Abstract
Objective
To evaluate the correlation between meniscal extrusion in the coronal plane with clinical and radiological outcomes at a minimum of 1 year after transtibial pullout fixation for medial meniscus posterior root tear (MMPRT).
Methods
Data from 30 patients (five males, 25 females) with MMPRT who underwent arthroscopic root fixation by the transtibial pullout technique between 2011 and January 2015 were retrospectively analyzed. The mean patient age was 60.7 ± 8.3years. The median time between injury and surgery was 3.8 months (range, 0.5–15 months). Medial meniscus radial displacement was assessed on magnetic resonance imaging performed preoperatively and at 1 year after fixation. The patients were divided into two groups based on the presence on magnetic resonance imaging of decreased meniscal extrusion (group A) or increased meniscal extrusion (group B) at 1 year postoperatively compared with preoperatively. The two groups were compared regarding factors including age at surgery, sex, body mass index, time between injury and surgery, and the Lysholm score and Kellgren-Lawrence (K-L) grade preoperatively and at 1 year postoperatively.
Results
There were seven knees in group A, and 23 in group B. Both groups had a significantly improved Lysholm score postoperatively compared with preoperatively (p < 0.001). Although the postoperative K-L grade was significantly worse than the preoperative K-L grade in group B (p < 0.001), the postoperative K-L grade did not worsen postoperatively in group A.
Conclusion
The K-L grade did not worsen postoperatively in the group with decreased meniscal extrusion at 1 year after transtibial pullout fixation for MMPRT compared with preoperatively.
Introduction
The anterior and posterior meniscus roots anchor the medial and lateral menisci to the tibial plateau, allowing the menisci to disperse axial loads into hoop stresses.1,2 Medial meniscus posterior root tear (MMPRT) is defined as an avulsion injury or radial tear occurring in the posterior bony attachment.3 Detachment of the posterior root completely disrupts the continuity of the circumferential fibers, leading to loss of hoop tension, loss of load-sharing ability, and unacceptably high peak pressures. It has been shown that a MMPRT has the same consequences as total meniscectomy, and that the resulting pathological loads lead to degenerative arthritis.4, 5, 6
The shift toward meniscal preservation in cases with meniscal root tears has led to the development of various techniques.7 The transtibial pullout repair technique for MMPRT strives to restore meniscal function, and has been biomechanically validated to restore tibiofemoral joint contact mechanics.8,9 Fixation of a MMPRT can restore meniscal hoop tension and slow the progression of arthritis.10, 11, 12
In knees with MMPRT, there is a consistent magnetic resonance imaging (MRI) finding of extrusion of a greater proportion of the meniscus than its width at the central tibial plateau.13 Additionally, it has been shown that greater meniscal extrusion is a significant predictor of the progression of arthritic changes in osteoarthritic knees.14 This suggests that the elimination or reduction of meniscal extrusion indicates that the MMPRT has been successfully repaired, and that the chance of subsequent degenerative arthritis will be reduced. However, few reports have investigated the correlation between meniscal extrusion and the quality of the outcome of MMPRT fixation.10
The current study aimed to determine the correlation between meniscal extrusion in the coronal plane with clinical and radiological outcomes at a minimum of 1 year after transtibial pullout fixation for MMPRT.
Materials and methods
All patients who underwent arthroscopic root fixation by the transtibial pullout technique for a MMPRT between 2011 and January 2015 and had been followed up for more than 1 year were enrolled. MMPRT was defined as a complete radial tear within 10 mm of the posterior bony attachment of the medial meniscus. There was no history of injury in all cases. The presence of two or more of the following signs on preoperative 1.5-T MRI (ECHELON, Hitachi Medical Systems, Tokyo, Japan) was considered as confirmation of a MMPRT: the absence of an identifiable meniscus or a high signal that replaced the normal dark meniscal signal in the sagittal view, a vertical linear defect at the meniscal root on the coronal view, or a radial linear defect at the posterior insertion on the axial view.15 The exclusion criteria were: (1) partial meniscectomy, (2) osteotomy or a Kellgren-Lawrence (K-L) grade of 2 or more, (3) concomitant ligament injury, and (4) a follow-up period of less than 1 year. The final study population included five males and 25 females. The mean patient age was 60.7 ± 8.3 years. The average time period between injury and surgery was 3.8 months (range, 0.5–15 months). The current study was approved by the institutional review board of Zensyukai Hospital (approval no. 2019010902).
Radiographic assessment
Anteroposterior weight-bearing radiographs of the knee were acquired with each patient in standing position with the knee fully extended. Knee radiographs were read using the K-L scale by a single experienced orthopedist who was blinded to each patient’s clinical status. The global radiographic severity of osteoarthritic changes was assessed using the K-L system as grade 0 (normal with no osteophytes), grade 1 (possible osteophytes), grade 2 (definite osteophytes and possible joint space narrowing), grade 3 (moderate/multiple osteophytes and definite joint space narrowing, some sclerosis, and possible attrition), or grade 4 (large osteophytes, marked joint space narrowing, severe sclerosis, and definite attrition).16,17 The femorotibial angle (FTA) was also measured.
Magnetic resonance imaging assessment
Medial meniscus radial displacement (MRD) (in mm) was defined as the amount of meniscal displacement from the superomedial aspect of the tibial plateau to the periphery of the meniscal body at the level of the medial collateral ligament in the coronal plane.18 Meniscal extrusion was assessed on MRI preoperatively, and reassessed on follow-up MRI performed 3 months and 1 year after fixation (Fig. 1).
Fig. 1.
Magnetic resonance image of the knee at the level of the medial collateral ligament in the coronal plane.
The ends of the sutures were then pulled through the tibial tunnel, followed by reduction and stabilization of the meniscus. The suture ends were tied over DSP placed on the anteromedial cortex of the proximal tibia, with 30
N of traction applied.
Surgical procedure
A Knee Scorpion (Arthrex, Naples, Florida) was loaded with 2–0 FiberWire® (Arthrex, Naples, Florida). The tip of the Knee Scorpion was inserted vertically at a location 3–5 mm medial to the torn edge of the detached portion of the meniscus. The 2-0 FiberWire was advanced through the meniscus, forming a simple cinch-loop suture.19,20 The same technique was used to place one or two more strands positioned 3–5 mm apart. A tibial tunnel was then created using an anterior cruciate ligament reconstruction tibial tunnel guide (Smith & Nephew Endoscopy, Andover, Massachusetts) with its tip in contact with the insertion site of the posterior root of the medial meniscus. The ends of the sutures were then pulled through the tibial tunnel, and the meniscus was reduced and stabilized (Fig. 2). The suture ends were tied over DSP (Smith & Nephew Endoscopy, Andover, Massachusetts) that had been placed on the anteromedial cortex of the proximal tibia, with 30 N of traction applied (Fig. 3).
Fig. 2.
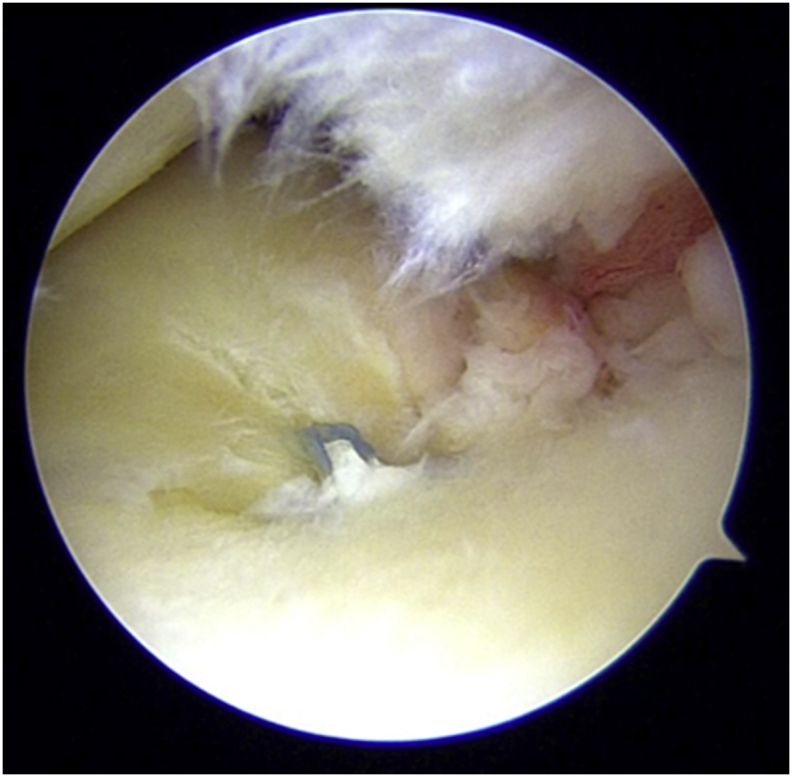
Intraoperative photograph showing the displacement of the medial meniscus.
The medial radial displacement was defined as the amount of meniscal displacement from the superomedial aspect of the tibial plateau to the periphery of the meniscal body at the level of the medial collateral ligament in the coronal plane.
Fig. 3.

Anteroposterior radiograph of the knee after transtibial pullout fixation of a medial meniscus posterior root tear.
The 2-0 FiberWire was advanced through the meniscus, forming a simple cinch-loop suture.
Postoperative rehabilitation
After surgery, an extension brace was applied. Patients were restricted to limited flexion and non-weight-bearing movements for 4 weeks postoperatively. The patients were then permitted to perform weight-bearing movements, as tolerated, and commenced physical therapy.
Postoperative evaluation
All patients underwent a clinical examination at 1 year postoperatively (range, 11.7–13.8 months). The Lysholm score and the Tegner activity score were determined.21
Intraoperative evaluation
The presence of concomitant cartilage injury of the medial femoral condyle and medial tibial plateau was evaluated using the International Cartilage Research Society grade.22 The number of sutures at the medial meniscus was also evaluated.
Statistical analysis
The patients were categorized into two groups based on whether the amount of meniscal extrusion on follow-up MRI was decreased (group A) or increased (group B) compared with preoperatively. The differences between groups A and B were evaluated using the Mann-Whitney test to compare continuous variables and other numerical values. The chi-squared test was used to compare categorical data. The Wilcoxon signed-rank test was used to compare the preoperative results with the final results within each group. All statistical analyses were conducted using the IBM SPSS Statistics 22 software program (IBM Japan, Ltd., Tokyo, Japan), and the critical value for significance was set at p < 0.05.
The intraobserver agreements were analyzed using kappa statistics. The intraobserver intraclass correlation coefficient (ICC) was 0.929 (p < 0.001) for the measurement of the MRD.
Results
The characteristics of the patients are presented in Table 1. Compared with group B, group A had a significantly greater proportion of males (p < 0.001), and a significantly greater preoperative MRD (p < 0.001). There were no significant differences between the two groups in the preoperative TAS. There were no significant differences between the two groups in the intraoperative findings (Table 2) or postoperative clinical and radiological outcomes (Table 3).
Table 1.
Preoperative demographics, clinical findings, and radiological findings.
| Group A (n = 7) | Group B (n = 23) | p value | |
|---|---|---|---|
| Sex (male/female) | 4/3 | 1/22 | 0.001 |
| Age (years) | 59.3 ± 7.9 | 61.5 ± 8.5 | 0.54 |
| BMI (kg/m2) | 26.7 ± 3.5 | 25.2 ± 3.6 | 0.32 |
| TBIS (months) | 3.5 ± 1.5 | 4.0 ± 3.2 | 0.63 |
| Preoperative TAS | 3.1 ± 1.8 | 3.1 ± 1.2 | 0.62 |
| Preoperative Lysholm score | 51.2 ± 22.2 | 48.8 ± 19.8 | 0.81 |
| Preoperative K-L grade (0/1/2) | 5/2/0 | 8/15/0 | 0.19 |
| Preoperative FTA (degree) | 177.9 ± 2.3 | 177.8 ± 2.1 | 0.94 |
| Preoperative MRD (mm) | 4.8 ± 1.0 | 3.6 ± 0.8 | 0.003 |
Group A: patients with decreased meniscal extrusion at 1 year after transtibial fixation of a medial meniscus posterior root tear compared with preoperatively, Group B: patients with increased meniscal extrusion at 1 year after transtibial fixation of a medial meniscus posterior root tear compared with preoperatively, BMI: body mass index, TAS: Tegner Activity Scale, TBIS: time period between injury and surgery, K-L: Kellgren-Lawrence, MRD: medial meniscus radial displacement.
Table 2.
Intraoperative findings.
| Group A (n = 7) | Group B (n = 23) | p value | |
|---|---|---|---|
| MFC cartilage injury, ICRS grade 0/1/2/3 |
1/2/3/1 | 1/7/11/4 | 0.84 |
| MTP cartilage injury, ICRS grade0/1/2/3 |
2/2/3/0 | 2/12/9/0 | 0.33 |
| Number of sutures at the medial meniscus | 1.1 ± 0.4 | 1.3 ± 0.5 | 0.53 |
Group A: patients with decreased meniscal extrusion at 1 year after transtibial fixation of a medial meniscus posterior root tear compared with preoperatively, Group B: patients with increased meniscal extrusion at 1 year after transtibial fixation of a medial meniscus posterior root tear compared with preoperatively, MFC: medial femoral condyle, MTP medial tibial plateau, ICRS: International Cartilage Research Society.
Table 3.
Postoperative clinical and radiological outcomes.
| Group A (n = 7) | Group B (n = 23) | p value | |
|---|---|---|---|
| Postoperative TAS | 3.3 ± 1.8 | 3.0 ± 1.2 | 0.33 |
| Postoperative Lysholm score | 81.8 ± 21.7 | 84.6 ± 15.2 | 0.73 |
| Postoperative K-L grade (0/1/2) | 5/1/1 | 6/5/12 | 0.08 |
| Postoperative FTA | 178.0 ± 1.7 | 178.6 ± 2.1 | 0.73 |
| Postoperative MRD at 3 month (mm) | 3.9 ± 1.1 | 4.4 ± 1.2 | 0.39 |
| Postoperative MRD (mm) | 4.3 ± 1.3 | 5.3 ± 5.3 | 0.09 |
Group A: patients with decreased meniscal extrusion at 1 year after transtibial fixation of a medial meniscus posterior root tear compared with preoperatively, Group B: patients with increased meniscal extrusion at 1 year after transtibial fixation of a medial meniscus posterior root tear compared with preoperatively, TAS: Tegner Activity Scale, K-L: Kellgren-Lawrence, MRD: medial meniscus radial displacement.
The postoperative Lysholm score was significantly improved compared with the preoperative Lysholm score in both group A and group B (p < 0.001). Although the postoperative K-L grade was significantly worse than the preoperative K-L grade in group B (p < 0.001), the K-L grade did not worsen postoperatively in group A (Table 4).
Table 4.
Pre-versus postoperative clinical and radiological outcomes within each group.
| Group A (n = 7) |
Group B (n = 23) |
|||||
|---|---|---|---|---|---|---|
| Preoperative | Postoperative | p value | Preoperative | Postoperative | p value | |
| TAS | 3.1 ± 1.8 | 3.3 ± 1.8 | 0.36 | 3.1 ± 1.2 | 3.0 ± 1.2 | 0.33 |
| Lysholm score | 51.2 ± 22.2 | 81.8 ± 21.7 | 0.001 | 48.8 ± 19.8 | 84.6 ± 15.2 | 0.001 |
| K-L grade (0/1/2) | 5/2/0 | 5/1/1 | 0.3 | 8/15/0 | 6/5/12 | 0.001 |
| MRD (mm) | 4.8 ± 1.0 | 4.3 ± 1.3 | 0.09 | 3.6 ± 0.8 | 5.3 ± 5.3 | 0.001 |
Group A: patients with decreased meniscal extrusion at 1 year after transtibial fixation of a medial meniscus posterior root tear compared with preoperatively, Group B: patients with increased meniscal extrusion at 1 year after transtibial fixation of a medial meniscus posterior root tear compared with preoperatively, TAS: Tegner Activity Scale, K-L: Kellgren-Lawrence, MRD: medial radial displacement.
Discussion
The major finding of the present study was that the postoperative K-L grade did not worsen in the group with decreased meniscal extrusion at 1 year after transtibial pullout fixation for MMPRT.
Chung et al.10 evaluated pullout fixation of MMPRT and reported that patients with decreased meniscal extrusion at 1 year postoperatively have more favorable clinical scores at midterm follow-up than those with increased meniscal extrusion at 1 year postoperatively. In the present study, the Lysholm score and the Tegner activity score did not significantly differ between the two groups. However, within each group, the postoperative Lysholm score was significantly improved compared with the preoperative Lysholm score.
There are a few reports of radiographic outcome after transtibial pullout fixation for MMPRT. Chung et al.10 showed that patients with decreased meniscal extrusion at 1 year postoperatively have more favorable radiographic findings (K-L grade) than those with increased meniscal extrusion at 1 year postoperatively. In contrast, the present study showed that the radiographic findings did not significantly differ between the two groups. However, the postoperative K-L grade was significantly worse than the preoperative K-L grade in the group with increased meniscal extrusion at 1 year postoperatively.
Greater meniscal extrusion is reportedly a significant predictor of the progression of arthritic changes in osteoarthritic knees.14 In the present study, the postoperative K-L grade was not worse than the preoperative K-L grade in the group with decreased meniscal extrusion at 1 year postoperatively. It has been suggested that the progression of arthritic changes can be prevented by preventing meniscal extrusion via the performance of transtibial pullout fixation for MMPRT.10 However, meniscal extrusion had progressed at 1 year postoperatively in 76% of the present cases. In the future, it may be necessary to improve the transtibial pullout fixation procedure by performing techniques such as supplementary suturing.23
The current study had several limitations that should be considered when interpreting the results. First, with respect to the items for which no significant differences were detected, it is possible that such differences were not detected statistically due to low power. Second, the follow-up period was 1 year. Future studies should also include more patients and a longer follow-up period. Third, it was a nonrandomized retrospective study. Forth, we only measured the meniscal displacement at the level of the medial collateral ligament. Fifth, the actual restoration of hoop tension and the healing status of the fixed root were not assessed, as second-look arthroscopy was not performed. Sixth, MRI was not performed immediately after surgical repair. Therefore, we could not evaluate whether the meniscus had been completely reduced. Seventh, the average age of patients in our study was already 60, it might have been acceptable to select other treatment methods such as total knee replacement.
Conclusion
The pullout technique produces favorable outcomes in the treatment of MMPRT, regardless of the resultant meniscal extrusion associated with the repair. The postoperative K-L grade was not worse than the preoperative grade in the group with decreased meniscal extrusion at 1 year after transtibial pullout fixation for MMPRT.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors declare no conflicts of interest in association with the present study.
Acknowledgments
We thank Kelly Zammit, BVSc, from Edanz Editing (www.edanzediting.com/ac), for editing a draft of this manuscript.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.asmart.2020.05.001.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Johannsen A.M., Civitarese D.M., Padalecki J.R., Goldsmith M.T., Wijdicks C.A., LaPrade R.F. Qualitative and quantitative anatomic analysis of the posterior root attachments of the medial and lateral menisci. Am J Sports Med. 2012;40:2342–2347. doi: 10.1177/0363546512457642. [DOI] [PubMed] [Google Scholar]
- 2.Kidron A., Thein R. Radial tears associated with cleavage tears of the medial meniscus in athletes. Arthroscopy. 2002;18(3):254–256. doi: 10.1053/jars.2002.30650. [DOI] [PubMed] [Google Scholar]
- 3.Bhatia S., LaPrade C.M., Ellman M.B., LaPrade R.F. Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med. 2014;42:3016–3030. doi: 10.1177/0363546514524162. [DOI] [PubMed] [Google Scholar]
- 4.Allaire R., Muriuki M., Gilbertson L., Harner C.D. Biomechanical consequences of a tear of the posterior root of the medial meniscus: similar to total meniscectomy. J Bone Joint Surg Am. 2008;90:1922–1931. doi: 10.2106/JBJS.G.00748. [DOI] [PubMed] [Google Scholar]
- 5.LaPrade C.M., Jansson K.S., Dorman G., Smith S.D., Wijdicks C.A., LaPrade R.F. Altered tibiofemoral contact mechanics due to lateral meniscus posterior horn root avulsions and radial tears can be restored with in situ pull-out suture repairs. J Bone Joint Surg Am. 2014;96(6):471–479. doi: 10.2106/JBJS.L.01252. [DOI] [PubMed] [Google Scholar]
- 6.Marzo J.M., Gurske-DePerio J. Effects of medial meniscus posterior horn avulsion and repair on tibiofemoral contact area and peak contact pressure with clinical implications. Am J Sports Med. 2009;37(1):124–129. doi: 10.1177/0363546508323254. [DOI] [PubMed] [Google Scholar]
- 7.LaPrade R.F., LaPrade C.M., James E.W. Recent advances in posterior meniscal root repair techniques. J Am Acad Orthop Surg. 2015;23(2):71–76. doi: 10.5435/JAAOS-D-14-00003. [DOI] [PubMed] [Google Scholar]
- 8.Padalecki J.R., Jansson K.S., Smith S.D. Biomechanical consequences of a complete radial tear adjacent to the medial meniscus posterior root attachment site: in-situ pullout repair restores derangement of joint mechanics. Am J Sports Med. 2014;42(3):699–707. doi: 10.1177/0363546513499314. [DOI] [PubMed] [Google Scholar]
- 9.LaPrade R.F., Matheny L.M., Moulton S.G., James E.W., Dean C.S. Posterior meniscal root repairs: outcomes of an anatomic transtibial pull-out technique. Am J Sports Med. 2017;45:884–891. doi: 10.1177/0363546516673996. [DOI] [PubMed] [Google Scholar]
- 10.Chung K.S., Ha J.K., Ra H.J., Nam G.W., Kim J.G. Pullout fixation of posterior medial meniscus root tears: correlation between meniscus extrusion and midterm clinical results. Am J Sports Med. 2017 Jan;45(1):42–49. doi: 10.1177/0363546516662445. [DOI] [PubMed] [Google Scholar]
- 11.Kim S.B., Ha J.K., Lee S.W. Medial meniscus root tear refixation: comparison of clinical, radiologic, and arthroscopic findings with medial meniscectomy. Arthroscopy. 2011;27:346–354. doi: 10.1016/j.arthro.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 12.Lee D.W., Ha J.K., Kim J.G. Medial meniscus posterior root tear: a comprehensive review. Knee Surg Relat Res. 2014;26:125–134. doi: 10.5792/ksrr.2014.26.3.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Park H.J., Kim S.S., Lee S.Y. Medial meniscal root tears and meniscal extrusion transverse length ratios on MRI. Br J Radiol. 2012;85:e1032–e1037. doi: 10.1259/bjr/26261821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Emmanuel K., Quinn E., Niu J. Quantitative measures of meniscus extrusion predict incident radiographic knee osteoarthritis: data from the Osteoarthritis Initiative. Osteoarthritis Cartilage. 2016;24:262–269. doi: 10.1016/j.joca.2015.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee Y.G., Shim J.C., Choi Y.S., Kim J.G., Lee G.J., Kim H.K. Magnetic resonance imaging findings of surgically proven medial meniscus root tear: tear configuration and associated knee abnormalities. J Comput Assist Tomogr. 2008;32:452–457. doi: 10.1097/RCT.0b013e31812f4eb0. [DOI] [PubMed] [Google Scholar]
- 16.Kellgren J.H., Lawrence J.S. Blackwell Scientific; Oxford: 1963. The Epidemiology of Chronic Rheumatism: Atlas of Standard Radiographs of Arthritis. [Google Scholar]
- 17.Kellgren J.H., Lawrence J.S. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lerer D.B., Umans H.R., Hu M.X., Jones M.H. The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skeletal Radiol. 2004;33:569–574. doi: 10.1007/s00256-004-0761-2. [DOI] [PubMed] [Google Scholar]
- 19.Krych A.J., Johnson N.R., Wu I.T., Smith P.A., Stuart M.J. A simple cinch is superior to a locking loop for meniscus root repair: a human biomechanical comparison of suture constructs in a transtibial pull-out model. Knee Surg Sports Traumatol Arthrosc. 2018;26(8):2239–2244. doi: 10.1007/s00167-017-4652-1. [DOI] [PubMed] [Google Scholar]
- 20.Smith P.A., Bley J.A. Simplified arthroscopic lateral meniscal root repair involving the use of 2 cinch-loop sutures. Arthrosc Tech. 2017;6(1):e73–e79. doi: 10.1016/j.eats.2016.09.002. 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tegner Y., Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]
- 22.Brittberg M., Winalski C.S. Evaluation of cartilage injuries and repair. J Bone Joint Surg Am. 2003;85-A(Suppl 2):58–69. doi: 10.2106/00004623-200300002-00008. [DOI] [PubMed] [Google Scholar]
- 23.Koga H., Watanabe T., Horie M. Augmentation of the pullout repair of a medial meniscus posterior root tear by arthroscopic centralization. Arthrosc Tech. 2017 Aug 21;6(4):e1335–e1339. doi: 10.1016/j.eats.2017.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.



