Abstract
The global communities have been grappling with health pandemics for months since the outbreak of COVID-19, which has been flagged a global health emergency by World Health Organisation, WHO. While the entire health sector has been overburdened, cancer patients are also at a high risk of getting infected during this COVID-19 pandemic; hence, there is a great concern for these patients because there is little to no data to support their management with the current health care structure in Africa. This article outlines the challenges that frontline health workers face in the management of cancer patients, as the entire health sector calls for effective policy formulation and implementation by the government in their role in ensuring the sound health of their citizenry.
Keywords: Africa, COVID-19, Cancer patients, Health care, Oncologists
Résumé
Les communautés mondiales sont aux prises avec des pandémies de santé depuis des mois, depuis l’apparition du COVID-19, qui a été signalé comme une urgence sanitaire mondiale par l’Organisation mondiale de la santé. Alors que l’ensemble du secteur de la santé a été surchargé, les patients atteints de cancer courent également un risque élevé d’être infectés pendant cette pandémie de COVID-19, d’où une grande inquiétude pour ces patients, car il n’existe que peu ou pas de données pour soutenir leur prise en charge avec la structure actuelle des soins de santé en Afrique. Cet article décrit les défis auxquels sont confrontés les travailleurs de la santé de première ligne dans la prise en charge des patients cancéreux, car l’ensemble du secteur de la santé exige une formulation et une mise en œuvre efficaces des politiques par le gouvernement dans son rôle de garant de la bonne santé de ses citoyens.
Mots clés: Afrique, COVID-19, Patients cancéreux, Santé, Oncologues
Introduction
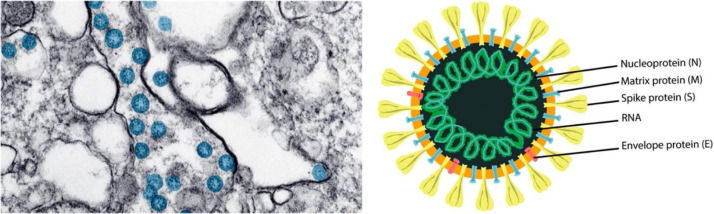
The world has been on a standstill for several months since the outbreak of coronavirus (SARS-COV2), which has been declared as a public health emergency (PHEIC) by the World Health Organisation (WHO). This was consequent upon its spread to almost all parts of the world in a short space of time, Africa inclusive. The spread of these new strains of pneumonia cases was linked to a large seafood and live animal market in Wuhan and is accompanied by clinical manifestations such as fever, cough and other respiratory symptoms [1], [2], [3], [4]. The average incubation period ranges from 2–14 days, with fever and respiratory symptoms appearing within 3–7 days after exposure to the virus [5]. Coronaviruses SARS-COV2, MERS-COV and SARS-COV all belong to the family Coronaviridae because of the unique crown-like shape of their viral envelopes that consist of club-shaped glycoprotein spikes (Fig. 1 ). Their reservoir hosts include bats, cats, camels and cattle, suggesting potential animal to human spread and then human to human spread which is a current major concern globally [6].
Figure 1.
Transmission electron microscope image of SARS-CoV-2 spherical viral particles in a cell.
Image au microscope électronique de la transmission des particules virales sphériques du SRAS-CoV-2 dans une cellule.
The spherical viral particles (colorised in blue) contain cross-sections through the viral genome, seen as black dots (as adapted from the US Centres for Disease Control). Representation of the viral structure is illustrated with its structural viral proteins. Reproduced with permission from Ref. [3], Copyright 2020 American Chemical Society and Ref. [7] Copyright Centre for Disease Control and Prevention. Accessed on May 14, 2020.
Africa's link with COVID-19 impact
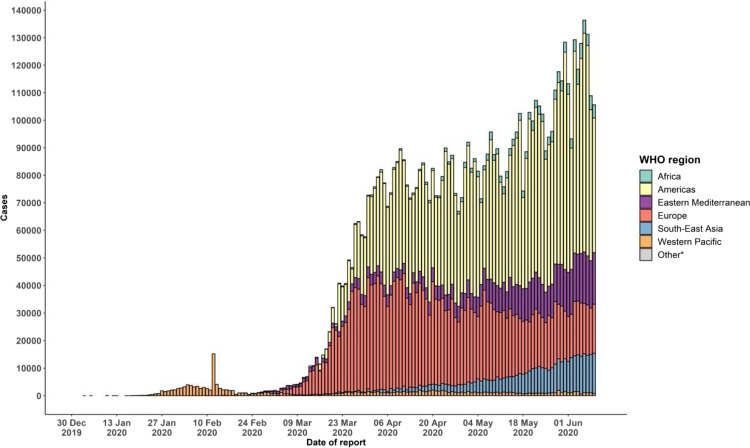
As from this moment and possibly for years to come, COVID-19 has the potential to progressively impact every aspect of life and humanity. This has been exacerbated by lockdown, quarantine and social distancing, pandemic control strategies which are still in use in most countries even to date. China has made remarkable progress to prevent the continuous spread of the virus and it is a known fact that the health sector of various nations all over the world has been in a tug of war situation with the coronavirus especially in Africa, where the health sector is inadequate to cater for the ∼1.3 billion human population. As at June 10, 2020, the globally confirmed cases summed up to 7,145,539 and 408,025 deaths out of which Africa as a continent, on the June 11, 2020 reported the lowest figures: 209,438 confirmed cases, 5678 deaths and 95,273 recoveries [8], [9] (Fig. 2 ).
Figure 2.
Number of confirmed COVID-19 cases, by date of report and WHO region.
Nombre de cas confirmés de COVID-19, par date de rapport et par région de l’OMS.
30 December 2019–11 June 2020. Reproduced with permission from Ref. [10] Copyright World Health Organisation.
It is not surprising that Africa has been heavily impacted by the pandemic but potential reasons for this should receive serious consideration. African countries have long histories of colonisation, being former colonies of France, United Kingdom, Germany, Italy, Portugal and Spain. This makes for constant travels between these places and Africa. Secondly, due to abundance of productive resources, Africa is a foreign investment destination for multinational organisations. Thirdly, due to the extensive human and mineral resources in Africa, there is constant influx of foreign nationals. Additionally, China, through the Silk Road (One Belt, One Road) Initiative, has been making efforts towards maintaining global relationship with different countries in the world, with different ethnicities residing in China and Chinese nationals residing in other parts of the world; hence, the major route of the spread of the virus from one country to another is through importation either by a citizen who has travelled to a highly infected region and returned to his or her home country or a foreigner/immigrant from an affected region travelling to another country. As at March 5, 2020, 27 cases were confirmed in Africa with Algeria being the epicentre having 17 cases, with all related to imported cases from Europe; Senegal's cases were 3 French nationals and a British citizen, while Nigeria's index case was an Italian business man, followed by 2 cases in Egypt, 1 case in Tunisia, Morocco and South Africa, respectively [11].
It is important to consider the oncological aspect of the health sector in relation to COVID-19 in Nigeria and Africa as the second largest continent of the world. COVID-19 has brought a huge impact on the general preparedness of the nation and population, be it economic, social, political or educational. Another important aspect plays out with regards to the restriction of mass gatherings as it involves social and religious activities and most profoundly, the psychological demeanour towards each other. COVID-19, as a public health emergency of international concern (PHEIC), provides an opportunity for the further expansion of knowledge based on the implementation of non-pharmaceutical interventions in order to quantify their utilities in pandemic mitigation, mass gatherings including the clearly-defined and spontaneously-occurring being the major determinants of the epidemiological expansion of disease outbreak [12].
Concern for health care workers; PPE donning
The route for the transmission of SARS-COV2 can be through contactand respiratory transmission; hence, in order for oncologists to function maximally, appropriate personal protective equipment (PPE) donning is of apparent need [13]. Currently, the number of COVID-19 cases in Nigeria is spiralling with a count of 5162 confirmed cases, 3815 active cases, 1180 discharged cases and 167 deaths on the 16th May, 2020, with the hotspots of infection being Lagos, Kano and Federal Capital Territory (FCT), while about 23,835 sample tests have so far been conducted in a population of ∼200 million [14]. However, the facts, that the speed of identifying active cases is slow and testing capacity is low, expose the frontline medical personnel to a higher risk as the work pressure has been huge and rising, hence the need for quick intervention of government (Fig. 3 ).
Figure 3.
COVID-19 public awareness poster on the functions of health workers.
Affiche de sensibilisation du public au COVID-19 sur les fonctions des travailleurs de la santé.
Reproduced from Ref. [15] Copyright 2020 Africa Union.
This can be achieved by speedily creating a quarantine zone for the infected patients, which will be distinguished and properly managed from a COVID-19 free zone for the non-infected patients, especially in healthcare establishments. Additionally, the effective protection of health workers will result in their willingness to serve in containing the viral infection, as they should be disallowed from activities that would aggravate contagion risk. On the other hand, hospitals are becoming a major point of infection with reported 70 deaths and about 6000 COVID-19 infected health workers by the end of March 2020. Additionally, the Body of Nurses and Midwives in Nigeria reported a loss of 15 health workers, with over 200,000 health care professionals being exposed to COVID-19, 85 nurses testing positive, ∼250 in isolation, in addition to 25 doctors testing positive. All these are attributed to inadequate PPEs and knowledge of using the PPEs, medical consumables and life support equipment, absence of life insurance, just to mention a few [16], [17], [18]. It is a glaring reality that during a time like this, the medical workers are the ones that receive the heaviest blow, hence the main reason that much attention should be directed towards them because the spread of COVID-19 cannot be curtailed without the bravery and sacrifice of the frontline medical workers. The consideration of all the above-mentioned as well as the need for government to efficiently play their role by paying more attention to communication and quick response coupled with fast action will go a long way handling reasons for the constant alarms raised by the medical community in Nigeria and Africa, in general. However, the major concern lies in the implementation of no-mass gatherings and social distancing, especially with the effective management of cancer patients by oncologists in Nigeria and Africa, in general. The informal sector, where the implementation of the no-mass gathering and social distancing is very difficult to control, plays a vital role in the advancement of the Nigerian economy, contributing 41.43% to Nigeria's Gross Domestic Products and 57.9% to Nigeria's Gross National Products at ∼US$212.6 billion [19]. Further question is the guarantee to enjoy quality life to infected cancer patients during the pandemic period, considering the associated stress of cancer. With all these questions in mind, a strategic plan has to be formulated to avoid any thriving failure during this and possible future pandemic.
Necessary intervention for cancer patients; screening and triaging
Apart from the elderly, chronically ill, pregnant women and young children, cancer patients are also very vulnerable to the infection because they are immunocompromised. It is an obvious fact that clinicians and clinical scientists have an in-depth knowledge of the impact of cancer on the body, especially the immune system. During this COVID-19 pandemic period, cancer-burdened patients have been regarded as a high-risk group due to their vulnerability to underlying illness as well as their immunosuppressed status. They are highly-risked to developing critical repercussions from the virus and this include intensive care hospitalisation or may even lead to death [20]. Alhalabi and Subbiah [21] reported the prevalence of cancer amongst patients with COVID-19 seems higher than its prevalence in the general populace, with 39–45% of cancer patients having severe events when infected.
Irrespective of the three primary disciplines of oncology; the medical, surgical and radiation including their team, the reality of all is the risk of being infected if they are inadequately protected and do not follow a strategic plan on how to triage. Porzio G. et al. [22], [23] reported non-availability of literature data and previously published experiences related to oncological home care during natural disasters. Moreover, the spread of infectious disease, especially due to COVID-19, has been presented from double-phased perspectives (i.e. associated risk of infected patients and health care professionals). The caregivers are expectedly required to devise methods for paying attention to the care seekers for the safety of both parties (the patients and health professionals), as the health care professional is regarded as a leader of the health care environment and society at large and hence can impact life-saving actions in order to decrease the possible human and economic damages from the COVID-19 outbreak [24]. Besides the fact that there is no specific vaccine at the moment in hospitals, it is necessary for cancer patients to stave off from contracting COVID-19. While aiming to bring down the meteoric rise, mitigating the spread would curb the potential of overpowering the health system in addition to allowing susceptible cancer patients to receive adequate conventional health service. In order to realise this aim, diagnostic biopsies and procedures and elective imaging for certain patients should be systemised to avoid relenting on the prospects of a cure [21].
Screening of patients play a very crucial role in reducing hospital cross infection, while having a definite structure in the management of infected cancer patients and infection-free cancer patients will reduce the limitations of available health workers, despite the stress toll. According to Shen Wu et al. [25], Li et al. [26], and Yao et al. [27], continuous provision of radiotherapy care has been the centre-point in cancer treatment with daily treatment deliveries because interruption of the treatment course can result in inferior local control and overall survival in cancer patients during a major outbreak, hence preventing and controlling the infection is crucial for the susceptible population due to their immunocompromised systems.
Alternative cancer care management
It is important to note that dealing with the COVID-19 infection is the first line of management for infected cancer patients with the infection, in order for them to be stable, recover and return to their previous treatment regime. This should be done with scrutiny based on daily observation, according to the manifestation of different patients and, of course, with a team of required specialists. For cancer patients who have developed COVID-19 symptoms, treatment of the infection should be firstly prioritised, while further cancer therapy could be delayed. Although such decisions must not be based on very early signs of the pandemicand small reports that are published, but on individual patients [20]. Due to the unique vulnerability of cancer patients as a result of their weak immune system, it is reasonable to suspend any form of therapy until they attain asymptomatic state, due to the non-availability of evidence to support withholding or supporting the chemo-/immunotherapy; hence, the use of steroid sparing strategies as well as streamlining testing to manage immune-related adverse events will go a long way reducing the COVID-19 impact [21].
Radiotherapy management of cancer patients with COVID-19 is sensitive as well, which may vary in terms of cancer type and stage. For example, in breast cancer management, despite the fact that a radiotherapy boost may decrease loco-regional reoccurrence in breast cancer, its negligible effect on survival and the possibility of omission should be considered. Patients with non-invasive disease with no survival benefit from radiotherapy should opt for omission, while low-risk, older patients with minimal survival benefit from radiotherapy and a much higher risk of mortality from COVID-19 should as well be considered for omission. Also, for prostate cancer management during a pandemic, this includes hypo fractionation and treatment delays where necessary as the overall strategies. At this time for low risk patients, being subjected to active surveillance and returning in 6 months for prostate-specific antigen (PSA) testing is recommended. The same is done for patients with favourable intermediate risk but their return should be in 3–6 months for PSA testing repetition, while for high risk patients, a shorter delay of 2–4 months with androgen deprivation therapy,(ADT) is a recommended safe and pragmatic approach with data supports to delay radiotherapy in a post-prostatectomy salvage situation [28].
Surgery is an important foundation of cancer treatment that can neither be ignored nor underestimated, as it is the only cure chance for most patients; hence, during this COVID-19 pandemic, it is important for surgical oncologists to find a way to overcome the challenges that are on ground in terms of surgery and follow up of cancer patients, especially having insights on rules adjustment for a secure stable system of management. Restivo et al. [17] reported that 80% of 371,000 diagnosed new cases of cancer were surgery candidates; however, the number of surgeries decreased after 30 days as a result of efficient management of only emergency cases during COVID-19 pandemic. With prompt health facilities’ reorganisation and swift knowledge evolution during this period, there needs to be formulation of recommendation for adaptation as well as hospital reorganisation and screening measures for futuristic developing situations.
The fears of cancer patients
During this COVID-19 outbreak, the major risk for cancer patients is the inability to access necessary medical services from dual points which is getting to the hospital and the provision of essential medical management on their arrival [29]. In regards to the psychological effects of COVID-19 on patients, that cannot be dispelled especially due to the daily media coverage about the COVID-19. There is palpable spreading of fear among healthy individuals about being infected with the virus, which, of course, will trigger depressive psychological effect amongst cancer patients’ community, based on the vulnerability of their health conditions, if affected by the virus. In this current time, the thoughts of potential cancer patients are more oriented towards the symptoms of COVID-19, indicating that they focus less on other associated signs of cancer including lumps, rectal or bladder bleeding, etc., that would give prompts to consulting physicians. Hence, the anecdotal evidence suggests that cancer patients are starting to fear COVID-19 than the cancer itself [30].
Telemedicine as an emancipator for constant health care provision
Currently, the best way to manage cancer patients during this pandemic crisis is through telemedicine. Telecommunication has always been a key tool to salvage this present situation, especially with the prohibition of mass gatherings and the implementation of social distancing as close contact between doctors and patients is very crucial in medical practice. So, since this cannot be manifested in present reality for some patients, except those in critical conditions, through telemedicine, patients can feel a sense of comfort during this COVID-19 pandemic period. Oncologists can strategise by splitting into two teams, namely the team that will attend to severe and less severe cancer cases, and the team to attend to severe and less severe infected cancer cases. This will assist in reducing the workload, curtailing the spread of infection and ensuring the safety of non-infected cancer patients. The teams have to follow and abide by infection control measures and screening strategies based on the WHO screening guidelines, with the follow-up of cancer patients and can always make consultation including referrals based on their findings. However, this strategy is to be put in place and supervised by the hospital management, especially in terms of the financial implications of telecommunication and stable internet service, in order to avoid financially overburdening the oncologists individually. The present COVID-19 pandemic period has, in an unprecedented way, created new opportunities for telemedicine innovations to remotely assist in the monitoring of patients in health management [21]. Sim et al. [28] suggested that financial burden in the name of taxes and levies to telephone communication should be removed from systems, wherever possible, to assist in efficient service delivery. Video consultations are also helpful addition to telemedicine but the lack of this technology, especially in poor countries, should not inhibit efforts to remote monitoring by telephone.
Cancellation/suspension of health forums and research
The academic aspect of oncology can as well not be exempted, as COVID-19 pandemic has resulted in the cancellation of many international medical forums and meetings. These include Flatiron Health which was slated for March 10–12th in Washington, DC USA, Healthcare Information and Management Systems Society Conference, slated for March 9–13th in Orlando, USA, International Summit on Interventional Pharmacoeconomics, which was slated for March 25–27th in Tel Aviv, Israel, The International Papillomavirus Conference slated for March 23–27th in Barcelona, Spain, amongst several others [31], [32]. Furthermore, clinical trials and research, which require physical laboratory work sometimes, have been indefinitely suspended and these will negatively have impact on the medical community. As known, continuous research is a major frontier of oncology for oncologists to get updated and advanced in their knowledge of patient management, which is also beneficial and apparently a need for cancer patients.
Concerns for Africa and cancer research
However, since the onset of the coronavirus pandemic, there has been few to rare publications from Africa on a clinical study being carried out on how cancer patients are affected, in relation to a number of infected cancer patients, cancer type and staging, other comorbidities, sexual predilection and mortality rate with highlights. These are in addition to the challenges that the medical personnel in Africa will encounter in order to give oncologists a sense of direction to enhanced patients’ management during this global pandemic. The increase in cases, which is still inevitable, should be a wakeup call for Africa, especially the governmental bodies, as the current cancer management in Africa has poor outcomes which has resulted in the loss of a staggering amount of lives and in addition to the present COVID-19 pandemic, it is just a very overwhelming situation. It was reported that ∼57.14% out of 14 million diagnosed cancer patients died in 2012, with over a half of the diagnosed cases from Africa resulting into two-thirds of deaths, including other low and middle income regions of the world, with a projection of rise in cases by 2030. [33] Cancer is the leading cause of death in the developed world and also a major cause of morbidity and mortality in low and middle income countries [30], [34]; however, the data associated with cancer incidences and mortalities is almost non-existing from Africa (except Mauritius, France Reunion, Egypt, Morocco, Tunisia, Republic of South Africa, Cape Verde and Sao Tome and Principe) and other low and middle income regions of the world [35].
Conclusion
In order to win the fight against COVID-19 and future occurrences, enhanced teamwork is required and with the underlying reality of the health care system in Africa, negligence should be avoided. Africa, with the huge human resources, is capable of managing this pandemic and bringing it to a halt, but only with the government paying greater attention to the needs on ground and by prioritising the health sector in addition to increase spending on further medical research.
Disclosure of interest
The authors declare that they have no competing interest.
Acknowledgment
The authors wish to acknowledge the funding from Southeast University Scholarship.
References
- 1.Driggin E., Madhavan M.V., Bikdeli B., Chuich T., Laracy J., Biondi-Zoccai G. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2352–2371. doi: 10.1016/j.jacc.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X. Clinical characteristics of Coronavirus disease 2019 in China. N Engl J Med. 2020 doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Udugama B., Kadhiresan P., Kozlowski H.N., Malekjahani A., Osborne M., Li V.Y.C. Diagnosing COVID-19: the disease and tools for detection. ACS Nano. 2020 doi: 10.1021/acsnano.0c02624. [DOI] [PubMed] [Google Scholar]
- 4.Wang Y., Wang Y., Chen Y., Qin Q. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J Med Virol. 2020;92:568–576. doi: 10.1002/jmv.25748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.CDC. Centers for Disease Control and Prevention; 2020. Coronavirus Disease 2019 (COVID-19) [ https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/summary.html (accessed May 14, 2020)] [Google Scholar]
- 7.Bullock H.A., Tamin A. Centers for Disease Control and Prevention; 2020. Details on COVID-19; Public Health Image Library (PHIL) [ https://phil.cdc.gov/Details.aspx?pid=23354 (accessed May 14, 2020)] [Google Scholar]
- 8.Africa Centre for Disease Control and Prevention . African Centres for Diseases Control and Prevention-Dashboard; 2020. Coronavirus Disease 2019 (COVID-19) [ https://africacdc.org/covid-19/ (accessed June 11, 2020)] [Google Scholar]
- 9.WHO. World Health Organisation; 2020. WHO Coronavirus Disease (COVID-19) Dashboard. [ https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (accessed June 11, 2020)] [Google Scholar]
- 10.WHO. 2020. Coronavirus disease COVID-2019. [Google Scholar]
- 11.Kazeem Y. Algeria is now the epicentre of coronavirus in Africa as South Africa confirms first case. Quartz Africa. 2020 [Google Scholar]
- 12.Ebrahim S.H., Memish Z.A. COVID-19 – the role of mass gatherings. Travel Med Infect Dis. 2020 doi: 10.1016/j.tmaid.2020.101617. [101617] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Holland M., Zaloga D.J., Friderici C.S. COVID-19 Personal Protective Equipment (PPE) for the emergency physician. Vis J Emerg Med. 2020;19:100740. doi: 10.1016/j.visj.2020.100740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.NCDC. National Centre for Diseases Control; 2020. COVID-19 Nigeria. [ https://covid19.ncdc.gov.ng/report/ (accessed May 16, 2020)] [Google Scholar]
- 15.African Union . African centres for diseases control and prevention; 2020. 2019 novel Coronavirus disease outbreak: what health care workers should know. [ https://africacdc.org/download/2019-novel-coronavirus-disease-outbreak-what-health-care-workers-should-know/ (accessed May 16, 2020)] [Google Scholar]
- 16.Maishanu A.A. COVID-19: 29 health workers tested positive, recover in Jigawa – NMA. Premium Times. 2020 [Google Scholar]
- 17.Restivo.A, De Luca R., Spolverato G., Delrio P., Lorenzon L., D’Ugo D. The need of COVID-19 free hospitals to maintain cancer care. Eur J Surg Oncol. 2020;3–4 doi: 10.1016/j.ejso.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Association of Nigeria Nurses and Midwives COVID-19: 250 nurses, midwives in isolation, 85 positive. Punch. 2020 [Google Scholar]
- 19.Akintimehin O.O., Eniola A.A., Alabi O.J., Eluyela D.F., Okere W., Ozordi E. Social capital and its effect on business performance in the Nigeria informal sector. Heliyon. 2019;5:e02024. doi: 10.1016/j.heliyon.2019.e02024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.The Lancet, Oncology COVID-19: global consequences for oncology. Lancet Oncol. 2020;21:467. doi: 10.1016/S1470-2045(20)30175-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alhalabi O., Subbiah V. Managing cancer care during the COVID-19 pandemic and beyond. Trends Cancer. 2020:1–3. doi: 10.1016/j.trecan.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Porzio G., Aielli F., Verna L., Aloisi P., Guadalupi F., Cannita K. Home care for cancer patients after an earthquake: the experience of the “l’Aquila per la Vita” home care unit. J Pain Symptom Manage. 2011;42:e1–e4. doi: 10.1016/j.jpainsymman.2011.06.004. [DOI] [PubMed] [Google Scholar]
- 23.Porzio G., Cortellini A., Bruera E., Verna L., Ravoni G., Peris F. Home care for cancer patients during COVID-19 pandemic: the “double triage” protocol. J Pain Symptom Manage. 2020 doi: 10.1016/j.jpainsymman.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Corley D.A., Peek R.M. COVID-19: what should clinicians and scientists do and when? Gastroenterol. 2020 doi: 10.1053/j.gastro.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wu S., Zheng D., Liu Y., Hu D., Wei W., Han G. Radiotherapy care during a major outbreak of COVID-19 in Wuhan. Adv Radiat Oncol. 2020 doi: 10.1016/j.adro.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li P.J., Jin T., Luo D.H., Shen T., Mai D.M., Hu W.H. Effect of prolonged radiotherapy treatment time on survival outcomes after intensity-modulated radiation therapy in nasopharyngeal carcinoma. PLoS ONE. 2015;10:1–14. doi: 10.1371/journal.pone.0141332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yao J.J., Jin Y.N., Wang S.Y., Zhang F., Zhou G.Q., Zhang W.J. The detrimental effects of radiotherapy interruption on local control after concurrent chemoradiotherapy for advanced T-stage nasopharyngeal carcinoma: an observational, prospective analysis. BMC Cancer. 2018;18:1–7. doi: 10.1186/s12885-018-4495-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Simcock R., Thomas T.V., Mercy C.E., Filippi A.R., Katz M.A., Pereira I.J. COVID-19: global radiation oncology's targeted response for pandemic preparedness. Clin Transl Radiat Oncol. 2020;22:55–68. doi: 10.1016/j.ctro.2020.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang H., Zhang L. Risk of COVID-19 for patients with cancer. Lancet Oncol. 2020;21:e181. doi: 10.1016/S1470-2045(20)30149-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vrdoljak E., Sullivan R., Lawler M. Cancer and coronavirus disease 2019; how do we manage cancer optimally through a public health crisis? Eur J Cancer. 2020;132:98–99. doi: 10.1016/j.ejca.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Carolan A. Coronavirus vs. Oncology: meeting cancellations, travel restrictions, fears about drug supply chain. Cancer Lett. 2020 [ https://cancerletter.com/articles/20200304_1/ (accessed May 27, 2020)] [Google Scholar]
- 32.EMSO. 2020. Cancelled – ESMO Breast Cancer 2020. EMSO Breast Cancer-Annual Congress. [ https://www.esmo.org/meetings/past-meetings/esmo-breast-cancer-2020 (accessed May 27, 2020)] [Google Scholar]
- 33.Dent J., Manner C.K., Milner D., Mutebi M., Ng A., Olopade O.I. 2017. Africa's emerging cancer crisis: a call to action. [Google Scholar]
- 34.International Agency for Research on Cancer-WHO. Data & Methods. Cancer Today; 2020. https://gco.iarc.fr/today/data-sources-methods. (accessed May 27, 2020).
- 35.International Agency for Research on Cancer-WHO. Cancer incidence and mortality data: sources and methods by country. Cancer Today; 2020. https://gco.iarc.fr/today/data-sources-methods#title-inc. (accessed May 27, 2020).