: ritikasachdev@gmail.com.
Mahipal S. Sachdev, Email: drmahipal@gmail.com.
References
- 1.Wollensak G., Spoerl E., Seiler T. Riboflavin/ultraviolet- A–induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003;135:620–627. doi: 10.1016/s0002-9394(02)02220-1. [DOI] [PubMed] [Google Scholar]
- 2.Brenner L.F., Alió J.L., Vega-Estrada A. Indications for intrastromal corneal ring segments in ectasia after laser in situ keratomileusis. J Cataract Refract Surg. 2012;38(12):2117–2124. doi: 10.1016/j.jcrs.2012.07.036. [DOI] [PubMed] [Google Scholar]
- 3.Spoerl E., Mrochen M., Sliney D., Trokel S., Seiler T. Safety of UVA–riboflavin cross-linking of the cornea. Cornea. 2007;26:385–389. doi: 10.1097/ICO.0b013e3180334f78. [DOI] [PubMed] [Google Scholar]
- 4.Sachdev M.S., Gupta D., Sachdev G., Sachdev R. Tailored stromal expansion with refractive lenticule for cross-linking the ultrathin cornea. J Cataract Refract Surg. 2015;41:918–923. doi: 10.1016/j.jcrs.2015.04.007. [DOI] [PubMed] [Google Scholar]
- 5.Pearson A.R., Soneji B., Sarvananthan N., Sandford-Smith J.H. Does ethnic origin influence the incidence or severity of keratoconus? Eye. 2000;14(Pt 4):625–628. doi: 10.1038/eye.2000.154. [DOI] [PubMed] [Google Scholar]
- 6.Jacob S., Kumar D.A., Agarwal A., Basu S., Sinha P., Agarwal A. Contact lens-assisted collagen cross-linking (CACXL): a new technique for cross-linking thin corneas. J Refract Surg. 2014;30:366–372. doi: 10.3928/1081597X-20140523-01. [DOI] [PubMed] [Google Scholar]
- 7.Filippello M., Stagni E., O'Brart D. Transepithelial corneal collagen crosslinking: bilateral study. J Cataract Refract Surg. 2012;38:283–291. doi: 10.1016/j.jcrs.2011.08.030. erratum, 1515. [DOI] [PubMed] [Google Scholar]
- 8.Kymionis G.D., Diakonis V.F., Coskunseven E., Jankov M., Yoo S.H., Pallikaris I.G. Customized pachymetric guided epithelial debridement for corneal collagen cross linking. BMC Ophthalmol. 2009;9:10. doi: 10.1186/1471-2415-9-10. [DOI] [PMC free article] [PubMed] [Google Scholar]