Abstract
Urbanisation will be one of the defining demographic trends of the 21st century—creating unique opportunities for sustainable capacity development, as well as substantial risks and challenges for managing public health and health emergencies. Plans and policies for responding to public health emergencies are generally framed at higher levels of governance, but developing, improving and sustaining the capacities necessary for implementing these policies is a direct function of local-level authorities. Evaluating local-level public health capacities is an important process for identifying strengths and weaknesses that can impact the preparedness for, detection of and response to health security threats. However, while various evaluations and assessments exist for evaluating capacities at other levels, currently, there are no readily available health security assessments for the local-level. In this paper, we describe a tool—the Rapid Urban Health Security Assessment (RUHSA) Tool—that is based on a variety of other relevant assessments and guidance documents. Assessing capacities allow for local-level authorities to identify the strengths and weaknesses of their local health security systems, create multiyear action plans and prioritise opportunities for improving capacities, effectively engage with development partners to target resources effectively and develop compelling narratives and a legacy of leadership. While the RUHSA Tool was not designed to be used in the midst of a public health emergency, such as the ongoing COVID-19 pandemic, it may also be adapted to inform a checklist for prioritising what capacities and activities a city needs to rapidly develop or to help focus requests for assistance.
Keywords: health policy, health systems, public health
Summary box.
Local authorities are often responsible for responding to health security threats, yet most plans and policies are framed at higher levels of governance.
There are a variety of national-level evaluations and local guidance documents, but a notable absence of local-level assessment tools.
To address this gap, we present here an assessment tool for rapidly evaluating local-level health security capacities.
The tool has potential applications for immediately informing outbreak response efforts, as well as informing long-term capacity development initiatives.
Introduction
Urbanisation is a complex socioeconomic process that refers to an increase in the movement and settling of people in urban environments.1 Catalysed by the Industrial Revolution in the 19th century, this process continues to drive demographic changes today. Between 1950 and 2018, the world’s urban population grew from an estimated 0.8 billion (30% of the world’s population) to an estimated 4.2 billion (55% of the world’s population).2 This development is significant because it marks the first time in human history that a majority of people have resided in cities.3 Furthermore, estimates suggest that this trend will continue and by 2050, the world’s urban population will total approximately 6.9 billion people (69% of the world’s population).2
As the world continues to urbanise, urbanisation should be viewed as a transformative force with the potential for addressing global challenges and a more sustainable development trajectory.4 5 Among these challenges are public health preparedness and health security.6 The rise of cities and increasing population density create unique risks and challenges for managing public health and emergencies.7 8 Cities have the potential to act as incubators for infectious disease outbreaks, where all the necessary conditions for epidemics are met.7 Dense urban populations can provide conditions that promote disease emergence and transmission which can compound the prevention and control of infectious diseases.7–9 Additionally, in our highly globalised world, cities often act as hubs for the transportation of people and goods. The presence of airports, seaports and train stations in cities creates networks that facilitate the mass movements of people and goods, but also infectious diseases.5 10–12 This can render cities a rate-enhancing or rate-limiting factor for infectious disease transmission.5
These realities have been demonstrated repeatedly in high-profile infectious disease outbreaks in the 21st century. Severe acute respiratory syndrome (SARS) first emerged in 2002 in China, before spreading internationally through global cities including Hong Kong, Singapore and Toronto.13 The swift spread of the 2009 H1N1 pandemic was facilitated by cities and highlighted several notable challenges including response coordination, disease surveillance, containment and mitigation strategies, the delivery of countermeasures and public communication.14 Presently, the rapid, global spread of a novel coronavirus once again highlights the unique role that cities play in the epidemiology of infectious disease outbreaks and serves to remind us that cities are at the front line of such events. In late December of 2019, a cluster of pneumonia cases of unknown aetiology was reported in the city of Wuhan—a megacity of over 11 million people. The outbreak was quickly attributed to a coronavirus (SARS-CoV-2) that caused a novel coronavirus disease in humans, COVID-19. Since that time, fuelled by global travel between cities, SARS-CoV-2 has spread through China and around the world, escalating into a pandemic,15 resulting in the declaration of a Public Health Emergency of International Concern by the WHO,16 the implementation of drastic public health interventions in urban areas,17–22 and severe societal and economic disruptions. By April, the virus had spread to over 200 countries and territories on every continent except Antarctica, and had resulted in over 750 800 laboratory confirmed cases and 36 400 deaths globally.23
Although plans and policies for responding to infectious disease outbreaks are often framed at higher levels of governance, cities and municipal authorities are often the first to respond to public health emergencies. Developing, improving and sustaining capacities necessary for the detection and control of infectious disease outbreaks are the direct functions of cities.5 24 Both for the ongoing outbreak response as well as for future planning, it is critical to systematically assess local-level public health preparedness.25 This process provides a means of identifying the strengths and weaknesses that impact the preparedness for, detection of and response to health security threats.
Herein, we present a methodology for supporting cities in responding to infectious disease threats. The rest of the paper is organised as follows: the second section introduces the Rapid Urban Health Security Assessment (RUHSA) Tool and details its salient features; the third section provides a brief overview of how the RUHSA Tool was developed; and the fourth section describes the potential impacts and benefits of completing an assessment using the RUHSA Tool.
The Rapid Urban Health Security Assessment Tool
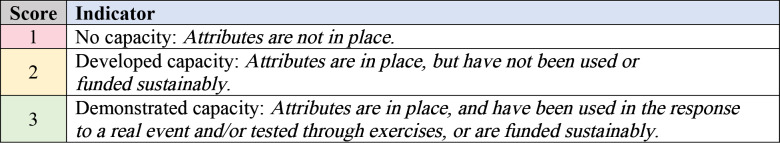
The RUHSA Tool is intended to evaluate local-level capacities necessary for preventing, detecting and responding to public health threats. The tool contains 20 core capacities and 46 indicators (figure 1). Structured similarly to the International Health Regulations (2005) Joint External Evaluation Tool,26 the capacities of the RUHSA Tool are categorised as relating to preventing, detecting or responding to outbreaks, or others related to public health emergencies. These categories are justified as capacities that prevent or reduce the likelihood of emergencies are inherently necessary for reducing risk; the early detection of emergencies can dramatically reduce the negative health, social and economic consequences of public health emergencies; and developed capacities for responding to public health emergencies are necessary for efficiently addressing threats and mitigating negative outcomes. The RUHSA tool also contains several other capacities that warrant consideration for ensuring local-level preparedness and health security.
Figure 1.
The capacities and indicators contained in the RUHSA Tool. RUHSA, Rapid Urban Health Security Assessment.
The tool contains five capacities for preventing public health emergencies, four capacities for detecting public health emergencies, eight capacities for responding to public health emergencies and three capacities relating to other considerations. Defined indicators are used to assess these capacities (figure 1).
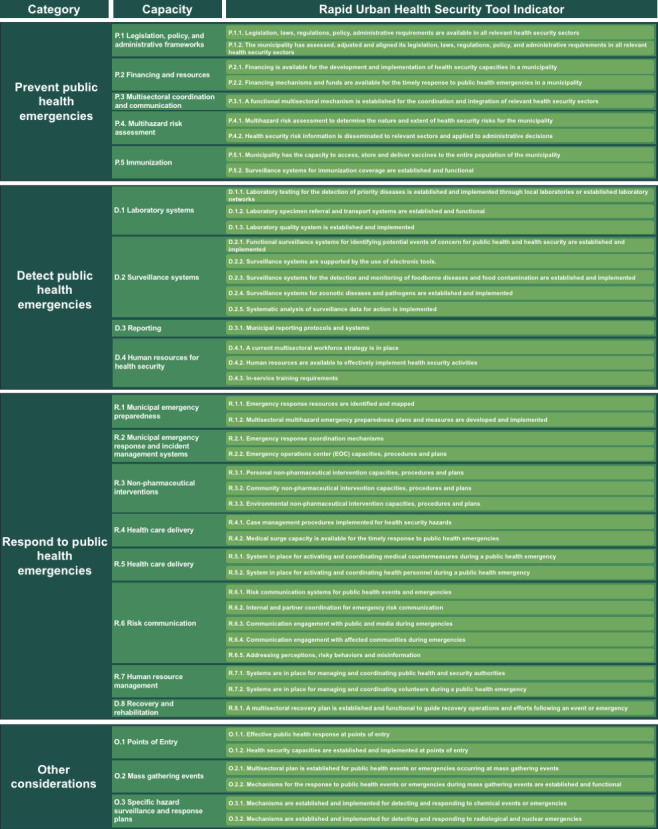
Every indicator included in the RUHSA has attributes that reflect various levels of capacity development. The indicators are scored on a three-point, colour-coated Likert scale based on the response to four to five technical questions. The technical questions are directly related to the indicators and related attributes, which enable users to systematically and reliably measure municipal capacities. Each assessment indicator is considered separately and receives a single score based on the current capacity of a municipality (figure 2).
Figure 2.
An overview of the scoring system used in the RUHSA Tool. RUHSA, Rapid Urban Health Security Assessment.
The RUHSA Tool also contains contextual questions related to each capacity. These questions do not inform the indicator scores but are questions relating to broader contexts or circumstances that could inform responses to the technical questions.
The RUHSA Tool can be accessed publicly online at the Georgetown University Center for Global Health Science & Security’s website.27
Development of the tool
We developed the RUHSA Tool by reviewing and mapping core capacities, indicators and metrics listed in a variety of relevant guidance documents. We conducted a review of emergency and health security guidance and assessments to identify guidance documents that warranted consideration for mapping. To be included, guidance was required to either focus on health security or local-level emergency preparedness and clearly define metrics or benchmarks. The list of included documents consists of the first and second editions of the International Health Regulations (2005) Joint External Evaluation Tool,26 28 the WHO Health Security Benchmarks,29 the WHO’s Chemical, Biological, Radiological and Nuclear capabilities checklist, the United Nations Office for Disaster Risk Reduction's Resilience Handbook for Local Government Leaders,30 United States Centers for Disease Control and Prevention Standards for State, Local, Tribal, and Territorial Public Health Emergency Preparedness and Response Capabilities31 and the Robert Wood Johnson Foundation's Health Security Preparedness Index.32
These documents were then reviewed and mapped to generate a list of health security capacities. Capacities that appeared in two or more guidance documents were flagged as core capacities that warranted consideration for inclusion. Based on this list, we then drafted a multidisciplinary framework for urban public health preparedness and developed indicators for assessing urban capacities.
We presented this framework at the 2019 Annual Summit of the Global Parliament of Mayors, held in Durban, South Africa in November 2019 and solicited feedback from attendees. The Global Parliament of Mayors includes mayors from a wide variety of countries including Afghanistan, Argentina, Belgium, Cameroon, France, the Gambia, Germany, Italy, Jordan, Kosovo, Liberia, Mozambique, Nepal, the Netherlands, Norway, Pakistan, Palestine, Poland, Portugal, Senegal, Sierra Leone, South Africa, Switzerland, Uganda, the United Kingdom and the USA. Summit participants included over 100 attendees, from the countries listed above, in addition to several other countries, including Albania, China, the Democratic Republic of the Congo, Ghana, India, Jamaica, Somalia and Zimbabwe.
We requested comments from participants on the framework and recorded feedback provided by the mayors. The feedback we received included adding considerations and capacities, combining capacities and removing certain capacities that the mayors felt were not relevant to their contexts. We reviewed these recommendations and discussed whether the suggestions had both practical application and global validity before incorporating these suggestions to modify and refine the framework and included indicators. On completion, we sent the tool back to the Global Parliament of Mayors who approved the resulting tool.
Potential applications, benefits and impacts
The RUHSA Tool will allow for municipal leaders (eg, mayors, municipal offices, other agencies), national leaders, researchers and other experts to identify the strengths and weaknesses of their local-level health security systems. Urban health authorities are developing strategies to meet the need for local-level data to inform decision-making for improving public health evidence-based policies,33 but assessments of infectious disease risk and related debates over resource prioritisation have been limited by the absence of robust and reliable data.25 The data that result from the RUHSA Tool will address these critical needs and help inform resulting strategies.
Most significantly, these efforts can inform the response to infectious disease outbreaks. As we have seen in the ongoing response to COVID-19, municipal leaders are making decisions in the absence of specific guidance from national governments and without a complete understanding of what capacities are required for protecting their jurisdictions. Accordingly, this tool could be used to quickly provide a solid foundation, based on validated sources and guidance for conceptualising the urgent tasks at hand and realising the gaps in local-level health security.
In addition to assessing immediate capacity for responding to disease threats, the RUHSA Tool can be used by municipal authorities to create multiyear action plans and better prioritise opportunities for improving local health security. Developing public health systems and capacities requires adequate financial resources and investment. However, countries often struggle to build capacities, in part because resource-constrained governments faced multiple competing priorities, and in part because financial resources were not readily available to provide desperately needed assistance in building public health infrastructure.34 35 These realities and cycles of panic and neglect are felt even more acutely at subnational levels. Over recent decades, many countries have relegated a growing list of responsibilities to local governments, often without devolving the resources necessary to finance them.36 This has resulted in a situation in which financial resources can be exceedingly scarce for developing these critical capacities.
For local government leaders, reducing disaster risk—including that posed by health security threats—can represent a compelling legacy opportunity.30 Mayors and other municipal leaders who complete evaluations using the RUHSA Tool over time will produce empirical data to support narratives and descriptions of the impacts their leadership had on society. In turn, this will afford them opportunities to strengthen trust in and the legitimacy of local political authorities, structures and systems.
Additionally, the RUHSA Tool can be used to promote accountability and transparency, which are key principles of effective planning for risk reduction.30 Ideally, cities will make the results of their assessments public to allow for transparency, so city residents can be fully informed and hold their local governments accountable for improving local public health preparedness and act as advocates when discussing the importance of preparedness with others. Better understanding the strengths and limitations of their own municipal capacities will also allow city leaders to engage with current and prospective development partners to advocate for additional resources and to target those resources effectively.
Conclusion
It is our hope that the RUHSA Tool will prove to be a valuable resource for municipal authorities as they grapple with developing effective, contextually appropriate responses to the COVID-19 pandemic. We also believe that the tool will have immense value following the pandemic, when efforts must be taken to ensure that cities around the world are better prepared for the next infectious disease outbreak. This assessment tool, one that has the potential to address a notable absence of data relating to local-level health security capacity, represents an important first step for those efforts.
Acknowledgments
We sincerely thank the mayors of the Global Parliament of Mayors for their valuable feedback and comments that supported the development and refining of this tool.
Footnotes
Handling editor: Seye Abimbola
Twitter: @mattrbo, @rebeccakatz5
Author Contributorship: RK conducted preliminary research that formed the basis for development of the tool. MRB and RK conceptualised the tool. MRB conducted the review and mapping of other tools and drafted the initial tool. Both MRB and RK contributed to revising the tool based on feedback received. MRB drafted the manuscript. Both MRB and RK contributed to editing the manuscript and have approved the final version submitted for publication.
Funding: These efforts were supported by the Open Philanthropy Project.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All relevant data are included in the article.
References
- 1.Phillips DR. Urbanization and human health. Parasitology 1993;106 Suppl:S93–107. 10.1017/S0031182000086145 [DOI] [PubMed] [Google Scholar]
- 2.United Nations, Department of Economic and Social Affairs, Population Division . World urbanization prospects: the 2018 revision. New York: United Nations, 2019. [Google Scholar]
- 3.World Health Organization Hidden cities: unmasking and overcoming health inequities in urban settings. Geneva: World Health Organization, 2010. [Google Scholar]
- 4.United Nations Human Settlements Programme World cities report 2016. Nairobi: UN Human Settlements Programme, 2016. [Google Scholar]
- 5.Ezzati M, Webster CJ, Doyle YG, et al. Cities for global health. BMJ 2018;363:k3794. 10.1136/bmj.k3794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee VJ, Ho M, Kai CW, et al. Epidemic preparedness in urban settings: new challenges and opportunities. Lancet Infect Dis 2020;20:527–9. 10.1016/S1473-3099(20)30249-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alirol E, Getaz L, Stoll B, et al. Urbanisation and infectious diseases in a globalised world. Lancet Infect Dis 2011;11:131–41. 10.1016/S1473-3099(10)70223-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Neiderud C-J. How urbanization affects the epidemiology of emerging infectious diseases. Infect Ecol Epidemiol 2015;5:27060. 10.3402/iee.v5.27060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morse SS, Mazet JAK, Woolhouse M, et al. Prediction and prevention of the next pandemic zoonosis. Lancet 2012;380:1956–65. 10.1016/S0140-6736(12)61684-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dalziel BD, Pourbohloul B, Ellner SP. Human mobility patterns predict divergent epidemic dynamics among cities. Proc Biol Sci 2013;280:20130763. 10.1098/rspb.2013.0763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gonçalves B, Balcan D, Vespignani A. Human mobility and the worldwide impact of intentional localized highly pathogenic virus release. Sci Rep 2013;3:810. 10.1038/srep00810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kissler SM, Gog JR, Viboud C, et al. Geographic transmission hubs of the 2009 influenza pandemic in the United States. Epidemics 2019;26:86–94. 10.1016/j.epidem.2018.10.002 [DOI] [PubMed] [Google Scholar]
- 13.Cherry JD. The chronology of the 2002-2003 SARS mini pandemic. Paediatr Respir Rev 2004;5:262–9. 10.1016/j.prrv.2004.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bell DM, Weisfuse IB, Hernandez-Avila M, et al. Pandemic influenza as 21st century urban public health crisis. Emerg Infect Dis 2009;15:1963–9. 10.3201/eid1512.091232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ghebreyesus TA. WHO Director-General's opening remarks at the media briefing on COVID-19. World Health Organization [speech], 2020. Available: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11-march-2020 [Accessed 5 Apr 2020].
- 16.World Health Organization Novel Coronavirus (2019-nCoV) Situation Report-11. World Health Organization [report], 2020. Available: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200131-sitrep-11-ncov.pdf?sfvrsn=de7c0f7_4 [Accessed 5 Apr 2020].
- 17.Wu JT, Leung K, Leung GM. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet 2020;395:689–97. 10.1016/S0140-6736(20)30260-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Du Z, Wang L, Cauchemez S, et al. Risk for transportation of coronavirus disease from Wuhan to other cities in China. Emerg Infect Dis 2020;26:1049–52. 10.3201/eid2605.200146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med 2020;27:taaa020. 10.1093/jtm/taaa020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spina S, Marrazzo F, Migliari M, et al. The response of Milan's emergency medical system to the COVID-19 outbreak in Italy. Lancet 2020;395:e49–50. 10.1016/S0140-6736(20)30493-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Order of the commissioner of health of the city of Chicago, no. 2020-1: shelter in place for COVID-19 illness, City of Chicago 2020.
- 22.Public order under city of Los Angeles emergency authority: safer at home. city of Los Angeles 2020.
- 23.World Health Organization Coronavirus disease 2019 (COVID-19) Situation Report-71. World Health Organization [report], 2020. Available: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200331-sitrep-71-covid-19.pdf?sfvrsn=4360e92b_8 [Accessed 5 Apr 2020].
- 24.Katz R, Mookherji S, Kaminski M, et al. Urban governance of disease. Administrative Sciences 2012;2:135–47. 10.3390/admsci2020135 [DOI] [Google Scholar]
- 25.Oppenheim B, Gallivan M, Madhav NK, et al. Assessing global preparedness for the next pandemic: development and application of an epidemic preparedness index. BMJ Glob Health 2019;4:e001157. 10.1136/bmjgh-2018-001157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.World Health Organization International health regulations (2005) joint external evaluation tool, 1st EDS. Geneva: World Health Organization, 2016. [Google Scholar]
- 27.Georgetown University Center for Global Health Science & Security Rapid Urban Health Security Assessment (RUHSA) Tool. GUCGHSS [website]. Available: https://ghss.georgetown.edu/urbanprep/ [Accessed 5 Apr 2020].
- 28.World Health Organization International health regulations (2005) joint external evaluation tool. 2nd eds Geneva: World Health Organization, 2018. [Google Scholar]
- 29.World Health Organization Benchmarks for international health regulations (IHR) capacities. Geneva: World Health Organization, 2019. [Google Scholar]
- 30.United Nations Office for Disaster Risk Reduction How to make cities more resilient: a Handbook for local government leaders. Geneva: UNDRR, 2012. [Google Scholar]
- 31.US Centers for Disease Control and Prevention Public health emergency preparedness and response capabilities: national standards for state, local, tribal, and territorial public health. Atlanta: US CDC, 2019. [Google Scholar]
- 32.Robert Wood Johnson Foundation The National Health Security Preparedness Index. RWJF [website]. Available: https://nhspi.org/ [Accessed 5 Apr 2020].
- 33.Castrucci BC, Rhoades EK, Leider JP, et al. What gets measured gets done: an assessment of local data uses and needs in large urban health departments. J Public Health Manag Pract 2015;21 Suppl 1:38–48. 10.1097/PHH.0000000000000169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sands P, Chawla M. Financing preparedness at a national level. Lancet 2017;389:2086–7. 10.1016/S0140-6736(17)31375-2 [DOI] [PubMed] [Google Scholar]
- 35.Katz R, Graeden E, Eaneff S, et al. Strengthening health security: an intuitive and user-friendly tool to estimate country-level costs. BMJ Glob Health 2018;3:e000864. 10.1136/bmjgh-2018-000864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Farvacque-Vitkovic C, Kopanyi M, Cities B. Better world: a Handbook on local governments Self-Assessments. Washington, DC: World Bank Group, 2019. [Google Scholar]