Abstract
Objective
The purpose of this manuscript is to analyze the evidence regarding etiopathogenesis of knee osteochondritis dissecans (OCD) lesions through a systematic review, so to summate the current understanding of the origin and progression of this pathologic articular processes.
Design
A systematic review of the literature was performed on the PubMed and Cochrane databases on October 2017 by 2 independent authors and included all levels of evidence. This included all English language literature, pertaining specifically to etiopathology of knee OCD with exclusions for review articles and expert opinion. Of 965 identified records, 154 full-text articles were assessed for eligibility and 86 studies met the inclusion criteria.
Results
According to these studies, the etiology of OCD can be of a biological or mechanical origin: 40 articles proposed a biological hypothesis, including genetic causes (27), ossification center deficit (12), and endocrine disorders (9); conversely, 52 articles supported a mechanical hypothesis, including injury/overuse (18), tibial spine impingement (5), discoid meniscus (16), and biomechanical alterations (20) as the cause of the onset of OCD. The pathogenic processes were investigated by 36 of these articles, with a focus on subchondral bone fracture and ischemia as the ultimate events leading to OCD.
Conclusions
Biological and mechanical factors are found to result in subchondral bone remodeling alterations, acting independently or more likely synergically in the progression of knee OCD. The former includes genetic causes, deficit of ossification centers and endocrine disorders; the latter, tibial spine impingement, discoid meniscus, and biomechanical alterations, together with injuries and overuse. The resultant subchondral bone ischemia and/or fracturing appears to determine the onset and progression of OCD.
Level of Evidence
Systematic review of level II-IV studies, level IV.
Keywords: osteochondritis dissecans, etiology, knee, osteochondral, cartilage
Introduction
Osteochondritis dissecans (OCD) is a pathology known for centuries,1 even before König2 coined the term in 1888, which is currently in use. It defines a pathologic process involving the osteochondral unit, resulting in delamination and sequestration of subchondral bone with or without articular cartilage involvement and instability.3 Orthopedic surgeons, family doctors, and sports medicine specialists should be aware of this condition, since OCD is not a rare source of knee pain and dysfunction, mostly affecting young patients between 10 and 20 years of age,3 with a prevalence of 15 to 29 per 100,000 population and an incidence reported to be increasing.4,5 Its impact on those affected varies significantly, with skeletal age at time of symptoms onset being the most important prognostic factor, in terms of selecting intervention algorithm and predicting outcome success. Thus, the disease is essentially divided into two categories according to the time of clinical recognition as either juvenile OCD or adult OCD. The former affects skeletally immature patients and has a generally better prognosis6 the latter is typical of young adult patients (defined by closed physis) and typically presents a poorer prognosis.7 Theories on the etiopathogenesis are postulated to explain both the occurrence, progression and thus the prognosis of OCD. Historically, traumatic events were deemed to be the cause of the loose bodies, but over the centuries this theory was dispelled by others, such as “quiet necrosis” by Sir James Paget or the inflammatory theory of König.1 Although the shortcomings of these hypotheses were highlighted by subsequent advancements in research, the exact nature of OCD remains elusive.
The purpose of this study is to assess the available evidence on the etiopathogenesis of knee OCD lesions through a systematic review, to better understand the origin and progression of the pathologic processes and possibly identifying areas for future curative therapeutic intervention.
Methods
A systematic review of the literature was performed. The search was conducted on the PubMed and Cochrane databases on October 2, 2017 using the following parameters: ((osteochondritis dissecans) AND (knee)). The guidelines for Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) were used.8 The screening process and analysis were conducted separately by two independent observers. In the first step, the articles were screened by title and abstract. Inclusion criteria for relevant articles used during the initial screening were reports of all levels of evidence, English language, no time limitation, specific to etiopathology of knee OCD. Exclusion criteria were reviews and expert opinions, or manuscripts with focus on joints other than the knee. In the second step, the full texts of selected articles were evaluated for exclusion according to same criteria. Reference lists from the selected papers and from the excluded reviews were reviewed for potential further potentially inclusive reports. Relevant data (type of study, number of patients, demographic of study population, lesion site, proposed theory for etiology and pathogenesis, and remarks) were then extracted. The etiologic theories about OCD proposed in the selected articles were the divided into biological and mechanical, based on the prevalent hypothesis endorsed in each study. A unique data set, composed of consensus of the 2 observers (LA and AC), was established and then analyze for the purposes of the present manuscript.
Results
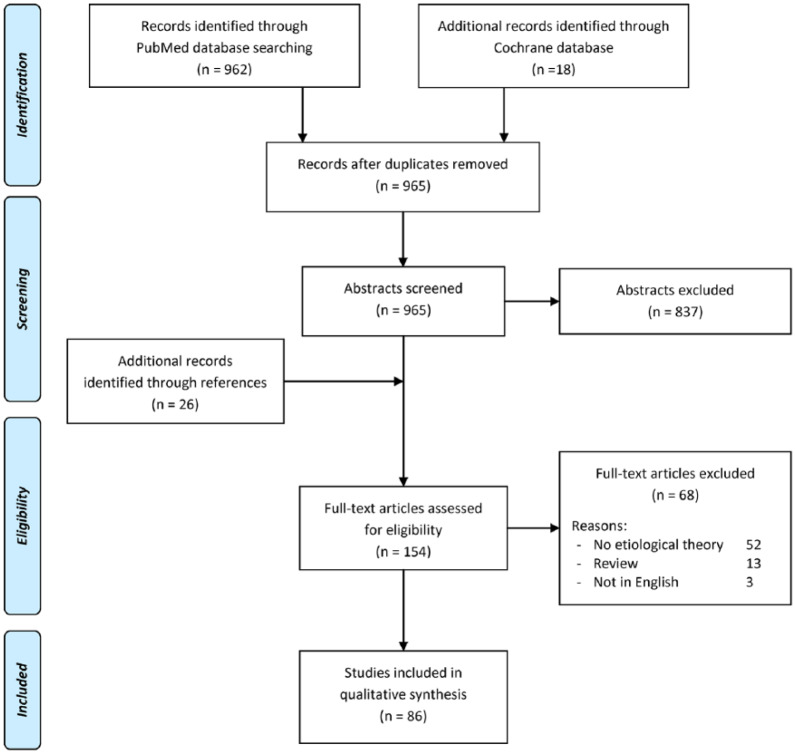
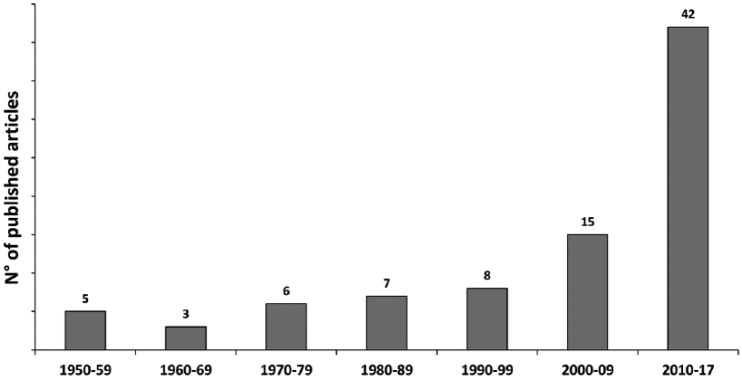
The PubMed and Cochrane search after duplicates removal identified 965 potential abstracts for inclusion, which were screened, as shown in Figure 1 , for a total of 154 full-text articles assessed for eligibility. Sixty-eight full-text articles were further excluded, thus leaving a total of 86 studies to meet the inclusion criteria and use for the literature analysis. These included studies from 1953 to 2017 and ranged from cohort studies up to 133 patients to laboratory studies up to 64 specimens. Of interest an increasing number of studies, almost half of the included articles, have been published in the past 7 years (42/86) ( Fig. 2 ).
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) flowchart of the systematic literature review.
Figure 2.
Etiopathogenesis studies published over time.
The levels of evidence of the included studies included: 39 case reports, 31 case series, 11 laboratory studies and 5 comparative studies. Among the included studies, 40 articles proposed a biological hypothesis,9-47 including genetic causes (n = 27), ossification center deficit (n = 12), and endocrine disorders (n = 9). Conversely, 52 articles supported a mechanical hypothesis,12,13,17,29,34,35,47-92 including injury/overuse (n = 18), tibial spine impingement (n = 5), discoid meniscus (n = 16), and biomechanical alterations (n = 20) as the cause of OCD onset.
Among biologic theories, genetic factors are the most investigated, with 27 studies on 548 patients. Theories vary from an autosomal dominant pattern of inheritance in older studies,39,40 to the association with genetic determined diseases12,27 and to gene mutations causing protein alteration leading to OCD in more recent articles.20,21,44 Other biological hypothesis concerned a deficit in the ossification center; one of the first theories was described in 195534 and was analyzed in 12 studies on 153 patients, or lastly endocrinological factors (including vitamin D deficit,10,42,43 glucocorticoid alterations,14 human growth hormone (hGH) deficiency,18 or association with endocrinologic and sexual abnormalities),36 stressed in 9 studies reporting data of 180 patients.
Among mechanical theories, the traumatic theory was the first one described in the early 1950s.35 This hypothesis, however, has evolved from that of a single event macrotrauma to one proposing repetitive microtraumatic. None the less, it remains one of the most accepted of the proposed etiologies with 18 articles on 297 patients. The other mechanical theories have gained interest more recently. Biomechanical alterations represent one of the most described theory, reported in 20 studies on 527 patients. This category includes lower limb deviation,59,91 ligament or meniscus instability,50,53 knee anatomical features,56,88 shearing stress on patella,71,80 or knee activity–related position.87 Discoid meniscus was first described in 1984 as factor associated with OCD lesions, and subsequently gained increasing credit, being described in 16 studies on 260 patients. The majority of those described the association between lateral discoid meniscus and lateral femoral condyle (LFC) OCD, but the presence of medial discoid meniscus has also been associated with OCD of the medial femoral condyle (MFC).51 Discoid meniscus plays its role in the etiopathogenesis of OCD both if normal or torn, and also related meniscal surgical procedures may influence the history of OCD lesions.89 Finally, tibial spine impingement represents a most recent theory, first described in the late nineties, and it was supported by 5 studies on 97 patients. However, this may explain only the “classic” OCD lesion (secondary to juxtaposition), on the notch side (lateral aspect) of the MFC.
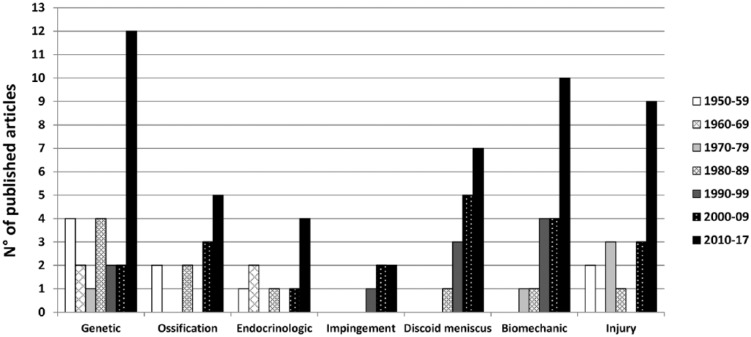
Interestingly, analyzing the number of articles published over the decades by etiology ( Fig. 3 ), a shift is seen in the past 20 years from biologic toward mechanical hypothesis. In fact, 55% of the articles published in the past century supported a biologic theory, while 61% of the studies published from 2000 to 2017 supported the mechanical hypothesis. Overall, based on the number of studies supporting their importance, the strongest factors are genetic causes (27), biomechanical alterations (20), injury/overuse (18), and discoid meniscus (16). Fewer studies supported the importance of ossification center deficit (12), endocrine disorders (9), and tibial spine impingement (5). Nevertheless, also these factors are likely to significantly contribute to the onset of OCD in some patients, with the importance of each factor and the interplay among concomitant factors leading to OCD being related to the specific case.
Figure 3.
Trend of etiological hypothesis over time.
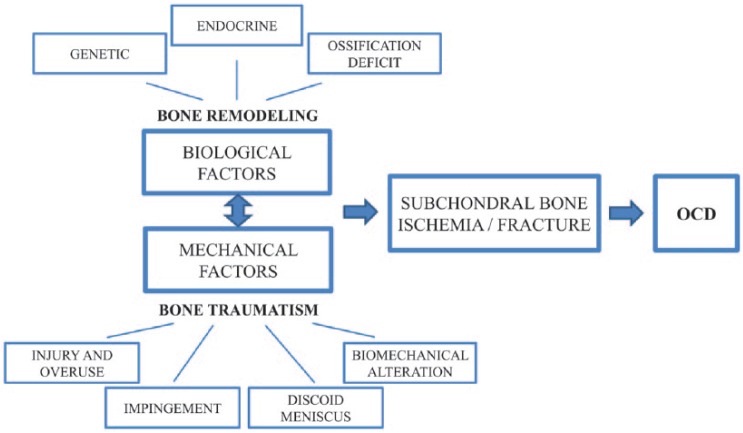
The cascade of events leading to OCD was specifically described in 36 articles, with subchondral bone fracture (28 articles) or subchondral bone ischemia (8 articles) as the most common final pathogenetic mechanisms ( Fig. 4 ). While subchondral bone is almost universally recognized as the primarily affected tissue, one article suggested that OCD is a cartilaginous disease with the subchondral bone secondarily damaged.19
Figure 4.
Trend of pathogenetic theories over time.
More detailed aspects of the selected studies, including type of study, number of patients, age, lesion site, proposed theory for etiology and pathogenesis, and results, are reported in Table 1 .
Table 1.
Detailed Description of the 86 Studies Selected in the Systematic Review.
| Author Year |
Type of Study | No. of Patients Mean Age Lesion Site |
Etiological Theory | Biologic | Mechanic | Pathogenesis | Note |
|---|---|---|---|---|---|---|---|
| Kumahashi 201792 |
Case report: bilateral OCD | 1 13 y lateral trochlea |
Repetitive microtrauma | ✓ | / | OCD of lateral femoral trochlea developed bilaterally without coexisting patellofemoral abnormalities | |
| Gonzalez-Herranz 201791 |
Retrospective study: mechanical axis and OCD | 48 13.7 y MFC, LFC |
Biomechanical alterations | ✓ | / | Lower limb mechanical axis deviations are more strictly associated than anatomical axis deviations with OCD lesions | |
| Takigami 201790 |
Case series: discoid lateral meniscus and OCD | 133 12 y LCF |
Discoid meniscus | ✓ | / | Male sex, young age and type C discoid lateral meniscus (Ahn) were found to be predictive factors for OCD of LFC | |
| Ishikawa 201689 |
Case report: OCD and lateral discoid meniscus | 1 19 y LFC |
Discoid meniscus (meniscectomy) | ✓ | / | A stable JOCD LFC lesion associated with lateral discoid meniscus developed into an unstable status after its meniscectomy (altered environment of mechanical force transmission) | |
| Ishikawa 201688 |
Case-control study: PCL anatomy and MFC OCD | 39 15 y MFC, LFC |
Biomechanical alterations | ✓ | /91 | PCL in patients with MCF OCD attached more distally at the lateral aspect of the MFC compared with LFC OCD, ACL and meniscal injuries | |
| Gornitzky 201646 |
Retrospective study: familial OCD | 103 13 y knee |
Genetic | ✓ | / | 14% of patients with OCD have a family history of the condition (higher than previously reported prevalence in general population) | |
| McElroy 201687 |
Retrospective study: OCD in baseball | 78 12 y knee |
Biomechanical alterations | ✓ | / | Catchers developed OCD at a younger age and in a more posterior location MFC and LFC than noncatchers, maybe because of repetitive and persistent hyperflexion | |
| Ellermann 201645 |
Case series: MRI findings | 13 14.9 y knee |
Ossification centers defect | ✓ | Epiphyseal cartilage ischemia | OCD may have an epiphyseal cartilage origin with subsequent osseous repair stages with osseous bridging, which can heal or detach | |
| Yellin 201544 |
Comparative study: genes in OCD vs. control | 209 / knee |
Genetic | ✓ | / | The genome analysis revealed 35 single-nucleotide polymorphism at several loci having a possible association with OCD | |
| Persiani 201586 |
Case report: OCD and osteogenesis imperfecta | 1 14 y LFC |
Trauma | ✓ | / | OCD developed after a trauma in a patient with weak bone structure due to osteogenesis imperfecta | |
| Tòth 201585 |
Laboratory study: MRI findings in human cadaver | 5 13.6 mo distal femur |
Biomechanical alterations | ✓ | Vascular failure and ischemia | Vascular architecture in human, with vessel primarily arising from perichondrium and disappearing with ages in OCD predilection sites, may cause vascular failure, due to biomechanical alteration or structural weakness | |
| Cavaignac 201584 |
Comparative study: OCD vs control | 37 (vs 42) 14.3 y MFC |
Tibial spine impingement | ✓ | / | Patients with OCD have a more prominent tibial spine that patients without OCD | |
| Gorter 20159 |
Case report: familial OCD | 3 13.3 y MFC |
Genetic | ✓ | / | Bilateral MFC OCD in a mother, her daughter and her MZ twin sister suggests a genetic role | |
| Krause 201543 |
Laboratory study: histological analysis and vitamin D | 64 12 y knee |
Endocrinologic (vitamin D) | ✓ | Subchondral insufficiency fracture | Vitamin D deficiency leads to lack of mineralization making the bone segment more prone to mechanical stress and may result in subchondral insufficiency fractures. No sign of ischemia | |
| Chow 201549 |
Case-control study: MFC OCD risk factors | 35 12 y MFC |
Tibial spine impingement | ✓ | Subchondral bone fracture | OCD knees have smaller notch width than controls, leading to tibial spine impingement and OCD | |
| Bruns 201410 |
Case series: vitamin D deficit | 23 31.3 y knee, talus, elbow |
Endocrinologic (vitamin D) | ✓ | / | 18/23 patients presented vitamin D3 deficit, which causes bone metabolism alterations | |
| Deroussen 201450 |
Case report: cruciates agenesis and OCD of LTP | 1 12 y LTP |
Biomechanical alterations | ✓ | Subchondral bone fracture | Anteroposterior instability caused by agenesis of ACL and PCL may lead to LM lesions and OCD | |
| Mine 201451 |
Case report: discoid medial meniscus and OCD | 1 13 y MFC |
Discoid meniscus | ✓ | / | Torn discoid medial meniscus may cause OCD through a stress redistribution | |
| Wechter 201452 |
Case series: proximal tibial morphology | 72 15.4 y MFC, LFC |
Biomechanical alterations | ✓ | / | Medial and posterior tibial slope lead to focally increased mechanical forces on condyles | |
| Camathias 201453 |
Cohort study: meniscal stabilization treating OCD | 28 / MFC, LFC |
Biomechanical alterations | ✓ | Subchondral bone stress | Meniscal instability (i.e., a hypermobile anterior horn) may impinge between articular surfaces leading to OCD | |
| Sebaaly 201483 |
Case report: discoid lateral meniscus and OCD | 1 14 y LFC |
Discoid meniscus | ✓ | / | OCD associated with Wrisberg variant of discoid meniscus, which is characterized by poor stabilization with subluxation of the anterior horn in the intercondylar notch | |
| Maruyama 201454 |
Case report: discoid lateral meniscus and OCD | 1 14 y LFC, trochlea |
Discoid meniscus | ✓ | Subchondral bone fracture | Discoid lateral meniscus and repeated trauma in sport activity might cause OCD | |
| Richie 201311 |
Case report: MZ twin brothers | 2 15 and 16 y lateral trochlea |
Genetic | ✓ | Subchondral bone fracture | Similar locations and timing are suggestive of a genetic component | |
| Park 201312 |
Case report: Wilson disease | 1 17 y MFC, LFC |
Genetic (Wilson disease)/trauma | ✓ | ✓ | / | Subchondral cysts, osteoporosis, copper deposition in joints/clumsy patients often sustaining trauma |
| Gans 201313 |
Case report: MZ twin brothers | 4 16 y LFC, MFC |
Genetic/discoid meniscus/trauma | ✓ | ✓ | Subchondral bone alteration | OCD associated with discoid meniscus, dominant limb, and genetic factors |
| Kroger 201314 |
Case series: juvenile idiopathic arthritis and OCD | 13 6.5 y knee, ankle |
Endocrinologic (glucocorticoid)/inflammation | ✓ | Subchondral bone fracture | Glucocorticoid injection and persistent synovitis affect osteochondral metabolism | |
| Jeong 201315 |
Case report: bilateral OCD in brothers | 2 32 and 28 y bilateral bicondylar |
Ossification centers defect/genetic | ✓ | / | Probable not-identified genetic factors affected structural integrity and pathophysiology | |
| Kilcoyne 201382 |
Case report: discoid lateral meniscus and OCD | 1 21 y LFC |
Discoid meniscus | ✓ | Subchondral bone stress | OCD developed in a skeletally mature patient with intact discoid meniscus after minor trauma | |
| Shea 201355 |
Case series: acute bone contusion and OCD | 2 11 and 15 y MFC, LFC |
Single trauma | ✓ | Acute subchondral bone contusion | Single traumatic events may also play a role in the development of OCD | |
| Grimm 201357 |
Case report: multiple OCD lesions in single knee | 1 15 y LFC, MFC, trochlea |
Biomechanical alterations | ✓ | / | OCD of MFC developed after using a varus unloader brace (repetitive stress on medial compartment) | |
| Onoda 201216 |
Case report: MZ twin brothers | 2 18 and 20 y MFC, LFC |
Genetic | ✓ | Subchondral bone alteration | Genetic factors are considered to affect the integrity of the subchondral bone | |
| Kamei 201256 |
Case series: lateral meniscus alterations and OCD | 58 17.7 y LFC |
Biomechanical alterations | ✓ | / | The shape of the LFC (prominence ratio of LFC) may be associated with the development of OCD | |
| Laor 201217 |
Comparative study: JOCD vs. normal ossification variants | 30 vs. 30 11.2 y MFC, LFC |
Ossification centers defect/ repetitive trauma | ✓ | ✓ | / | JOCD results from an insult (repetitive trauma) affecting endochondral ossification |
| Jans 201258 |
Comparative study: JOCD vs. normal ossification variants | 116 11.5 y knee |
Repetitive microtrauma | ✓ | Subchondral bone ischemia | Ossification variants do not correlate with OCD. Repetitive microtrauma may compromise the physis blood supply (typical MRI sign) | |
| Hussain 201118 |
Case report: hGH deficiency and multiple OCD | 1 16 y MFC, LFC, elbow |
Endocrinologic/ossification centers defect | ✓ | Subchondral bone fracture | Changes in hGH (deficit or supplementation) levels may lead to atypical ossification nuclei and OCD | |
| Skagen 201119 |
Case series: histologic findings | 4 23.3 y MFC, LFC |
Genetic/ossification centers defect | ✓ | Cartilaginous disease | OCD may be an endoplasmic reticulum storage disease, which disturbs endochondral ossification | |
| Stattin 201020 |
Case series: familial OCD | 15 / knee, hip, elbow |
Genetic (ACAN gene) | ✓ | / | The altered protein is involved in the organization of cartilage matrix | |
| Jackson 201021 |
Case series: OCD associated with collagen deseases | 19 / / |
Genetic (collagen IX gene) | ✓ | / | Collagen mutation causes endoplasmic reticulum stress with increased chondrocyte apoptosis | |
| Jacobi 201059 |
Case series: OCD and mechanical axis of the limb | 93 22 y MFC, LFC |
Biomechanical alterations | ✓ | / | Varus axis is associated with MFC OCD and valgus with LFC OCD (higher compartment loading) | |
| Yonetani 201060 |
Case series: histologic findings | 8 13 y MFC |
Trauma | ✓ | Subchondral bone fracture | The initial damage may occur at the border between hyaline articular cartilage and subchondral bone | |
| Mackie 201022 |
Case report: MZ twin brothers | 2 17 and 19 y MFC |
Genetic | ✓ | Subchondral bone lesion | The presence of identical lesions in MZ twins suggests the possibility of a genetic predisposition | |
| Lippi 201062 |
Historical article: examination of skeletal remains | 1 16.5 y patella |
Trauma | ✓ | / | Repetitive microtrauma or macrotrauma during sport activity (kickball) may have caused OCD | |
| Uozumi 200961 |
Laboratory study: histologic findings | 11 16 y MFC |
Repetitive microtrauma | ✓ | Subchondral bone fracture or necrosis | The initial subchondral change is fracture or necrosis depending on the etiology of OCD | |
| Beyzadeoglu 200863 |
Case report: hypoplastic medial meniscus and OCD | 1 10 y MFC |
Biomechanical alterations/impingement | ✓ | / | Big tibial spine (impingement) and abnormal menisci (repetitive microtrauma) may cause OCD | |
| Hashimoto 200864 |
Case report: discoid lateral meniscus and OCD | 1 12 y LFC |
Biomechanical alterations/discoid meniscus | ✓ | / | Discoid lateral meniscus, valgus axis after meniscectomy and sport cause repetitive trauma on LFC | |
| Stattin 200823 |
Case report: familial OCD | 15 / knee, hip, elbow |
Genetic | ✓ | / | OCD with an autosomal dominant inheritance. Hypothesis of candidate genes (cartilage and bone proteins) | |
| Hanna 200824 |
Case report: bicondylar OCD and histologic findings | 2 15 y MFC, LFC |
Ossification centers defect | ✓ | / | Defect in ossification centers of distal femur causes OCD. Trauma separates ossification nucleus | |
| Deie 200665 |
Case series: discoid lateral meniscus and OCD | 28 13.3 y LFC |
Discoid meniscus | ✓ | / | Correlation between intact discoid lateral menisci and LFC OCD (increased mechanical stress) | |
| Quan 200542 |
Case report: OCD and rickets | 1 12 MFC |
Endocrinologic (vitamin D) | ✓ | / | Since the osteoid matrix is abnormal and weakened, rachitic joints are prone to trauma | |
| Cetik 200525 |
Case report: bilateral LFC OCD | 1 20 y LFC |
Ossification centers defect | ✓ | / | Defect in the ossification center of the distal LFC may play a role in the etiology of OCD | |
| Gebarski 200526 |
Case series: stage-I OCD vs normal ossification variants | 23 13 y knee |
Ossification centers defect | ✓ | Subchondral bone defect | Central condylar lesion with edema and characteristic puzzle aspect favors OCD diagnosis | |
| Stanitski 200466 |
Case report: discoid lateral meniscus and OCD | 2 6 y LFC |
Discoid meniscus | ✓ | Subchondral bone fracture | LFC OCD is related to increased stress caused by the discoid lateral meniscus or its meniscectomy | |
| Bramer 200467 |
Retrospective study: increased tibial exotorsion and OCD | 23 13 y MFC |
biomechanical alterations/impingement | ✓ | / | Increased tibial exotorsion may cause OCD because enhances the tibial spine impingement on MFC | |
| Hughes 200368 |
Case series: pathologic progression of OCD | 19 11.3 y knee |
Trauma | ✓ | Subchondral bone stress fracture | Intact cartilage becomes vulnerable to trauma if it loses support of the damaged subchondral bone | |
| Kilic 200227 |
Case report: hyper IgE syndrome | 1 13 y LFC |
Genetic (hyper IgE syndrome) | ✓ | Subchondral bone fracture | Osteopenia caused by hyper IgE syndrome is a favorable etiologic factor of OCD | |
| Atay 200270 |
Case report: menisci anomalies and OCD | 1 16 y MFC |
Biomechanical alterations/discoid meniscus | ✓ | / | MFC OCD is associated with a ring-shape lateral meniscus with cystic formation | |
| Mizuta 200169 |
Case series: discoid lateral meniscus and OCD | 6 9 y LFC |
Discoid meniscus/trauma | ✓ | / | Meniscectomy of discoid LM and repeated sporting impaction on the immature structures may cause OCD | |
| Bruns 199971 |
Case series: patellar OCD | 15 / patella |
Biomechanical alterations | ✓ | Subchondral bone damage | Repetitive motions of a plain patellar surface result in subchondral damage, initiating the OCD process | |
| Mitsuoka 199972 |
Case series: discoid lateral meniscus and OCD | 13 18.4 y LFC, MFC |
Discoid meniscus | ✓ | / | Discoid meniscus produces repetitive stress on weaker growing structures leading to OCD | |
| Raber 199874 |
Case series: discoid lateral meniscus and OCD | 14 9 y LFC |
Biomechanical alterations/discoid meniscus | ✓ | / | Weak correlation between total meniscectomy of discoid lateral meniscus and OCD; it may be due to the increased focal stress concentration after total meniscectomy | |
| Mitsuoka 199873 |
Case report: OCD and tibial spine impingement | 1 13 y MFC |
Tibial spine impingement | ✓ | / | Anterior tibial spine impinging on the MFC because of the narrow intercondylar notch may cause OCD | |
| Koch 199775 |
Laboratory study: histologic findings | 30 30 y MFC |
Biomechanical alterations | ✓ | Subchondral bone lesion | Biomechanical alterations cause the first change in subchondral bone and the progression to OCD | |
| Livesley 199247 |
Case report: patellar OCD | 3 16, 15, 12 y patella |
Biomechanical alterations/genetic | ✓ | ✓ | / | Recurrent patella subluxation in this family may be the biomechanical alteration causing OCD |
| Aichroth 199176 |
Case series: discoid lateral meniscus and OCD | 52 10.5 y LFC |
Discoid meniscus | ✓ | / | Among 52 patients with lateral discoid meniscus, 7 presented OCD and 4 ossification defects | |
| Fonseca 199028 |
Case report: familial OCD | 3 16, 11, 9.7 y MFC |
Genetic | ✓ | Subchondral bone ischemia | The higher incidence of OA suggests for familial OCD a separate pathogenesis from nonfamilial OCD | |
| Desai 198777 |
Case series: patellar OCD | 11 16 y patella |
Biomechanical alterations | ✓ | Subchondral bone alteration | OCD might be caused by the repetitive shear stress on patella during knee flexion | |
| Kozlowski 198593 |
Case reports: familial OCD | 2 12, 44 y knee, elbow, metacarpal |
Genetic | ✓ | / | Familial OCD may be a hereditary dysplasia of articular cartilage characterized by abnormal chondrocyte metabolism | |
| Phillips 198541 |
Case report: familial multiple OCD | 3 20, 25, 45 y knee, elbow |
Genetic | ✓ | / | Association of OCD involving multiple joints with short stature | |
| Irani 198478 |
Case report: discoid lateral meniscus and OCD | 1 15 y LFC |
Discoid meniscus | ✓ | Subchondral bone fracture | First case of association between injured discoid lateral meniscus and OCD of the LFC | |
| Barrie 198429 |
Laboratory study: histologic findings of loose bodies | / / / |
Ossification centers defect/trauma | ✓ | ✓ | Subchondral bone fracture | Ossification defect causes subchondral bone separation. Trauma detach cartilage, including tidemark |
| Andrew 198140 |
Case report: familial OCD and dwarfism | 12 / knee, elbow |
Genetic (associated with dwarfism) | ✓ | / | OCD may be associate with dwarfism, and its pedigree is consistent with an autosomal dominant pattern of inheritance | |
| Mubarak 198130 |
Case series: role of constitutional factors | 73 13.4 y MFC, LFC, patella |
genetic/endocrinologic/ossification centers defect | ✓ | / | Genetics, endocrine dysfunction, epiphyseal abnormalities seem the most important for OCD onset | |
| Mubarak 197839 |
Case series: familial OCD | 20 / MFC, LFC, patella |
Genetic (associated with dwarfism) | ✓ | / | The autosomal dominant pattern of OCD and association with mild dwarfism were observed during a study of 4 generation of one family, with 20 of 31 members affected | |
| Milgram 197879 |
Laboratory study: histologic findings | 50 / knee |
Trauma | ✓ | Osteochondral fracture | Major or minor (e.g., sudden pivoting) trauma might cause OCD through an osteochondral fracture | |
| Edwards 197780 |
Case series: patellar OCD | 5 15.4 y patella |
Biomechanical alterations | ✓ | Fracture | Repetitive shearing stress on patella associated with recurrent subluxation could cause OCD | |
| Petrie 197794 |
Case series: relatives of patients with OCD | 34 / knee, ankle, elbow |
Multifactorial | / | Only 1 of 86 relatives of 34 patients presents the disease: common form of OCD is not familial | ||
| Linden 197748 |
Laboratory study: histologic findings | 14 20 y MFC |
Trauma | ✓ | Subchondral bone fracture | Single/repetitive trauma cause sub-chondral bone fracture; poor blood supply blocks reparative process | |
| Chiroff 197581 |
Laboratory study: histologic findings | 6 22.6 y MFC |
Single trauma | ✓ | Osteochondral fracture | OCD represents the effect of a trauma and the subsequent reparative process | |
| Hanley 196738 |
Case report: familial OCD | 2 16 and 14 y knee, elbow |
genetic/endocrinologic | ✓ | / | Description of OCD in 2 brothers with associated multiple abnormalities (endocrinal problems, pectum excavatum, short little fingers, altered facies) | |
| Campbell 196631 |
Laboratory study: histologic findings | / / / |
Ischemic/metabolic | ✓ | Subchondral bone ischemia | A vascular or localized metabolic disturbance in the distal end of the long bone during a period of rapid growth causes subchondral bone necrosis | |
| Stougaard 196437 |
Case report: familial OCD | 10 / knee, elbow |
Genetic | ✓ | / | In this family 10 of 31 members affected by OCD. Association with short stature | |
| White 195736 |
Case report: familial OCD | 3 28, 21, 21 y knee, elbow |
Genetic/endocrinologic | ✓ | / | Association with endocrinologic and sexual abnormalities | |
| Tobin 195732 |
Case report: OCD associated with tibia vara | 4 / MFC |
Genetic/ossification centers defect | ✓ | / | OCD in 4 members of the same family affected by adolescent type of tibia vara supports a genetic theory | |
| Pick 195533 |
Case report: familial OCD | 4 17.5 y knee, elbow |
Genetic | ✓ | / | Occurrence of bilateral knee or elbow OCD in various member of a family supports a genetic theory | |
| Ribbing 195534 |
Case series and laboratory study: histologic findings | / / / |
Ossification centers defect/trauma | ✓ | ✓ | Subchondral bone ischemia | Mild trauma alters blood supply of partially detached bone nucleus, which is a locus minoris resistentiae |
| Green 195335 |
Laboratory study: histologic findings | 27 9.5 y knee, elbow, ankle |
Trauma/genetic | ✓ | ✓ | Subchondral bone aseptic necrosis | In a genetic predisposition context, trauma cause OCD directly or by subchondral blood supply alteration |
hGH = human growth hormone; JOCD = juvenile osteochondritis dissecans; LFC = lateral femoral condyle; LM = lateral meniscus; MFC = medial femoral condyle; MRI = magnetic resonance imaging; MZ = monozygotic; OA = osteoarthritis; OCD = osteochondritis dissecans.
Discussion
This systematic review presented the entire spectrum of evidence on the etiopathology of OCD in the knee. The main study finding is that, based on the results provided by the selected articles, OCD can be caused by biological and/or mechanical factors. Furthermore, most of the studies identified subchondral bone fracture and ischemia as the ultimate cause in the pathogenetic processes leading to knee OCD.
It has to be pointed out that the level of evidence for the literature on OCD etiopathogenesis is generally low, with several case reports and studies reporting a relatively low number of patients. More over these studies are very heterogeneous for what concerns methods and results, thus making impossible to perform a quantitative evaluation of the overall data reported. Nevertheless, the theories documented in the current literature were reported, summarized and critically analyzed to best fit the spectrum of hypotheses into a etiopathogenic categorical framework ( Fig. 5 ).
Figure 5.
Framework of the etiopathogenetic theories documented in the current literature.
Biological Etiological Factors
Genetic Hypothesis
Several authors9,11-13,15,16,19-23,27,28,30,32,33,35-41,44,46,47,93 found a familial occurrence of OCD and some also identified specific gene alterations which can directly or indirectly cause the disease. Stattin et al.20 identified a possible candidate gene, the ACAN gene, which encodes a protein involved in the organization of the aggrecan network, whose alteration leads to the disruption of extracellular matrix interactions causing a familial OCD with an autosomal dominant inheritance. Extra-cellular matrix alterations were also investigated by Jackson et al.,21 who found that patients with type IX collagen gene mutations presented OCD lesions combined with multiple epiphyseal dysplasia and a form of mild myopathy. They postulated that the expression of mutant type IX collagen may elicit a stress response involving endoplasmic reticulum and mitochondrial function. Skagen et al.19 speculated a role for altered chondrocyte extracellular matrix synthesis that may cause similarly effect endoplasmic reticulum storage. This effect then disturbs the endochondral ossification leading to OCD.
Alterations of bone remodeling and bone quality were found to be associated with OCD in 2 case reports about patients affected by systemic disease. Kilic et al.27 described a patient with hyper IgE syndrome who developed a knee OCD lesion, proposing osteopenia related to the immunologic condition may represent an etiological factor. Park et al.12 described development of OCD in a patient affected by Wilson disease, suggesting a correlation between the osteochondral lesion and osteoporosis, osteomalacia, and copper deposition in joints typical of this genetically determined condition.
Several reports describe patients affected by OCD within families and among several generations, stressing the importance of a genetic susceptibility and considering the frequent involvement of both in monozygotic twins.11,13,15,19,22,30,35,47 Nevertheless, Petrie et al.94 examined first- and second-degree relatives of 34 patients with OCD and found only 1 affected by OCD, concluding that the most common form of this disorder is not familial.
Ossification Deficit Hypothesis
Defects in the ossification centers of the distal femur are thought to predispose to OCD lesions.15,17,19,24-26,29,30,32,34,45 Ribbing34 was the first (1955) to describe an accessory bone nucleus detachment in childhood, that may partly fuse during adolescence into the adjacent cancellous bone, remaining partially separated from the latter by islands of persisting cartilage. The incomplete connection between the vascular system of the bone nucleus causes a locus minoris resistentiae, which enables mild injury or strain to produce a slight dislocation with deleterious effects and the separation of the osteochondral unit. Pathologically this seemed consistent with analysis of loose bodies later performed by Barrie.29 Conversely, Laor et al.17 suggested how an exogenous chronic mechanical insult can affect endochondral ossification of the physis resulting in juvenile OCD.
The detection of pathologic ossification can be challenged by the presence of physiologic variants. In fact, in skeletally immature patients, early stages of OCD might be confused with normal ossification variants, which might account for the “better prognosis” of JOCD with respect to AOCD.26 Jans et al.58 confirmed the independent occurrence of normal variants and OCD in a comparative study on large cohorts of patients: 12% out of 116 patients affected by OCD presented normal ossification variants, the same percentage reported in the analysis of the healthy population. A correct differential diagnosis is thus fundamental to prevent unnecessary treatment: location in the inferocentral posterior femoral condyles with intact overlying cartilage, accessory ossification centers, spiculations, residual cartilaginous model, and lack of bone marrow edema are features of normal variants and not typical of OCD.
Endocrine Hypothesis
Hormonal alterations might affect bone metabolism by inducing a process of bone remodeling and subsequent onset of osteochondral lesions. A link between various endocrine abnormalities and OCD was first suggested in 1981 by Mubarak and Carrol,30 who observed a common occurrence of endocrine dysfunction in their patients, but the endocrine theory was further explored only recently.10,14,18,30 In 2013, Kröger et al.14 documented 13 cases of OCD in children with juvenile idiopathic arthritis, and suggested either an alteration of the articular surface due to the persistent synovitis, or the possible detrimental effects of glucocorticosteroid injections on cartilage metabolism. Hussain et al.18 focused instead on changes in hGH levels (it is still not clear whether it is the deficit itself or the hormone supplementation) which may lead to atypical ossification nuclei and subsequent OCD lesions. Finally, in 2014, Bruns et al.10 shed light on another contributing factor in the progression of the pathology, with 21 out of 23 patients affected by OCD presenting low vitamin D3 levels.
Mechanical Etiological Factors
Injury and Overuse
Historically, the most advocated theory is the traumatic one, even though a singular macrotrauma was not found to be common, but rather a curiosity.12,13,29,31,35,48,55,58,60-62,68,69,79,81,86,92 Shea et al.55 reported the case of a patient who developed OCD after an acute traumatic event and proposed a correlation between femoral condyle bone contusion and disease development as an explanation for the OCD finding. What seems more likely is repetitive microtrauma or chronic loading might play a role in the OCD etiopathogenetic process. These events can act by themselves48,55,58,60-62,68,79,81 or in combination with other predisposing factors, (e.g. biological or the other mechanical factors).
Tibial Spine Impingement Hypothesis
In 1933, Fairbank was the first to suggest the role of tibial spine impingement against the lateral aspect of the medial condyle as an etiological factor for OCD: abnormal shear forces, caused by the impingement, are generated during internal rotation of the tibia with loading in flexion.95 Bramer et al.67extended this hypothesis noting increased external tibial torsion might play a role, compensating for the externally rotated position of the foot. Although this theory fails to account for OCD lesions at other sites, it has been subsequently advocated by several authors, thus suggesting that impingement is a valid explanation for OCD in specific joint locations.49,63,67,73,84
Discoid Meniscus Hypothesis
A link between the discoid meniscus variant and femoral condyle OCD is well described.13,51,54,64-66,69,72,74,76,78,82 The alterations of joint mechanics produced by the presence of a discoid meniscus may cause an increase in peak loading forces to the subchondral bone lesion predisposing onset of fragment formation.66 This hypothesis is supported by the fact that the lateral location is uncommon for OCD except in patients with discoid lateral meniscus.65 Furthermore, Deie et al.65 even linked the type of lateral discoid meniscus, complete or incomplete, to OCD at specific sites of the lateral femoral condyle.
Although it is likely that the abnormal menisci may cause OCD due to the effect of repetitive abnormal stress on weaker osteochondral growing structures,63 it is still unclear whether the link derives more from the presence of an intact discoid meniscus,65,82 a torn discoid meniscus,51,78 or if it is secondary to the alterations provoked by the meniscectomy of the discoid meniscus.64,66,69,74
More controversial is the role of skeletal maturity on the effects of discoid meniscus presence. While Mitsuoka et al.72 underlined the consequences of the abnormal stress produced by a discoid meniscus on the weaker osteochondral structures in the growing period, Kilcoyne et al.82 stated that the link between discoid meniscus and OCD extended also beyond the skeletally immature phase.
Biomechanical Alteration Hypothesis
Abnormal biomechanics may have chronic effects on the articular load distribution with a marked impact on the joint homeostasis, which may also contribute to onset of OCD.47,50,52,53,56,57,59,63,64,67,70,71,74,75,77,80
Many conditions can account for this, such as meniscectomy, joint instability, genu recurvatum, and condylar flattening, that increase contact forces at the joint and explain chronic repetitive microtrauma.5,96 Camathias et al.53 suggested that meniscal instability, specifically a hypermobile anterior horn, might be a decisive factor in the origin of OCD. The meniscus in this condition may work like a “doorstop,” so that the peripheral edge of the loose meniscus impinges repeatedly between the tibial plateau and femoral condyle as the knee moves from flexion to extension, in the end damaging the corresponding femoral osteochondral unit.53
Other examples of OCD associated with biomechanical alterations include: a greater tibial slope,52a more prominent lateral femoral condyle,56 or the agenesis of both cruciate ligaments causing anteroposterior instability.50 Similarly, varus or valgus deviations of the knee lead to increased mechanical loading of the respective knee compartments.57,59,75 Besides femoral condyles, the patellar surface may also suffer from abnormalities, thus causing a biomechanical disequilibrium: an atypical patellar surface71 as well as a recurrent patellar subluxation can cause a repetitive shear stress during knee flexion.47,77,80 All these conditions might result in a chronic mechanical insult of the osteochondral unit and subsequent development of OCD.
Pathogenetic Mechanisms
Many of the selected articles refer to a pathogenetic progression of OCD through either ischemia28,31,35,58 or subchondral fracture.11,14,18,22,26,27,29,48-50,54,60,61,66,68,71,75,78-81 Whether there is interplay of these 2 conditions or how they are interdependent remains unclear. Uozumi et al.61 following a histologic analysis hypothesized that the pathologic progression depends on the cause of OCD. Thus, resulting subchondral bone changes reflect the pathologic “primum movens.” In the case of ischemic etiology, the initial change in the subchondral area is necrosis followed by subchondral fracture. In support of a primarily vascular cause, Campbell and Ranawat31 point to the simultaneous occurrence of OCD and Osgood-Schlatter disease in childhood and early adolescence. Thereby suggesting a regional vascular insufficiency based metabolic disturbance of the long bone during rapid growth periods, as a common etiology.31 If the underlaying cause is a repetitive microtrauma, it is possible to find a subchondral fracture with subsequent bone necrosis due to the lack of the blood supply from the basal side.61
In any case, regardless of the initiating events, there is agreement on the primary involvement of the subchondral bone in the development of OCD.11,14,16,18,22,26-29,31,34,35,48-50,53-55,58,60,61,66,68,71,75,77-82 In fact, besides an isolated position suggesting that OCD is a cartilaginous disease with the subchondral bone secondarily damaged,19 all other authors referred to the ischemia or fracture of the subchondral bone as etiological “primum movens” acting primarily on the subchondral bone.
Ischemia
Green and Banks35 emphasized the role of ischemic subchondral bone back in 1953. Their histological examination confirmed the basic process in OCD is an aseptic necrosis involving the subchondral bone and subsequent changes are secondary. They speculated that in the earlier phases of the pathologic progression the cartilage remains healthy, because of the nutrition received from the synovial fluid. As dead bone is absorbed, the cartilage gradually loses its mechanical and structural support, becoming more susceptible to trauma and exogenous factors. A few years later, Ribbing34 introduced the hypothesis of ossification nuclei defects, stressing how the bone nucleus partially connected to the cancellous bone represents a locus minoris resistentiae, which enables low-intensity trauma to produce harmful effects on the blood supply of the bone nucleus.
Campbell and Ranawat31 subsequently classified OCD as idiopathic aseptic necrotic lesions of the growing epiphysis. Their histological examinations showed a large area beneath the detached fragment which had the characteristic findings of a bone infarct. This, together with the intact overlying articular cartilage, confirmed the necrosis of the underlying bone as a primary event for the formation of the loose body.
The idea of subchondral bone ischemia was recently emphasized by Jans et al.,58 who supported the involvement of arterial end branches for the developmental OCD sequence beginning with the separation of the subchondral bone. However, they also advocated repetitive microtrauma as the cause of the compromised blood supply in rapidly growing patients, with interplay of vascular and traumatic factors leading to the onset of OCD.
Fractures
The impingement etiology supports a traumatic mechanism of onset leading to the subchondral bone fracture. Shea et al.55 even reported a case ascribed to a single macrotrauma, whereas others observed repetitive microtrauma that provoked a subchondral bone stress fracture which leading to OCD in otherwise normal knee joints.49,54,68 The occurrence of OCD at the patella also supports the traumatic origin. The plain patellar surface or the recurrent subluxation of the sesamoid bone during knee flexion causes repetitive microtrauma.71,77,80 Moreover, besides the biomechanical predisposition, the site of the lesion is more suggestive of a traumatic source rather than an ischemic one. In fact, whereas the type of patellar vascularization might entail proximal damage in case of a vascular mechanism, the most common OCD location is in the lower and middle thirds of the articular surface, which are the patellofemoral contact areas subjected to the maximal forces during knee flexion.77
Constitutional factors may weaken the subchondral bone and favor the fracture mechanism. Among these, osteopenia caused by hyper IgE syndrome27 or endocrine abnormalities alter metabolism, structure and function of the subchondral bone.18 Changes in hGH levels may lead to atypical ossification nuclei and decreased ability of the growth plate to absorb energy, and vitamin D deficit10 has also been indicted as predisposing factor in leaving the subchondral bone susceptible to damage and separation and eventually the development of OCD lesions.
Conclusions
According to this summation of the historic literature, the etiology of OCD can be attributed to either biological or mechanical factors. The former includes genetic causes, deficit of ossification centers and endocrine disorders; the latter, tibial spine impingement, discoid meniscus, and biomechanical alterations, together with injuries and overuse. Interplay of the hypothesized factors that affect the osteochondral unit may support a connection of the different theories in a common etiopathologic framework. These hypotheses, however, are based on generally low levels of evidence. Moreover, these studies are heterogeneous and confound performing a quantitative evaluation of the overall data reported. Despite this, we have presented and organized an account of the historical and current thinking on OCD of the knee in the English literature to better understand and compare the evidence to date. Confirmation and exploration of this framework by further study may allow further clarification of risk factors and mechanisms to be better identified. This in turn may enable customized treatment, and the development of more effective etiology-based therapies for OCD.
Footnotes
Acknowledgments and Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1. Tarabella V, Filardo G, Di Matteo B, Andriolo L, Tomba P, Viganò A, et al. From loose body to osteochondritis dissecans: a historical account of disease definition. Joints. 2016;4(3):165-70. doi: 10.11138/jts/2016.4.3.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Konig F. The classic: on loose bodies in the joint. 1887. Clin Orthop Relat Res. 2013;471(4):1107-15. doi: 10.1007/s11999-013-2824-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kocher MS, Tucker R, Ganley TJ, Flynn JM. Management of osteochondritis dissecans of the knee: current concepts review. Am J Sports Med. 2006;34(7):1181-91. doi: 10.1177/0363546506290127. [DOI] [PubMed] [Google Scholar]
- 4. Pareek A, Sanders TL, Wu IT, Larson DR, Saris DBF, Krych AJ. Incidence of symptomatic osteochondritis dissecans lesions of the knee: a population-based study in Olmsted County. Osteoarthritis Cartilage. 2017;25(10):1663-71. doi: 10.1016/j.joca.2017.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Crawford DC, Safran MR. Osteochondritis dissecans of the knee. J Am Acad Orthop Surg. 2006;14(2):90-100. [DOI] [PubMed] [Google Scholar]
- 6. Andriolo L, Candrian C, Papio T, et al. Osteochondritis Dissecans of the Knee - Conservative Treatment Strategies: A Systematic Review. Cartilage. 2018. doi: 10.1177/1947603518758435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cahill BR, Berg BC. 99m-Technetium phosphate compound joint scintigraphy in the management of juvenile osteochondritis dissecans of the femoral condyles. Am J Sports Med. 1983;11(5):329-35. [DOI] [PubMed] [Google Scholar]
- 8. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gorter J, van Raay JJ. A Suspected genetic form of bilateral osteochondritis dissecans of the knee in a Dutch family. Knee. 2015;22(6):677-82. doi: 10.1016/j.knee.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 10. Bruns J, Werner M, Soyka M. Is vitamin D insufficiency or deficiency related to the development of osteochondritis dissecans? Knee Surg Sports Traumatol Arthrosc. 2014;24(5):1575-9. doi: 10.1007/s00167-014-3413-7. [DOI] [PubMed] [Google Scholar]
- 11. Richie LB, Sytsma MJ. Matching osteochondritis dissecans lesions in identical twin brothers. Orthopedics. 2013;36(9):e1213-16. doi: 10.3928/01477447-20130821-27. [DOI] [PubMed] [Google Scholar]
- 12. Park NH, Kim HS, Yi SY, Min BC. Multiple osteochondritis dissecans of knee joint in a patient with Wilson disease, focusing on magnetic resonance findings. Knee Surg Relat Res. 2013;25(4):225-9. doi: 10.5792/ksrr.2013.25.4.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gans I, Sarkissian EJ, Grant SF, Ganley TJ. Identical osteochondritis dissecans lesions of the knee in sets of monozygotic twins. Orthopedics. 2013;36(12):e1559-e1562. [DOI] [PubMed] [Google Scholar]
- 14. Kroger L, Piippo-Savolainen E, Tyrvainen E, Penttila P, Kroger H. Osteochondral lesions in children with juvenile idiopathic arthritis. Pediatr Rheumatol Online J. 2013;11(1):18. doi: 10.1186/1546-0096-11-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jeong JH, Mascarenhas R, Yoon HS. Bilateral osteochondritis dissecans of the femoral condyles in both knees: a report of two sibling cases. Knee Surg Relat Res. 2013;25(2):88-92. doi: 10.5792/ksrr.2013.25.2.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Onoda S, Sugita T, Aizawa T, Ohnuma M, Takahashi A. Osteochondritis dissecans of the knee in identical twins: a report of two cases. J Orthop Surg (Hong Kong). 2012;20(1):108-10. [DOI] [PubMed] [Google Scholar]
- 17. Laor T, Zbojniewicz AM, Eismann EA, Wall EJ. Juvenile osteochondritis dissecans: is it a growth disturbance of the secondary physis of the epiphysis? AJR Am J Roentgenol. 2012;199(5):1121-28. doi: 10.2214/AJR.11.8085. [DOI] [PubMed] [Google Scholar]
- 18. Hussain WM, Hussain HM, Hussain MS, Ho SS. Human growth hormone and the development of osteochondritis dissecans lesions. Knee Surg Sports Traumatol Arthrosc. 2011;19(12):2108-10. doi: 10.1007/s00167-010-1370-3. [DOI] [PubMed] [Google Scholar]
- 19. Skagen PS, Horn T, Kruse HA, Staergaard B, Rapport MM, Nicolaisen T. Osteochondritis dissecans (OCD), an endoplasmic reticulum storage disease? A morphological and molecular study of OCD fragments. Scand J Med Sci Sports. 2011;21(6):e17-33. doi: 10.1111/j.1600-0838.2010.01128.x. [DOI] [PubMed] [Google Scholar]
- 20. Stattin EL, Wiklund F, Lindblom K, Onnerfjord P, Jonsson BA, Tegner Y, et al. A missense mutation in the aggrecan C-type lectin domain disrupts extracellular matrix interactions and causes dominant familial osteochondritis dissecans. Am J Hum Genet. 2010;86(2):126-37. doi: 10.1016/j.ajhg.2009.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jackson GC, Marcus-Soekarman D, Stolte-Dijkstra I, Verrips A, Taylor JA, Briggs MD. Type Ix collagen gene mutations can result in multiple epiphyseal dysplasia that is associated with osteochondritis dissecans and a mild myopathy. Am J Med Genet A. 2010;152A(4):863-9. doi: 10.1002/ajmg.a.33240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mackie T, Wilkins RM. Case report: osteochondritis dissecans in twins: treatment with fresh osteochondral grafts. Clin Orthop Relat Res. 2010;468(3):893-7. doi: 10.1007/s11999-009-1017-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Stattin EL, Tegner Y, Domellof M, Dahl N. Familial osteochondritis dissecans associated with early osteoarthritis and disproportionate short stature. Osteoarthritis Cartilage. 2008;16(8):890-6. doi: 10.1016/j.joca.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 24. Hanna SA, Aston WJ, Gikas PD, Briggs TW. Bicondylar osteochondritis dissecans in the knee: a report of two cases. J Bone Joint Surg Br. 2008;90(2):232-5. doi: 10.1302/0301-620X.90B2.19705. [DOI] [PubMed] [Google Scholar]
- 25. Cetik O, Turker M, Uslu M. Bilateral osteochondritis dissecans of lateral femoral condyle. Knee Surg Sports Traumatol Arthrosc. 2005;13(6):468-71. doi: 10.1007/s00167-004-0543-3. [DOI] [PubMed] [Google Scholar]
- 26. Gebarski K, Hernandez RJ. Stage-I osteochondritis dissecans versus normal variants of ossification in the knee in children. Pediatr Radiol. 2005;35(9):880-6. doi: 10.1007/s00247-005-1507-6. [DOI] [PubMed] [Google Scholar]
- 27. Kilic SS, Sanal O, Tezcan I, Ersoy F. Osteochondritis dissecans in a patient with hyperimmunoglobulin E syndrome. Turk J Pediatr. 2002;44(4):357-9. [PubMed] [Google Scholar]
- 28. Fonseca AS, Keret D, MacEwen GD. Familial osteochondritis dissecans. Orthopedics. 1990;13(11):1259-62. [DOI] [PubMed] [Google Scholar]
- 29. Barrie HJ. Hypothesis—a diagram of the form and origin of loose bodies in osteochondritis dissecans. J Rheumatol. 1984;11(4):512-3. [PubMed] [Google Scholar]
- 30. Mubarak SJ, Carroll NC. Juvenile osteochondritis dissecans of the knee: etiology. Clin Orthop Relat Res. 1981(157):200-11. [PubMed] [Google Scholar]
- 31. Campbell CJ, Ranawat CS. Osteochondritis dissecans: the question of etiology. J Trauma. 1966;6(2):201-21. [PubMed] [Google Scholar]
- 32. Tobin WJ. Familial osteochondritis dissecans with associated tibia vara. J Bone Joint Surg Am. 1957;39-A(5):1091-1105. [PubMed] [Google Scholar]
- 33. Pick MP. Familial osteochondritis dissecans. J Bone Joint Surg Br. 1955;37-B(1):142-5. [DOI] [PubMed] [Google Scholar]
- 34. Ribbing S. The hereditary multiple epiphyseal disturbance and its consequences for the aetiogenesis of local malacias—particularly the osteochondrosis dissecans. Acta Orthop Scand. 1955;24(4):286-99. [DOI] [PubMed] [Google Scholar]
- 35. Green WT, Banks HH. Osteochondritis dissecans in children. J Bone Joint Surg Am. 1953;35-A(1):26-47. [PubMed] [Google Scholar]
- 36. White J. Osteochondritis dissecans in association with dwarfism. J Bone Joint Surg Br. 1957;39-B(2):261-7. [DOI] [PubMed] [Google Scholar]
- 37. Stougaard J. Familial occurrence of osteochondritis dissecans. J Bone Joint Surg Br. 1964;46:542-3. [PubMed] [Google Scholar]
- 38. Hanley WB, McKusick VA, Barranco FT. Osteochondritis dissecans with associated malformations in two brothers. A review of familial aspects. J Bone Joint Surg Am. 1967;49(5):925-37. [PubMed] [Google Scholar]
- 39. Mubarak SJ, Carroll NC. Familial osteochondritis dissecans of the knee. Clin Orthop Relat Res. 1979(140):131-6. [PubMed] [Google Scholar]
- 40. Andrew TA, Spivey J, Lindebaum RH. Familial osteochondritis dissecans and dwarfism. Acta Orthop Scand. 1981;52(5):519-23. [DOI] [PubMed] [Google Scholar]
- 41. Phillips HO, Grubb SA. Familial multiple osteochondritis dissecans. Report of a Kindred. J Bone Joint Surg Am. 1985;67(1):155-6. [PubMed] [Google Scholar]
- 42. Quan AW, Beall DP, Berry ER, Ly JQ, Sweet CF, Fish JR. A case of osteochondritis dissecans in rickets. Emerg Radiol. 2005;11(4):219-21. doi: 10.1007/s10140-004-0387-7. [DOI] [PubMed] [Google Scholar]
- 43. Krause M, Lehmann D, Amling M, Rolvien T, Frosch KH, Puschel K, et al. Intact bone vitality and increased accumulation of nonmineralized bone matrix in biopsy specimens of juvenile osteochondritis dissecans: a histological analysis. Am J Sports Med. 2015;43(6):1337-47. doi: 10.1177/0363546515572579. [DOI] [PubMed] [Google Scholar]
- 44. Yellin JL, Trocle A, Grant SF, Hakonarson H, Shea KG, Ganley TJ. Candidate loci are revealed by an initial genome-wide association study of juvenile osteochondritis dissecans. J Pediatr Orthop. 2017;37(1):e32-6. doi: 10.1097/BPO.0000000000000660. [DOI] [PubMed] [Google Scholar]
- 45. Ellermann J, Johnson CP, Wang L, Macalena JA, Nelson BJ, LaPrade RF. Insights into the epiphyseal cartilage origin and subsequent osseous manifestation of juvenile osteochondritis dissecans with a modified clinical MR imaging protocol: a pilot study. Radiology. 2017;282(3):798-806. doi: 10.1148/radiol.2016160071. [DOI] [PubMed] [Google Scholar]
- 46. Gornitzky AL, Mistovich RJ, Atuahuene B, Storey EP, Ganley TJ. Osteochondritis dissecans lesions in family members: does a positive family history impact phenotypic potency? Clin Orthop Relat Res. 2017;475(6):1573-80. doi: 10.1007/s11999-016-5059-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Livesley PJ, Milligan GF. Osteochondritis dissecans patellae. Is there a genetic predisposition? Int Orthop. 1992;16(2):126-9. [PubMed] [Google Scholar]
- 48. Linden B. Osteochondritis dissecans of the femoral condyles: a long-term follow-up study. J Bone Joint Surg Am. 1977;59(6):769-76. [PubMed] [Google Scholar]
- 49. Chow RM, Guzman MS, Dao Q. Intercondylar notch width as a risk factor for medial femoral condyle osteochondritis dissecans in skeletally immature patients. J Pediatr Orthop. 2016;36(6):640-4. doi: 10.1097/BPO.0000000000000511. [DOI] [PubMed] [Google Scholar]
- 50. Deroussen F, Hustin C, Moukoko D, Collet LM, Gouron R. Osteochondritis dissecans of the lateral tibial condyle associated with agenesis of both cruciate ligaments. Orthopedics. 2014;37(2):e218-20. doi: 10.3928/01477447-20140124-30. [DOI] [PubMed] [Google Scholar]
- 51. Mine T, Ihara K, Kawamura H, Date R, Chagawa K. Unusual appearance of an osteochondral lesion accompanying medial meniscus injury. Arthrosc Tech. 2014;3(1):e111-e114. doi: 10.1016/j.eats.2013.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Wechter JF, Sikka RS, Alwan M, Nelson BJ, Tompkins M. Proximal tibial morphology and its correlation with osteochondritis dissecans of the knee. Knee Surg Sports Traumatol Arthrosc. 2014;23(12):3717-22. doi: 10.1007/s00167-014-3289-6. [DOI] [PubMed] [Google Scholar]
- 53. Camathias C, Hirschmann MT, Vavken P, Rutz E, Brunner R, Gaston MS. Meniscal suturing versus screw fixation for treatment of osteochondritis dissecans: clinical and magnetic resonance imaging results. Arthroscopy. 2014;30(10):1269-79. doi: 10.1016/j.arthro.2014.05.010. [DOI] [PubMed] [Google Scholar]
- 54. Maruyama Y, Kaneko K, Baba T. A case of osteochondritis dissecans of the lateral femoral condyle and patellofemoral joint surface occurring in the same knee. Eur Orthop Traumatol. 2014;5:171-4. doi: 10.1007/s12570-013-0227-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Shea KG, Jacobs JC, Jr, Grimm NL, Pfeiffer RP. Osteochondritis dissecans development after bone contusion of the knee in the skeletally immature: a case series. Knee Surg Sports Traumatol Arthrosc. 2013;21(2):403-7. doi: 10.1007/s00167-012-1983-9. [DOI] [PubMed] [Google Scholar]
- 56. Kamei G, Adachi N, Deie M, Nakamae A, Nakasa T, Shibuya H, et al. Characteristic shape of the lateral femoral condyle in patients with osteochondritis dissecans accompanied by a discoid lateral meniscus. J Orthop Sci. 2012;17(2):124-8. doi: 10.1007/s00776-011-0190-8. [DOI] [PubMed] [Google Scholar]
- 57. Grimm NL, Tisano B, Carey JL. Three osteochondritis dissecans lesions in one knee: a case report. Clin Orthop Relat Res. 2013;471(4):1186-90. doi: 10.1007/s11999-012-2324-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Jans L, Jaremko J, Ditchfield M, De Coninck T, Huysse W, Moon A, et al. Ossification variants of the femoral condyles are not associated with osteochondritis dissecans. Eur J Radiol. 2012;81(11):3384-9. doi: 10.1016/j.ejrad.2012.01.009. [DOI] [PubMed] [Google Scholar]
- 59. Jacobi M, Wahl P, Bouaicha S, Jakob RP, Gautier E. Association between mechanical axis of the leg and osteochondritis dissecans of the knee: radiographic study on 103 knees. Am J Sports Med. 2010;38(7):1425-8. doi: 10.1177/0363546509359070. [DOI] [PubMed] [Google Scholar]
- 60. Yonetani Y, Nakamura N, Natsuume T, Shiozaki Y, Tanaka Y, Horibe S. Histological evaluation of juvenile osteochondritis dissecans of the knee: a case series. Knee Surg Sports Traumatol Arthrosc. 2010;18(6):723-30. doi: 10.1007/s00167-009-0898-6. [DOI] [PubMed] [Google Scholar]
- 61. Uozumi H, Sugita T, Aizawa T, Takahashi A, Ohnuma M, Itoi E. Histologic findings and possible causes of osteochondritis dissecans of the knee. Am J Sports Med. 2009;37(10):2003-8. doi: 10.1177/0363546509346542. [DOI] [PubMed] [Google Scholar]
- 62. Lippi D, Matucci-Cerinic M, Villari N, Fornaciari G, Mascalchi M. Osteochondritis dissecans of the patella in a XVII century player of the Florentine historic kickball. Knee. 2010;17(2):172-3. doi: 10.1016/j.knee.2009.07.016. [DOI] [PubMed] [Google Scholar]
- 63. Beyzadeoglu T, Gokce A, Bekler H. Osteochondritis dissecans of the medial femoral condyle associated with malformation of the menisci. Orthopedics. 2008;31(5):504. [DOI] [PubMed] [Google Scholar]
- 64. Hashimoto Y, Yoshida G, Tomihara T, Matsuura T, Satake S, Kaneda K, et al. Bilateral osteochondritis dissecans of the lateral femoral condyle following bilateral total removal of lateral discoid meniscus: a case report. Arch Orthop Trauma Surg. 2008;128(11):1265-8. doi: 10.1007/s00402-007-0499-0. [DOI] [PubMed] [Google Scholar]
- 65. Deie M, Ochi M, Sumen Y, Kawasaki K, Adachi N, Yasunaga Y, et al. Relationship between osteochondritis dissecans of the lateral femoral condyle and lateral menisci types. J Pediatr Orthop. 2006;26(1):79-82. doi: 10.1097/01.bpo.0000191554.34197.fd. [DOI] [PubMed] [Google Scholar]
- 66. Stanitski CL, Bee J. Juvenile osteochondritis dissecans of the lateral femoral condyle after lateral discoid meniscal surgery. Am J Sports Med. 2004;32(3):797-801. [DOI] [PubMed] [Google Scholar]
- 67. Bramer JA, Maas M, Dallinga RJ, te Slaa RL, Vergroesen DA. Increased external tibial torsion and osteochondritis dissecans of the knee. Clin Orthop Relat Res. 2004(422):175-9. [DOI] [PubMed] [Google Scholar]
- 68. Hughes JA, Cook JV, Churchill MA, Warren ME. Juvenile osteochondritis dissecans: a 5-year review of the natural history using clinical and MRI evaluation. Pediatr Radiol. 2003;33(6):410-7. doi: 10.1007/s00247-003-0876-y. [DOI] [PubMed] [Google Scholar]
- 69. Mizuta H, Nakamura E, Otsuka Y, Kudo S, Takagi K. Osteochondritis dissecans of the lateral femoral condyle following total resection of the discoid lateral meniscus. Arthroscopy. 2001;17(6):608-12. doi: 10.1053/jars.2001.19979. [DOI] [PubMed] [Google Scholar]
- 70. Atay OA, Aydingoz U, Doral MN, Tetik O, Leblebicioglu G. Symptomatic ring-shaped lateral meniscus: magnetic resonance imaging and arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2002;10(5):280-3. doi: 10.1007/s00167-002-0292-0. [DOI] [PubMed] [Google Scholar]
- 71. Bruns J, Luessenhop S, Lehmann L. Etiological aspects in osteochondritis dissecans patellae. Knee Surg Sports Traumatol Arthrosc. 1999;7(6):356-9. doi: 10.1007/s001670050180. [DOI] [PubMed] [Google Scholar]
- 72. Mitsuoka T, Shino K, Hamada M, Horibe S. Osteochondritis dissecans of the lateral femoral condyle of the knee joint. Arthroscopy. 1999;15(1):20-6. doi: 10.1053/ar.1999.v15.015002. [DOI] [PubMed] [Google Scholar]
- 73. Mitsuoka T, Horibe S, Hamada M. Osteochondritis dissecans of the medial femoral condyle associated with congenital hypoplasia of the lateral meniscus and anterior cruciate ligament. Arthroscopy. 1998;14(6):630-3. [DOI] [PubMed] [Google Scholar]
- 74. Raber DA, Friederich NF, Hefti F. Discoid lateral meniscus in children. Long-term follow-up after total meniscectomy. J Bone Joint Surg Am. 1998;80(11):1579-86. [DOI] [PubMed] [Google Scholar]
- 75. Koch S, Kampen WU, Laprell H. Cartilage and bone morphology in osteochondritis dissecans. Knee Surg Sports Traumatol Arthrosc. 1997;5(1):42-5. doi: 10.1007/s001670050023. [DOI] [PubMed] [Google Scholar]
- 76. Aichroth PM, Patel DV, Marx CL. Congenital discoid lateral meniscus in children. A follow-up study and evolution of management. J Bone Joint Surg Br. 1991;73(6):932-6. [DOI] [PubMed] [Google Scholar]
- 77. Desai SS, Patel MR, Michelli LJ, Silver JW, Lidge RT. Osteochondritis dissecans of the patella. J Bone Joint Surg Br. 1987;69(2):320-5. [DOI] [PubMed] [Google Scholar]
- 78. Irani RN, Karasick D, Karasick S. A possible explanation of the pathogenesis of osteochondritis dissecans. J Pediatr Orthop. 1984;4(3):358-60. [DOI] [PubMed] [Google Scholar]
- 79. Milgram JW. Radiological and pathological manifestations of osteochondritis dissecans of the distal femur. A study of 50 cases. Radiology. 1978;126(2):305-11. doi: 10.1148/126.2.305. [DOI] [PubMed] [Google Scholar]
- 80. Edwards DH, Bentley G. Osteochondritis dissecans patellae. J Bone Joint Surg Br. 1977;59(1):58-63. [DOI] [PubMed] [Google Scholar]
- 81. Chiroff RT, Cooke CP., 3rd Osteochondritis dissecans: a histologic and microradiographic analysis of surgically excised lesions. J Trauma. 1975;15(8):689-96. [PubMed] [Google Scholar]
- 82. Kilcoyne KG, Dickens JF, Rue JP, Keblish DJ. Bilateral combined discoid lateral menisci and lateral femoral condyle osteochondritis dissecans lesions in a division I varsity athlete: a case report. J Knee Surg. 2013;26(Suppl 1):S58-62. doi: 10.1055/s-0031-1299657. [DOI] [PubMed] [Google Scholar]
- 83. Sebaaly A, Boueri W, Nabhane L. Bilateral Wrisberg discoid menisci mimicking bucket handle tears associated with osteochondritis dissecans: case report. J Pediatr Orthop B. 2015;24(1):75-8. doi: 10.1097/BPB.0000000000000094. [DOI] [PubMed] [Google Scholar]
- 84. Cavaignac E, Perroncel G, Thepaut M, Vial J, Accadbled F, De Gauzy JS. Relationship between tibial spine size and the occurrence of osteochondritis dissecans: an argument in favour of the impingement theory. Knee Surg Sports Traumatol Arthrosc. 2017;25(8):2442-6. doi: 10.1007/s00167-015-3907-y. [DOI] [PubMed] [Google Scholar]
- 85. Toth F, Nissi MJ, Ellermann JM, Wang L, Shea KG, Polousky J, et al. Novel application of magnetic resonance imaging demonstrates characteristic differences in vasculature at predilection sites of osteochondritis dissecans. Am J Sports Med. 2015;43(10):2522-7. doi: 10.1177/0363546515596410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Persiani P, Di Domenica M, Martini L, Ranaldi FM, Zambrano A, Celli M, et al. Osteochondritis dissecans of the lateral femoral condyle in a patient affected by osteogenesis imperfecta: a case report. J Pediatr Orthop B. 2015;24(6):521-5. doi: 10.1097/BPB.0000000000000180. [DOI] [PubMed] [Google Scholar]
- 87. McElroy MJ, Riley PM, Tepolt FA, Nasreddine AY, Kocher MS. Catcher’s knee: posterior femoral condyle juvenile osteochondritis dissecans in children and adolescents. J Pediatr Orthop. 2018;38(8):410-7. doi: 10.1097/BPO.0000000000000839. [DOI] [PubMed] [Google Scholar]
- 88. Ishikawa M, Adachi N, Yoshikawa M, Nakamae A, Nakasa T, Ikuta Y, et al. Unique anatomic feature of the posterior cruciate ligament in knees associated with osteochondritis dissecans. Orthop J Sports Med. 2016;4(5):2325967116648138. doi: 10.1177/2325967116648138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Ishikawa M, Adachi N, Nakamae A, Deie M, Ochi M. Progression of stable juvenile osteochondritis dissecans after 10 years of meniscectomy of the discoid lateral meniscus. J Pediatr Orthop B. 2017;26(5):487-90. doi: 10.1097/BPB.0000000000000316. [DOI] [PubMed] [Google Scholar]
- 90. Takigami J, Hashimoto Y, Tomihara T, Yamasaki S, Tamai K, Kondo K, et al. Predictive factors for osteochondritis dissecans of the lateral femoral condyle concurrent with a discoid lateral meniscus. Knee Surg Sports Traumatol Arthrosc. 2018;26(3):799-805. doi: 10.1007/s00167-017-4451-8. [DOI] [PubMed] [Google Scholar]
- 91. Gonzalez-Herranz P, Rodriguez ML, de la, Fuente C. Femoral osteochondritis of the knee: prognostic value of the mechanical axis. J Child Orthop. 2017;11(1):1-5. doi: 10.1302/1863-2548-11-160173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Kumahashi N, Matsumoto A, Kuwata S, Kadowaki M, Uchio Y. Sporadically occurred bilateral osteochondritis dissecans on the trochlea of the femur: case report. J Pediatr Orthop B. 2017;26(5):482-6. doi: 10.1097/BPB.0000000000000398. [DOI] [PubMed] [Google Scholar]
- 93. Kozlowski K, Middleton R. Familial osteochondritis dissecans: a dysplasia of articular cartilage? Skeletal Radiol. 1985;13(3):207-10. [DOI] [PubMed] [Google Scholar]
- 94. Petrie PW. Aetiology of osteochondritis dissecans. Failure to establish a familial background. J Bone Joint Surg Br. 1977;59(3):366-7. [DOI] [PubMed] [Google Scholar]
- 95. Nambu T, Gasser B, Schneider E, Bandi W, Perren SM. Deformation of the distal femur: a contribution towards the pathogenesis of osteochondrosis dissecans in the knee joint. J Biomech. 1991;24(6):421-33. [DOI] [PubMed] [Google Scholar]
- 96. Smillie IS. Treatment of osteochondritis dissecans. J Bone Joint Surg Br. 1957;39-B(2):248-60. [DOI] [PubMed] [Google Scholar]