Abstract
Introduction
This study aims to establish the Knowledge, Attitudes and Practices (KAP) of the general population (people with and without diabetes) towards diabetes. The study will examine (a) recognition and understanding of causes, prevention and treatment strategies of diabetes; (b) identify the knowledge gaps and behavioural patterns that may hamper diabetes prevention and control; (c) stigma towards and stigma perceived by people with diabetes and (d) awareness of anti-diabetes campaigns.
Methods and analysis
The study is a nationwide, cross-sectional study of Singapore’s general population aged 18 years and above (n=3000), comprising Chinese, Malay, Indian and other ethnic groups, who can understand English, Chinese, Malay or Tamil language. The sample was derived using a disproportionate stratified sampling using age and ethnicity. The proportion of respondents in each ethnic group (Chinese, Malay and Indian) was set to approximately 30%, while the proportion of respondents in each age group was set around 20% in order to ensure a sufficient sample size. The respondents will be administered questionnaires on diabetes KAP, stigma towards diabetes, lifestyle, diet and awareness of local anti-diabetes campaigns. The analysis will include descriptive statistics and multiple logistic and linear regression analyses to determine the socio-demographic correlates of correct recognition of diabetes, help-seeking preferences, as well as overall knowledge and attitudes among those with and without diabetes. We will consider a p value ≤0.05 as significant.
Ethics and dissemination
This study protocol has been reviewed by the Institutional Research Review Committee and the National Healthcare Group Domain Specific Review Board (NHG DSRB Ref 2018/00430). The results of the study will be shared with policymakers and other stakeholders. There will be a local mass media briefing to disseminate the findings online, in print and on television and radio. The results will be published in peer-reviewed journals and presented in scientific meetings.
Keywords: diabetes & endocrinology, epidemiology, public health
Strengths and limitations of this study.
This is the largest nationwide survey conducted to date to track the Knowledge, Attitudes and Practices (KAP) pertaining to diabetes.
The protocol includes strict quality controls to ensure the accuracy and integrity of the data.
Multiple methodological considerations such as disproportionate stratified sampling, cognitive testing of survey questionnaire and recruitment of supplementary groups have been adopted to improve the quality of the study.
The limitation of this household survey is that it excludes people who are institutionalised (hospitalised, long-term care, imprisoned, and so on) during the entire field period of the survey.
Background
Diabetes mellitus (DM) is one of the most prevalent metabolic diseases in the world. The prevalence of diabetes worldwide among adults over 18 years has doubled from 4.7% (equivalent to 108 million) in 1980 to 8.5% (equivalent to 422 million) in 20141 and is projected to increase to 693 million in 2045.2 The social and financial implications due to this disease are complex and include higher rates of mortality, morbidity and economic costs. In 2017, 5 million deaths worldwide were attributable to diabetes or diabetes-related complications among people aged 20 to 99 years.2 Significant complications of diabetes include microvascular (neuropathy, nephropathy, retinopathy), macrovascular (cardiovascular, cerebrovascular, peripheral vascular diseases) and miscellaneous complications (cardiomyopathy, metabolic crisis, and so on).3 Diabetes and the complications arising from it not only affect the individuals and their family but also impact the healthcare system and the national economy, due to the higher medical costs and loss of productivity resulting from the condition. The cost of diabetes treatment was estimated to be US$727 billion for people aged 20 to 79 years old in 2017 and is predicted to increase to US$776 billion in 2045 globally.2
Singapore is a highly developed country in Southeast Asia, with a competitive economy ranked number one in the world.4 It has a multi-ethnic population comprising mainly Chinese, Malays and Indians. Despite its efficient healthcare system,5 it has a higher prevalence of diabetes compared with the global prevalence rate, with one in nine Singaporeans (11.3%) suffering from the disease.6 Diabetes was the seventh leading cause of disability-adjusted life years in Singapore in 2017.7 In 2010, the total economic costs of diabetes per working-age patient in Singapore was estimated to be US$5646, of which 42% were excess direct medical costs and 58% were indirect productivity-related losses.8 Thus, diabetes is a significant public health concern in Singapore. The Ministry of Health, Singapore, declared a ‘War on Diabetes’ campaign in 2016 to mobilise citizens to promote (1) healthy lifestyles to prevent diabetes, (2) early detection and intervention to reduce the complications associated with diabetes and (3) effective management of diabetes. The Ministry of Health, Singapore, recruited a citizen’s jury of 76 volunteers belonging to diverse backgrounds, comprising those living with/without diabetes, caregivers and healthcare providers who came up with recommendations to (a) improve awareness of diabetes through education, (b) promote healthy living through exercise, healthy diet, etc. (c) strengthen peer/community support initiatives, (d) enhance the skills of healthcare providers and (e) improve funding for medical costs. The ‘War on Diabetes’ was further strengthened recently with recommendations to ban advertisements for drinks with very high sugar content along with recommendations to colour code the beverages to indicate the sugar content.9
KAP studies collect information on what is known, believed and done in relation to a particular topic in a specific community. Understanding the levels of knowledge, personal attitudes and practices can enable a more efficient process of awareness creation by identifying specific gaps, which allows tailoring of programmes to the needs of the community.10 KAP surveys thus reveal misconceptions among the population and diabetics that may pose obstacles to the activities that agencies would like to implement, as well as potential barriers to behaviour change. Previous studies have shown the usage of such KAP surveys in determining the need for tailored preventive and educational initiatives.11 12
There are three main types of diabetes (type 1 (T1DM), type 2 (T2DM) and gestational diabetes), however T1DM forms a very small proportion (5% to 10%) of the total diabetes cases and gestational diabetes occurs transiently. Moreover, T2DM is more amenable to prevention through lifestyle and dietary changes, therefore, the current study mainly targets T2DM in Singapore. For the purposes of this study, diabetes thus refers to T2DM.
The current study aims to:
Conduct a nationwide survey to examine the KAP pertaining to the prevention and early detection of diabetes among Singapore’s general population.
Examine the differences in lifestyle and preventive health behaviours of Singapore residents (Singapore citizens and permanent residents (PR)) with and without diabetes as well as to explore specific treatment-related behaviours of those diagnosed with diabetes.
Identify the knowledge gaps and behavioural patterns that may hamper diabetes prevention, and control in Singapore’s resident population.
Identify socio-demographic correlates of diabetes KAP.
Examine diabetes-related stigma from the perspective of those with diabetes (self-stigma) and those without diabetes (public stigma).
Explore lifestyle factors and elucidate facilitators and barriers to the adoption of a healthy lifestyle in the population.
Understand the awareness of the population towards anti-diabetes campaigns.
Methods
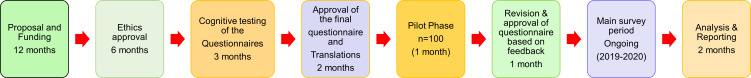
This cross-sectional study will be conducted among 3000 respondents who will be randomly selected across the country. A flow chart of the study processes is presented in figure 1. The study is currently in the data collection phase with fieldwork actively ongoing. All the study related activities were initiated after obtaining the relevant approval from the Institute of Mental Health’s Institutional Research Review Committee as well as the Ethics Committee of National Healthcare Group Domain Specific Review Board (NHG DSRB Ref 2018/00430). Only persons who are capable of providing written informed consent will be included in the study. Parental consent will be sought for those who are 18 to 20 years of age as the official age of adulthood in Singapore is 21 years and above. As this survey assesses the knowledge, including the subject’s ability to recognise the symptoms of diabetes, the study will not be introduced as a KAP study of diabetes in the consent form or in any other information material given to the respondent before answering the specific knowledge related questions. Instead, the term ‘chronic physical condition’ will be used to introduce this study. The actual disease of interest will be revealed only after the diabetes recognition questionnaire is administered to them. The purpose of this ‘blinding’ will be explained to the subjects during the consent phase with the assurance to unblind them later during the study. The survey (data collection) was launched in February 2019 and is expected to conclude by December 2020.
Figure 1.
Flow chart of the KAP study. KAP, Knowledge, Attitudes and Practices.
Patient and public involvement
Patients and members of the public were involved in the development of the research questions and the outcome measures. Prior to the commencement of the survey, the questionnaires were cognitively tested among members of the general public and the diabetes patients to improve the quality of the questionnaire and to adapt it to the local population. This step helped to identify questions, words or phrases that were difficult to understand or unacceptable to them. Participants were asked to provide feedback on the mode of administration of the questionnaires and suggest domains/questions that may be important to assess the KAP but had been missed out by the researchers. Patients with diabetes were explicitly asked about the acceptability and relevance of the stigma related questions and social constraints scale. There was no patient/public involvement in the recruitment and conduct of the study. The results of the study will be shared with the public through media releases, public sharing sessions and open access publications.
Study design
This nationwide, cross-sectional study includes Singapore citizens and PRs aged 18 years and above, comprising Chinese, Malay, Indian and Other ethnic groups, who can understand English, Chinese, Malay or Tamil. The inclusion and exclusion criteria are included in table 1.
Table 1.
Inclusion and exclusion criteria
| Inclusion criteria | Exclusion criteria |
| Singapore citizens and PRs residing in Singapore | Non-Singapore citizens and non-PRs |
| Age ≥18 years | |
| Ethnicity: Chinese, Malay, Indian and Other ethnic groups | Incapable of doing the interview |
| Can speak English, Mandarin, Malay or Tamil | Living out of the country throughout the field period |
| Long-term hospitalisation or institutionalisation throughout the field period |
PRs, permanent residents.
Study population, recruitment strategy and training of interviewers
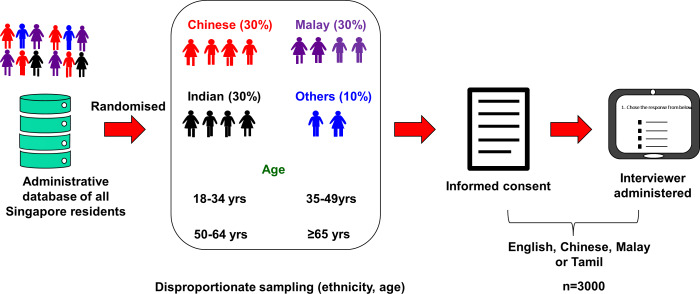
Sample size calculations, sampling and sample release
The sample size estimates for the general population sample were produced by running statistical power calculations for binary proportions to determine what sample sizes are necessary overall, as well as for subgroups, to produce a precise estimate with a margin of error less than or equal to 0.05. It was assumed that a statistical power of 0.80 was required, while the Type 1 error rate is controlled at α=0.05, as is standard. Power calculations were generated based on prevalence rates of general knowledge on diabetes and its risk factors. Data from the study by Wee et al,13 revealed that, on average, about 60% of respondents interviewed had correct responses to the questions related to the general knowledge on diabetes and its risk factors. The sample size was adjusted to account for deviations from simple random sampling. These deviations are known as the design effect (DEFF). The estimated DEFF after over-sampling on age and race was 2.029. In this study, the sample was derived using a disproportionate stratified sampling design. Sampling was done based on a total of 12 strata: a combination of 3 strata for ethnicities (Chinese, Malay and Indian) and 4 strata for age (18 to 34 years, 35 to 49 years, 50 to 64 years and 65 years and above) were employed. The proportion of respondents in each ethnic group (Chinese, Malay and Indian) was set to approximately 30% while the proportion of respondents in each age group was set around 20% in order to ensure that sufficient sample size for these population subgroups could be achieved to improve the reliability of our estimates. We have incorporated all DEFF values in the calculation. In our calculation, realistic sample sizes were assumed (eg, n=2500 and n=3000) and then the margin of error was computed. A target sample size of 3000 was estimated to be adequate to determine the general knowledge of diabetes in the population. The margin of error for the overall prevalence estimate was 2.5%, while the margin of error for the subgroups defined by age and ethnic groups was between 4.5% and 5%. Note that as the margin of error (or precision) of a binary proportion depends on the estimate, we also computed the relative SE (RSE), which is acceptable if <30%. It was noted that RSE was excellent for an overall estimate (2.1%) and for subgroups (age and ethnicity group) estimates which ranged between 3.9% and 4.21%.
The sample was drawn from a national administrative database of all residents in Singapore which served as a sampling frame. A total sample of 10 000 individuals was drawn, which will be released during the active survey period (1 to 1.5 years) in 5 to 10 replicates while closely monitoring the recruitment to ensure a good response rate and inclusion of hard-to-reach population. We intend to achieve a response rate of 65% to 70% and a final recruitment target of 3000 respondents. The size and number of the replicates will be estimated based on the finalisation and response rates of the previous releases. Finalisation rates will be calculated based on the ineligible cases and refusals. We foresee approximately 15% to 20% ineligible cases and 10% to 15% refusals, based on our previous national surveys.14 15 An overview of the sampling strategy and processes are shown in figure 2.
Figure 2.
Sampling and procedure: The sample was drawn from a national administrative database of all residents in Singapore which served as a sampling frame. Household surveys are being conducted among those who provide written informed consent.
Recruitment strategy and interviewer training
The fieldwork for the survey will be conducted by a survey firm that was selected following the institutional guidelines. All the interviewers (30 to 40 interviewers) involved in the fieldwork are aged more than 21 years and experienced in door-to-door surveys. All field interviewers undergo training over 2 weeks on the study methodology and fieldwork which included lectures and hands-on sessions on ethics, techniques on approaching a household, initial self-introduction/communication with the respondent, consent taking, questionnaire administration, maintaining visitation records and other administrative tasks. All the interviewers underwent an evaluation and those who did not pass the requirements set by the study team were not allowed to conduct the survey. The training was conducted in English followed by language-specific training for interviewers who are conversant in one of the three local languages—Chinese, Malay and Tamil. The field supervisors and/or members from the research team will accompany the interviewers during the initial weeks to identify and resolve any problems during the survey. The interviews will be administered via a computer-assisted personal interview which allows real-time data collection. This method is an effective method for data collection and has been used in our previous national surveys.14 This innovative application is available in dual language—English, together with Chinese, Malay or Tamil. The dual-language interface aids standardisation across languages and allows interviewers to rephrase hard-to-understand questions easily. The real-time data capture protects confidential content against loss and theft, and data are available for analysis instantaneously.
The selected respondents will receive an invitation letter 1 to 2 weeks before the actual household visit by trained interviewers. The invitation letters include the details of the study, contact numbers they could use to get more information about the survey, provide feedback or register their refusal for the survey. A maximum of 10 visits will be made per household on different days and times before finalising the case. For cases where the respondent is not at home during the visit, ‘while you were out’ cards will be dropped in the letterbox or at their doorstep to allow the respondent to contact the survey firm. On completion of the survey, the participants will be given a SGD40 inconvenience fee in cash.
Quality assurance
Quality control is ensured at different phases of the study starting from the interviewer selection and training, where interviewers are selected only if they have at least secondary level education, are proficient in one of the main local languages, have basic computer skills and have prior experience in door-to-door surveys. The training for the interviewers is intense and the evaluation involves a simulation of the entire survey setting using a lay respondent, starting from the first contact with the respondent until the final administration procedures after payment of the inconvenience fee. Only those interviewers who pass this evaluation will be allowed to conduct the survey. The initial visits and the interviews will be done in the presence of the trained team member or field supervisors. The details of the quality assurance procedures that are followed in all our surveys are reported elsewhere.15
A trained team will constantly monitor the progress of replicates, ageing cases and visitation records to monitor the trends and highlight the discrepancies to the team for clarification and resolution. Around 10% of the interviews per interviewer will be selected for routine quality checks (QC) which involve verification of the survey and responses for the selected questions over the phone, on-site during the interview or by visiting the respondent’s house. Apart from the QC, regular monitoring will be conducted to verify that the consent process, visitation records and payment of inconvenience fees follow approved procedures. Quality will be assured at the data processing stages through logic checks that are in place for data verification. Trained staff will closely monitor the data influx to identify and highlight any errors occurring in this phase.
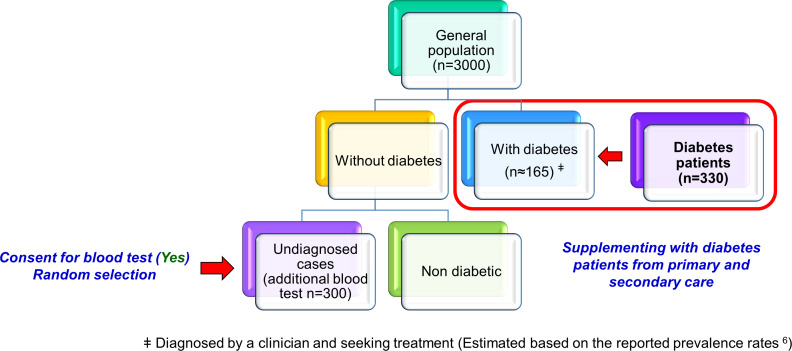
Supplementing the general population sample with patients with diabetes
Although previous studies have shown that the prevalence of diabetes in Singapore is 11%, many were not diagnosed.6 It is therefore expected that only a limited number of respondents (approximately n=165) diagnosed with diabetes will be recruited from the general population, which would, therefore, reduce the power to detect differences between those with and without diabetes in the general population. Hence, we will be supplementing this group with patients already diagnosed with diabetes who are seeking care from either primary care or specialist care settings with 1:2 allocation ratios. We will recruit approximately 330 (330=2×165) additional patients already diagnosed with diabetes, who will be matched to those with diabetes in the general population by age group, gender and ethnicity. Both the populations, that is, those with and without diabetes will be administered a similar set of questionnaires with some key differences. The subjects in the general population who indicate that they are not seeking treatment for their diabetes will not be included in the diabetes group. Depending on the numbers, we will consider a separate analysis for this group.
The study population is represented in figure 3.
Figure 3.
Study sample and recruitment plan: The study population involved in this national survey includes the general population who do not have diabetes and those who self-report a diagnosis of diabetes. The diabetes population will be supplemented with age, gender and ethnicity matched treatment seeking patients (n=330) for a robust analysis. ‡ Diagnosed by a clinician and seeking treatment (estimated based on the reported prevalence).
Screening for diabetes in the general public
Since a significant proportion of the population is likely to be unaware of their diabetes status,6 those without a history of diabetes will be offered a blood test to measure their fasting blood glucose and glycosylated haemoglobin (HbA1c). Among those who provide consent for the blood test, a maximum of 300 respondents will be randomly chosen to undergo the test. The selection of the respondents is indicated in figure 3. The results will provide information on the extent of ‘undiagnosed’ diabetes in the population. This group will be considered as 'undiagnosed diabetes’ and compared against those with and without diabetes.
Questionnaires
The following questionnaires are included in the survey. The details of the questionnaire are included in the online supplementary section.
bmjopen-2020-037125supp001.pdf (132.9KB, pdf)
Socio-demographic information
Diabetes recognition and knowledge using vignettes
Diabetes KAP questionnaire
Diabetes stigma questionnaire
Chronic conditions checklist
Health related quality of life (Short Form (SF)- 12)
Global physical activity questionnaire
Brief health literacy screen
Marlowe-Crowne social desirability scale
Lepore’s social constraints scale
Diet screener
Barriers and facilitators of diabetes health screen
Disability screening questionnaire
Barrier to physical activity questionnaire
Awareness towards diabetes programme
Lifestyle questionnaire
E-health
The Diabetes Mellitus Disease Severity Index (DCSI)
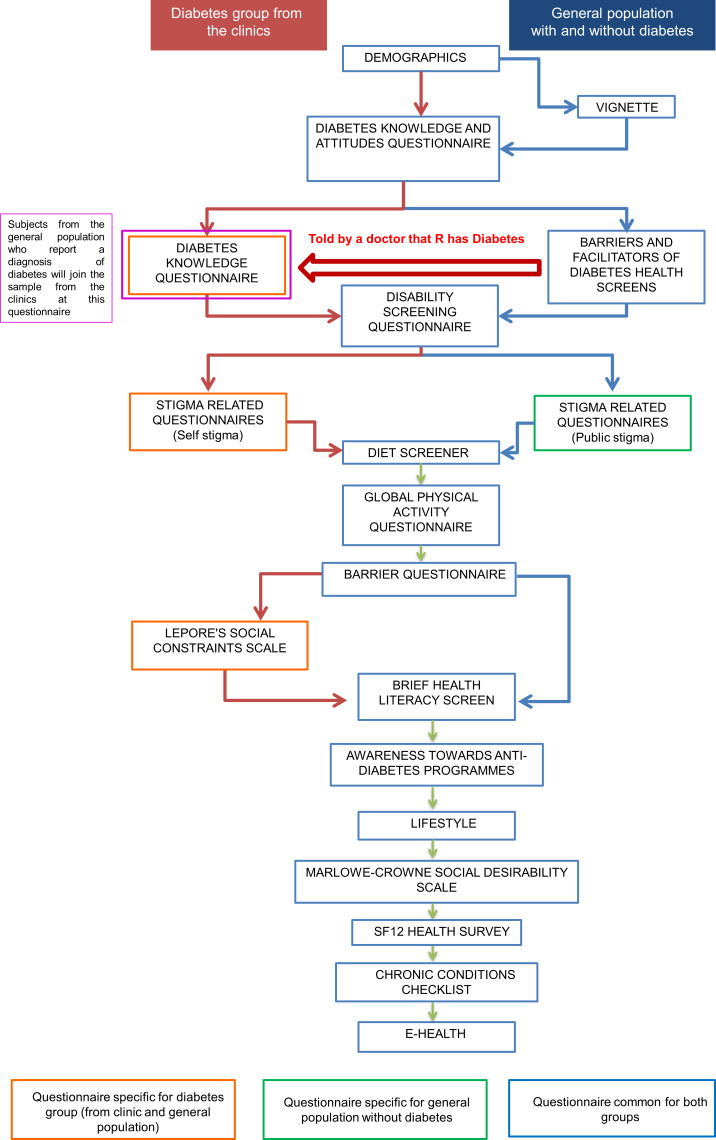
Additional data collected among patients with diabetes
The flow of the questionnaires between those with and without diabetes is represented in figure 4. Those with diabetes will be asked additional questions on diabetes knowledge (care and management), self-stigma and social constraints. The DCSI data will be captured for diabetes patients by the attending clinician or a researcher supervised by the clinician.
Figure 4.
Flow chart of the questionnaires.
Translation and cognitive interviews
All survey measures were available or translated into the three local languages—Chinese, Malay and Tamil using a professional translating firm. The translation procedure undertaken was aimed at achieving conceptual equivalence using a four-step process that was adapted from the WHO method: (1) two independent forward translations, (2) expert panel review, (3) pre-testing and cognitive interviewing and (4) development of a final version. (1) Forward translation, the initial translation of the original English version into the three main local languages spoken in Singapore (Chinese, Malay and Tamil) was done by professional translators. (2) An expert panel review, in which members who acted as expert consultants in various fields pertinent to the study, as well as a layperson, offered advice and possible solutions to problems identified in the first draft of the translation. Issues were resolved by critical evaluation of the considerations and recommendations by each expert in their respective fields. (3) Pre-testing and cognitive interviews (CIs) were undertaken to assess how well the measures were likely to be received by the lay members of the public, the target audience for the survey, in each of the specified languages. Around 25 CIs were conducted to ensure that the vignette and questionnaires would be well understood by lay respondents for comprehension, retrieval, decision-making and response processes. The questionnaire was modified based on the CI, by incorporating the respondents' feedback and suggestions.
Data analysis plan
Descriptive statistics will be used to describe the socio-demographic characteristics of the sample. Since the majority of the questionnaires are being used for the first time in the local population, they will be validated. To evaluate reliability, Cronbach’s alpha for each of the questionnaires will be calculated. Internal consistency of the knowledge questionnaire, including items related to diabetes care principles, will be measured. Similarly, the reliability of other questionnaires for attitude, diet and physical activity behaviour and stigma will be calculated. The construct validity of the KAP questionnaire will be assessed with exploratory factor analysis.
Cross tabulation will be used to determine the findings relating to recognition, and KAP across the two groups. Significant differences in the proportions of people endorsing various KAPs will be determined using a χ2 test. Beliefs about the causes and treatment options for diabetes as well as the expected outcomes for someone with diabetes will also be similarly described. We will use listwise deletion to deal with missing data when analysing the data set. However, if the proportion of missing data is significantly high, we will examine the missing data pattern to determine if it is missing at random, missing completely at random or missing not at random before performing imputations on the data set.16
Multiple logistic and linear regression analyses will be carried out to determine the socio-demographic correlates of correctly recognising diabetes, help-seeking preferences, as well as overall knowledge and attitudes among those with and without diabetes. Practices and attitudes regarding treatment and stigma will be investigated among important subgroups. In order to ensure that the findings from the household survey represent the Singapore adult population, all estimates will be analysed using survey weights to adjust for oversampling, non-response and post-stratification according to age and ethnicity of the Singapore population. Sampling errors will be assessed by an estimated 95% CIs around the estimates and performing relevant sensitivity analyses. We will consider a p value of ≤0·05 as significant.
Discussion
This is one of the first population-wide studies that aims to explore diabetes KAP among the resident population in Singapore. The majority of the studies conducted in Asia and Southeast Asia, have focussed on either patients with a known diagnosis of diabetes or the general population who are not representative of the overall population of the country.17–21 The methodology, which includes the use of a vignette-based approach, has been used previously in Singapore to capture recognition, knowledge and attitudes towards people with mental illness in a recently completed national mental health literacy study.22 23 The current study will serve as a baseline measure of diabetes knowledge for Singapore’s general population and will be used to inform future health policies as part of ongoing efforts in the ‘War on Diabetes’. More specifically, it will identify whether people are able to recognise the signs and symptoms of diabetes and whether they know where to seek help or treatment for diabetes. It will also identify subgroups of the population who may have poor recognition or knowledge of diabetes, which will then allow for targeted efforts to improve their knowledge.
While the concept of stigma has been largely examined in association with mental illness, there are very few studies that have examined stigma among those with diabetes. An online survey of over 5000 people with diabetes in the USA found that 61% of people with T2DM on intensive insulin therapies and 51% of people taking pills reported feeling stigmatised.24 This could be due in part to the therapy’s visibility such as finger pricks and shots, as people without diabetes may not fully understand it leading to awkwardness or questions which may lead to self-stigma. Schabert et al25 highlighted the adverse consequences of the stigma, for example, distress, poorer psychological well-being and suboptimal self-care, and they emphasised the need for strategies to reduce diabetes-related stigma. This study is the first in Singapore to explore the components and associations of stigma with KAP among those with diabetes. This hitherto neglected area would have important implications in the management of diabetes.
The study will also capture and compare the dietary and lifestyle practices of the respondents with and without diabetes. Several studies have shown that a large proportion of cases of T2DM can be prevented. The results of a meta-analysis of the evidence from cohort studies suggest that high glycaemic index diets may increase the risk of diabetes26 27 while a diet rich in dietary fibre may reduce the risk.28 Pan et al29 conducted a cluster randomised trial that showed a healthy diet, exercise and a combination of diet and exercise can all substantially reduce the risk of diabetes. A 20-year follow-up study combining the three lifestyle intervention groups showed a 43% lower diabetes risk compared with the control group.30 Similarly, multiple studies conducted in Japan, Finland and the Middle East have shown a decrease in diabetes incidence through active intervention.31–34 The information gathered in our study will help us to understand the current lifestyle, factors contributing to unhealthy lifestyle, reasons for the choice of lifestyle practices, current physical activity and barriers and facilitators of physical activity of the general population with and without diabetes. This knowledge is helpful to estimate the effectiveness of ongoing public lifestyle campaigns and to identify areas of improvement.
We acknowledge several challenges with our study design. As the survey pertains to lifestyle and health practices, the respondents may provide socially desirable answers leading to social desirability bias, this will, however, be controlled through the scores on the Marlowe-Crowne Social Desirability questionnaire that has been embedded in the survey. This being a cross-sectional study we will not be able to rule out the intrinsic risk of reverse causation.
In summary, this study will form the first nationwide survey representative of the entire Singapore population, conducted in the last 10-year period to understand the Singapore residents’ KAP towards diabetes. This study will further our understanding of the current lifestyle of Singapore residents, as well as preventive and management strategies adopted by the residents towards diabetes. The study will also shed light on the awareness of the public towards on-going ‘War on Diabetes’ and other government initiatives to tackle diabetes and thus help the policymakers to design meaningful and suitable programmes that have better penetration and are aligned with the expectations of the public.
Ethics and dissemination
This study protocol has been reviewed by the Institutional Research Review Committee and the National Healthcare Group Domain Specific Review Board (NHG DSRB Ref 2018/00430). Following the analysis, the study findings will be disseminated to the relevant stakeholders. This will include a press briefing informing the local mass media of the study findings and using this platform to disseminate the findings to the general population, via online, television, print and radio. A structured dissemination plan has been developed and will encompass various forms of communication that will occur via multiple platforms including publishing in academic journals, presentations at scientific meetings and conferences, presentation of the key findings to key stakeholders, for example, Ministry of Health, Singapore, Health Promotion Board, Diabetes Society of Singapore, general practitioners and other healthcare providers involved in the care of people with diabetes.
Supplementary Material
Acknowledgments
We thank the participants from the general public and diabetes clinics who gave us valuable inputs in the questionnaire development phase that helped us to improve the questionnaire and adapt it for local population.
Footnotes
Contributors: MS, SAC, RVD, ELS and SCF were involved in the conceptualisation of the study. AP wrote and revised the manuscript. JAV, RK, FDSK, AJ, AP, MS, SAC, RVD, ESL, SCF and SS were involved in the questionnaire design. MS, AP, FDSK and RK conducted cognitive testing of the survey questionnaire. EA provided the statistical design and sampling strategy. BYC designed and supports the database. All the authors reviewed and approved the manuscript. MS and SAC take full responsibility of the protocol design.
Funding: This study is funded by National Medical Research Council of Singapore (NMRC/HSRG/0085/2018).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting or dissemination plans of this research. Refer to the Methods section for further details.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.World Health Organization Global report on diabetes, 2016. Available: https://www.who.int/diabetes/global-report/en/ [Accessed 2 Dec 2019].
- 2.Cho NH, Shaw JE, Karuranga S, et al. IDF diabetes atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract 2018;138:271–81. 10.1016/j.diabres.2018.02.023 [DOI] [PubMed] [Google Scholar]
- 3.Papatheodorou K, Papanas N, Banach M, et al. Complications of diabetes 2016. J Diabetes Res 2016;2016:1–3. 10.1155/2016/6989453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.The Straits Times Aw Cheng Wei Singapore Economy ranked world’s most competitive, 2019. Available: https://www.straitstimes.com/business/economy/singapore-economy-ranked-worlds-most-competitive [Accessed 2 Dec 2019].
- 5.World Health Organisation World Health Organisation assesses the world’s Health systems, 2000. Available: https://www.who.int/whr/2000/media_centre/press_release/en/ [Accessed 25 Oct 2019].
- 6.Ministry of Health National health survey, 2010. Available: https://www.moh.gov.sg/content/dam/moh_web/Publications/Reports/2011/NHS2010%20-%20low%20res.pdf [Accessed 25 Oct 2019].
- 7.Epidemiology & Disease Control Division The burden of disease in Singapore, 1990–2017: an overview of the global burden of disease study 2017 results. Seattle, WA: IHME, 2019. http://www.healthdata.org/sites/default/files/files/policy_report/2019/GBD_2017_Singapore_Report.pdf [Google Scholar]
- 8.Png ME, Yoong J, Phan TP, et al. Current and future economic burden of diabetes among working-age adults in Asia: conservative estimates for Singapore from 2010-2050. BMC Public Health 2016;16:153. 10.1186/s12889-016-2827-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khalik S. Singapore to ban ads of packaged drinks with high sugar, 2019. Available: https://www.straitstimes.com/singapore/health/spore-to-ban-ads-of-packaged-drinks-with-very-high-sugar [Accessed 25 Oct 2019].
- 10.Kaliyaperumal K. Guideline for conducting a knowledge, attitude and practice (KAP) study. AECS Illumination 2004;4:7–9. [Google Scholar]
- 11.Aljofan M, Altebainawi A, Alrashidi MN. Public knowledge, attitude and practice toward diabetes mellitus in hail region, Saudi Arabia. Int J Gen Med 2019;12:255. 10.2147/IJGM.S214441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gillani AH, Amirul Islam FM, Hayat K, Islam A, Mohammad F, et al. Knowledge, attitudes and practices regarding diabetes in the general population: a cross-sectional study from Pakistan. Int J Environ Res Public Health 2018;15:1906. 10.3390/ijerph15091906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wee HL, Ho HK, Li SC. Public awareness of diabetes mellitus in Singapore. Singapore Med J 2002;43:128–34. [PubMed] [Google Scholar]
- 14.Subramaniam M, Abdin E, Vaingankar JA, et al. Tracking the mental health of a nation: prevalence and correlates of mental disorders in the second Singapore mental health study. Epidemiol Psychiatr Sci 2019;29:e29. 10.1017/S2045796019000179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Subramaniam M, Vaingankar J, Heng D, et al. The Singapore mental health study: an overview of the methodology. Int J Methods Psychiatr Res 2012;21:149–57. 10.1002/mpr.1351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Little RJ, Rubin DB. Statistical analysis with missing data (Vol. 793). John Wiley & Sons, 2019. [Google Scholar]
- 17.Rajbhandari S, Riewpaiboon A, Rattanaphanit S, et al. Knowledge, attitude, practice (KAP) and health related quality of life of priests with type 2 diabetes mellitus in Thailand. Pharm Sci Asia 2018;45:93–104. 10.29090/psa.2018.02.093 [DOI] [Google Scholar]
- 18.Binh TQ, Phuong PT, Nhung BT. Knowledge and associated factors towards type 2 diabetes among a rural population in the red River delta region, Vietnam. Rural Remote Health 2015;15:3275. [PubMed] [Google Scholar]
- 19.Islam FMA, Chakrabarti R, Dirani M, et al. Knowledge, attitudes and practice of diabetes in rural Bangladesh: the Bangladesh population based diabetes and eye study (BPDES). PLoS One 2014;9:e110368. 10.1371/journal.pone.0110368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Herath HMM, Weerasinghe NP, Dias H, et al. Knowledge, attitude and practice related to diabetes mellitus among the general public in Galle district in southern Sri Lanka: a pilot study. BMC Public Health 2017;17:535. 10.1186/s12889-017-4459-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mahdi HJ, Hassan Y, Aziz NA, et al. Diabetes knowledge and practice in Malaysian and the United Arab Emirates diabetic patients. Res Jof Pharm Biol Chem Sci 2013;4:653–65. [Google Scholar]
- 22.Chong SA, Abdin E, Picco L, et al. Recognition of mental disorders among a multiracial population in Southeast Asia. BMC Psychiatry 2016;16:121. 10.1186/s12888-016-0837-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Subramaniam M, Abdin E, Picco L, et al. Stigma towards people with mental disorders and its components - a perspective from multi-ethnic Singapore. Epidemiol Psychiatr Sci 2017;26:371–82. 10.1017/S2045796016000159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Folias AE, Brown AS, Carvalho J, et al. Investigation of the presence and impact on patients of diabetes social stigma in the USA. Diabetes 2014;15. [Google Scholar]
- 25.Schabert J, Browne JL, Mosely K, et al. Social stigma in diabetes : a framework to understand a growing problem for an increasing epidemic. Patient 2013;6:1–10. 10.1007/s40271-012-0001-0 [DOI] [PubMed] [Google Scholar]
- 26.Hu FB, Manson JE, Stampfer MJ, et al. Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N Engl J Med 2001;345:790–7. 10.1056/NEJMoa010492 [DOI] [PubMed] [Google Scholar]
- 27.Malik VS, Popkin BM, Bray GA, et al. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis. Diabetes Care 2010;33:2477–83. 10.2337/dc10-1079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.de Munter JSL, Hu FB, Spiegelman D, et al. Whole grain, bran, and germ intake and risk of type 2 diabetes: a prospective cohort study and systematic review. PLoS Med 2007;4:e261. 10.1371/journal.pmed.0040261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pan XR, Li GW, Hu YH, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The da qing IGT and diabetes study. Diabetes Care 1997;20:537–44. 10.2337/diacare.20.4.537 [DOI] [PubMed] [Google Scholar]
- 30.Li G, Zhang P, Wang J, et al. The long-term effect of lifestyle interventions to prevent diabetes in the China da qing diabetes prevention study: a 20-year follow-up study. Lancet 2008;371:1783–9. 10.1016/S0140-6736(08)60766-7 [DOI] [PubMed] [Google Scholar]
- 31.Lindström J, Ilanne-Parikka P, Peltonen M, et al. Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the finnish diabetes prevention study. Lancet 2006;368:1673–9. 10.1016/S0140-6736(06)69701-8 [DOI] [PubMed] [Google Scholar]
- 32.Kosaka K, Noda M, Kuzuya T. Prevention of type 2 diabetes by lifestyle intervention: a Japanese trial in IGT males. Diabetes Res Clin Pract 2005;67:152–62. 10.1016/j.diabres.2004.06.010 [DOI] [PubMed] [Google Scholar]
- 33.Harati H, Hadaegh F, Momenan AA, et al. Reduction in incidence of type 2 diabetes by lifestyle intervention in a middle Eastern community. Am J Prev Med 2010;38:628–36. 10.1016/j.amepre.2010.03.003 [DOI] [PubMed] [Google Scholar]
- 34.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346:393–403. 10.1056/NEJMoa012512 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-037125supp001.pdf (132.9KB, pdf)