Functional restoration of the TP53 tumor suppressor holds great promise for anticancer therapy. Current strategies are focused on modulating TP53 regulatory proteins. Long noncoding RNAs (lncRNAs) have emerged as important regulators of TP53 as well as modulators of downstream tumor-suppressive transcriptional responses. Unlike many other cancer types, human papillomavirus (HPV)-positive cancer cells retain wild-type TP53 that is rendered dysfunctional by the viral E6 protein. We show that acute expression of the damage-induced long noncoding RNA, DINO, a known TP53 transcriptional target and functional modulator, causes TP53 reactivation in HPV-positive cervical cancer cells. This causes increased vulnerability to standard chemotherapeutics as well as biguanide compounds that cause metabolic stress. Hence, strategies that target DINO may be useful for restoring TP53 tumor suppressor activity in HPV-positive cancers and other tumor types that retain wild-type TP53.
KEYWORDS: human papillomaviruses, cervical cancer, lncRNA, DINO, DINOL, TP53, UBE3A, E6-AP, DNA damage, cellular transformation, chemoresistance, metabolism
ABSTRACT
Tumor cells overcome the cytostatic and cytotoxic restraints of TP53 tumor suppressor signaling through a variety of mechanisms. High-risk human papillomavirus (HPV)-positive tumor cells retain wild-type TP53 because the HPV E6/UBE3A ubiquitin ligase complex targets TP53 for proteasomal degradation. While restoration of TP53 in tumor cells holds great promise for cancer therapy, attempts to functionally restore the dormant TP53 tumor suppressor in HPV-positive cancer cells by inhibiting the HPV E6/UBE3A ubiquitin ligase complex have not yet been successful. The damage-induced long noncoding RNA, DINO (DINOL), is a TP53 transcriptional target that has been reported to bind to and stabilize TP53, thereby amplifying TP53 signaling. We show that HPV-positive cervical carcinoma cells contain low levels of DINO because of HPV E6/UBE3A-mediated TP53 degradation. Acute DINO expression overrides HPV16 E6/UBE3A-mediated TP53 degradation, causing TP53 stabilization and increased expression of TP53 transcriptional target genes. This causes a marked sensitization to chemotherapy agents and renders cells vulnerable to metabolic stress. Acute DINO expression in HPV-positive cervical cancer cells induces hallmarks of DNA damage response signaling, and TP53 activation involves ATM/CHK2 signaling. DINO upregulation in response to DNA damage is independent of ATM/CHK2 and can occur in cancer cells that express mutant TP53.
INTRODUCTION
The productive viral life cycle of human papillomaviruses (HPVs) is confined to postmitotic, terminally differentiated squamous epithelial cells. Synthesis of viral progeny is critically dependent on cellular replication proteins. Hence, HPVs need to enforce continued expression of cellular proteins that are necessary for synthesis of viral genomes in terminally differentiated epithelial cells. High-risk HPV E7 proteins target the retinoblastoma tumor suppressor protein (RB1) for degradation (1, 2). This causes aberrant S-phase entry, which is sensed and leads to activation of the TP53 tumor suppressor protein. TP53 is a DNA binding transcription factor that is present at low levels in normal cells due to rapid proteasome-mediated turnover by the MDM2 ubiquitin ligase (3–5). When activated, TP53 is stabilized, accumulates to high levels, and engages cytostatic and cytotoxic transcriptional programs (6, 7). To blunt cell-abortive signals caused by HPV E7 expression, the high-risk HPV E6 proteins inactivate TP53 by forming a complex with the cellular ubiquitin ligase, UBE3A (E6-AP), thereby targeting TP53 for ubiquitination and proteasomal degradation (8–10). As a consequence of HPV E6/UBE3A-mediated inactivation, most high-risk HPV-associated tumors retain wild-type TP53 (11, 12).
The TP53 tumor suppressor is mutated and rendered dysfunctional in most human cancers by mutation or by dysregulated expression of TP53 tumor suppressor pathway components (7). Restoration of TP53 signaling caused tumor regression in a variety of preclinical mouse models of human cancers, albeit through different mechanisms (13–18). This has prompted a keen interest in developing therapies aimed at restoring TP53 activity in cancers. Most of the pharmacological strategies that are currently tested in preclinical models or are in clinical trials target the MDM2-mediated TP53 degradation pathway (19–21). In HPV oncogene-expressing cells, there is a switch from MDM2- to HPV E6/UBE3A-mediated TP53 degradation (22). Reactivation of the dormant TP53 tumor suppressor in the HPV18-positive HeLa cervical cancer line by selectively repressing endogenous HPV18 E6 expression was shown to cause senescence and apoptosis (23). Hence, reactivation of TP53 tumor suppressor signaling may also have therapeutic benefits in HPV-positive human tumors. Multiple strategies to hinder E6/UBE3A-mediated TP53 inactivation have been explored, including inhibition of E6 or UBE3A expression (24, 25), and disruption of the TP53/E6/UBE3A complex with cellular proteins (26, 27), artificial E6 targeting microRNAs (28), RNA aptamers (29), and synthetic peptides (30–32) as well as small molecules (33–35). However, none of these strategies has been translated to the clinic. Therefore, alternative approaches to reactivate the TP53 tumor suppressor pathway in HPV-associated cancers need to be explored.
The vast majority of the human transcriptome consists of noncoding RNAs. Several classes of noncoding RNAs, including microRNAs, circular RNAs, and long noncoding RNAs (lncRNAs), regulate cellular processes that are dysregulated during carcinogenesis (36). Long noncoding RNAs (lncRNAs) are a large family of RNAs of >200 nucleotides and with no or limited coding capacity of <100 amino acids. lncRNAs can form complexes with RNAs, DNAs, and proteins and modulate cellular processes that have been referred to as hallmarks of human cancer (37, 38). Similarly, expression of the HPV E6 and E7 genes has been shown to remodel the cellular lncRNA transcriptome (39). Many lncRNAs have been identified as upstream and/or downstream components of the TP53 tumor suppressor pathway (40–42). The damage-induced noncoding (DINO) lncRNA is induced by TP53 in response to DNA damage. In addition, DINO has been reported to amplify the TP53 transcriptional response by binding and stabilizing TP53, and TP53/DINO complexes were detected bound to TP53 transcriptional response elements (43). Here, we report that acute DINO expression at levels similar to those observed in response to DNA damage stabilizes TP53 and restores TP53 tumor suppressor activity in HPV-positive cervical cancer cell lines. This causes increased sensitivity to standard-of-care chemotherapy agents and vulnerability to metabolic stress. Surprisingly, we found that, unlike the canonical TP53 target CDKN1A, DINO upregulation in response to DNA damage is through a pathway that is independent of ATM/CHK2 and was also observed in the HPV-negative C33A cervical cancer cell line that expresses a DNA binding-defective TP53 mutant. Moreover, acute DINO expression in HPV-positive cervical cancer cells induces hallmarks of DNA damage signaling and activates TP53 through ATM/CHK2 signaling.
RESULTS
Low DINO levels in HPV-positive cervical cancer cells are a result of HPV E6-mediated TP53 degradation.
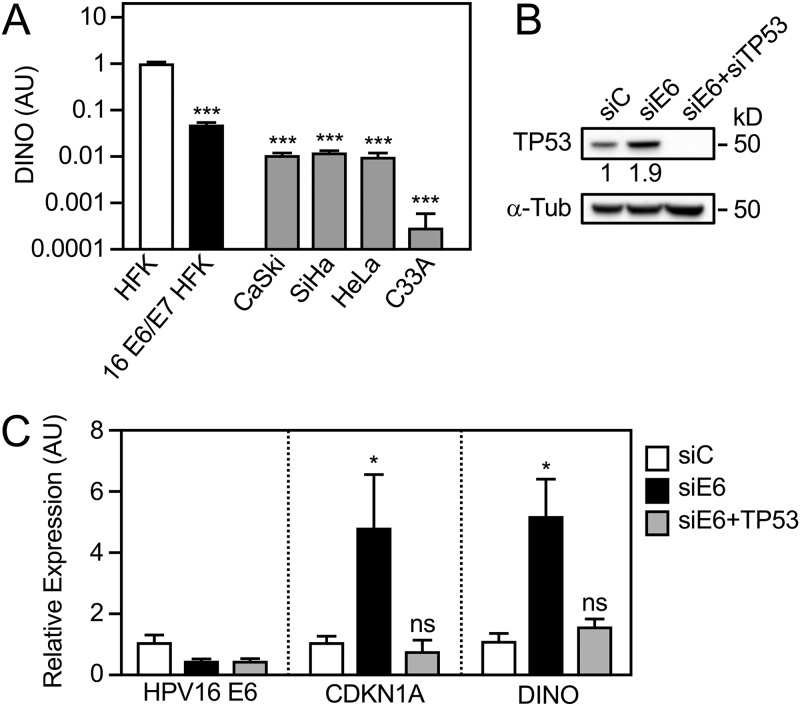
We previously reported that DINO expression correlated with TP53 levels in HPV E6 and/or E7 expressing human foreskin keratinocytes (HFKs) (44). Given that HPV-positive cervical cancer lines express E6 and E7 and retain wild-type TP53, we hypothesized that they may express DINO at similarly low levels as HPV16 E6/E7-expressing HFKs. To test this, we assessed DINO expression in HPV16-positive CaSki, HPV16-positive SiHa, and HPV18-positive HeLa cervical carcinoma lines by quantitative reverse transcription-PCR (qRT-PCR) assays. As a control, we analyzed DINO expression in the HPV-negative C33A cervical carcinoma line that expresses a DNA binding-defective TP53 cancer hot spot mutant where the arginine residue at position 273 is changed to a histidine (R273H) (45–47). These experiments showed that HPV-positive cervical carcinoma lines expressed DINO at levels that were lower than HPV16 E6/E7-expressing HFKs. The mutant TP53-expressing, HPV-negative C33A cervical cancer cells contained even lower DINO levels (Fig. 1A).
FIG 1.
Low DINO levels in HPV-positive cervical cancer cells are a result of E6-mediated TP53 inactivation. DINO levels in HPV-positive CaSki (HPV16), SiHa (HPV16), and HeLa (HPV18) and HPV-negative C33A cervical carcinoma cell lines were determined by quantitative reverse transcription-PCR (qRT-PCR) assays. DINO levels in control vector-transduced primary human foreskin keratinocytes (HFKs) and HPV16 E6/E7-expressing HFKs (16 E6/E7 HFKs) are shown for comparison (A). SiHa cells were transfected with an siRNA targeting HPV16 E6 alone or in combination with TP53 targeting siRNAs. HPV16 E6 and TP53 depletion was validated by measuring TP53 protein levels by immunoblotting (B) and by quantifying E6 mRNA levels by qRT-PCR (C). The TP53-dependent effects of HPV16 E6 depletion on DINO and the canonical TP53 transcriptional target CDKN1A were also assessed by qRT-PCR (C). Expression data are presented in arbitrary units (AU) and normalized to expression of the RPLP0 housekeeping gene. The positions of marker proteins with their apparent molecular weights in kilodaltons (kD) are indicated for the Western blots. Bar graphs represent means ± standard errors of the means (SEM) (n = 3). ***, P < 0.001; *, P < 0.05; ns, nonsignificant (Student’s t test).
To determine whether the low DINO levels in HPV-positive cervical cancer lines were a consequence of HPV E6/UBE3A-mediated TP53 destabilization, HPV16 E6, alone or in combination with TP53, was depleted in HPV16-positive SiHa cells by transient transfection of the corresponding small interfering RNAs (siRNAs). To assess the efficiency of HPV16 E6 and TP53 depletion, TP53 protein levels were assessed by Western blotting. As expected, HPV16 E6 depletion caused an increase in TP53 steady-state levels, which was abrogated by TP53 codepletion (Fig. 1B). Like the canonical TP53 transcriptional target, CDKN1A, DINO levels increased upon E6 depletion, and this effect was abrogated by codepletion of TP53 (Fig. 1C). Hence, the low levels of DINO in HPV-positive cervical carcinoma lines likely represent a consequence of E6/UBE3A-mediated TP53 destabilization.
Acute DINO expression in HPV-positive cervical cancer cells reconstitutes dormant TP53 tumor suppressor activity.
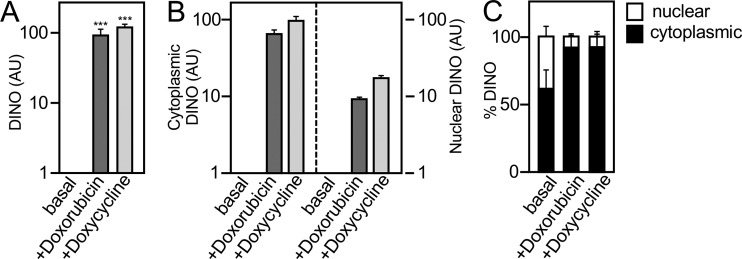
DINO expression is regulated by TP53 and has been reported to bind and stabilize TP53, thereby amplifying TP53 signaling. We have previously shown that HPV16 E7 expression causes TP53 stabilization and activation through DINO (44). Given that HPV16 E6 depletion increased DINO levels and caused a TP53-dependent increase in the TP53 transcriptional target CDKN1A in the HPV-positive SiHa cervical cancer line (Fig. 1), we next determined whether the dormant TP53 tumor suppressor pathway may be restored by DINO expression. Because high-level ectopic DINO expression may trigger TP53-dependent cytotoxic and/or cytostatic responses, we created vectors for doxycycline-regulated DINO expression and generated HPV16-positive SiHa and CaSki cervical cancer cell populations with doxycycline-regulated DINO expression. Cells expressing a vector with doxycycline-inducible green fluorescent protein (GFP) expression were also made to be used as controls. To ensure that doxycycline-induced DINO expression by this method mimics DINO induction by a biologically relevant stimulus, we compared SiHa cells with doxycycline-induced DINO expression to DINO expression in response to DNA damage. The chemotherapy agent doxorubicin, a known, potent inducer of DINO expression (43), was used for these experiments. Doxycycline induction caused a similar increase in DINO expression as treatment with doxorubicin (Fig. 2A). Moreover, subcellular fractionation experiments revealed that increases in cytoplasmic and nuclear DINO (Fig. 2B and C) were similar in doxycycline-induced and doxorubicin-treated SiHa cells. Hence, doxycycline-mediated DINO expression closely mirrors DINO induction in response to DNA damage.
FIG 2.
Doxycycline-mediated DINO expression mimics induction by DNA damage. DINO expression as analyzed by qRT-PCR in control vector-transduced SiHa cells (basal) or treated with 0.2 μg/ml doxorubicin for 24 h (+Doxorubicin) compared to acute DINO expression by treating inducible DINO vector-transduced SiHa cells with 1 μg/ml doxycycline for 48 h (+Doxycycline) (A). Quantification of the increases in the cytoplasmic and nuclear DINO levels by qRT-PCR (B). Assessment of the relative increases in the nuclear and cytoplasmic DINO pools by qRT-PCR (C). Expression data are presented in arbitrary units (AU) and are normalized to expression of the RPLP0 housekeeping gene. Bar graphs represent means ± SEM (n = 3). ***, P < 0.001 (Student’s t test).
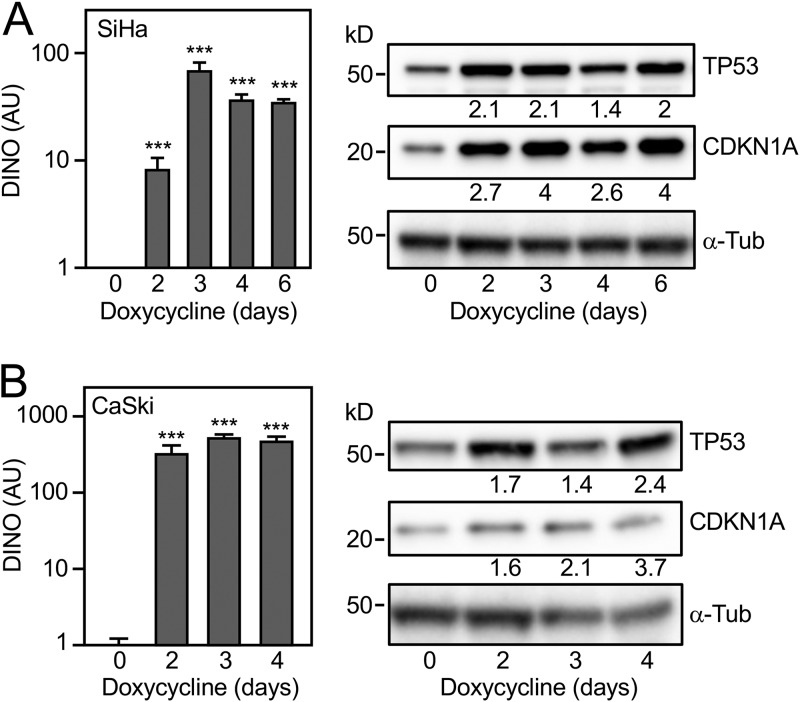
After validating the doxycycline-mediated expression system, we tested whether doxycycline-induced, acute DINO expression may override HPV16 E6/UBE3A-mediated TP53 inactivation and restore TP53 levels and/or activity in the HPV16-positive SiHa (Fig. 3A) and CaSki (Fig. 3B) cervical cancer cell lines. DINO expression was validated by qRT-PCR assays (Fig. 3A and B, left panels). Immunoblot experiments revealed higher levels of TP53 and concomitant increased expression of the canonical TP53 transcriptional target, CDKN1A, in SiHa and CaSki cells in response to DINO expression (Fig. 3A and B, right panels). These results show that acute DINO expression causes functional reactivation of dormant TP53 tumor suppressor signaling in HPV-positive cervical carcinoma lines.
FIG 3.
Acute DINO expression in HPV-positive cervical cancer cells causes reactivation of TP53 signaling. DINO expression in inducible DINO vector-transduced HPV16-positive SiHa (A) and CaSki (B) cervical cancer cells after treatment with 1 μg/ml doxycycline for the indicated number of days as determined by qRT-PCR. Expression data are presented in arbitrary units (AU) and are normalized to expression of the RPLP0 housekeeping gene. Bar graphs represent means ± SEM (n = 3). ***, P < 0.001; *, P < 0.05 (Student’s t test) (left panels). Changes in TP53 and CDKN1A protein levels were measured by immunoblotting with α-tubulin (α-Tub) serving as a loading control (right panels). The positions of marker proteins with their apparent molecular weights in kilodaltons (kD) are indicated.
DINO overrides HPV16 E6/UBE3A-mediated TP53 degradation.
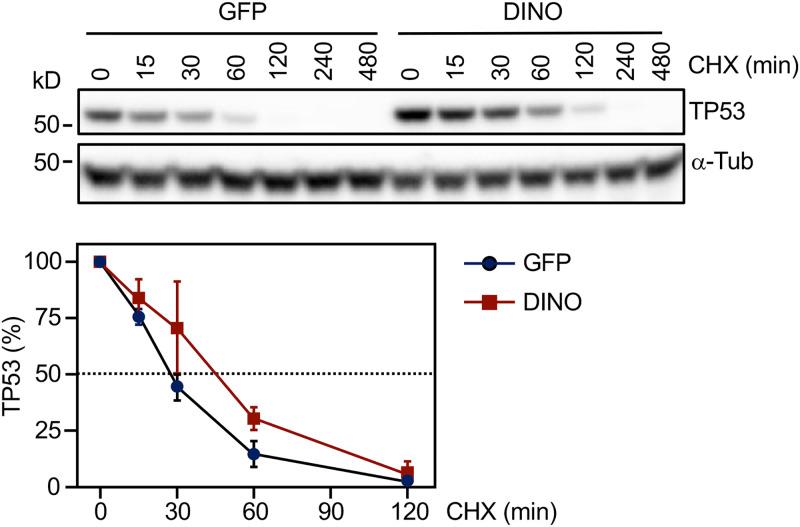
DINO was shown to stabilize TP53 in normal human cells where TP53 turnover is governed by MDM2-mediated ubiquitination (43). To determine whether the observed increases in TP53 upon DINO expression are caused by overriding HPV E6/UBE3A-mediated TP53 turnover, we performed a cycloheximide chase experiment. After inducing DINO expression in SiHa cells by a 48-h doxycycline treatment, cycloheximide was added to inhibit new protein synthesis. SiHa cells with conditional GFP expression were used as controls. TP53 steady-state levels were determined in extracts harvested at different times after cycloheximide treatment (Fig. 4, top panel). Quantification revealed that TP53 half-life was increased from ∼30 min in GFP-expressing control cells to ∼45 min in DINO-expressing SiHa cells (Fig. 4, bottom panel). Hence, acute DINO expression can override HPV16 E6/UBE3A-mediated TP53 degradation.
FIG 4.
DINO expression increases TP53 protein stability. HPV16-positive SiHa cervical cancer cells transduced with inducible DINO or GFP control vector were treated with 1 μg/ml doxycycline for 48 h, followed by 100 μg/ml cycloheximide (CHX) to block protein synthesis. Proteins lysates were prepared at various time points after cycloheximide addition, and TP53 levels were measured by immunoblotting and quantified to estimate the half-life of TP53 with α-tubulin (α-Tub) serving as a loading control. A representative blot is shown in the top panel. The positions of marker proteins with their apparent molecular weights in kilodaltons (kD) are indicated. Quantification representing means ± SEM from three experiments is shown in the bottom panel.
Ectopic DINO increases the susceptibility of HPV-positive cervical cancer cell lines to inducer of metabolic stress.
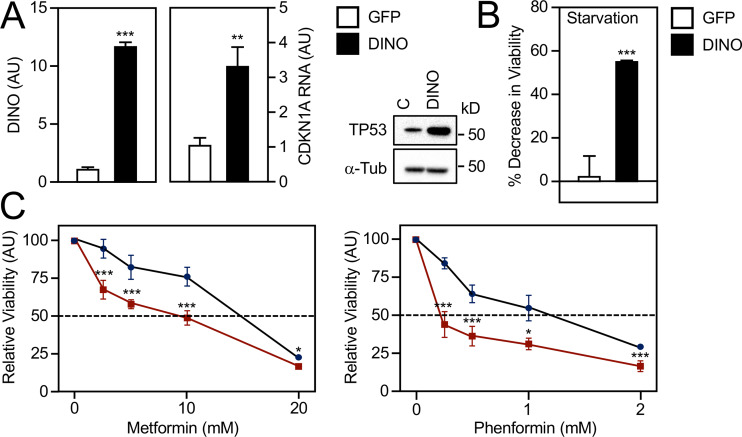
We previously reported that HPV16 E7-expressing HFKs have elevated DINO and that DINO depletion protected these cells from metabolic stress induced by starvation or by treatment with the antidiabetic biguanide drug metformin (44). Metformin and related biguanides are antidiabetic drugs that are being investigated for potential repurposing as anticancer agents because they activate AMP-activated protein kinase, which in turn has been reported to activate TP53 (48–50). Hence, we tested whether acute DINO expression in HPV-positive cancer cells with low endogenous DINO expression may render them vulnerable to metabolic stress. As expected, doxycycline induction of DINO in CaSki cells triggered increased mRNA expression of the TP53 transcriptional target CDKN1A and elevated TP53 steady-state levels (Fig. 5A). CaSki cells with acute DINO overexpression were significantly more vulnerable to serum deprivation and exhibited significantly enhanced sensitivity to metformin and the related more-potent biguanide drug phenformin (Fig. 5B). These experiments revealed that, consistent with our previous study (44), DINO is a crucial modulator of cell death during metabolic stress.
FIG 5.
Acute DINO expression increases susceptibility to metabolic stress. HPV16-positive CaSki cervical cancer cells transduced with inducible DINO or GFP control vector were each treated with 1 μg/ml doxycycline for 48 h. DINO expression and mRNA levels of the TP53 transcriptional target CDKN1A were determined by qRT-PCR. Expression data are presented in arbitrary units (AU) and are normalized to expression of the RPLP0 housekeeping gene (A, left panel). Concomitant changes in TP53 protein levels were assessed by immunoblotting, with α-tubulin (α-Tub) serving as a loading control. The positions of marker proteins with their apparent molecular weights in kilodaltons (kD) are indicated (A, right panel). GFP- or DINO-expressing CaSki cells were incubated with serum-free medium (B) or grown in normal-serum-containing medium supplemented with the indicated concentrations of metformin or phenformin for 72 h (C), and cell viability was assessed. Graphs represent means ± SEM (n = 3). ***, P < 0.001; **, P < 0.01; *, P < 0.05 (Student’s t test).
Ectopic DINO increases susceptibility of HPV-positive cervical cancer cell lines to chemotherapeutics.
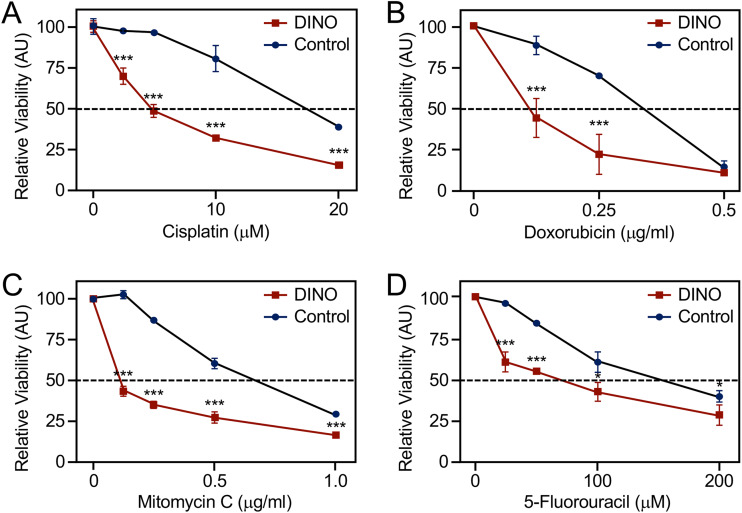
The lack of functional TP53 likely renders HPV-positive cervical tumors refractory to standard chemotherapy and radiation treatments (51). Hence, we tested whether acute, ectopic DINO expression may sensitize HPV-positive cervical cancer cells to chemotherapy drugs. We used CaSki cells for these experiments because SiHa cells were shown to be highly resistant to chemotherapy drugs (52). Chemotherapy involving the alkylating agent cisplatin and related platinum compounds has long been the standard-of-care for advanced, recurrent cervical cancers (53). Other widely used anticancer chemotherapy agents include the antimetabolite 5-fluorouracil (5-FU), the alkylating agent mitomycin C, and the DNA intercalating agent doxorubicin. Acute, doxycycline-mediated DINO expression rendered CaSki markedly more sensitive to cisplatin (Fig. 6A), doxorubicin (Fig. 6B), mitomycin C (Fig. 6C), and 5-FU (Fig. 6D) compared to control cells with doxycycline-regulated GFP expression. Hence, the sensitivity of cervical cancer cells to a variety of chemotherapy agents is modulated by DINO and presumably represents a consequence of reactivating the dormant TP53 tumor suppressor pathway.
FIG 6.
Acute DINO expression increases susceptibility to chemotherapy agents. Inducible DINO vector-transduced, HPV16-positive CaSki cervical cancer cells were treated with the indicated concentrations of cisplatin (A), doxorubicin (B), mitomycin C (C), and 5-fluorouracil (D). Cell viability was assessed at 72 h posttreatment. Graphs represent means ± SEM from single representative experiments, each performed in triplicate. ***, P < 0.001; *, P < 0.05 (Student’s t test). Similar results were obtained in three independent experiments.
DINO induction by DNA damage is independent of the ATM/CHK2/TP53 DNA damage signaling pathway.
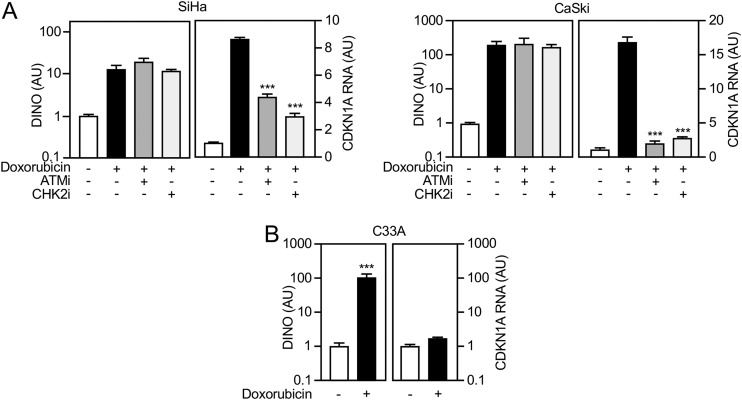
Increased DINO expression in response to DNA damage has been reported to be TP53 dependent (43). To discern whether DNA damage-mediated DINO expression is also TP53 dependent in cervical carcinoma lines, we performed epistasis analysis using small-molecule inhibitors of ataxia-telangiectasia mutated (ATM) and checkpoint kinase 2 (CHK2), two kinases that are well known to signal DNA damage to TP53 (54, 55). As expected, doxorubicin treatment of SiHa and CaSki cells caused a robust increase of DINO as well as the TP53 transcriptional target CDKN1A (Fig. 7A, right and left panels, respectively). Consistent with efficient inhibition of DNA damage-mediated TP53 activation by ATM or CHK2 inhibition, expression of the canonical TP53 target gene CDKN1A was dramatically reduced. In contrast, however, ATM or CHK2 inhibition did not significantly interfere with induction of DINO expression by doxorubicin in either SiHa or CaSki cells (Fig. 7A). These results indicate that DINO induction by doxorubicin is less dependent on ATM/CHK2-mediated TP53 activation than CDKN1A.
FIG 7.
DINO induction by DNA damage can occur independently of ATM/CHK2/TP53 DNA damage signaling. (A) The HPV16-positive SiHa (left) and CaSki (right) cervical cancer lines were treated with 0.2 μg/ml doxorubicin and either 10 μM ATM inhibitor KU-55933 (ATMi) or 5 μM CHK2 inhibitor BML-277 (CHK2i). After 24 h, expression of DINO and the canonical TP53 target gene CDKN1A was determined by qRT-PCR. (B) Doxorubicin-mediated induction of DINO and CDKN1A mRNA was also assessed in the HPV-negative C33A cell line that expresses the DNA binding-defective, TP53 R273H cancer hot spot mutant. Expression data are presented in arbitrary units (AU) and are normalized to expression of the RPLP0 housekeeping gene. Bar graphs represent means ± SEM (n = 3). ***, P < 0.001 (Student’s t test).
Based on this finding, we next tested whether doxorubicin treatment may also trigger DINO expression in the HPV-negative C33A cervical carcinoma line which expresses the DNA binding-defective TP53 R273H mutant (45–47). Doxorubicin treatment caused a robust increase in DINO levels whereas expression of the TP53 target gene CDKN1A remained unaltered (Fig. 7B). Hence, DINO induction in response to doxorubicin can efficiently occur in cells that lack functional TP53.
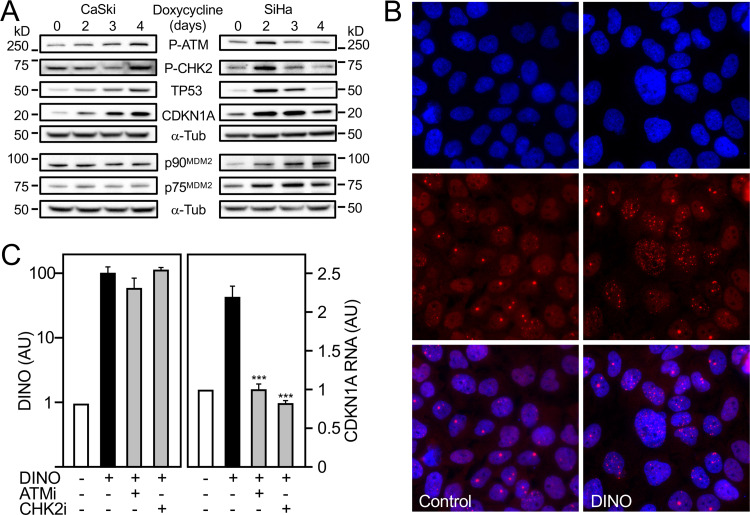
Acute DINO expression induces hallmarks of DNA damage signaling.
DINO has been reported to bind TP53, thereby stabilizing TP53 and amplifying DNA damage signaling (43). This predicts that acute DINO expression will cause TP53 stabilization independently of upstream DNA damage signaling. To experimentally test this model, we assessed ATM and CHK2 phosphorylation as well as TP53 stabilization and induction of TP53 transcriptional targets in response to acute, doxycycline-mediated DINO expression in CaSki and SiHa cervical carcinoma cells (Fig. 8A). Surprisingly, we detected robust phosphorylation of CHK2 at threonine 68 and ATM phosphorylation at serine 1981 that paralleled increases in TP53 and CDKN1A protein levels in both cell lines. In SiHa but not in CaSki cells, we also observed induction of the p90 and p75 MDM2 isoforms with a concomitant decrease in TP53 levels and CDKN1A expression (Fig. 8A). These results show that acute DINO expression triggers ATM and CHK2 activation. To determine whether acute DINO expression also induces other hallmarks of the DNA damage response, we investigated the appearance of 53BP1 nuclear foci in CaSki cells. Doxycycline-treated cells with conditional GFP expression were used as negative controls. Acute expression of DINO caused an increased appearance of 53BP1 nuclear foci (Fig. 8B).
FIG 8.
Acute DINO expression induces hallmarks of DNA damage signaling. HPV16-positive CaSki (left) and SiHa (right) cervical cancer lines with inducible DINO expression were treated with 1 μg/ml doxycycline, and levels of phospho-Ser1981 ATM (P-ATM), phospho-Thr68 CHK2 (P-CHK2), TP53, CDKN1A, and the p90 and p75 MDM2 isoforms were assessed by immunoblot analysis with α-tubulin (α-Tub) serving as a loading control. The MDM2 blotting assays were performed in a separate experiment but using aliquots of the same protein extracts as those used for the other blotting assays. The positions of marker proteins with their apparent molecular weights in kilodaltons (kD) are indicated (A). Nuclear 53BP1 foci in CaSki cells in control and after doxycycline-mediated DINO expression. Nuclei were stained with DAPI. Representative immunofluorescence microscopy images are shown; similar results were obtained in two independently performed microscopy experiments. Top panels show DAPI-stained nuclei, middle panels show nuclear 53BP1 foci, and lower panels show merged images (B). CaSki cells with inducible DINO expression were treated with 1 μg/ml doxycycline and 10 μM ATM inhibitor KU-55933 (ATMi) or 5 μM CHK2 inhibitor BML-277 (CHK2i), and expression of DINO and the canonical transcriptional TP53 target gene CDKN1A was determined by qRT-PCR. Expression data are presented in arbitrary units (AU) and are normalized to expression of the RPLP0 housekeeping gene. Bar graphs represent means ± SEM (n = 3). ***, P < 0.001 (Student’s t test) (C).
To determine whether TP53 activation in response to acute DINO expression was dependent on ATM and CHK2 activation, we treated CaSki cells with CHK2 or ATM inhibitors and assessed mRNA expression of the canonical TP53 transcriptional target CDKN1A. While ATM and CHK2 inhibition did not interfere with doxycycline-mediated DINO induction, these treatments blocked TP53-mediated CDKN1A mRNA expression (Fig. 8C).
Taken together, our results indicate that DINO-mediated TP53 stabilization and activation in cervical carcinoma cells occur through a pathway that involves activation of the DNA damage signaling pathway.
DISCUSSION
The TP53 tumor suppressor, dubbed the “guardian of the genome,” is a key component of an innate cellular defense signaling network that functions to remove cells that have suffered genetic or epigenetic alterations that interfere with normal cellular homeostasis from the proliferative pool (6). Hence, acquisition of defects in the TP53 surveillance pathway is an almost universal and rate-limiting step in human carcinogenesis. Functional restoration of TP53 tumor suppressor signaling in human cancers was shown to have cytostatic or cytotoxic effects (56). In addition to proteins, noncoding RNAs, particularly microRNAs and lncRNAs, have emerged as key regulators and modulators of TP53 signaling (40–42, 57).
DINO is an lncRNA that functions as a regulator as well as a modulator of TP53 (43). DINO was identified as a TP53 transcriptional target that can amplify TP53 signaling by binding and stabilizing TP53 and was shown to be a component of DNA-bound TP53 tetramers. DINO binding involves the C-terminal 31 amino acids of TP53 whereas MDM2, the ubiquitin ligase that targets TP53 for rapid proteasomal degradation, binds to TP53 sequences within the amino-terminal transactivation domain (43, 58). Hence, it is unlikely that DINO and MDM2 directly compete for binding to the same TP53 sequences. Similarly, the TP53 C-terminal 31 amino acids are not necessary for E6/UBE3A binding, and hence, interaction with DINO is not predicted to directly compete with E6/UBE3A binding (59). Interestingly, TP53 has long been known to interact with RNAs, and the TP53 C terminus has been reported to be critical for RNA binding, which is regulated by the acetylation status of multiple lysine residues (60). It will be interesting to determine whether DINO binding is similarly regulated by TP53 posttranslational modifications.
In this study, we show that HPV-positive cervical cancer lines contain low levels of DINO as a consequence of HPV16 E6/UBE3A-mediated degradation. Acute DINO expression that mimics DINO induction in response to DNA damage causes TP53 stabilization and functional reactivation as evidenced by increased expression of the canonical TP53 transcriptional target CDKN1A. In the case of SiHa cells, we consistently observed a dip in the increase of TP53 and CDKN1A protein levels at day 3 or 4 after doxycycline-induced DINO expression. TP53 levels and activity are regulated by positive and negative feedback loops (61–63). The observed transient TP53 decrease may indeed be caused by increased expression of the MDM2 p90 and p75 isoforms (64), which we observed in SiHa cells but less so in CaSki cells within the analyzed time course. Alternatively, given that these experiments were performed with polyclonal cell populations, the observed dip might be attributable to the heterogeneity of DINO induction levels. Nonetheless, the observed ∼2-fold increase in TP53 levels in response to acute DINO expression is similar to what we observed upon HPV16 E6 silencing.
Despite multiple attempts, we did not succeed in generating cervical cancer lines with constitutive, ectopic, high-level DINO expression. Hence, we generated cervical cancer lines with doxycycline-regulated DINO expression. Doxycycline treatment increased DINO to similar levels as in cells that were treated with the DNA damage-inducing chemotherapy agent doxorubicin. Under both conditions, there is a more dramatic increase of DINO in the cytoplasm than in the nucleus. The biological significance of these two DINO populations is currently unknown. It is noted, however, that TP53 shuttles between the nucleus and cytoplasm and that nuclear export is necessary for degradation by MDM2 and E6/UBE3A (65). Therefore, nuclear and cytoplasmic DINO could each modulate TP53 turnover and activity.
We were initially surprised that despite TP53 stabilization and functional reactivation, acute, doxycycline-mediated induction of DINO did not noticeably inhibit the viability of SiHa and CaSki cells. This suggests that DINO expression achieved by doxycycline induction may not reach levels that surpass the critical threshold required to drive a TP53-mediated cytotoxic response (66). Importantly, however, TP53-mediated transcriptional responses also include expression of negative regulatory proteins, including the MDM2 ubiquitin ligase, that dampen TP53 activity. We consistently observed increased MDM2 protein expression in SiHa cells upon acute DINO expression in cells with a concomitant decrease in TP53 and CDKN1A levels. Moreover, HPV16 E7-expressing keratinocytes express high levels of DINO and TP53, and they proliferate at a similar rate as parental or HPV16 E6/E7-coexpressing cells, which express low TP53 and DINO (44). HPV16 E7-expressing cells, however, are susceptible to cell death when subjected to metabolic stress (2). The vulnerability to metabolic stress was shown to be TP53 dependent (67) and abrogated upon DINO depletion (44). Here, we show that that acute DINO expression markedly increases the vulnerability of cervical carcinoma cells to a variety of inducers of metabolic stress and increases their susceptibility to multiple classes of DNA damage-inducing chemotherapy agents, including cisplatin, which has long been the standard-of-care chemotherapy agent for the treatment of invasive cervical carcinoma.
After DNA damage, DINO was found in complex with TP53 and detected in DNA-bound TP53 transcription factor complexes, thereby amplifying TP53 tumor suppressor signaling (43). We were thus surprised that even after DNA damage, the major fraction of DINO was detected in the cytoplasm. Hence, DINO may have other cellular targets and may possess biological activities that are independent of transcriptional, nuclear TP53 tumor suppressor signaling.
In support of this model, we discovered that in contrast to other TP53-responsive genes, induction of DINO by doxorubicin-mediated DNA damage occurs even when the CHK2 and ATM DNA damage kinases are inhibited. Moreover, DINO is induced by DNA damage in C33A cells that express the DNA binding-defective TP53 R273H cancer hot spot mutant, suggesting that DINO can be induced through additional ATM/CHK2- and TP53-independent mechanisms, although the molecular consequences of increased DINO expression in TP53 mutant cells are currently unknown. In addition to ATM/CHK2, DNA damage may also lead to activation of the ATM-and Rad3-related (ATR) kinase and/or the DNA-dependent protein kinase (DNA-PK) pathways, which, together with ATM, comprise “the trinity of kinases” that signal the DNA damage response (68). TP53-independent, epigenetic mechanisms of DINO expression have also been described. The initial trigger of HPV16 E7-mediated DINO induction that leads to TP53 stabilization and activation involves the H3K27 demethylase KDM6A (44), and HPV16 E7 is well known to cause double-strand DNA breaks (69, 70). Similarly, an orphan nuclear receptor, nuclear receptor subfamily 2 group E member 3 (NR2E3), and the associated KDM1A (LSD1) H3K4 demethylase were shown to be necessary for efficient induction of DINO and TP53 activity in response to liver damage by N-acetyl-p-benzoquinone imine-mediated oxidative stress (71). It is noted that in addition to DNA damage, doxorubicin can also induce free radical release, thereby causing oxidative stress (72).
Our studies also provide evidence that in addition to TP53 binding and stabilization and by functioning as a component of DNA-bound TP53 transcription factor complexes (43), DINO can cause or amplify TP53 activation through a mechanism that involves activation of DNA damage response signaling as evidenced by ATM and ATR activation and the appearance of cells that contain larger numbers of 53BP1 nuclear foci. Moreover, ATM or CHK2 inhibition interfered with DINO-mediated TP53 activation as assessed by CDKN1A transcription.
lncRNAs have emerged as critical regulators of cellular DNA damage responses, but the molecular mechanisms by which DINO drives DNA damage signaling remain to be determined. Similarly to DINO, the long intergenic radiation-responsive noncoding RNAs (LIRRs) induce DNA damage signaling through mechanisms that are not clear (73). On the other hand, the GUARDIN lncRNA, which is essential for genomic stability, inhibits DNA damage through mechanisms involving the stabilization of telomeric repeat-binding factor 2 (TRF2) and breast cancer type 1 susceptibility protein (BRCA1) (74). One possibility is that DINO expression induces double-stranded DNA breaks. Alternatively, DINO may drive the DNA damage response by modulating signaling events by scaffolding and recruiting critical proteins such as ATM, 53BP1, H2A.X, and RNF168. Lastly, it is possible that the effect is indirect, i.e., that DINO regulates expression of other, coding or noncoding genes that may induce DNA damage or modulate DNA damage repair or DNA damage repair signaling. The HITT (HIF-1α inhibitor at translation level) lncRNA, for example, was reported to blunt ATM activation by directly binding to ATM and blocking recruitment of the MRE11-RAD50-NBS1 complex (75).
Taken together, these results indicate that DINO not only is a “damage-induced noncoding” RNA but may also function as a “damage-inducing noncoding RNA.” This hypothesis is based on results obtained with cells that were engineered to acutely express DINO in response to doxycycline. While this represents an artificial method of modulating DINO expression, it is noted that the overall increase in DINO expression and the subcellular DINO localization mirrors what is observed upon induction of DNA damage, and hence, it is unlikely to be entirely supraphysiological. Moreover, it is widely recognized that lncRNAs can act as components of DNA damage response and repair processes (76). It will be important to determine whether DINO directly induces DNA damage and whether it is a component of complexes that form to sense or mark sites of DNA damage and/or are involved in DNA break repair.
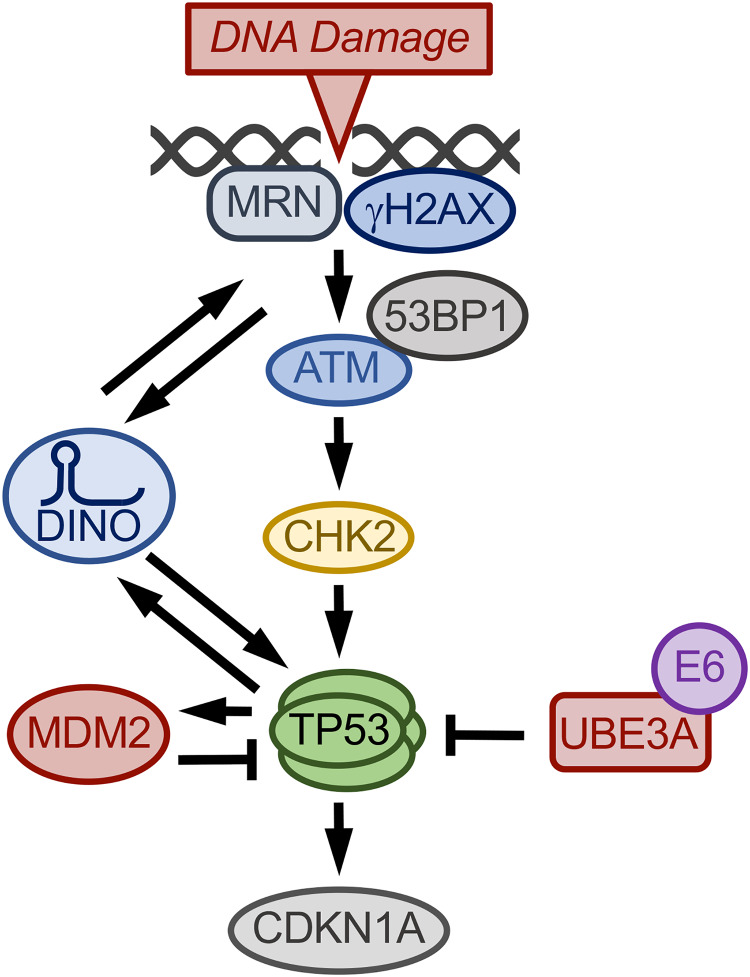
In summary, we show that the dormant TP53 tumor suppressor pathway in HPV-positive cervical cancer lines can be functionally reactivated by modulating DINO. Our results support a model whereby DINO activates TP53 through a CHK2/ATM-dependent pathway. The concomitant ATM/CHK-mediated activation of TP53 then triggers a further, TP53-dependent increase in DINO, which in turn amplifies DNA damage repair signaling. This causes further TP53 activation. DINO may also augment TP53 signaling as a component of DNA-bound TP53 transcription factor complexes (43) (Fig. 9). DINO-mediated TP53 reactivation causes cervical cancer cells to be more sensitive to standard chemotherapeutics and induces marked vulnerability to metabolic stress. Moreover, we found that DNA damage can induce DINO expression despite ATM/CHK2 inhibition and in C33A cells that express the DNA binding-defective TP53 R273H cancer hot spot mutant. These findings warrant further studies examining whether these DINO activities are also operative in non-HPV-associated tumors with different aberrations in the TP53 tumor suppressor pathway. Given that lncRNAs can be targeted therapeutically by nucleic acid-based mimics and inhibitors, our findings suggest that modulation of DINO activity may have therapeutic value by restoring TP53 tumor suppressor activity in some tumor types, including HPV-positive tumors.
FIG 9.
Model of DINO regulation in HPV-positive cervical cancer cells. In response to DNA damage, DINO is induced through an ATM/CHK2/TP53-independent mechanism. DNA damage also triggers TP53 activation through ATM/CHK2-dependent signaling, which causes increased expression of TP53 transcriptional target genes, including CDKN1A and DINO. DINO further activates TP53 by inducing hallmarks of the DNA damage response signaling pathway as evidenced by 53BP1 nuclear foci and ATM and CHK2 activation. By binding to DNA-bound TP53 transcription factor complexes, DINO may enhance TP53 transcriptional activity. DINO activity is balanced by TP53-mediated MDM2 upregulation as well as the E6/UBE3A complex, which targets TP53 for proteasomal degradation.
MATERIALS AND METHODS
Cell culture.
Isolation, generation, and maintenance of primary human foreskin keratinocytes (HFKs) and HPV16 E6/E7-expressing HFKs have been previously described (44). The C33A, CaSki, HeLa, and SiHa cervical cancer cell lines were purchased from the American Type Culture Collection (ATCC, Manassas, VA) and maintained in Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 10% fetal bovine serum. Subcellular fractionation was carried out using the “Rapid, Efficient And Practical” (REAP) method (77). Doxycycline, cisplatin, and doxorubicin were purchased from Sigma-Aldrich (St. Louis, MO). Mitomycin C was purchased from Thermo Fisher Scientific (Waltham, MA). Fluorouracil (5-FU), ATMi (KU-55933), and CHK2i (BML-277) were purchased from Selleck Chemicals (Houston, TX). Acute DINO expression was induced by treating cells with 1 μg/ml doxycycline, made freshly for each use.
Expression plasmids.
The expression vector for acute DINO expression was created by inserting the full-length DINO sequence into the pLIX_403 Puro vector backbone (a gift from David Root; Addgene: plasmid no. 41395). In short, DINO sequences were PCR amplified from a previously published plasmid (a gift from Howard Chang) (43) using primers 5′-CACCGCCGAGTTCCAGC-3′ (forward) and 5′-TTCCAGAATTGTCCTTTATTTATGTCATCTCC-3′ (reverse) and cloned into the Gateway entry vector using the pENTR directional TOPO cloning kit (Invitrogen). DINO sequences were then transferred to the pLIX_403 Puro destination vector by standard Gateway-based in vitro recombination according to the manufacturer’s protocols. The inserted DINO sequences were verified by DNA sequencing. The pLIX-based plasmid for doxycycline-regulated green fluorescent protein (GFP) expression was a kind gift from James DeCaprio (78).
Western blotting and antibodies.
Western blot assays were performed as previously described (44), using TP53 (OP43; Calbiochem), RB1 (OP66; Millipore), CDKN1A (ab109520; Abcam), phospho-ATM (Ser1981) (5833; CST), phospho-Chk2 (Thr68) (2197; CST) and MDM2 (OP46; Millipore), and α-tubulin (ab18251; Abcam) specific antibodies at the dilutions recommended by the manufacturers. Secondary antibodies were horseradish peroxidase (HRP)-conjugated anti-mouse antibody (NA931; GE Healthcare Life Sciences) and HRP-conjugated anti-rabbit antibody (NA934V; GE Healthcare Life Sciences; 1:10,000). Antigen-antibody complexes were visualized by Enhanced Chemiluminescence (Life Technologies), and signals were digitally acquired on a G:Box Chemi-XX6 imager with Genesys software (Syngene). Protein bands were quantified using GeneTools software (Syngene).
RNA interference.
The following siRNAs were purchased from Thermo Scientific Dharmacon: nontargeting pool (D-001810-10), TP53 targeting pool (L-003329-00), and a custom-designed HPV16 E6 siRNA duplex, 5′-CCACAGUUAUGCACAGAGCTT-3′ (79). Cells were transfected at a 30 nM siRNA concentration using the Lipofectamine RNAiMax reagent (Invitrogen) per the manufacturer’s instructions.
qRT-PCR.
Total RNA was isolated and analyzed as previously described (44). The following primer pairs were used for qRT-PCR assays: HPV16 E6, 5′-TGCAATGTTTCAGGACCCA-3′ (forward) and 5′-CATGTATAGTTGTTTGCAGCTCTGT-3′ (reverse); DINO, 5′-GGAGGCAAAAGTCCTGTGTT-3′ (forward) and 5′-GGGCTCAGAGAAGTCTGGTG-3′ (reverse); CDKN1A, 5′-CATGTGGACCTGTCACTGTCTTGTA-3′ (forward) and 5′-GAAGATCAGCCGGCGTTTG-3′ (reverse); RPLP0, 5′-ATCAACGGGTACAAACGAGTC-3′ (forward) and 5′-CAGATGGATCAGCCAAGAAGG-3′ (reverse). The expression data shown were quantified using the threshold cycle (ΔΔCT) method by normalizing expression of all the qPCR targets to a housekeeping gene, RPLP0.
Immunofluorescence microscopy.
Cells grown on coverslips were fixed in 3.7% formaldehyde for 30 min, permeabilized in 1% Triton X-100 for 10 min, and blocked in 2.5% donkey serum in phosphate-buffered saline (PBS) for 1 h. After brief washing in PBS, coverslips were incubated with rabbit anti-53BP1 antibody (ab36823; Abcam; 1:250) for 1 h at room temperature. An Alexa Fluor-conjugated secondary antibody (donkey anti-rabbit 594, A21207 [Thermo], 1:1,000) was used. Nuclei were stained with 4′,6-diamidino-2-phenylindole (DAPI) in ProLong Diamond antifade mountant (Thermo Fisher catalog no. P36971). Images were captured using a Nikon Eclipse Ti2 microscope. DAPI and Alexa Fluor 594 fluorophores were excited with 405-nm and 594-nm laser lines, respectively. Images with merged DAPI and Alexa Fluor 594 channels were generated using FIJI (https://imagej.net/Fiji).
Cell viability assays.
Twenty thousand CaSki cells per well were seeded in a 12-well plate. Drugs were added at 24 h after doxycycline induction. At 72 h after drug treatment, cells were incubated with fresh medium containing 10 μg/ml resazurin (Sigma). Resazurin conversion was measured with a Synergy H1 microplate reader (BioTek) with 560-nm excitation and 590-nm emission filters as previously described (80).
ACKNOWLEDGMENTS
We thank Howard Chang (Stanford University) and James DeCaprio (Dana-Farber Cancer Institute) for generously sharing reagents; Al Klingelhutz (University of Iowa) for providing telomerase-immortalized human foreskin keratinocytes; Malavika Raman for the use of her fluorescence microscope facility; Warda Aman for help with immunofluorescence experiments; Amy Yee, Philip Hinds, Peter Juo, Claire Moore, and members of the Munger Lab for stimulating discussions and valuable suggestions throughout the course of this work; and the reviewers for their constructive comments and suggestions on the manuscript.
This work was supported by PHS grants AI147176, CA066980, and CA228543 (K.M.) and a Dean’s Fellowship and a Tufts Collaborative Cancer Biology Award from the Tufts Graduate School of Biomedical Sciences (S.S.).
Footnotes
This article is a direct contribution from Karl Munger, a Fellow of the American Academy of Microbiology, who arranged for and secured reviews by Alison McBride, NIAID, NIH, and Laimonis Laimins, Northwestern University.
Citation Sharma S, Munger K. 2020. Expression of the long noncoding RNA DINO in human papillomavirus-positive cervical cancer cells reactivates the dormant TP53 tumor suppressor through ATM/CHK2 signaling. mBio 11:e01190-20. https://doi.org/10.1128/mBio.01190-20.
REFERENCES
- 1.Boyer SN, Wazer DE, Band V. 1996. E7 protein of human papilloma virus-16 induces degradation of retinoblastoma protein through the ubiquitin-proteasome pathway. Cancer Res 56:4620–4624. [PubMed] [Google Scholar]
- 2.Jones DL, Munger K. 1997. Analysis of the p53-mediated G1 growth arrest pathway in cells expressing the human papillomavirus type 16 E7 oncoprotein. J Virol 71:2905–2912. doi: 10.1128/JVI.71.4.2905-2912.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Momand J, Zambetti GP, Olson DC, George D, Levine AJ. 1992. The mdm-2 oncogene product forms a complex with the p53 protein and inhibits p53-mediated transactivation. Cell 69:1237–1245. doi: 10.1016/0092-8674(92)90644-r. [DOI] [PubMed] [Google Scholar]
- 4.Haupt Y, Maya R, Kazaz A, Oren M. 1997. Mdm2 promotes the rapid degradation of p53. Nature 387:296–299. doi: 10.1038/387296a0. [DOI] [PubMed] [Google Scholar]
- 5.Kubbutat MH, Jones SN, Vousden KH. 1997. Regulation of p53 stability by Mdm2. Nature 387:299–303. doi: 10.1038/387299a0. [DOI] [PubMed] [Google Scholar]
- 6.Lane DP. 1992. Cancer. p53, guardian of the genome. Nature 358:15–16. doi: 10.1038/358015a0. [DOI] [PubMed] [Google Scholar]
- 7.Kastenhuber ER, Lowe SW. 2017. Putting p53 in context. Cell 170:1062–1078. doi: 10.1016/j.cell.2017.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huibregtse JM, Scheffner M, Howley PM. 1993. Cloning and expression of the cDNA for E6-AP, a protein that mediates the interaction of the human papillomavirus E6 oncoprotein with p53. Mol Cell Biol 13:775–784. doi: 10.1128/mcb.13.2.775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scheffner M, Werness BA, Huibregtse JM, Levine AJ, Howley PM. 1990. The E6 oncoprotein encoded by human papillomavirus types 16 and 18 promotes the degradation of p53. Cell 63:1129–1136. doi: 10.1016/0092-8674(90)90409-8. [DOI] [PubMed] [Google Scholar]
- 10.Scheffner M, Huibregtse JM, Vierstra RD, Howley PM. 1993. The HPV-16 E6 and E6-AP complex functions as a ubiquitin-protein ligase in the ubiquitination of p53. Cell 75:495–505. doi: 10.1016/0092-8674(93)90384-3. [DOI] [PubMed] [Google Scholar]
- 11.Cancer Genome Atlas Research Network. 2017. Integrated genomic and molecular characterization of cervical cancer. Nature 543:378–384. doi: 10.1038/nature21386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cancer Genome Atlas Network. 2015. Comprehensive genomic characterization of head and neck squamous cell carcinomas. Nature 517:576–582. doi: 10.1038/nature14129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Larsson CA, Moyer SM, Liu B, Michel KA, Pant V, Yang P, Wong J, El-Naggar AK, Krahe R, Lozano G. 2018. Synergistic and additive effect of retinoic acid in circumventing resistance to p53 restoration. Proc Natl Acad Sci U S A 115:2198–2203. doi: 10.1073/pnas.1719001115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li Q, Zhang Y, El-Naggar AK, Xiong S, Yang P, Jackson JG, Chau G, Lozano G. 2014. Therapeutic efficacy of p53 restoration in Mdm2-overexpressing tumors. Mol Cancer Res 12:901–911. doi: 10.1158/1541-7786.MCR-14-0089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martins CP, Brown-Swigart L, Evan GI. 2006. Modeling the therapeutic efficacy of p53 restoration in tumors. Cell 127:1323–1334. doi: 10.1016/j.cell.2006.12.007. [DOI] [PubMed] [Google Scholar]
- 16.Ventura A, Kirsch DG, McLaughlin ME, Tuveson DA, Grimm J, Lintault L, Newman J, Reczek EE, Weissleder R, Jacks T. 2007. Restoration of p53 function leads to tumour regression in vivo. Nature 445:661–665. doi: 10.1038/nature05541. [DOI] [PubMed] [Google Scholar]
- 17.Wang Y, Suh Y-A, Fuller MY, Jackson JG, Xiong S, Terzian T, Quintás-Cardama A, Bankson JA, El-Naggar AK, Lozano G. 2011. Restoring expression of wild-type p53 suppresses tumor growth but does not cause tumor regression in mice with a p53 missense mutation. J Clin Invest 121:893–904. doi: 10.1172/JCI44504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xue W, Zender L, Miething C, Dickins RA, Hernando E, Krizhanovsky V, Cordon-Cardo C, Lowe SW. 2007. Senescence and tumour clearance is triggered by p53 restoration in murine liver carcinomas. Nature 445:656–660. doi: 10.1038/nature05529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Burgess A, Chia KM, Haupt S, Thomas D, Haupt Y, Lim E. 2016. Clinical overview of MDM2/X-targeted therapies. Front Oncol 6:7. doi: 10.3389/fonc.2016.00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang S, Zhao Y, Aguilar A, Bernard D, Yang CY. 2017. Targeting the MDM2-p53 protein-protein interaction for new cancer therapy: progress and challenges. Cold Spring Harb Perspect Med 7:a026245. doi: 10.1101/cshperspect.a026245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Espadinha M, Barcherini V, Lopes EA, Santos MM. 2018. An update on MDMX and dual MDM2/X inhibitors. Curr Top Med Chem 18:647–660. doi: 10.2174/1568026618666180604080119. [DOI] [PubMed] [Google Scholar]
- 22.Hengstermann A, Linares LK, Ciechanover A, Whitaker NJ, Scheffner M. 2001. Complete switch from Mdm2 to human papillomavirus E6-mediated degradation of p53 in cervical cancer cells. Proc Natl Acad Sci U S A 98:1218–1223. doi: 10.1073/pnas.98.3.1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Horner SM, DeFilippis RA, Manuelidis L, DiMaio D. 2004. Repression of the human papillomavirus E6 gene initiates p53-dependent, telomerase-independent senescence and apoptosis in HeLa cervical carcinoma cells. J Virol 78:4063–4073. doi: 10.1128/jvi.78.8.4063-4073.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.DeFilippis RA, Goodwin EC, Wu L, DiMaio D. 2003. Endogenous human papillomavirus E6 and E7 proteins differentially regulate proliferation, senescence, and apoptosis in HeLa cervical carcinoma cells. J Virol 77:1551–1563. doi: 10.1128/jvi.77.2.1551-1563.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beer-Romero P, Glass S, Rolfe M. 1997. Antisense targeting of E6AP elevates p53 in HPV-infected cells but not in normal cells. Oncogene 14:595–602. doi: 10.1038/sj.onc.1200872. [DOI] [PubMed] [Google Scholar]
- 26.Wei Q. 2005. Pitx2a binds to human papillomavirus type 18 E6 protein and inhibits E6-mediated P53 degradation in HeLa cells. J Biol Chem 280:37790–37797. doi: 10.1074/jbc.M502974200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhou Y, Wei Y, Zhu J, Wang Q, Bao L, Ma Y, Chen Y, Feng D, Zhang A, Sun J, Nallar SC, Shen K, Kalvakolanu DV, Xiao W, Ling B. 2011. GRIM-19 disrupts E6/E6AP complex to rescue p53 and induce apoptosis in cervical cancers. PLoS One 6:e22065. doi: 10.1371/journal.pone.0022065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bonetta AC, Mailly L, Robinet E, Trave G, Masson M, Deryckere F. 2015. Artificial microRNAs against the viral E6 protein provoke apoptosis in HPV positive cancer cells. Biochem Biophys Res Commun 465:658–664. doi: 10.1016/j.bbrc.2015.07.144. [DOI] [PubMed] [Google Scholar]
- 29.Belyaeva TA, Nicol C, Cesur O, Trave G, Blair GE, Stonehouse NJ. 2014. An RNA aptamer targets the PDZ-binding motif of the HPV16 E6 oncoprotein. Cancers (Basel) 6:1553–1569. doi: 10.3390/cancers6031553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zanier K, Stutz C, Kintscher S, Reinz E, Sehr P, Bulkescher J, Hoppe-Seyler K, Travé G, Hoppe-Seyler F. 2014. The E6AP binding pocket of the HPV16 E6 oncoprotein provides a docking site for a small inhibitory peptide unrelated to E6AP, indicating druggability of E6. PLoS One 9:e112514. doi: 10.1371/journal.pone.0112514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stutz C, Reinz E, Honegger A, Bulkescher J, Schweizer J, Zanier K, Trave G, Lohrey C, Hoppe-Seyler K, Hoppe-Seyler F. 2015. Intracellular analysis of the interaction between the human papillomavirus type 16 E6 oncoprotein and inhibitory peptides. PLoS One 10:e0132339. doi: 10.1371/journal.pone.0132339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ramirez J, Poirson J, Foltz C, Chebaro Y, Schrapp M, Meyer A, Bonetta A, Forster A, Jacob Y, Masson M, Deryckere F, Trave G. 2015. Targeting the two oncogenic functional sites of the HPV E6 oncoprotein with a high-affinity bivalent ligand. Angew Chem Int Ed Engl 54:7958–7962. doi: 10.1002/anie.201502646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Malecka KA, Fera D, Schultz DC, Hodawadekar S, Reichman M, Donover PS, Murphy ME, Marmorstein R. 2014. Identification and characterization of small molecule human papillomavirus E6 inhibitors. ACS Chem Biol 9:1603–1612. doi: 10.1021/cb500229d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Celegato M, Messa L, Goracci L, Mercorelli B, Bertagnin C, Spyrakis F, Suarez I, Cousido-Siah A, Travé G, Banks L, Cruciani G, Palù G, Loregian A. 2020. A novel small-molecule inhibitor of the human papillomavirus E6-p53 interaction that reactivates p53 function and blocks cancer cells growth. Cancer Lett 470:115–125. doi: 10.1016/j.canlet.2019.10.046. [DOI] [PubMed] [Google Scholar]
- 35.Ricci-López J, Vidal-Limon A, Zunñiga M, Jimènez VA, Alderete JB, Brizuela CA, Aguila S. 2019. Molecular modeling simulation studies reveal new potential inhibitors against HPV E6 protein. PLoS One 14:e0213028. doi: 10.1371/journal.pone.0213028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Anastasiadou E, Jacob LS, Slack FJ. 2018. Non-coding RNA networks in cancer. Nat Rev Cancer 18:5–18. doi: 10.1038/nrc.2017.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hanahan D, Weinberg RA. 2011. Hallmarks of cancer: the next generation. Cell 144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 38.Schmitt AM, Chang HY. 2016. Long noncoding RNAs in cancer pathways. Cancer Cell 29:452–463. doi: 10.1016/j.ccell.2016.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sharma S, Munger K. 2020. The role of long noncoding RNAs in human papillomavirus-associated pathogenesis. Pathogens 9:289. doi: 10.3390/pathogens9040289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chaudhary R, Lal A. 2017. Long noncoding RNAs in the p53 network. Wiley Interdiscip Rev RNA 8:e1410. doi: 10.1002/wrna.1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Grossi E, Sanchez Y, Huarte M. 2016. Expanding the p53 regulatory network: LncRNAs take up the challenge. Biochim Biophys Acta 1859:200–208. doi: 10.1016/j.bbagrm.2015.07.011. [DOI] [PubMed] [Google Scholar]
- 42.Lin T, Hou P-F, Meng S, Chen F, Jiang T, Li M-L, Shi M-L, Liu J-J, Zheng J-N, Bai J. 2019. Emerging roles of p53 related lncRNAs in cancer progression: a systematic review. Int J Biol Sci 15:1287–1298. doi: 10.7150/ijbs.33218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schmitt AM, Garcia JT, Hung T, Flynn RA, Shen Y, Qu K, Payumo AY, Peres-da-Silva A, Broz DK, Baum R, Guo S, Chen JK, Attardi LD, Chang HY. 2016. An inducible long noncoding RNA amplifies DNA damage signaling. Nat Genet 48:1370–1376. doi: 10.1038/ng.3673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sharma S, Munger K. 2020. KDM6A mediated expression of the long noncoding RNA DINO causes TP53 tumor suppressor stabilization in human papillomavirus type 16 E7 expressing cells. J Virol 94:e02178-19. doi: 10.1128/JVI.02178-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kitayner M, Rozenberg H, Kessler N, Rabinovich D, Shaulov L, Haran TE, Shakked Z. 2006. Structural basis of DNA recognition by p53 tetramers. Mol Cell 22:741–753. doi: 10.1016/j.molcel.2006.05.015. [DOI] [PubMed] [Google Scholar]
- 46.Bullock AN, Fersht AR. 2001. Rescuing the function of mutant p53. Nat Rev Cancer 1:68–76. doi: 10.1038/35094077. [DOI] [PubMed] [Google Scholar]
- 47.Scheffner M, Münger K, Byrne JC, Howley PM. 1991. The state of the p53 and retinoblastoma genes in human cervical carcinoma cell lines. Proc Natl Acad Sci U S A 88:5523–5527. doi: 10.1073/pnas.88.13.5523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhou G, Myers R, Li Y, Chen Y, Shen X, Fenyk-Melody J, Wu M, Ventre J, Doebber T, Fujii N, Musi N, Hirshman MF, Goodyear LJ, Moller DE. 2001. Role of AMP-activated protein kinase in mechanism of metformin action. J Clin Invest 108:1167–1174. doi: 10.1172/JCI13505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.He G, Zhang YW, Lee JH, Zeng SX, Wang YV, Luo Z, Dong XC, Viollet B, Wahl GM, Lu H. 2014. AMP-activated protein kinase induces p53 by phosphorylating MDMX and inhibiting its activity. Mol Cell Biol 34:148–157. doi: 10.1128/MCB.00670-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jones RG, Plas DR, Kubek S, Buzzai M, Mu J, Xu Y, Birnbaum MJ, Thompson CB. 2005. AMP-activated protein kinase induces a p53-dependent metabolic checkpoint. Mol Cell 18:283–293. doi: 10.1016/j.molcel.2005.03.027. [DOI] [PubMed] [Google Scholar]
- 51.Koivusalo R, Krausz E, Ruotsalainen P, Helenius H, Hietanen S. 2002. Chemoradiation of cervical cancer cells: targeting human papillomavirus E6 and p53 leads to either augmented or attenuated apoptosis depending on the platinum carrier ligand. Cancer Res 62:7364–7371. [PubMed] [Google Scholar]
- 52.Filippova M, Filippov V, Williams VM, Zhang K, Kokoza A, Bashkirova S, Duerksen-Hughes P. 2014. Cellular levels of oxidative stress affect the response of cervical cancer cells to chemotherapeutic agents. Biomed Res Int 2014:574659. doi: 10.1155/2014/574659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pectasides D, Kamposioras K, Papaxoinis G, Pectasides E. 2008. Chemotherapy for recurrent cervical cancer. Cancer Treat Rev 34:603–613. doi: 10.1016/j.ctrv.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 54.Xu Y, Baltimore D. 1996. Dual roles of ATM in the cellular response to radiation and in cell growth control. Genes Dev 10:2401–2410. doi: 10.1101/gad.10.19.2401. [DOI] [PubMed] [Google Scholar]
- 55.Chehab NH, Malikzay A, Appel M, Halazonetis TD. 2000. Chk2/hCds1 functions as a DNA damage checkpoint in G(1) by stabilizing p53. Genes Dev 14:278–288. [PMC free article] [PubMed] [Google Scholar]
- 56.Bykov VJN, Eriksson SE, Bianchi J, Wiman KG. 2018. Targeting mutant p53 for efficient cancer therapy. Nat Rev Cancer 18:89–102. doi: 10.1038/nrc.2017.109. [DOI] [PubMed] [Google Scholar]
- 57.Liu J, Zhang C, Zhao Y, Feng Z. 2017. MicroRNA control of p53. J Cell Biochem 118:7–14. doi: 10.1002/jcb.25609. [DOI] [PubMed] [Google Scholar]
- 58.Chen J, Marechal V, Levine AJ. 1993. Mapping of the p53 and mdm-2 interaction domains. Mol Cell Biol 13:4107–4114. doi: 10.1128/mcb.13.7.4107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Martinez-Zapien D, Ruiz FX, Poirson J, Mitschler A, Ramirez J, Forster A, Cousido-Siah A, Masson M, Vande Pol S, Podjarny A, Travé G, Zanier K. 2016. Structure of the E6/E6AP/p53 complex required for HPV-mediated degradation of p53. Nature 529:541–545. doi: 10.1038/nature16481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Riley KJ, Maher LJ III. 2007. p53 RNA interactions: new clues in an old mystery. RNA 13:1825–1833. doi: 10.1261/rna.673407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Harris SL, Levine AJ. 2005. The p53 pathway: positive and negative feedback loops. Oncogene 24:2899–2908. doi: 10.1038/sj.onc.1208615. [DOI] [PubMed] [Google Scholar]
- 62.Stewart-Ornstein J, Lahav G. 2017. p53 dynamics in response to DNA damage vary across cell lines and are shaped by efficiency of DNA repair and activity of the kinase ATM. Sci Signal 10:eaah6671. doi: 10.1126/scisignal.aah6671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhang X-P, Liu F, Cheng Z, Wang W. 2009. Cell fate decision mediated by p53 pulses. Proc Natl Acad Sci U S A 106:12245–12250. doi: 10.1073/pnas.0813088106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cheng T-H, Cohen SN. 2007. Human MDM2 isoforms translated differentially on constitutive versus p53-regulated transcripts have distinct functions in the p53/MDM2 and TSG101/MDM2 feedback control loops. Mol Cell Biol 27:111–119. doi: 10.1128/MCB.00235-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Freedman DA, Levine AJ. 1998. Nuclear export is required for degradation of endogenous p53 by MDM2 and human papillomavirus E6. Mol Cell Biol 18:7288–7293. doi: 10.1128/mcb.18.12.7288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Paek AL, Liu JC, Loewer A, Forrester WC, Lahav G. 2016. Cell-to-cell variation in p53 dynamics leads to fractional killing. Cell 165:631–642. doi: 10.1016/j.cell.2016.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Eichten A, Rud DS, Grace M, Piboonniyom SO, Zacny V, Munger K. 2004. Molecular pathways executing the “trophic sentinel” response in HPV-16 E7-expressing normal human diploid fibroblasts upon growth factor deprivation. Virology 319:81–93. doi: 10.1016/j.virol.2003.11.008. [DOI] [PubMed] [Google Scholar]
- 68.Blackford AN, Jackson SP. 2017. ATM, ATR, and DNA-PK: the trinity at the heart of the DNA damage response. Mol Cell 66:801–817. doi: 10.1016/j.molcel.2017.05.015. [DOI] [PubMed] [Google Scholar]
- 69.Duensing S, Munger K. 2002. The human papillomavirus type 16 E6 and E7 oncoproteins independently induce numerical and structural chromosome instability. Cancer Res 62:7075–7082. [PubMed] [Google Scholar]
- 70.Mehta K, Laimins L. 2018. Human papillomaviruses preferentially recruit DNA repair factors to viral genomes for rapid repair and amplification. mBio 9:e00064-18. doi: 10.1128/mBio.00064-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Khanal T, Leung Y-K, Jiang W, Timchenko N, Ho S-M, Kim K. 2019. NR2E3 is a key component in p53 activation by regulating a long noncoding RNA DINO in acute liver injuries. FASEB J 33:8335–8348. doi: 10.1096/fj.201801881RR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Thorn CF, Oshiro C, Marsh S, Hernandez-Boussard T, McLeod H, Klein TE, Altman RB. 2011. Doxorubicin pathways: pharmacodynamics and adverse effects. Pharmacogenet Genomics 21:440–446. doi: 10.1097/FPC.0b013e32833ffb56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jiao Y, Liu C, Cui FM, Xu JY, Tong J, Qi XF, Wang LL, Zhu W. 2015. Long intergenic non-coding RNA induced by X-ray irradiation regulates DNA damage response signaling in the human bronchial epithelial BEAS-2B cell line. Oncol Lett 9:169–176. doi: 10.3892/ol.2014.2622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hu WL, Jin L, Xu A, Wang YF, Thorne RF, Zhang XD, Wu M. 2018. GUARDIN is a p53-responsive long non-coding RNA that is essential for genomic stability. Nat Cell Biol 20:492–502. doi: 10.1038/s41556-018-0066-7. [DOI] [PubMed] [Google Scholar]
- 75.Zhao K, Wang X, Xue X, Li L, Hu Y. 2020. A long noncoding RNA sensitizes genotoxic treatment by attenuating ATM activation and homologous recombination repair in cancers. PLoS Biol 18:e3000666. doi: 10.1371/journal.pbio.3000666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Dianatpour A, Ghafouri-Fard S. 2017. The role of long non coding RNAs in the repair of DNA double strand breaks. Int J Mol Cell Med 6:1–12. [PMC free article] [PubMed] [Google Scholar]
- 77.Suzuki K, Bose P, Leong-Quong RY, Fujita DJ, Riabowol K. 2010. REAP: a two minute cell fractionation method. BMC Res Notes 3:294. doi: 10.1186/1756-0500-3-294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Park DE, Cheng J, Berrios C, Montero J, Cortes-Cros M, Ferretti S, Arora R, Tillgren ML, Gokhale PC, DeCaprio JA. 2019. Dual inhibition of MDM2 and MDM4 in virus-positive Merkel cell carcinoma enhances the p53 response. Proc Natl Acad Sci U S A 116:1027–1032. doi: 10.1073/pnas.1818798116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Martinez LA, Naguibneva I, Lehrmann H, Vervisch A, Tchénio T, Lozano G, Harel-Bellan A. 2002. Synthetic small inhibiting RNAs: efficient tools to inactivate oncogenic mutations and restore p53 pathways. Proc Natl Acad Sci U S A 99:14849–14854. doi: 10.1073/pnas.222406899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sharma S, Munger K. 2018. Expression of the cervical carcinoma expressed PCNA regulatory (CCEPR) long noncoding RNA is driven by the human papillomavirus E6 protein and modulates cell proliferation independent of PCNA. Virology 518:8–13. doi: 10.1016/j.virol.2018.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]