Abstract
Objective
This retrospective case series describes a hybrid fixation technique and determines the clinical outcomes, knee function, and activity level of patients at short-term follow-up.
Design
Seventeen patients (18 knees) with unstable osteochondritis dissecans (OCD) lesions involving the knee were treated with a hybrid fixation technique in which the salvageable fragment was fixed and osteochondral autograft transplantation system (OATS) was used for the unsalvageable fragment. Thirteen lesions involved the medial femoral condyle, 4 involved the lateral femoral condyle, and 1 involved the patella. Mean patient age was 17 years (range 12-28 years). All lesions were International Cartilage Repair Society (ICRS) grade III or IV. The patients were prospectively followed postoperatively. Outcome measures included the International Knee Documentation Committee (IKDC) score, Knee injury and Osteoarthritis Outcome Score (KOOS), and the Tegner activity scale.
Results
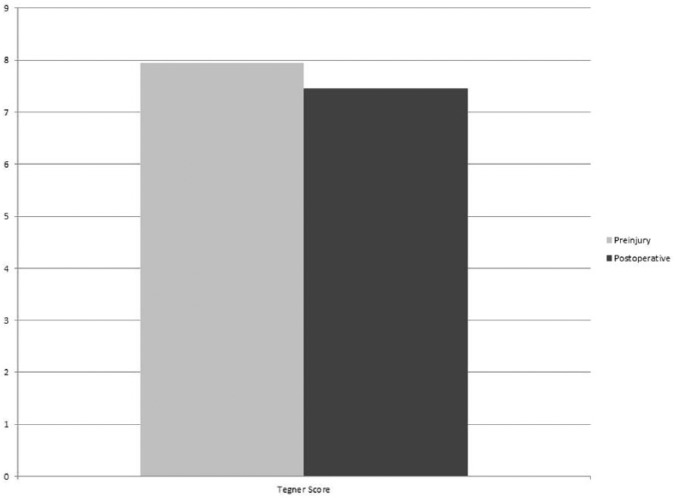
At mean follow-up of 36 months (range 24-67.2 months), the mean postoperative KOOS scores, given as mean (SD), were as follows: Quality of Life (QoL) 91.1 (17.0), Activities of Daily Living (ADL) 99.5 (1.5), Sport 94.5 (11.2), Pain 97.4 (5.8), and Symptoms 95.9 (6.5). Mean IKDC score was 96.2 (7.0). There was no significant difference between mean preinjury (7.95, SD = 1.1) and mean postoperative (7.45, SD = 1.5) Tegner scores (P = 0.363). The mean Magnetic Resonance Observation of Cartilage Repair Tissue (MOCART) score was 87.5 at a mean 7.8 months (range 3-18 months) postoperation. There were no reported complications.
Conclusion
The results of this case series suggest that patients with partially salvageable OCD lesions involving the knee can have positive short-term outcomes and can expect a low complication rate when treated with a hybrid technique of fixation with osteochondral autograft transfer.
Keywords: osteochondritis dissecans, unstable, cartilage repair, knee pain
Introduction
Osteochondritis dissecans (OCD) of the knee can cause significant pain and disability in both skeletally immature and mature patients.1 These lesions are characterized by an osteochondral fragment that is no longer fixed to its osseous and cartilaginous surroundings. This may lead to an unstable fragment that becomes necrotic due to lack of local blood supply.2,3 Operative management is frequently needed to treat symptomatic lesions that have failed conservative management.
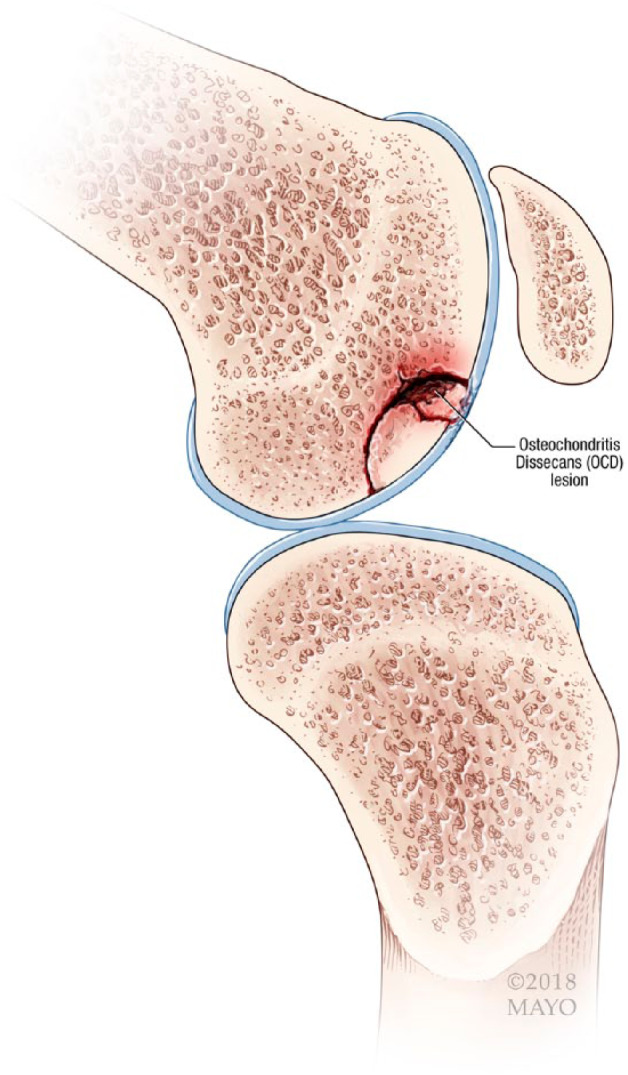
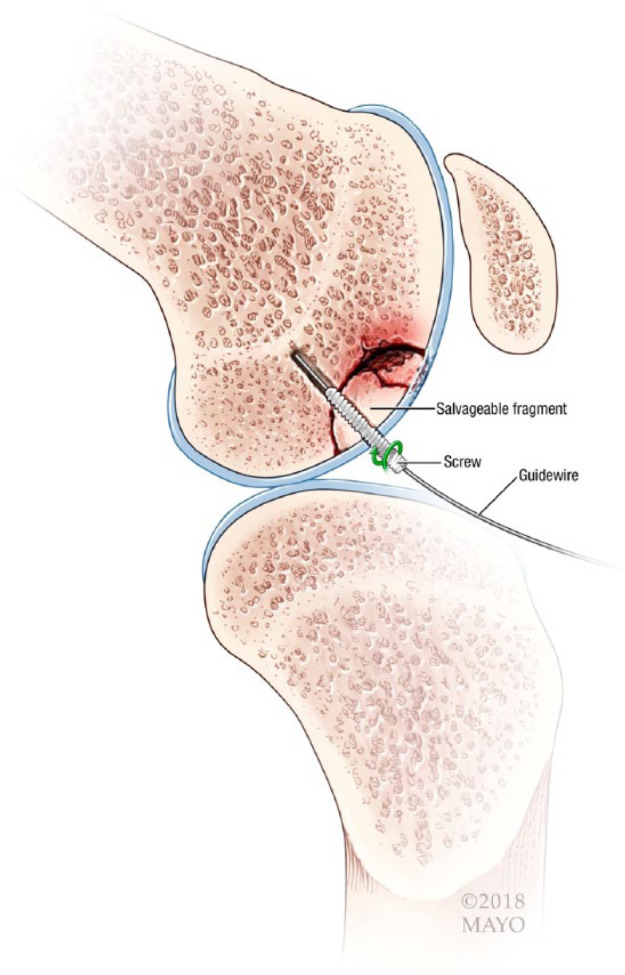
When approaching an unstable lesion at the time of surgery, the progeny fragment is determined to be salvageable—good bone for fixation and intact overlying articular cartilage, or unsalvageable—fragmented bone or damaged overlying articular cartilage. A salvageable fragment can be fixed with compression screws.4,5 An unsalvageable fragment can be excised, but restoration of the bone and cartilage leads to better long-term results with less risk of arthritis.6 Many surgical techniques have been described, but consensus on ideal surgical treatment techniques are lacking. Isolated use of mosaicplasty has been shown to produce good outcomes,7-9 but is only indicated when the entire OCD fragment is unsalvageable, and concerns over donor site morbidity with multiple donor plugs remains.10 Corticocancellous bone pegs have been associated with a high rate of loosening.11,12 Fixation of the OCD fragment using mosaicplasty has also been described with quality mid-term13 and long-term14 outcomes, but this may cause unnecessary disruption of the salvageable progeny fragment. In a small retrospective study of 7 patients, biologic fixation to completely salvage the fragment was shown to produce quality outcomes at minimum 7-month follow-up.10 To our knowledge, there is a lack of longer term data evaluating the mid-term outcomes of patients with unstable OCD lesions treated with hybrid fixation to partially salvage the progeny fragment.
Therefore, the purpose of this retrospective case series study was to describe a hybrid fixation surgical technique to treat unstable OCD lesions of the knee and to analyze patient reported outcomes, knee function, and activity level of patients at short-term follow-up. It was hypothesized that the use of a hybrid fixation surgical technique for the treatment of unstable OCD lesions of the knee would result in good clinical outcomes and few complications at short-term follow-up.
Methods
Experienced surgeons performed all procedures at the Mayo Clinic, Rochester, Minnesota, and Osaka University Hospital, Osaka, Japan. All patients undergoing cartilage restoration procedures were included in a registry. The institutional review board (IRB ID No. 15-000601) at both centers approved the study. Informed consent was obtained from all study participants. All patients were evaluated preoperatively and postoperatively at minimum 2 years.
Inclusion Criteria
Patients were included in the study if they had (1) an unstable osteochondritis dissecans lesion involving the medial condyle or lateral condyle of the femur diagnosed by magnetic resonance imaging (MRI), (2) a surgical procedure using the novel hybrid fixation technique for treatment, and (3) a minimum 2-year follow-up. Patients were excluded if they had (1) an OCD lesion with no salvageable fragment, (2) an OCD lesion that was entirely salvageable, or (3) uncorrected malalignment, meniscal deficiency or ligament instability. Given the symptomatic and unstable, yet potentially salvageable, nature of the OCD lesions in this study, an attempt at nonoperative management was in many cases not attempted.
Patients
Seventeen patients (18 knees) with unstable OCD lesions of the knee who were treated with a hybrid fixation technique between the years 2002 to 2015 were included in the study (Table 1). All patients except 1 was male and 12 involved the left knee. The average patient age at time of surgery was 17 years (range 12-28 years) and the average body mass index was 23.8 kg/m2 (range 21-32 kg/m2). Four of the knees were skeletally immature. Thirteen of the lesions were located on the medial femoral condyle (MFC), 3 on the lateral femoral condyle (LFC), 1 on the patella, and 1 consisted of a “kissing lesion” with an OCD lesion on the LFC and a grade 3 chondral lesion on the lateral tibial plateau. The tibial lesion was treated with chondroplasty. Only 1 patient had undergone a previous surgical procedure for treatment of the lesion, which consisted of arthroscopy and retrograde drilling. Additionally, only 2 patients underwent concurrent procedures consisting of a tibial chondroplasty and a partial lateral meniscectomy.
Table 1.
Patient Characteristics.
| Characteristic | Patient Knees (n = 18) |
|---|---|
| Age, years, mean (range) | 17 (12-28) |
| Sex, n, male:female | 17:1 |
| Body mass index, kg/m2, mean (range) | 23.8 (21-32) |
| Laterality, n, left:right | 12:6 |
| Lesion location, n, (MFC:LFC:patella) | 13:4:1 |
| Defect size, cm2, mean (range) | 2.8 (0.8-6.25) |
| Open physis, n, (yes:no) | 4:14 |
MFC = medial femoral condyle; LFC = lateral femoral condyle.
Surgical Technique
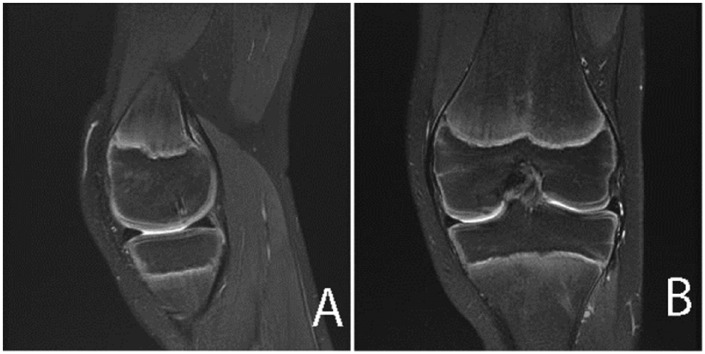
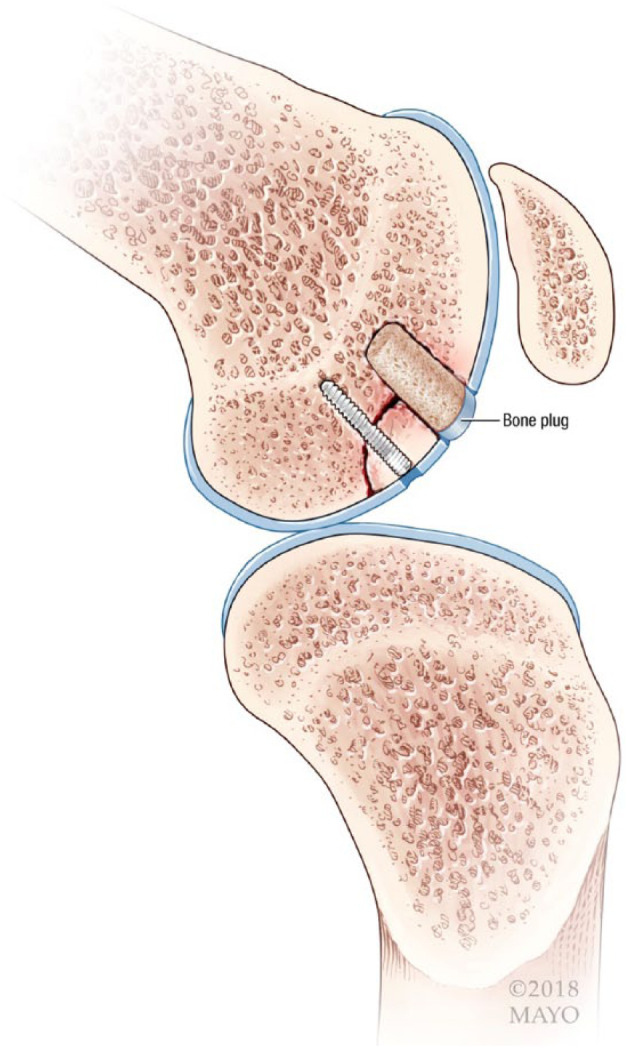
All operations were performed by surgeons with extensive experience performing cartilage restoration procedures (AJK, BAL, YT, SH, and NN). Each procedure began with a diagnostic arthroscopy to further characterize the OCD lesion and identify associated pathology. A mini-medial parapatellar incision was made by extending the previously made anteromedial arthroscopy portal. For lesions involving the LFC, the incision was made laterally. Although all arthroscopic management of unstable OCD lesions has been described,13 a mini-open technique was used in all instances for improved fixation visualization. The knee was then flexed to 90° in order to visualize the lesion (Fig. 1). The OCD lesions were further examined, and it was determined based on the quality of the cartilage and subchondral bone whether they were salvageable. Non-viable bone, cartilage, and fibrous tissue were debrided. The salvageable fragment was stabilized using a Kirschner wire and then BioCompression screws were used for fixation of the fragment to the underlying bone (Fig. 2). In some cases, fixation was achieved using a GRAND FIX pin (Gunze Ltd, Japan). This device is made from poly-l-lactic acid and is absorbable. The unsalvageable portion was completely debrided (Fig. 3) and filled using an osteochondral autograft transplantation system (OATS) technique (Fig. 4). The autograft was typically harvested from the superolateral trochlea of the femur. The tourniquet was deflated and the wounds were closed. The above technique is similar to fixation techniques that have been described in the literature.15,16
Figure 1.
Example of an unstable osteochondritis dissecans lesion with a salvageable and unsalvageable fragment.
Figure 2.
The salvageable fragment is fixated with a screw.
Figure 3.
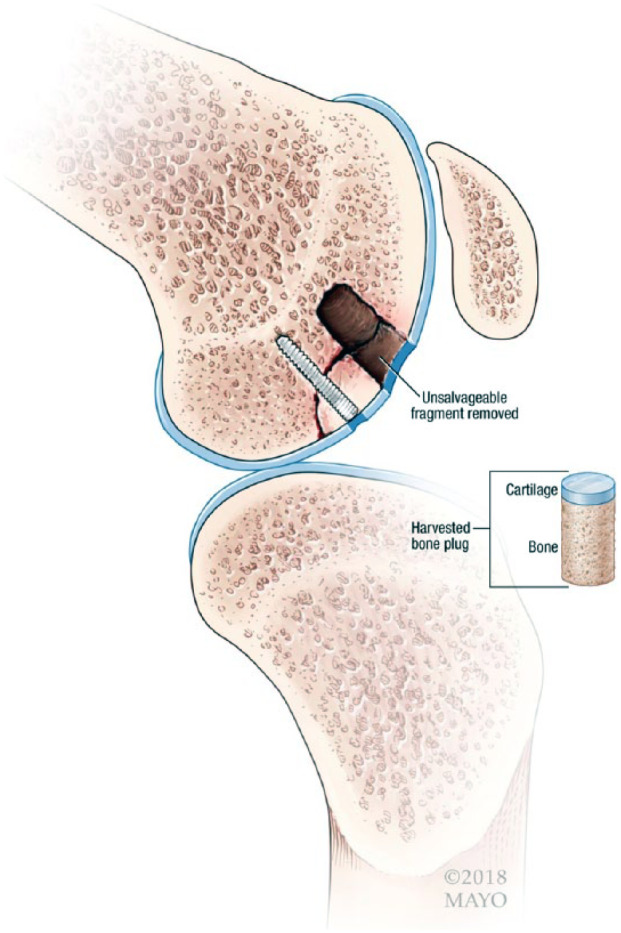
Unsalvageable portion is removed.
Figure 4.
Osteochondral autograft transplantation system (OATS) plug is used to restore the articular surface and subchondral bone from where the unsalvageable fragment was removed.
For 6 weeks postoperatively, all patients remained partially weightbearing with the knee brace locked in full extension while ambulating. When not ambulating, immediate active and passive range of motion as tolerated was encouraged. Continuous passive motion machines were used starting at 0° to 30° and advanced as tolerated. Gradual weight bearing as tolerated was allowed after 6 weeks and the brace was discontinued. Typically, patients returned to all activities by 6 months after surgery.
Outcome Measures
The Knee injury and Osteoarthritis Outcome Score (KOOS)17 Quality of Life (QoL) and Activities of Daily Living (ADL) subscales were used to assess health and well-being. KOOS has been shown to correlate with other measures of general health and well-being such as the Short Form–36 (SF-36) in patients with articular cartilage procedures.18 Knee function was assessed using the International Knee Documentation Committee (IKDC) subjective knee score19 and the KOOS Pain and Symptoms subscales. Each of these has been shown to be a valid measure of knee function following articular cartilage repair operations.20,21 The Tegner activity scale22 and KOOS Sport (Sport/Rec) subscale were used to report patient activity level and sports-related disability. The Tegner activity level was assessed preinjury and postoperatively. Reoperation and complication rates were analyzed. Healing was assessed by MRI (5 knees) by using the Magnetic Resonance Observation of Cartilage Repair Tissue (MOCART) score,23,24 second-look arthroscopy (5 knees), MRI and arthroscopy (5 knees), computed tomography scan (3 knees), or clinical examination (1 knee).
Statistical Analysis
Descriptive analyses of the patient data were performed using means and ranges. Comparisons of preoperative versus postoperative clinical scores were conducted using Wilcoxon rank-sum tests. A 2-tailed t test was used for all statistical analysis with a critical α set to 0.05. Analysis was performed using SAS Statistical Discovery JMP version 7.0 (SAS, Inc. Cary, NC).
Results
Eighteen knees (17 patients) underwent hybrid fixation of an unstable OCD lesion of the knee between the years of 2002 and 2015. All patients had OCD lesions that were graded type III or IV based on the International Cartilage Repair Society (ICRS) scale of OCD lesions.25 The mean follow-up was 36 months (range 24-67.2 months) with all patients reaching the minimum 2-years of follow up. All procedures were performed open, the salvageable fragment was stabilized with a pin, screw, or bone plug, and the unstable fragment was removed and replaced using an OATS technique (Table 2). The autograft harvest site was the superolateral trochlea in 17 knees and the superomedial trochlea in 1 patient.
Table 2.
Surgical Details.
| Patient Knees (n = 18) | |
|---|---|
| Open: Arthroscopic | 18:0 |
| Salvageable Fragment Stabilization (Bone plug: BioCompression screw: Bioabsorbable pin) | 3:5:10 |
| Mean no. of OATS plugs (range) | 1.6 (1-5) |
| Autograft harvest site (SLT:SMT) | 17:1 |
| Concomitant procedures (yes:no) | 2:16 |
OATS, osteochondral autograft transplantation site; SLT = superolateral trochlea; SMT = superomedial trochlea.
Health Outcomes and Knee Function
The mean postoperative KOOS and IKDC scores are reported in Table 3.
Table 3.
KOOS and IKDC Scores.
| Scores, Mean ± SD (Range) | |
|---|---|
| IKDC | 96.2 ± 7.0 (75.9-100) |
| KOOS | |
| QoL | 91.1 ± 17.0 (31.3-100) |
| ADL | 99.5 ± 1.5 (94.1-100) |
| Sport | 94.5 ± 11.2 (55-100) |
| Pain | 97.4 ± 5.8 (77.9-100) |
| Symptoms | 95.9 ± 6.5 (78.6-100) |
IKDC = International Knee Documentation Committee; KOOS = Knee injury and Osteoarthritis Outcome Score; QoL = Quality of Life; ADL = Activities of Daily Living.
Activity Level
All patients returned to sport. The mean postoperative KOOS Sport score was 94.5 (range 55-100). There was no significant difference between the mean preinjury (7.95; range 4-9) and mean postoperative (7.45; range 4-9) Tegner scores (P = 0.363) (Fig. 5).
Figure 5.
Preinjury and postoperative activity level.
Lesion Healing
Healing was assessed by MRI only in 5 knees, second-look arthroscopy and MRI in 5 knees, arthroscopy only in 5 knees, computed tomography scan in 3 knees, and clinically based on physical examination and rehabilitation clearance in 1 knee. The one patient in which healing was assessed clinically declined repeat imaging or arthroscopy. All were determined to be healed at a mean 5.6 months (range 4-7 months). Eight knees underwent repeat arthroscopy at a mean 5.8 months (range 4-7 months) to assess healing and 2 knees underwent planned repeat arthroscopy for screw removal at 5 months postoperatively. At that time, all lesions were stable to probing and the cartilage was completely filled (Fig. 6). The 10 knees with postoperative MRI (Fig. 7) had a mean MOCART score of 87.5 (range 75-100) and they were performed at a mean 7.8 months (range 3-18 months) postoperation. Lesions were determined to be healed on MRI if the autograft plugs were incorporated, minimal inflammation and cystic changes were present, and the articular surface was congruent. We were unable to reliably detect differences between the portions of individual lesions treated with fixation versus OATS on MRI.
Figure 6.
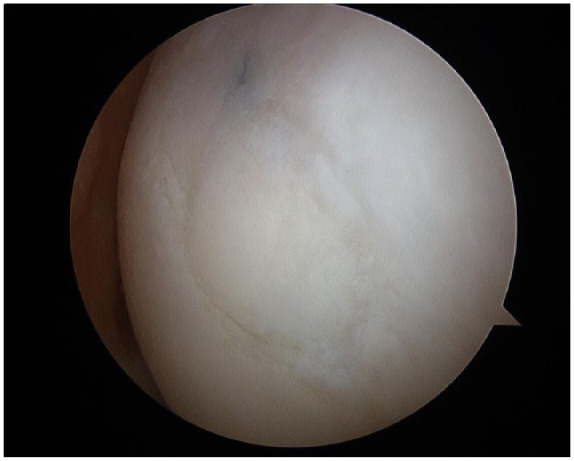
Osteochondritis dissecans lesion 5 months following treatment using the hybrid fixation technique.
Figure 7.
Magnetic resonance images demonstrating an osteochondritis dissecans lesion preoperatively (A, B), and 6 months postoperatively (C, D) following treatment with the hybrid fixation technique.
Complications
There were no reported patient complications. Two knees (1 patient) underwent planned removal of the BioCompression screw used to stabilize the salvageable fragment. Otherwise, no reoperations were performed.
One patient accounted for the low KOOS Sport (55) and KOOS QoL (31.3) scores. In this patient, repeat MRI showed their lesion to be well healed without recurrence. It should be noted that this particular patient had progressive valgus malalignment and gained a significant amount of weight postoperatively.
Discussion
The main finding in the present study was that patients with unstable OCD lesions with both salvageable and unsalvageable fragments can have positive short-term outcomes and expect few complications following surgical treatment with a hybrid fixation technique which uses fragment fixation and OATS.
The technique described has the advantage of repairing an unstable OCD lesion in one surgical stage. It is indicated for lesions that have both a salvageable and unsalvageable fragment. The salvageable fragment is fixated to underlying healthy bone and the void left by the removed unsalvageable fragment is filled with an OATS plug(s). Lintz et al.,10 and Chadli et al.26 more recently, described a “hybrid fixation” technique to stabilize the OCD fragment with both screws and OATS plugs. In this technique the entire fragment was salvageable, and the hybrid fixation was used to maintain the fixation benefits of the screw and improved revascularization benefits of the OATS plugs. Additionally, Miniaci et al.13 and Berlet et al.27 have described a technique in which the complete fragment was salvageable, and the lesion was fixated entirely with OATS plugs and no screws. In our technique, the osteochondral autograft plug is used to restore the bone and cartilage in a situation where a portion of the progeny fragment is fragmented and unsalvageable. Typically, this fragmented portion would lead to removal of the entire progeny fragment, with consideration of a second stage salvage procedure with an ACI sandwich technique28 or the use of nonnative tissue in the form of osteochondral scaffolds29 or osteochondral allograft transplant.30 One stage autologous tissue with this technique may be considered an advantage for a young patient.
In the present study, KOOS and IKDC scores were used to assess health outcomes and knee function. The mean postoperative IKDC and KOOS scores were similar to that of prior studies, which evaluated patients following surgical treatment with other various techniques that salvaged the entire fragment.4,5,10,31 The technique described in this study is indicated when the entire fragment is unstable. Osteochondral allograft transplantation (OCA) and autologous chondrocyte implantation (ACI) are also options in this scenario and have shown positive results.32-34 However, ACI requires a second stage more costly procedure with extended rehabilitation time and allograft tissue for OCA is not always readily available. We believe that it makes sense to salvage autologous tissue in one surgical stage. Another viable option is the use of osteochondral scaffolds, which allow for a single-stage procedure. Perdisa et al.29 reported mean IKDC scores of 82.2 and 90.1 at mean 2 and 5 years postoperatively, respectively, following the treatment of unstable OCD lesions with osteochondral scaffolds. These results are comparable to that of the present study. Unfortunately, this technique uses foreign material and does not preserve native tissue.
Activity level was assessed pre- and postoperatively using the Tegner activity scale. No significant difference was seen between preinjury and postoperative Tegner scores (P = 0.363). The return to preinjury activity level is consistent with that of other studies. Miniaci et al.13 reported continued improvements in activity level as rated by a visual analog scale up to 18 months postoperatively following their described surgical technique. Lintz et al.10 reported improved Hughston scores following a surgical procedure to fully salvage the progeny fragment with “hybrid fixation.” These are both very reasonable options for treatment of unstable OCD lesions but their described indications for use do not include instances in which the progeny fragment is only partially salvageable.
All knees except for one received either postoperative MRI or repeat arthroscopy. Lesion healing was adequately assessed by these measures. The 10 knees that underwent repeat arthroscopy demonstrated well healed lesions that were stable to probing. On MRI at a mean 7.8 months postoperatively, the mean MOCART score was 87.5. This mean MOCART score is slightly higher than that of a comparable study in which unstable OCD lesions were fixated with compression screws. In this study, the mean MOCART score was 72.0.35 Additionally, Perdisa et al.29 used MOCART to asses healing following the use of an osteochondral scaffold for treatment of unstable OCD lesions. They reported mean postoperative scores of 74.2 and 81.4 at 2 and 5 years, respectively.29 Although Miniaci et al.13 did not assess the lesions using the MOCART grading system, they noted healed lesions on MRI at 9 months postoperatively with only slight articular surface irregularity. Additionally, repeat arthroscopy on 2 patients showed smooth, stable lesions.13
There were no reported complications at mid-term follow up. This may be due to the small number of patients included in this study, but it does suggest that this technique can be performed safely with a low risk for postoperative sequelae. Complications reported following other OCD lesion treatment options include graft failure with matrix-induced autologous chondrocyte implantation (MACI) use (low rate),34 reoperation requiring revision with OCA,32 and screw back-out with metal screw fixation.5
The limitations of this study include the small sample size. This was due to the narrow indications for its use when both a salvageable and unsalvageable fragment make up the OCD lesion. The retrospective nature did not allow for assessment of pretreatment values and therefore true improvement cannot be assessed. Adult and juvenile OCD lesions were included. Assessment of lesion healing was heterogeneous. All patients achieved minimum 2-year follow-up, but the overall follow-up was short term. Patients were not randomized to this procedure and there was no control. Despite these limitations, this technique has not been previously described and provides a viable option for the treatment of unstable OCD lesions which have proven to be difficult to treat.
This case series introduces a surgical technique to treat unstable OCD lesions of the knee and suggests that patients can have positive short-term outcomes and expect few complications following its use. Longer term studies are needed to further compare its benefits to other reported surgical treatment options.
Footnotes
Acknowledgments and Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Bruce A. Levy receives or has received IP royalties and research support from Arthrex Inc., Biomet, Smith & Nephew, and Stryker; is a paid consultant for Arthrex, Inc. and Smith & Nephew; and is in the editorial or governing board of Arthroscopy: The Journal of Arthroscopic and Related Surgey, CORR, Journal of Knee Surgery, and Knee Surgery, Sports Traumatology, Arthroscopy. Norimasa Nakamura is a paid consultant for Biomet and Novartis; is on the board or is a committee member of the International Cartilage Repair Society and the International Society of Arthroscopy, Knee Surgery, and Orthopaedic Sports Medicine; and in on the editorial or governing board of Journal of Experimental Orthopaedics (Springer), Journal of Orthopaedic Science (Springer), and Cartilage (Sage). Aaron J. Krych receives or has received research support from Aesculap/B. Braun, Arthritis Foundation, Ceterix, and Histogenics; receives IP royalties from Arthrex Inc.; is a paid consultant for Arthrex Inc. and Vericel; is on the board or is a committee member of the International Cartilage Repair Society, International Society of Arthroscopy, Knee Surgery, and Orthopaedic Sports Medicine, Minnesota Orthopedic Society, and Musculoskeletal Transplantation Foundation; and is on the editorial or governing board of the American Journal of Sports Medicine.
Ethical Approval: The institutional review board (IRB ID No. 15-000601) at the Mayo Clinic, Rochester, Minnesota, and Osaka University Hospital, Osaka, Japan. approved the study.
Informed Consent: Written informed consent was obtained from all study participants.
Trial Registration: Not applicable.
ORCID iD: Aaron J. Krych  https://orcid.org/0000-0003-3248-8007
https://orcid.org/0000-0003-3248-8007
References
- 1. Accadbled F, Vial J, Sales de Gauzy J. Osteochondritis dissecans of the knee. Orthop Traumatol Surg Res. 2018;104(1 S):S97-105. [DOI] [PubMed] [Google Scholar]
- 2. Erickson BJ, Chalmers PN, Yanke AB, Cole BJ. Surgical management of osteochondritis dissecans of the knee. Curr Rev Musculoskelet Med. 2013;6(2):102-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Shea KG, Jacobs JC, Jr, Carey JL, Anderson AF, Oxford JT. Osteochondritis dissecans knee histology studies have variable findings and theories of etiology. Clin Orthop Relat Res. 2013;471(4):1127-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Webb JE, Lewallen LW, Christophersen C, Krych AJ, McIntosh AL. Clinical outcome of internal fixation of unstable juvenile osteochondritis dissecans lesions of the knee. Orthopedics. 2013;36(11):e1444-9. [DOI] [PubMed] [Google Scholar]
- 5. Barrett I, King AH, Riester S, van Wijnen A, Levy BA, Stuart MJ, et al. Internal fixation of unstable osteochondritis dissecans in the skeletally mature knee with metal screws. Cartilage. 2016;7(2):157-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sanders TL, Pareek A, Johnson NR, Carey JL, Maak TG, Stuart MJ, et al. Nonoperative management of osteochondritis dissecans of the knee: progression to osteoarthritis and arthroplasty at mean 13-year follow-up. Orthop J Sports Med. 2017;5(7):2325967117704644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hangody L, Vasarhelyi G, Hangody LR, Sukosd Z, Tibay G, Bartha L, et al. Autologous osteochondral grafting—technique and long-term results. Injury. 2008;39(Suppl 1):S32-9. [DOI] [PubMed] [Google Scholar]
- 8. Cognault J, Seurat O, Chaussard C, Ionescu S, Saragaglia D. Return to sports after autogenous osteochondral mosaicplasty of the femoral condyles: 25 cases at a mean follow-up of 9 years. Orthop Traumatol Surg Res. 2015;101(3):313-7. [DOI] [PubMed] [Google Scholar]
- 9. Hangody L, Dobos J, Baló E, Pánics G, Hangody LR, Berkes I. Clinical experiences with autologous osteochondral mosaicplasty in an athletic population: a 17-year prospective multicenter study. Am J Sports Med. 2010;38(6):1125-33. [DOI] [PubMed] [Google Scholar]
- 10. Lintz F, Pujol N, Pandeirada C, Boisrenoult P, Beaufils P. Hybrid fixation: evaluation of a novel technique in adult osteochondritis dissecans of the knee. Knee Surg Sports Traumatol Arthrosc. 2011;19(4):568-71. [DOI] [PubMed] [Google Scholar]
- 11. Navarro R, Cohen M, Filho MC, da Silva RT. The arthroscopic treatment of osteochondritis dissecans of the knee with autologous bone sticks. Arthroscopy. 2002;18(8):840-4. [DOI] [PubMed] [Google Scholar]
- 12. Slough JA, Noto AM, Schmidt TL. Tibial cortical bone peg fixation in osteochondritis dissecans of the knee. Clin Orthop Relat Res. 1991;(267):122-7. [PubMed] [Google Scholar]
- 13. Miniaci A, Tytherleigh-Strong G. Fixation of unstable osteochondritis dissecans lesions of the knee using arthroscopic autogenous osteochondral grafting (mosaicplasty). Arthroscopy. 2007;23(8):845-51. [DOI] [PubMed] [Google Scholar]
- 14. Ronga M, Stissi P, LA Barbera G, Valoroso M, Angeretti G, Genovese E, et al. Treatment of unstable osteochondritis dissecans in adults with autogenous osteochondral grafts (mosaicplasty): long-term results. Joints. 2016;3(4):173-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Yonetani Y, Matsuo T, Nakamura N, Natsuume T, Tanaka Y, Shiozaki Y, et al. Fixation of detached osteochondritis dissecans lesions with bioabsorbable pins: clinical and histologic evaluation. Arthroscopy. 2010;26(6):782-9. [DOI] [PubMed] [Google Scholar]
- 16. Uchida R, Toritsuka Y, Yoneda K, Hamada M, Ohzono K, Horibe S. Chondral fragment of the lateral femoral trochlea of the knee in adolescents. Knee. 2012;19(5):719-23. [DOI] [PubMed] [Google Scholar]
- 17. Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88-96. [DOI] [PubMed] [Google Scholar]
- 18. Bekkers JE, de Windt TS, Raijmakers NJ, Dhert WJ, Saris DB. Validation of the Knee Injury and Osteoarthritis Outcome Score (KOOS) for the treatment of focal cartilage lesions. Osteoarthritis Cartilage. 2009;17(11):1434-9. [DOI] [PubMed] [Google Scholar]
- 19. Irrgang JJ, Anderson AF, Boland AL, Harner CD, Neyret P, Richmond JC, et al. Responsiveness of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med. 2006;34(10):1567-73. [DOI] [PubMed] [Google Scholar]
- 20. Hambly K, Griva K. IKDC or KOOS? Which measures symptoms and disabilities most important to postoperative articular cartilage repair patients? Am J Sports Med. 2008;36(9):1695-704. [DOI] [PubMed] [Google Scholar]
- 21. Roos EM, Engelhart L, Ranstam J, Anderson AF, Irrgang JJ, Marx RG, et al. ICRS Recommendation Document: patient-reported outcome instruments for use in patients with articular cartilage defects. Cartilage. 2011;2(2):122-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;(198):43-9. [PubMed] [Google Scholar]
- 23. Marlovits S, Singer P, Zeller P, Mandl I, Haller J, Trattnig S. Magnetic resonance observation of cartilage repair tissue (MOCART) for the evaluation of autologous chondrocyte transplantation: determination of interobserver variability and correlation to clinical outcome after 2 years. Eur J Radiol. 2006;57(1):16-23. [DOI] [PubMed] [Google Scholar]
- 24. Marlovits S, Striessnig G, Resinger CT, Aldrian SM, Vecsei V, Imhof H, et al. Definition of pertinent parameters for the evaluation of articular cartilage repair tissue with high-resolution magnetic resonance imaging. Eur J Radiol. 2004;52(3):310-9. [DOI] [PubMed] [Google Scholar]
- 25. Brittberg M, Winalski CS. Evaluation of cartilage injuries and repair. J Bone Joint Surg Am. 2003;85-A(Suppl 2):58-69. [DOI] [PubMed] [Google Scholar]
- 26. Chadli L, Steltzlen C, Toanen C, Boisrenoult P, Beaufils P, Pujol N. Hybrid fixation in adult osteochondritis dissecans of the knee. Orthop Traumatol Surg Res. 2018;104:223-5. [DOI] [PubMed] [Google Scholar]
- 27. Berlet GC, Mascia A, Miniaci A. Treatment of unstable osteochondritis dissecans lesions of the knee using autogenous osteochondral grafts (mosaicplasty). Arthroscopy. 1999;15(3):312-6. [DOI] [PubMed] [Google Scholar]
- 28. Minas T, Ogura T, Headrick J, Bryant T. Autologous chondrocyte implantation “Sandwich” technique compared with autologous bone grafting for deep osteochondral lesions in the knee. Am J Sports Med. 2018;46(2):322-32. [DOI] [PubMed] [Google Scholar]
- 29. Perdisa F, Kon E, Sessa A, Andriolo L, Busacca M, Marcacci M, et al. Treatment of knee osteochondritis dissecans with a cell-free biomimetic osteochondral scaffold: clinical and imaging findings at midterm follow-up. Am J Sports Med. 2018;46(2):314-21. [DOI] [PubMed] [Google Scholar]
- 30. Sadr KN, Pulido PA, McCauley JC, Bugbee WD. Osteochondral allograft transplantation in patients with osteochondritis dissecans of the knee. Am J Sports Med. 2016;44(11):2870-5. [DOI] [PubMed] [Google Scholar]
- 31. Makino A, Muscolo DL, Puigdevall M, Costa-Paz M, Ayerza M. Arthroscopic fixation of osteochondritis dissecans of the knee: clinical, magnetic resonance imaging, and arthroscopic follow-up. Am J Sports Med. 2005;33(10):1499-504. [DOI] [PubMed] [Google Scholar]
- 32. Emmerson BC, Görtz S, Jamali AA, Chung C, Amiel D, Bugbee WD. Fresh osteochondral allografting in the treatment of osteochondritis dissecans of the femoral condyle. Am J Sports Med. 2007;35(6):907-14. [DOI] [PubMed] [Google Scholar]
- 33. Gudas R, Simonaityte R, Cekanauskas E, Tamosiūnas R. A prospective, randomized clinical study of osteochondral autologous transplantation versus microfracture for the treatment of osteochondritis dissecans in the knee joint in children. J Pediatr Orthop. 2009;29(7):741-8. [DOI] [PubMed] [Google Scholar]
- 34. Vijayan S, Bartlett W, Bentley G, Carrington RW, Skinner JA, Pollock RC, et al. Autologous chondrocyte implantation for osteochondral lesions in the knee using a bilayer collagen membrane and bone graft: a two- to eight-year follow-up study. J Bone Joint Surg Br. 2012;94(4):488-92. [DOI] [PubMed] [Google Scholar]
- 35. Anderson CN, Magnussen RA, Block JJ, Anderson AF, Spindler KP. Operative fixation of chondral loose bodies in osteochondritis dissecans in the knee: a report of 5 cases. Orthop J Sports Med. 2013;1(2):2325967113496546. [DOI] [PMC free article] [PubMed] [Google Scholar]