Abstract
Background
The effectiveness of personal health records (PHRs) in diabetes management has already been verified in several clinical trials; however, evidence of their effectiveness in real-world scenarios is also necessary. To provide solid real-world evidence, an analysis that is more accurate than the analyses solely based on patient-generated health data should be conducted.
Objective
This study aimed to conduct a more accurate analysis of the effectiveness of using PHRs within electronic medical records (EMRs). The results of this study will provide precise real-world evidence of PHRs as a feasible diabetes management tool.
Methods
We collected log data of the sugar function in the My Chart in My Hand version 2.0 (MCMH 2.0) app from Asan Medical Center (AMC), Seoul, Republic of Korea, between December 2015 and April 2018. The EMR data of MCMH 2.0 users from AMC were collected and integrated with the PHR data. We classified users according to whether they were continuous app users. We analyzed and compared their characteristics, patterns of hemoglobin A1c (HbA1c) levels, and the proportion of successful HbA1c control. The following confounders were adjusted for HbA1c pattern analysis and HbA1c regulation proportion comparison: age, sex, first HbA1c measurement, diabetes complications severity index score, sugar function data generation weeks, HbA1c measurement weeks before MCMH 2.0 start, and generated sugar function data count.
Results
The total number of MCMH 2.0 users was 64,932, with 7453 users having appropriate PHRs and diabetes criteria. The number of continuous and noncontinuous users was 133 and 7320, respectively. Compared with noncontinuous users, continuous users were younger (P<.001) and had a higher male proportion (P<.001). Furthermore, continuous users had more frequent HbA1c measurements (P=.007), shorter HbA1c measurement days (P=.04), and a shorter period between the first HbA1c measurement and MCMH 2.0 start (P<.001). Diabetes severity–related factors were not statistically significantly different between the two groups. Continuous users had a higher decrease in HbA1c (P=.02) and a higher proportion of regulation of HbA1c levels to the target level (P=.01). After adjusting the confounders, continuous users had more decline in HbA1c levels than noncontinuous users (P=.047). Of the users who had a first HbA1c measurement higher than 6.5% (111 continuous users and 5716 noncontinuous users), continuous users had better regulation of HbA1c levels with regard to the target level, 6.5%, which was statistically significant (P=.04).
Conclusions
By integrating and analyzing patient- and clinically generated data, we demonstrated that the continuous use of PHRs improved diabetes management outcomes. In addition, the HbA1c reduction pattern was prominent in the PHR continuous user group. Although the continued use of PHRs has proven to be effective in managing diabetes, further evaluation of its effectiveness for various diseases and a study on PHR adherence are also required.
Keywords: personal health record, mobile health, electronic medical record, diabetes mellitus, glycated hemoglobin A
Introduction
Background
Diabetes mellitus is a global issue, and its contribution to numerous complications and increased mortality is well known. Moreover, diabetes prevalence is constantly growing, a trend that might continue until 2030 or longer [1,2]. According to the American Diabetes Association (ADA), diabetes care is mainly based on insulin delivery [3]. According to the Korean Diabetes Association (KDA), the target value of hemoglobin A1c (HbA1c) is recommended to be 6.5% for patients with type 2 diabetes, and antihyperglycemic therapy is mainly considered in Korea. Metformin is considered to be the first-line therapy. However, these traditional drug therapies result in inevitable hypoglycemic events and body weight change. An unachieved glycemic target can only be solved by increasing drugs in mono, dual, or triple therapy [4]. Traditional methods are expensive, and this is becoming a national health care problem [5,6]. To overcome several limitations of traditional diabetes management, mobile health (mHealth) technology and personal health record (PHR) implementation have been suggested as innovative solutions.
In the diabetes management market, new treatments with new devices and apps are being introduced. Most functions of diabetes apps focus on maintaining a blood glucose diary. Some are also connected with blood glucose sensors and treatment devices. Among diabetes apps, OneTouch Reveal had the best validation [7]. This app is wirelessly connected to the OneTouch Verio Flex meter, making users self-monitor their blood glucose. Blood glucose data are delivered to health care professionals, and users receive text message feedback [8]. Technologies using automatic alarm systems have also been introduced. The Dexcom G6 Continuous Glucose Monitoring system effectively reduced hyperglycemia and also hypoglycemic events with the Urgent Low Soon automatic alert system [9]. Monitoring insulin delivery became possible with internet-based connections. NovoPen 6 and NovoPen Echo Plus are called smart insulin pens, which can monitor the insulin injection amount and provide both health providers and patients treatment accuracy [10,11].
Previous studies have shown the health improvement of PHR users, thus suggesting that a digital health care system is feasible for improving health behavior and chronic conditions. According to a systematic review, users experienced a positive effect on their health-related behavior and clinical results when using health apps on their mobile devices [12]. Another systematic review in South Korea showed that mHealth interventions were effective in improving self-management behaviors, biomarkers, or patient-reported outcome measures [13]. However, the positive effect of mHealth and PHR interventions is not always ensured.
In diabetes care, PHR and mHealth interventions are expected to be effective treatments. WellDoc, a remote blood glucose monitoring system, was effective in lowering HbA1c levels, thereby improving clinical, behavioral, and diabetes knowledge outcomes [14]. A phone-based treatment and behavioral coaching intervention also improved HbA1c levels [15]. A similar improvement in HbA1c control for type 2 diabetes was seen with another mobile-based intervention [16]. The addition of a tailored mobile coaching system for patients with diabetes showed reduced HbA1c levels and improved diabetes self-management; the results were reproducible and durable [17].
Along with the expectations of the clinical implications of PHRs, some concerns and slightly controversial results have been reported. Despite its advantages, studies have reported the barriers in PHR implementation. Patients are concerned about the security of their health information. Health care providers are concerned about patients altering their own PHR information. Other issues are that there is no practical difference in health outcomes, the use of stand-alone PHRs with electronic medical records (EMRs) and electronic health records, and a low health care literacy rate, which can diminish the benefits of PHRs [18]. Moreover, the barriers associated with patients’ age, sex, socioeconomic status, education level, internet and computer access, and health have been reviewed [19]. Contrasting results of the relation between PHR use and diabetes management have been reported. A study using a regression model claimed that there was no association between the increasing number of days of PHR use and better diabetes quality measure profiles [20].
Objectives
In this study, we used a 4-year mobile PHR (mPHR) log and users’ EMR data to analyze the effects of diabetes management on the continuous use of the PHR system distributed by a tertiary hospital in South Korea. A study with the earlier version of the mPHR app was conducted to verify characteristics of continuous users [21], and patient-generated health data (PGHD) of continuous users had a higher proportion of a chronic disease diagnosis, such as diabetes, than noncontinuous users [22]. With the new version, we will verify its effect in glycemic control on patients with diabetes. To the best of our knowledge, this is the first study to verify the effectiveness of disease management by integrating a long-term mPHR log and EMR data.
Methods
Data and Mobile Personal Health Record Description
We collected log data from an mPHR app called My Chart in My Hand (MCMH) and their EMR data at the Asan Medical Center (AMC), which is the largest general hospital in South Korea. Launched in January 2011, MCMH is the first mPHR in South Korea; it enables patients to view and manage their own health records [21]. We used the MCMH version 1.0 log to identify patterns of continuous generation of PGHD in specific populations [22]. This study performed a diabetes management analysis using the MCMH version 2.0 log and EMR data. For patients with diabetes, MCMH version 2.0 provides sugar, diabetes calendar, insulin treatment, food intake, and exercise input functions. Among these functions, we only used the log data of the sugar and diabetes calendar function; the remaining functions had very few records. The items in Figure 1 show the details of the sugar function. Users enter the date, time, situation, and result of their blood glucose measurement in these PGHD functions.
Figure 1.
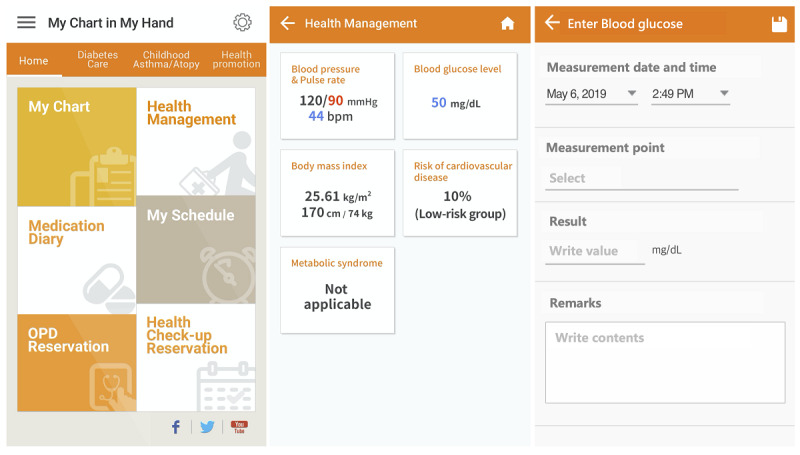
Screenshots of My Chart in My Hand version 2.0. Inputting data in the sugar function follows from the home page to Enter Blood Glucose.
We also gathered demographic and medical record information of patients, such as age, sex, residence, and health information, including hospital visits, HbA1c level, diagnosis, and medication data, using our clinical research data warehouse.
Study Design
MCMH version 2.0 replaced MCMH version 1.0 on December 31, 2015, but some patients had already created their accounts in December 2015 before the replacement. For each user, the records generated in MCMH version 2.0 functions were analyzed, but only records generated after account creation were used.
The user log of the sugar function contained user access ID and time stamps of data input. We gathered the HbA1c measurement results of MCMH version 2.0 users from January 2014 to November 2018.
For user selection, we used the criteria of diabetes for diagnosis. First, the criterion of Glasheen et al [23] was adopted: a user should have one or more International Classification of Diseases 10th Revision (ICD-10) diabetes codes in the diagnosis record, which are E08, E09, E10, E11, and E13. Second, the HbA1c cutoff value of 6.5% for diagnosing diabetes was used [24]. For the complication classification and diabetes complications severity index (DCSI) scoring, the selected complication fields from the diagnosis record were retinopathy, nephropathy, neuropathy, cerebrovascular, cardiovascular, peripheral vascular disease, and metabolic complications. DCSI scoring used the criteria of the study by Glasheen et al [23]. However, urine laboratory data were not included in DCSI scoring because of its unavailability. Above all, we classified all diseases according to ICD-10.
The criterion for whether a user was a continuous user was adopted from the PGHD pattern analysis study of MCMH version 1.0: a user entering data in the sugar function at least once per week and doing so for at least four weeks (28 days) [22].
We analyzed the pattern of HbA1c levels with the trend line slope of HbA1c levels. The fluctuation of HbA1c levels was compared with the r-squared value of the trend line and the standard deviation of the patient’s HbA1c level.
In this study, the trend line slope considerably depended on the measurement days between the first and last HbA1c measurement. Therefore, we created a patient filter called appropriate HbA1c measurement. This criterion excluded patients with short periods between measures because a short period will lead to an exaggeratedly steep slope, which is inappropriate for the analysis. The criterion for an appropriate HbA1c measurement is patients should have at least two HbA1c measurements and the period between the first and last HbA1c measurement should be over 100 days. To normalize the effect of measurement days between the first and last HbA1c measurement, we defined a variable called decline. Decline is defined as a trend line slope times the period (in days) divided by 100. This normalization is represented in the equation in Multimedia Appendix 1.
This study was approved by the Institutional Review Board (IRB) of the AMC (IRB number: 2018-0321). The need for informed consent was waived by the ethics committee because this study utilized routinely collected log data that were anonymously managed at all stages, including during data cleaning and statistical analyses.
Study Participants
Figure 2 shows the patient selection flow in this study. Among 64,932 users who downloaded and created an MCMH version 2.0 account, we first excluded 51,433 users with inappropriate HbA1c measurements. We considered 13,499 users with the appropriate HbA1c measurements, excluded 6046 users without diabetes, and selected 7453 users with diabetes.
Figure 2.
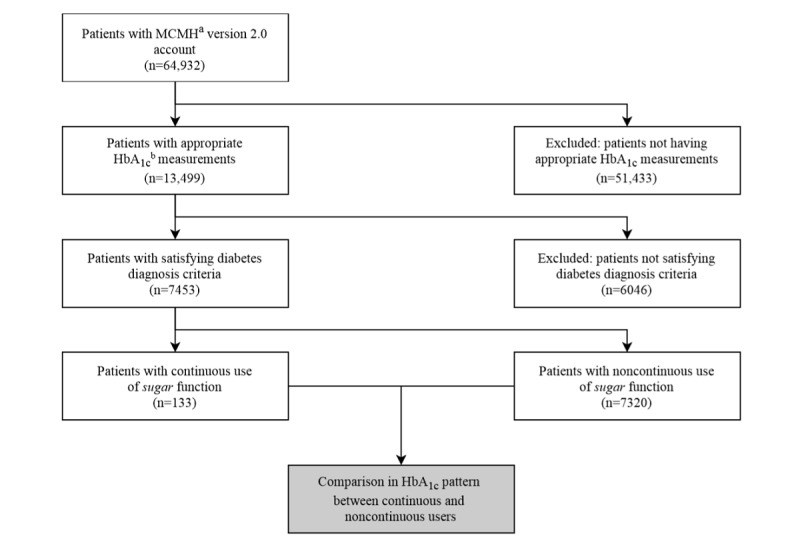
Patient inclusion and exclusion criteria (white boxes) and flow through the study. The gray box shows user hemoglobin A1c (HbA1c) analyses. Criteria for appropriate HbA1c measurement: two or more HbA1c measurements, duration of the first and last measurement over 100 days, and creating My Chart in My Hand version 2.0 account during HbA1c measurement. Criteria for diabetes diagnosis: having International Classification of Diseases 10th Revision code E08, E09, E10, E11, or E13 or first HbA1c measurement ≥6.5%. Criteria for continuous use of sugar function: patient-generated health data entered in the sugar function at least once per week and used for at least 28 days. aHbA1c: hemoglobin A1c; bMCMH: My Chart in My Hand.
Data Analysis
We first compared the general characteristics of continuous (n=133) and noncontinuous users (n=7320). The following characteristics were compared: age, gender proportion, sugar and diabetes calendar function use pattern, HbA1c measurement pattern, HbA1c value, DCSI score, and complication proportion. A Student t test was conducted for the comparison of age, the number of HbA1c measurements, measurement days, and measurement days before MCMH version 2.0 start. A Wilcoxon rank-sum test was used for individual sugar and diabetes calendar function data generation, HbA1c measure frequency, first HbA1c measurement, and DCSI score comparison. The median test was used for the individual sugar and diabetes calendar function data generation comparison. The Z test was conducted for sugar and diabetes function generation user proportion, first HbA1c measurement over 6.5% proportion, and complications proportion comparisons. For gender proportion comparison and DCSI score distribution, a chi-square test was used.
Next, comparative analyses of HbA1c decline, r-squared value, and standard deviation between continuous and noncontinuous users were performed. We used the Shapiro-Wilk test and D’Agostino K-squared test to determine if these data followed a normal distribution. HbA1c decline, r-squared value, and standard deviation were compared using the Wilcoxon rank-sum test. For confounder adjustment, we used an analysis of covariance (ANCOVA) with some variables: continuous use, age, sex, first HbA1c measurement, DCSI, sugar function data generation weeks, HbA1c measurement in weeks before MCMH version 2.0 start, and sugar function data generation count.
Finally, the Z test was conducted for comparing the proportions of 4 groups between continuous and noncontinuous users. The 4 groups were divided by whether the first HbA1c measurement was higher or lower than 6.5% and whether the last HbA1c measurement was higher or lower than 6.5%. For confounder adjustment, multivariable logistic regression was used for users with the first HbA1c measurement over 6.5%. The same variables, as used in ANCOVA, were used for logistic regression. Data analyses were conducted using Python 3.6.7, with Jupyter Notebook.
Results
Overall Characteristics
Within 29 months of operation of MCMH version 2.0, 64,932 users created an account and logged in at least once. Among these users, 7453 users were selected on the basis of the inclusion criteria of this study. Approximately 1.78% (133/7453) of these users were continuous users, and 98.22% (7320/7453) were noncontinuous users. Continuous and noncontinuous users had no statistically significant difference in the number of HbA1c measurements and the period between the first and last HbA1c measurements.
Table 1 summarizes the results of a basic characteristic analysis between continuous and noncontinuous users. In Table 1, measure frequency refers to the number of measurements per day, measurement days refers to days between the first and last HbA1c measurement, and measurement days before MCMH version 2.0 start refers to days between the first HbA1c measurement and MCMH version 2.0 account generation period. Compared with noncontinuous users, continuous users were younger (mean 53.59, SD 9.89 years vs mean 57.58, SD 11.95 years, respectively) and had a higher male proportion (110/133, 82.7% vs 4859/7320, 66.38%, respectively), which was statistically significant (both P<.001). The number of HbA1c measurements was not significantly different. The frequency and period between the first and last measurements exhibited a significant difference between continuous and noncontinuous users (P=.007 and P=.04, respectively). The proportion of patients with the first HbA1c measurement below 6.5% had no significant difference (P=.14), but continuous users had a higher first HbA1c measurement, and this was statistically significant (P=.01). Furthermore, among continuous users, there were a higher proportion of users who generated data in the sugar function and diabetes calendar function (both P<.001). Continuous users also entered more sugar and diabetes calendar data (both P<.001). The DCSI score had no significant difference (P=.99). The proportion of complications, defined by the DCSI criteria, also showed no significant difference between continuous and noncontinuous users. Although the difference was statistically insignificant, retinopathy and cardiovascular complications had a proportional difference.
Table 1.
General characteristics of continuous and noncontinuous users.
| Variables | Users | Total (N=7453) | P valuea | ||||
|
|
Continuous (n=133) | Noncontinuous (n=7320) |
|
|
|||
| Age (years), mean (SD) | 53.59 (9.89) | 57.58 (11.95) | 57.51 (11.92) | <.001 | |||
| Sex, n (%) | <.001 | ||||||
|
|
Male | 110 (82.7) | 4859 (66.37) | 4969 (66.67) |
|
||
|
|
Female | 23 (17.3) | 2461 (33.62) | 2484 (33.33) |
|
||
| Sugar function | |||||||
|
|
Data generated by users, n (%) | 133 (100.0) | 289 (3.95) | 422 (5.66) | <.001 | ||
|
|
Total data generated, n | 22,350 | 1345 | 23,695 | —b | ||
|
|
Individually generated data | <.001 | |||||
|
|
|
Mean (SD) | 168.0 (204.0) | 0.2 (1.8) | 3.2 (35.1) |
|
|
|
|
|
Median (IQR) | 97 (43-186) | 0 (0-0) | 0 (0-0) |
|
|
| Diabetes calendar function | |||||||
|
|
Data generated by users, n (%) | 133 (100.0) | 297 (4.06) | 430 (5.77) | <.001 | ||
|
|
Total data generated, n | 16,407 | 1453 | 17,860 | — | ||
|
|
Individually generated data | <.001 | |||||
|
|
|
Mean (SD) | 123.4 (143.3) | 0.2 (4.0) | 2.4 (25.4) |
|
|
|
|
|
Median (IQR) | 67 (35-145) | 0 (0-0) | 0 (0-0) |
|
|
| HbA1cc , mean (SD) | |||||||
|
|
Number of measurements | 12.44 (6.90) | 11.90 (6.82) | 11.92 (6.82) | .38 | ||
|
|
Measure frequency | 0.011 (0.010) | 0.009 (0.005) | 0.009 (0.005) | .007 | ||
|
|
Measurement days | 1254 (461) | 1336 (445) | 1335 (446) | .04 | ||
|
|
Measurement days before MCMHd version 2.0 start | 546 (348) | 712 (377) | 710 (377) | <.001 | ||
| First HbA1c measurement ≥6.5%, n (%) | 111 (83.4) | 5716 (78.09) | 5827 (78.18) | .14 | |||
| First HbA1c measurement, mean (SD) | 7.86 (1.78) | 7.51 (1.62) | 7.51 (1.62) | .01 | |||
| DCSIe, mean (SD) | 1.17 (1.65) | 1.15 (1.64) | 1.15 (1.64) | .99 | |||
| Complications, n (%) | |||||||
|
|
Retinopathy or ophthalmic | 31 (23.3) | 1516 (20.71) | 1547 (20.75) | .46 | ||
|
|
Nephropathy | 13 (9.8) | 765 (10.45) | 778 (10.44) | .80 | ||
|
|
Neuropathy | 23 (17.3) | 1267 (17.31) | 1290 (17.31) | >.99 | ||
|
|
Cerebrovascular | 20 (15.0) | 950 (13.00) | 970 (13.01) | .48 | ||
|
|
Cardiovascular | 16 (12.0) | 1366 (18.7) | 1382 (18.54) | .05 | ||
|
|
Peripheral vascular disease | 1 (0.8) | 59 (0.8) | 60 (0.81) | .94 | ||
|
|
Metabolic complications | 1 (0.8) | 37 (0.5) | 38 (0.51) | .69 | ||
aChi-square test or Z test (for categorical variables); Student t test or Wilcoxon rank-sum test (for continuous variables).
bStatistical comparison was not conducted in total generated data of sugar and diabetes calendar function.
cHbA1c: hemoglobin A1c.
dMCMH: My Chart in My Hand.
eDCSI: diabetes complications severity index.
The DCSI score proportion of continuous and noncontinuous users had no significant difference in the chi-square test. This can be found in Multimedia Appendix 2. Among the 14 DCSI scores, those with zero proportion in both patient groups (scores 10, 12, and 13) were excluded in the analysis using the chi-square test, because calculation with the chi-square test is only possible when each score does not have zero proportion in any group.
Hemoglobin A1c Pattern Analysis According to Continuous Use
Figure 3 shows the trend of the HbA1c pattern for continuous and noncontinuous users. The HbA1c decline of continuous and noncontinuous users was also compared. The HbA1c decline (mean −0.00533, SD 0.0144) in continuous users was significantly steeper than that of noncontinuous users (mean −0.00278, SD 0.0137; P=.02). The SD of continuous users (mean 0.832, SD 0.574) was significantly higher than that of noncontinuous users (mean 0.719, SD 0.541; P=.005). However, the r-squared value had no statistically significant difference between continuous and noncontinuous users (P=.40).
Figure 3.
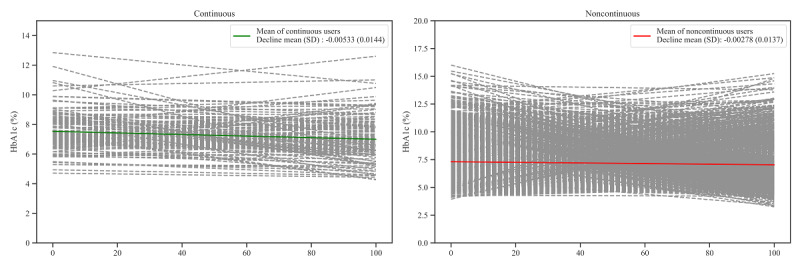
Hemoglobin A1c (HbA1c) patterns (decline, r-squared value, and SD) of continuous and noncontinuous users. The x-axis is the percentage of days past from the first HbA1c measurement compared with the period between the first and last HbA1c measurements. The dashed lines are the HbA1c decline of each patient. The slope and y-axis intercept of the continuous lines indicates the mean of slope and y-axis of patients, respectively.
When adjusting confounders that can contribute to the decline, continuous use had a statistically significant effect (P=.047) on making decline steeper, as seen in Table 2. In addition, age, first HbA1c measurement, DCSI, weeks of sugar function data generation, and HbA1c measurement in weeks before MCMH version 2.0 start showed statistically significant effects (P=.004; P<.001; P=.01; P=.003; P<.001, respectively).
Table 2.
Results of adjusting confounders with the analysis of covariance in decline comparison.
| Variables | F test (df=1) | P value |
| Continuous users | 3.94 | .047 |
| Age (years) | 8.07 | .004 |
| Sex | 0.17 | .68 |
| First HbA1ca measurement | 3054.90 | <.001 |
| DCSIb | 6.45 | .01 |
| Sugar function data generation (weeks) | 8.68 | .003 |
| HbA1c measurement weeks before MCMH version 2.0 start | 154.25 | <.001 |
| Generated sugar function data count | 0.03 | .86 |
aHbA1c: hemoglobin A1c.
bDCSI: diabetes complications severity index.
Comparison of Hemoglobin A1c Regulation With Target Level in Continuous Use
Table 3 lists the proportion with regard to HbA1c patterns. The proportion of users with the first HbA1c measurement higher than 6.5% and the last HbA1c measurement lower than 6.5% had a statistical difference (P=.01). Among users with the first HbA1c measurement lower than 6.5%, the proportion of patients with the last HbA1c measurement lower than 6.5% and the last HbA1c measurement higher than 6.5% had no significant difference (P=.34 and P=.29, respectively). No significant difference was found between proportions of patients with the first HbA1c measurement of 6.5% or higher and the last HbA1c measurement higher than 6.5% (P=.41).
Table 3.
Pre– and post–hemoglobin A1c management comparison by continuous use.
| HbA1ca pattern | Users | P value | |||
|
|
Continuous (n=133) | Noncontinuous (n=7320) |
|
||
| First measurement <6.5% | |||||
|
|
Last measurement | ||||
|
|
|
<6.5%, n (%) | 15 (11.3) | 1040 (14.21) | .34 |
|
|
|
≥6.5%, n (%) | 7 (5.3) | 564 (7.70) | .29 |
| First measurement ≥ 6.5% | |||||
|
|
Last measurement | ||||
|
|
|
<6.5%, n (%) | 38 (28.6) | 564 (7.70) | .01 |
|
|
|
≥6.5%, n (%) | 73 (54.9) | 4278 (58.44) | .41 |
aHbA1c: hemoglobin A1c.
Similar to the decline analysis, the result of confounder adjustment by logistic regression for users with a high first HbA1c measurement is summarized in Table 4. The continuous use of MCMH version 2.0 had a statistically significant effect in helping users move from an HbA1c measurement above 6.5% to an HbA1c measurement below 6.5% (P=.04). In addition, age, first HbA1c measurement, and HbA1c measurement in weeks before MCMH version 2.0 start showed statistically significant effects (all: P<.001).
Table 4.
The result of logistic regression against users with a high first hemoglobin A1c measurement (n=111 continuous and n=5716 noncontinuous users).
| Variables | Coefficient | P value |
| Constant | 1.640 | <.001 |
| Continuous | 0.618 | .04 |
| Age (years) | −0.010 | <.001 |
| Sex | −0.085 | .20 |
| First HbA1ca measurement | −0.171 | <.001 |
| DCSIb | −0.041 | .05 |
| Sugar function data generation (weeks) | −0.004 | .23 |
| HbA1c measurement in weeks before MCMHc version 2.0 use start | −0.008 | <.001 |
| Generated sugar function data count | −0.001 | .52 |
aHbA1c: hemoglobin A1c.
bDCSI: diabetes complications severity index.
cMCMH: My Chart in My Hand.
Discussion
Principal Findings
For the following reasons, this study supports the use of mPHRs as an effective platform for diabetes management by integrating patient-generated health and clinical data from PHRs and EMRs, respectively. First, analyzing the characteristics of continuous users of MCMH version 2.0, male patients with a high HbA1c level seemed to use MCMH version 2.0 more continuously. Second, the continuous use of PHRs resulted in a higher decrease of HbA1c levels and enhanced the regulation of high HbA1c levels of patients to the target range. Therefore, male users with high HbA1c levels had a higher decrease in HbA1c levels and improved HbA1c regulation to the target level. By analyzing the characteristics of continuous users and their HbA1c patterns, we also suggest the use of mPHR as a diabetes care support tool enabling personalized management.
This study is unique when compared with previous studies on the basis of the following characteristics. First, we suggested the health improvement effect of mPHRs on the basis of the integration of PHRs and EMRs. In this study, we expected two benefits of integrating PHRs and EMRs. One is suggesting a different methodology for real-world data analysis and presenting additional real-world evidence, which supports previous studies. Another is ensuring a high-quality data analysis is conducted. There are many previous studies implying the advantages of PHRs and PGHD with positive conclusions of the use of mPHRs [14-17]. The results of these studies were collected on the basis of clinical trials such as nonblinded, open-label randomized controlled trials (RCTs) and cluster-randomized trial designs. As a real-world data analysis covers bias limitations in RCTs and can handle unknown factors of PHRs, the results of a real-world data analysis provide strong and necessary support to previous RCTs [25]. Moreover, the integration of EMRs gave high-quality HbA1c data and diagnosis data, which made the analysis more precise.
Second, previous studies mainly discussed about the decrease in HbA1c levels as an advantage of using PHRs. However, as the main goal of glycemic control is regulating a patient’s HbA1c level to the recommended range, we compared both HbA1c decrease and proportions of patients who initially had a high HbA1c level but their HbA1c level decreased to a low value. According to the 2015 and 2019 diabetes management guidelines from the KDA, the recommended target HbA1c level is 6.5% in patients with type 2 diabetes, and this differs from the guideline by the ADA [4,26,27]. As this study was conducted in AMC, South Korea, we used the guidelines from KDA and defined the cutoff value of the HbA1c level as 6.5%. Recent studies recommend that patients with severe diabetes mellitus should be controlled to lower than 7%, depending on the severity and complications of diabetes [28-30]. Moreover, a stable decrease in blood glucose levels is also an important task in glycemic control. We also focused on the r-squared value of the trend line and SD as an indicator of stabilized HbA1c decrease, but we could not achieve any outstanding results.
Overall User Characteristics
Analyzing users who had access to MCMH version 1.0 indicated that these users visited hospitals more with chronic diseases [21]. Continuous users were younger than noncontinuous users (P<.001), and there was a significant difference in sex proportion; the continuous user group had a higher male ratio (P<.001). In previous research, groups that used a PHR system had young users and a high proportion of males or generated more PGHD, especially those related to diabetes [21,22]. This is because male users aged between 51 and 70 years tend to adopt the PHR system [31]. In addition, in this study, the HbA1c level in continuous users was measured for a shorter period (P=.04) and more frequently (P=.007) than noncontinuous users. However, the number of HbA1c measurements had no significant difference between continuous and noncontinuous user groups. In South Korea, the social health insurance program was introduced with the 1977 National Health Insurance Act. This program was thereafter progressively rolled out to the general public, and it finally achieved universal coverage in 1989. According to the National Health Insurance Act, the criteria for the method, procedure, scope, and upper limit of health care shall be prescribed by the Ministry of Health and Welfare [17].
National insurance only supports up to 6 HbA1c tests per year, in accordance with the National Health Insurance Act. First, we considered the number of HbA1c measurements as another indicator of diabetes severity. This is because well-controlled patients typically undergo HbA1c tests twice a year, whereas poorly controlled individuals undergo testing 4 times a year [32]. However, the number of measurements seems to be similar because of the policy in South Korea. Although continuous users had shorter periods (approximately 80 days) between the first and last measurements, this group took HbA1c tests more frequently. This may be because of the increase in hospital visits, along with more satisfaction and loyalty to the hospital [33]. To compare diabetes severity, the proportion of patients with an HbA1c level of 6.5% or above, a first HbA1c level measurement, and a DCSI score distribution were compared between continuous and noncontinuous groups. The two groups had no significant difference in the proportion of high HbA1c levels and DCSI distribution; however, continuous users had a higher HbA1c level (P=.01). Retinopathy patients tended to use MCMH version 2.0 more continuously, but the complication proportion also had an insignificant difference between the two groups. Except for the first HbA1c level measurement, most diabetic-related baseline characteristics appeared to have no significant difference, and the first HbA1c measurement can be adjusted as confounders in an additional analysis. By using PHR and EMR integration, the general characteristics and severity of diabetes were compared.
As the period of HbA1c measurement before MCMH version 2.0 use was shorter in the continuous group (P<.001), continuous users seemed to have an earlier MCMH version 2.0 start compared with noncontinuous users. In addition, continuous users tended to use the sugar and diabetes calendar functions more and generate more data. This was because continuous users tended to use MCMH version 2.0 functions with fewer burdens.
Verifying the Effect of Personal Health Record Use in Hemoglobin A1c Control
The main advantage of PHRs and PGHD is health improvement, especially in diabetes. Among the types of diabetes management, determining the change in HbA1c levels was the most effective method to verify the effectiveness of PHRs in the real world. The results of this study indicate that continuous users had a larger decline; a greater increase in HbA1c levels was observed in users who continuously used the diabetes management–related sugar function in MCMH version 2.0. As decline is the result of the trend line slope normalized to 100 days, the value itself also refers to the change in the HbA1c level. For example, HbA1c was 6.9% on January 1, 2014, and HbA1c was 6.4% on October 19, 2018, in one particular continuous user; therefore, the decline value was −0.0044, which means that this patient’s change in HbA1c level was approximately −0.44% (100 times the value of decline). Thus, the decrease in HbA1c levels in continuous users was approximately 1.9 times that in noncontinuous users. The result of ANCOVA shows that along with continuous use, other factors were also important: age, first HbA1c measurement, DCSI, duration of using the sugar function, and HbA1c measurement period before using MCMH version 2.0. Glycemic control is important for reducing both microvascular risk and emergent risk for myocardial infarction and death [34]. This indicates that the group that continuously used PHRs had health improvement with a decreasing trend of HbA1c levels.
In glycemic control, it is important to reduce not only blood glucose levels but also hypoglycemic events [35]. Traditional diabetes care includes insulin delivery using syringes, pens, or pumps [3]. Although hypoglycemic side effects can occur with multiple daily injections and continuous subcutaneous insulin injection, the invasive characteristic of such forms of care is an inevitable disadvantage [36-39]. In this study, we tried to minimize the risk of hypoglycemic events in PHR-implemented diabetes management by using stability indicators, r-squared value and SD. However, stability was not ensured. In fact, a previous study showed increased glucose stability with the use of an internet-based glucose monitoring system [40]. This indicates that patients can improve hyperglycemia and hypoglycemia management by using PHRs with a blood glucose meter through continuous glucose monitoring diabetic care.
The goal of decreasing the HbA1c level is to prevent the occurrence and aggravation of diabetic complications. Although the criterion for HbA1c in a diagnostic test for diabetes has been recommended by the American Association of Clinical Endocrinologists and ADA, it is an “acceptable complementary diagnostic test for diabetes in Korean patients” [28,41]. Among the many glycemic controls, the tight regulation of HbA1c levels is essential for health improvement and for lowering complication risks such as diabetic retinopathy [42]. In addition, the tight glycemic control of HbA1c levels to 7.0% induces a lower risk of fracture in elderly patients with diabetes [43]. When comparing the ratio of patients with HbA1c levels above and below 6.5% before and after the use of MCMH version 2.0, the group that continuously used MCMH version 2.0 had a higher proportion of regulated patients; initially, the first HbA1c level measurement was over 6.5%, and then it reduced to lower than 6.5%. In addition, among users with the first HbA1c level measurement over 6.5%, the logistic regression results showed that regulation was associated not only with continuous use but also with age, first HbA1c level measurement, and how fast MCMH version 2.0 was adapted. The data generation amount was thought to be important too, but it was statistically insignificant. Therefore, we can claim that the improvement of HbA1c levels by PHR use can eventually affect diabetes management by controlling HbA1c levels to 6.5% in practice.
Limitations of This Research
The main limitation of this study is the concern of general biases in real-world studies: selection bias, information bias, recall bias, and detection bias [44]. As this study mainly focused on analyzing real-world data, strict criteria and inevitable exclusion are necessary, leading to concerns in selection bias and detection bias. However, the criteria for the comparison group were the same, and despite including and excluding many patient criteria and comparing with the MCMH 1.0 user analysis, the study scale is almost similar [22]. The size of the continuous user groups is sometimes larger than that used in other RCT studies and had little baseline differences in diabetic severity [17]. As MCMH version 2.0 data are PGHD, continuous use can only be analyzed by its log data, which does not represent adherence to the app and can lead to information bias. On the contrary, we note that information bias that can occur in HbA1c level scaling can be controlled with the integration of EMRs. This integration helped in reducing recall bias in diabetes and complication diagnosis.
Time scale is also another limitation. In RCTs, the HbA1c measurement point, the app account creation point, and app use frequency can be controlled and optimized for convenient data analysis. However, in real-world data, patients have diverse points of HbA1c measurement and MCMH version 2.0 starting points. Even though there were limitations with regard to missing data, inappropriate data, and ambiguous time scale standards, we used patient selection criteria to choose patients who can be analyzed and used the decline factor to monitor the HbA1c level for minimizing the effect of irregular time points. The decline factor is a variable that has been coined for the purpose of this study and has an uncertain clinical rationale. However, as the decline variable also implies a decrease in HbA1c levels, and the decreasing trend is being maintained, the quantitative comparison of decline between groups is meaningful. In diabetes care, lowering HbA1c levels to the target level and maintaining the decreased HbA1c level is the primary goal. Thus, the decline is a reasonable variable for analysis in studies with data having unspecific HbA1c measurement points.
An additional limitation is that AMC is a territorial hospital, and almost all the study patients are residing in South Korea. The small size of the study population and short duration are other limitations. The low frequency of PHR data generation and short-term MCMH version 2.0 operation is not an ideal database for analyzing chronic diseases such as diabetes. A larger study size and longer study duration will provide stronger real-world evidence of the clinical meaning of PHRs.
On the basis of the proportion of continuous and noncontinuous users, further research for encouraging patients to use PHRs more continuously is essential. In this study, continuous users had better diabetes management outcomes than noncontinuous users. However, continuous users were only 1.78% (133/7453) of the study population and were only 0.20% (133/64,932) of users who started using MCMH version 2.0. Thus, studies for maintaining active PGHD-generating users and turning noncontinuous users into continuous users are necessary. Finding out whether giving health-related advice on the basis of MCMH version 2.0 encourages patients to use a PHR app for changing app use patterns needs to be studied to prevent usability issues [45]. Furthermore, for personalized PHR advice, if larger and better quality of data is provided, the glycemic control outcome analysis by treatment is important. Further studies in diverse territories and a deeper analysis of MCMH version 2.0 should be performed to prove the effectiveness of PHRs as a diabetes management tool in decreasing HbA1c levels.
Conclusions
By integrating and analyzing patient- and clinically generated data, the continuous use of PHRs improves diabetes management outcomes. A greater decrease in HbA1c levels was observed in continuous users, and HbA1c levels were regulated to the target level in continuous users compared with noncontinuous users. Previous clinical trials and the results of this study proved that PHRs are effective in managing diabetes. However, further evaluation of the effectiveness of PHRs in various diseases and studies for adherence to PHRs are needed. A larger study population and longer duration will be necessary for the accurate analysis of the clinical rationale of PHRs on chronic diseases.
Acknowledgments
The authors would like to thank the Medical Information Office of AMC for providing log data of the mobile EMR and supporting data analysis and interpretation. This study was supported by a grant of the Research and Development Project, Ministry of Trade, Industry and Energy, Republic of Korea (no. 20004503) and a grant of the National Research Foundation of Korea funded by the Korean government (Ministry of Science and ICT; no NRF-2019M3E5D4064682).
Abbreviations
- ADA
American Diabetes Association
- AMC
Asan Medical Center
- ANCOVA
analysis of covariance
- DCSI
diabetes complications severity index
- EMR
electronic medical record
- HbA1c
hemoglobin A1c
- ICD-10
International Classification of Diseases 10th Revision
- IRB
institutional review board
- KDA
Korean Diabetes Association
- MCMH
My Chart in My Hand
- mHealth
mobile health
- mPHR
mobile personal health record
- PGHD
patient-generated health data
- PHR
personal health record
- RCT
randomized controlled trial
Appendix
Formula of decline.
Diabetes complications severity index score proportion comparison of continuous and noncontinuous users.
Footnotes
Authors' Contributions: DS, YP, and JL conceived and designed the study; DS, YL, and JK reviewed records and collected the data; DS analyzed the data; DS and YP wrote the manuscript; and YP, JP, and JL reviewed the manuscript.
Conflicts of Interest: None declared.
References
- 1.Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010 Jan;87(1):4–14. doi: 10.1016/j.diabres.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 2.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004 May;27(5):1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 3.American Diabetes Association 7. Diabetes Technology: Standards of Medical Care in Diabetes-2019. Diabetes Care. 2019 Jan;42(Suppl 1):S71–80. doi: 10.2337/dc19-S007. [DOI] [PubMed] [Google Scholar]
- 4.Kim MK, Ko S, Kim B, Kang ES, Noh J, Kim S, Park S, Hur KY, Chon S, Moon MK, Kim N, Kim SY, Rhee SY, Lee K, Kim JH, Rhee E, Chun S, Yu SH, Kim DJ, Kwon H, Park KS, Committee of Clinical Practice Guidelines‚ Korean Diabetes Association 2019 clinical practice guidelines for type 2 diabetes mellitus in Korea. Diabetes Metab J. 2019 Aug;43(4):398–406. doi: 10.4093/dmj.2019.0137. https://e-dmj.org/DOIx.php?id=10.4093/dmj.2019.0137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Riddle MC, Herman WH. The cost of diabetes care-an elephant in the room. Diabetes Care. 2018 May;41(5):929–32. doi: 10.2337/dci18-0012. [DOI] [PubMed] [Google Scholar]
- 6.American Diabetes Association Economic costs of diabetes in the US in 2017. Diabetes Care. 2018 May;41(5):917–28. doi: 10.2337/dci18-0007. http://europepmc.org/abstract/MED/29567642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rodríguez AQ, Wägner AM. Mobile phone applications for diabetes management: A systematic review. Endocrinol Diabetes Nutr. 2019 May;66(5):330–7. doi: 10.1016/j.endinu.2018.11.005. [DOI] [PubMed] [Google Scholar]
- 8.Grady M, Katz LB, Cameron H, Levy BL. Diabetes app-related text messages from health care professionals in conjunction with a new wireless glucose meter with a color range indicator improves glycemic control in patients with type 1 and type 2 diabetes: randomized controlled trial. JMIR Diabetes. 2017 Aug 7;2(2):e19. doi: 10.2196/diabetes.7454. https://diabetes.jmir.org/2017/2/e19/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Derdzinski M, Welsh J, Puhr S, Walker TC, Parker A, Jimenez A. 391-P: Hypoglycemia Reductions with the Dexcom G6 CGM System’s Predictive Alert. Diabetes. 2019 Jun;68(Supplement 1):391-P. doi: 10.2337/db19-391-p. [DOI] [Google Scholar]
- 10.Adolfsson P, Hartvig NV, Kaas A, NygÅRd NK, MÅRdby AC, Hellman J. 1076-P: Increased Time-in-Range (TIR) Observed after Introduction of a Connected Insulin Pen. Diabetes. 2019;68(Supplement 1):1076-P. doi: 10.2337/db19-1076-p. [DOI] [Google Scholar]
- 11.Adolfsson P, Hartvig NV, Kaas A, Knudsen NN, MÅRdby A, MøLler JB, Hellman J. 126-LB: Improved Insulin Adherence after Introduction of a Smart Connected Insulin Pen. Diabetes. 2019 Jun;68(Supplement 1):126-LB. doi: 10.2337/db19-126-lb. [DOI] [Google Scholar]
- 12.Han M, Lee E. Effectiveness of mobile health application use to improve health behavior changes: a systematic review of randomized controlled trials. Healthc Inform Res. 2018 Jul;24(3):207–26. doi: 10.4258/hir.2018.24.3.207. https://www.e-hir.org/DOIx.php?id=10.4258/hir.2018.24.3.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yi JY, Kim Y, Cho Y, Kim H. Self-management of chronic conditions using mHealth interventions in Korea: a systematic review. Healthc Inform Res. 2018 Jul;24(3):187–97. doi: 10.4258/hir.2018.24.3.187. https://www.e-hir.org/DOIx.php?id=10.4258/hir.2018.24.3.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Quinn CC, Clough SS, Minor JM, Lender D, Okafor MC, Gruber-Baldini A. WellDoc mobile diabetes management randomized controlled trial: change in clinical and behavioral outcomes and patient and physician satisfaction. Diabetes Technol Ther. 2008 Jun;10(3):160–8. doi: 10.1089/dia.2008.0283. [DOI] [PubMed] [Google Scholar]
- 15.Quinn CC, Shardell MD, Terrin ML, Barr EA, Ballew SH, Gruber-Baldini AL. Cluster-randomized trial of a mobile phone personalized behavioral intervention for blood glucose control. Diabetes Care. 2011 Sep;34(9):1934–42. doi: 10.2337/dc11-0366. http://europepmc.org/abstract/MED/21788632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yu Y, Yan Q, Li H, Li H, Wang L, Wang H, Zhang Y, Xu L, Tang Z, Yan X, Chen Y, He H, Chen J, Feng B. Effects of mobile phone application combined with or without self-monitoring of blood glucose on glycemic control in patients with diabetes: A randomized controlled trial. J Diabetes Investig. 2019 Sep;10(5):1365–71. doi: 10.1111/jdi.13031. doi: 10.1111/jdi.13031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee DY, Park J, Choi D, Ahn H, Park S, Park C. The effectiveness, reproducibility, and durability of tailored mobile coaching on diabetes management in policyholders: A randomized, controlled, open-label study. Sci Rep. 2018 Feb 26;8(1):3642. doi: 10.1038/s41598-018-22034-0. doi: 10.1038/s41598-018-22034-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lester M, Boateng S, Studeny J, Coustasse A. Personal health records: beneficial or burdensome for patients and healthcare providers? Perspect Health Inf Manag. 2016;13:1h. http://europepmc.org/abstract/MED/27134613. [PMC free article] [PubMed] [Google Scholar]
- 19.Showell C. Barriers to the use of personal health records by patients: a structured review. PeerJ. 2017;5:e3268. doi: 10.7717/peerj.3268. doi: 10.7717/peerj.3268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tenforde M, Nowacki A, Jain A, Hickner J. The association between personal health record use and diabetes quality measures. J Gen Intern Med. 2012 Apr;27(4):420–4. doi: 10.1007/s11606-011-1889-0. http://europepmc.org/abstract/MED/22005937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee G, Park JY, Shin S, Hwang JS, Ryu HJ, Lee JH, Bates DW. Which users should be the focus of mobile personal health records? Analysis of user characteristics influencing usage of a tethered mobile personal health record. Telemed J E Health. 2016 May;22(5):419–28. doi: 10.1089/tmj.2015.0137. http://europepmc.org/abstract/MED/26447775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Park YR, Lee Y, Kim JY, Kim J, Kim HR, Kim Y, Kim WS, Lee J. Managing patient-generated health data through mobile personal health records: analysis of usage data. JMIR Mhealth Uhealth. 2018 Apr 9;6(4):e89. doi: 10.2196/mhealth.9620. https://mhealth.jmir.org/2018/4/e89/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Glasheen WP, Renda A, Dong Y. Diabetes Complications Severity Index (DCSI)-Update and ICD-10 translation. J Diabetes Complications. 2017 Jun;31(6):1007–13. doi: 10.1016/j.jdiacomp.2017.02.018. https://linkinghub.elsevier.com/retrieve/pii/S1056-8727(16)31042-X. [DOI] [PubMed] [Google Scholar]
- 24.World Health Organization. Geneva: World Health Organization; 2011. [2020-03-12]. Use of Glycated Haemoglobin (HbA1c) in the Diagnosis of Diabetes Mellitus: Abbreviated Report of a WHO Consultation https://www.who.int/diabetes/publications/report-hba1c_2011.pdf. [Google Scholar]
- 25.Jadad AR, Enkin MW. Bias in randomized controlled trials. In: Jadad AR, Enkin MW, editors. Randomized Controlled Trials: Questions, Answers and Musings. Paris: BMJ Books; 2007. pp. 29–47. [Google Scholar]
- 26.Ha KH, Kim DJ. Current status of managing diabetes mellitus in Korea. Korean J Intern Med. 2016 Sep;31(5):845–50. doi: 10.3904/kjim.2016.253. doi: 10.3904/kjim.2016.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fruh SM. Obesity: Risk factors, complications, and strategies for sustainable long-term weight management. J Am Assoc Nurse Pract. 2017 Oct;29(S1):S3–14. doi: 10.1002/2327-6924.12510. http://europepmc.org/abstract/MED/29024553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Handelsman Y, Bloomgarden ZT, Grunberger G, Umpierrez G, Zimmerman RS, Bailey TS, Blonde L, Bray GA, Cohen AJ, Dagogo-Jack S, Davidson JA, Einhorn D, Ganda OP, Garber AJ, Garvey WT, Henry RR, Hirsch IB, Horton ES, Hurley DL, Jellinger PS, Jovanovič L, Lebovitz HE, LeRoith D, Levy P, McGill JB, Mechanick JI, Mestman JH, Moghissi ES, Orzeck EA, Pessah-Pollack R, Rosenblit PD, Vinik AI, Wyne K, Zangeneh F. American association of clinical endocrinologists and american college of endocrinology - clinical practice guidelines for developing a diabetes mellitus comprehensive care plan - 2015. Endocr Pract. 2015 Apr;21(Suppl 1):1–87. doi: 10.4158/EP15672.GL. http://europepmc.org/abstract/MED/25869408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.American Diabetes Association 6. Glycemic Targets. Diabetes Care. 2017;40(Supplement 1):S48–56. doi: 10.2337/dc17-s009. [DOI] [PubMed] [Google Scholar]
- 30.Qaseem A, Wilt TJ, Kansagara D, Horwitch C, Barry MJ, Forciea MA, Clinical Guidelines Committee of the American College of Physicians Hemoglobin A1c targets for glycemic control with pharmacologic therapy for nonpregnant adults with type 2 diabetes mellitus: a guidance statement update from The American College of Physicians. Ann Intern Med. 2018 Apr 17;168(8):569–76. doi: 10.7326/M17-0939. [DOI] [PubMed] [Google Scholar]
- 31.Nazi KM. Veterans' voices: use of the American Customer Satisfaction Index (ACSI) Survey to identify My HealtheVet personal health record users' characteristics, needs, and preferences. J Am Med Inform Assoc. 2010;17(2):203–11. doi: 10.1136/jamia.2009.000240. http://europepmc.org/abstract/MED/20190065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Canadian Agency for Drugs and Technologies in Health. 2014. [2020-03-12]. HbA1c Testing Frequency: A Review of the Clinical Evidence and Guidelines https://www.cadth.ca/hba1c-testing-frequency-review-clinical-evidence-and-guidelines.
- 33.Cho WH, Lee H, Kim C, Lee S, Choi K. The impact of visit frequency on the relationship between service quality and outpatient satisfaction: a South Korean study. Health Serv Res. 2004 Feb;39(1):13–33. doi: 10.1111/j.1475-6773.2004.00213.x. http://europepmc.org/abstract/MED/14965075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008 Oct 9;359(15):1577–89. doi: 10.1056/NEJMoa0806470. [DOI] [PubMed] [Google Scholar]
- 35.Amiel SA, Sherwin RS, Simonson DC, Tamborlane WV. Effect of intensive insulin therapy on glycemic thresholds for counterregulatory hormone release. Diabetes. 1988 Jul;37(7):901–7. doi: 10.2337/diab.37.7.901. [DOI] [PubMed] [Google Scholar]
- 36.Wong JC, Dolan LM, Yang TT, Hood KK. Insulin pump use and glycemic control in adolescents with type 1 diabetes: Predictors of change in method of insulin delivery across two years. Pediatr Diabetes. 2015 Dec;16(8):592–9. doi: 10.1111/pedi.12221. http://europepmc.org/abstract/MED/25387433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wheeler BJ, Heels K, Donaghue KC, Reith DM, Ambler GR. Insulin pump-associated adverse events in children and adolescents--a prospective study. Diabetes Technol Ther. 2014 Sep;16(9):558–62. doi: 10.1089/dia.2013.0388. [DOI] [PubMed] [Google Scholar]
- 38.Kordonouri O, Biester T, Schnell K, Hartmann R, Tsioli C, Fath M, Datz N, Danne T. Lipoatrophy in children with type 1 diabetes: an increasing incidence? J Diabetes Sci Technol. 2015 Mar;9(2):206–8. doi: 10.1177/1932296814558348. http://europepmc.org/abstract/MED/25411060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yeh H, Brown TT, Maruthur N, Ranasinghe P, Berger Z, Suh YD, Wilson LM, Haberl EB, Brick J, Bass EB, Golden SH. Comparative effectiveness and safety of methods of insulin delivery and glucose monitoring for diabetes mellitus: a systematic review and meta-analysis. Ann Intern Med. 2012 Sep 4;157(5):336–47. doi: 10.7326/0003-4819-157-5-201209040-00508. [DOI] [PubMed] [Google Scholar]
- 40.Cho J, Chang S, Kwon H, Choi Y, Ko S, Moon S, Yoo S, Song K, Son H, Kim H, Lee W, Cha B, Son H, Yoon K. Long-term effect of the internet-based glucose monitoring system on HbA1c reduction and glucose stability: a 30-month follow-up study for diabetes management with a ubiquitous medical care system. Diabetes Care. 2006 Dec;29(12):2625–31. doi: 10.2337/dc05-2371. [DOI] [PubMed] [Google Scholar]
- 41.Jeon JY, Ko S, Kwon H, Kim NH, Kim JH, Kim CS, Song K, Won JC, Lim S, Choi SH, Jang M, Kim Y, Oh K, Kim DJ, Cha B, Taskforce Team of Diabetes Fact Sheet of the Korean Diabetes Association Prevalence of Diabetes and Prediabetes according to Fasting Plasma Glucose and HbA1c. Diabetes Metab J. 2013 Oct;37(5):349–57. doi: 10.4093/dmj.2013.37.5.349. https://e-dmj.org/DOIx.php?id=10.4093/dmj.2013.37.5.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rajalakshmi R, Prathiba V, Mohan V. Does tight control of systemic factors help in the management of diabetic retinopathy? Indian J Ophthalmol. 2016 Jan;64(1):62–8. doi: 10.4103/0301-4738.178146. http://www.ijo.in/article.asp?issn=0301-4738;year=2016;volume=64;issue=1;spage=62;epage=68;aulast=Rajalakshmi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Conway BN, Long DM, Figaro MK, May ME. Glycemic control and fracture risk in elderly patients with diabetes. Diabetes Res Clin Pract. 2016 May;115:47–53. doi: 10.1016/j.diabres.2016.03.009. http://europepmc.org/abstract/MED/27242122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Blonde L, Khunti K, Harris SB, Meizinger C, Skolnik NS. Interpretation and impact of real-world clinical data for the practicing clinician. Adv Ther. 2018 Nov;35(11):1763–74. doi: 10.1007/s12325-018-0805-y. http://europepmc.org/abstract/MED/30357570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jeon E, Park H. Development of the IMB model and an evidence-based diabetes self-management mobile application. Healthc Inform Res. 2018 Apr;24(2):125–38. doi: 10.4258/hir.2018.24.2.125. https://www.e-hir.org/DOIx.php?id=10.4258/hir.2018.24.2.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Formula of decline.
Diabetes complications severity index score proportion comparison of continuous and noncontinuous users.


