Abstract
Objective:
To compare the effect of preoperative administration of an antihistamine, an analgesic, or a placebo on postoperative pain in maxillary molar teeth with symptomatic apical periodontitis.
Design: A randomized, controlled trial.
Methods:
Population: A total of 51 patients with moderate-to-severe maxillary molar tooth pain who have undergone a root canal treatment.
Intervention: Preoperative administration of either an antihistamine or an analgesic.
Control: Versus placebo
Outcomes: Reduction in postoperative pain? The data were analyzed with chi-square, one-way analysis of variance (ANOVA) and least significant difference (LSD) post-hoc tests.
Results:
At days 1 and 3, preoperative administration of the antihistamine and analgesic resulted in lower pain levels than the placebo. At days 5 and 7, however, while preoperative administration of the antihistamine still resulted in less pain than the placebo, there was no significant difference between the analgesic and placebo (P>0.05).
Conclusion:
Within the limitations of the present study, the preoperative administration of an antihistamine can be beneficial in reducing the postoperative pain of endodontic treatments.
Keywords: Analgesic, antihistamine, endodontics, postoperative pain
INTRODUCTION
Prevention of pain after endodontic treatment is an important issue. Extrusion of microorganisms or debris during endodontic treatment results in inflammatory response (1-4). A recent systematic review showed that between 3% and 58% of patients were reported to have experienced endodontic postoperative pain (5). The management of postoperative pain has been the subject of many research studies, including preoperative explanations and instructions (6), long-acting anesthesia (7), the glide path (8), occlusal reduction (9, 10), medication using salicylic acid (11), non-steroid anti-inflammatory drugs (NSAIDs) (12), combination of ibuprofen and acetaminophen (13), narcotic analgesics (14), a combination of narcotic analgesics with aspirin (15) or acetaminophen (16), and steroidal anti-inflammatory drugs (17, 18).
Antihistamines have been used in endodontics for a variety of different purposes, including intracanal medicament (19), reducing postoperative pain by local prophylactic Benadryl injections (20), anesthesia (21), management of sodium hypochlorite accident (22), and itching (23). The first study of antihistamines in endodontics was conducted by Stewart (19), who prepared an antihistamine-antibiotic compound for root canal medication and found that this compound inhibits the growth of heavy concentrations of mixed microorganisms in vitro.
Since the vasodilator action was demonstrated in 1918 (24), histamine has been widely researched in medicine. Histamine facilitates migration of cells to inflammatory sites, stimulates lymphocyte activity, modulates aspects of eosinophil, neutrophil, and mast cell behavior (25). The effect of histamine is mediated by the H1, H2, H3, and H4 receptors. Among these, H1-receptor plays a major role in potentiation of proinflammatory immune cell activity (25). In the present study, pheniramine hydrogen maleate-an H1 receptor antagonist-was administered. H1 receptor antagonist antihistamines reduce inflammation by inhibiting NF-κB production (25) and also play a role in central pain processing (26).
Pain perception is a highly subjective and variable experience modulated by multiple physical and psychological factors, and pain reporting is influenced by factors other than the experimental procedure (27). Activation of nociceptive sensory nerve fibers may also be related to concentrations of inflammatory mediators like histamine (28). Also, histamine, an inflammatory mediator, is capable of sensitizing and activating nociceptive sensory nerve fibres (29). Oliveira et al. (30) demonstrated that pre-treatment with antihistamines decreased postoperative nociception in mice. However, there is no study related to the effect of preoperative oral administration of antihistamine on postoperative pain. Thus, the purpose of this study was to evaluate the effect of preoperative administration of antihistamine on postoperative pain in molar teeth with symptomatic apical periodontitis as compared to that of an analgesic and a placebo. The null hypothesis was that there would be no difference among the groups in postoperative pain.
MATERIALS AND METHODS
Study design
A parallel group, randomized, controlled trial with three arms.
The study was conducted in the Department of Endodontics, Erzurum Atatürk University School of Dentistry, Turkey, between April 01, 2015 and November 14, 2015 (approximately 7 months).
The Research Ethics Board of Erzurum Atatürk University, approved the study protocol (03-2015). The inclusion criteria were healthy patients, aged ≥18, with a maxillary molar tooth with symptomatic apical periodontitis. Following Cohen’s Pathways of the Pulp, symptomatic apical periodontitis was determined on the basis of the clinical symptoms severe preoperative pain (VAS>60) and severe percussion pain (VAS>60). The exclusion criteria were the following: patients under 18 years old; the presence of any systemic disease or allergic reactions; patients who had used any type of analgesic or antibiotic medication within three days; patients whose affected tooth had had root canal treatment, sinus tracts, or showed local gum swelling; patients with severe periodontal disease, periodontal pockets more than 3 mm in the affected tooth, or a periapical radiolucency more than 3 cm diameter. Also excluded were patients whose affected tooth and related work had any of the following issues: curved roots, excessively long or short root length, problems in determining working length, broken files, over-instrumentation, and over- or incomplete filling.
The patients were randomly divided into three groups using a web program. The patient number and group number were recorded. Informed consent was obtained from each patient and the possible discomforts and risks were fully explained.
A total of 51 patients were divided into three groups (n=17) according to the type of preoperative drug administrated, as follows: antihistamine (22.7 mg pheniramine hydrogen maleate [Avil; Sandoz, Kocaeli, Turkey]), analgesic (600 mg ibuprofen [Brufen; Abott, Istanbul, Turkey]), and placebo (capsule filled with sugar). The administration of drugs and root canal treatment were performed by two different researchers. The drugs were placed into capsules of the same size and color. One researcher knew the allocation and the drug type in the capsules, but the operator and the patient did not know which drug type was administered.
Fifteen minutes after drug administration, all patients received 1 cartridge of anesthetic with 4% articaine with 1:100 000 epinephrine (UltracaineDS® forte; Aventis, Istanbul, Turkey). All procedures were completed under rubber-dam isolation.
Root canal preparation
Root canal preparation was performed after electronic determination of working length with a Propex Pixi (Dentsply Maillefer, Ballaigues, Switzerland). Reciproc instruments were used to complete the root canal preparation according to the manufacturer’s instructions, using new instruments for each patient.
A size 10 K-file was used to maintain apical patency, 2 mL 1% NaOCl was used between pecking in-out motions, and a final rinse was performed using 5 mL of 1% NaOCl for 1 min and 5 mL of 5% EDTA for 1 min to remove the smear layer. After final irrigation, the root canals were dried with absorbent paper points and then filled using matched single cones and 2 seal sealer (2 seal; VDW, Munich, Germany). The pulp chamber was filled with a flowable composite resin, and a nanohybrid composite resin was inserted into the cavity using an incremental technique and cured for 20 minute using a LED light-curing unit (Valo Cordless; Ultradent, South Jordan, UT, USA) with an output of 1000 mW/cm2.
If patients experienced pain, they were advised to take 600 mg ibuprofen (Brufen; Abott, Istanbul, Turkey). Patients recorded their pain experience on a customized form, which they also used to record any analgesic intake. Also recorded were age; gender; tooth number; pulp vitality; periapical lesion; preoperative pain on the VAS; preoperative and postoperative percussion pain levels on the VAS (10 cm); pain level on the 1st, 3rd, 5th, and 7th days; palpation sensitivity; swelling and sinus tract postoperatively; and unscheduled appointment.
Statistical analysis
A linear regression analysis was used to determine the variable (group, age, gender, tooth number, preoperative pain, preoperative percussion, preoperative palpation, pulp status, or radiological situation) that best correlated with postoperative pain at day 1. Data were analyzed using the chi-square test for demographic data, pulp and periapical status, one way ANOVA and LSD post-hoc tests for pain levels (P=0.05).
RESULTS
A summary of the study can be seen in the Consort diagram. There were no significant differences among the groups in terms of demographic data (Table 1) or pulp and periapical status (Table 2) (P>0.05). Similarly, there were no significant differences among the groups in terms of preoperative pain levels (P=0.429) and percussion pain levels (P=0.558). No patient referred for an unscheduled appointment.
TABLE 1.
Demographic data (One way ANOVA or chi-square were used to analyze the data)
| Placebo | Analgesic | Antihistamine | P value | |
|---|---|---|---|---|
| Age | 31.87±7.35 | 30.69±9.02 | 28.12±5.99 | 0.351 |
| Gender | ||||
| Female | 7 | 7 | 7 | 0.789 |
| Male | 8 | 6 | 10 | |
| Tooth number | ||||
| Tooth 16 | 6 | 5 | 4 | 0.448 |
| Tooth 17 | 4 | 3 | 3 | |
| Tooth 18 | 0 | 0 | 0 | |
| Tooth 26 | 2 | 4 | 3 | |
| Tooth 27 | 3 | 1 | 7 | |
| Tooth 28 | 0 | 0 | 0 |
TABLE 2.
Pulp and periapical status of teeth and postoperative palpation, swelling, and sinus tract according to the groups. Pulp vitality was confirmed according to the presence of bleeding in pulp chamber. Periapical status was scored according to Ørstavik et al. Score 1: normal, Score 2: small changes in bone structure, Score 3: changes in bone structure with some mineral loss, Score 4: periodontitis with well-defined radiolucent area, and Score 5: severe periodontitis with exacerbating features (chi-square were used to analyze the data)
| Placebo | Analgesic | Antihistamine | P value | |
|---|---|---|---|---|
| Pulp status | ||||
| Vital | 14 | 13 | 16 | 0.650 |
| Non-vital | 1 | 0 | 1 | |
| Periapical status | ||||
| Score 1 | 14 | 12 | 16 | 0.981 |
| Score 2 | 1 | 1 | 1 | |
| Score 3 | 0 | 0 | 0 | |
| Score 4 | 0 | 0 | 0 | |
| Score 5 | 0 | 0 | 0 | |
| Presence of | ||||
| Preoperative | ||||
| Palpation | 0 | 1 | 0 | 0.284 |
| Presence of | ||||
| Preoperative | ||||
| Swelling | 0 | 0 | 0 | NA |
| Presence of | ||||
| Preoperative | ||||
| Sinus tract | 0 | 0 | 0 | NA |
| Postoperative | ||||
| Palpation | 0 | 0 | 0 | NA |
| Postoperative | ||||
| Swelling | 0 | 0 | 0 | NA |
| Postoperative | ||||
| Sinus tract | 0 | 0 | 0 | NA |
A total of 11 patients needed analgesics postoperatively: seven of these were in the placebo group, two in the analgesic group, and two in the antihistamine group. The regression analysis shows that most significant correlation with postoperative pain at day 1 was group variable (P=0.031).
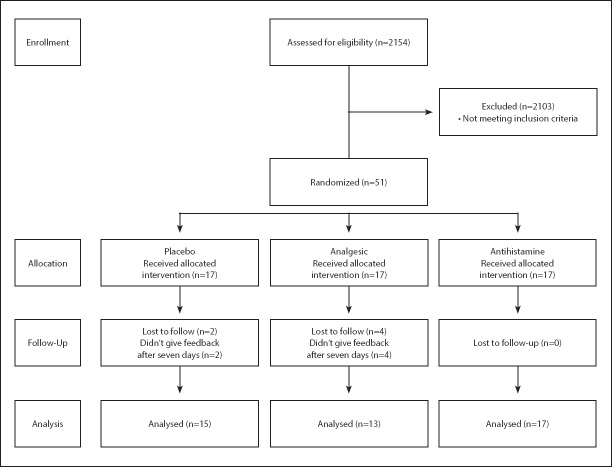
Figure 1 shows the postoperative pain levels by group. According to the LSD post-hoc test, at days 1 and 3, the preoperative administration of antihistamine and analgesic groups recorded lower pain levels than did the placebo group. At days 5 and 7, the preoperative administration of antihistamine group recorded less pain than did the placebo, but there was no significant difference between the analgesic and placebo administration groups (P>0.05) (Table 3).
Figure 1.
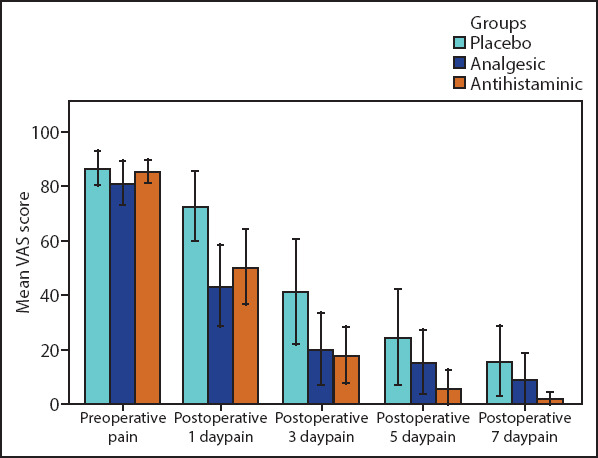
Change in pain levels according to day. There were no significant differences among the groups in terms of preoperative pain (P>0.05). At days 1 and 3, the preoperative administration of antihistamine and analgesic resulted in lower pain levels than a placebo (P<0.05). At days 5 and 7, the preoperative administration of antihistamine resulted in less pain than the placebo (P<0.05), but there was no significant difference between the placebo and analgesic administration (P>0.05)
TABLE 3.
Pain levels±standard deviations according to the groups. One way ANOVA test was performed to analyze if there is a statistical significant differences among the groups. LSD post hoc test was performed for pairwise comparison
| Placebo | Analgesic | Antihistamine | P value | Observed power | |
|---|---|---|---|---|---|
| Preoperative percussion | 78.40±10.86 | 74.92±16.74 | 80.59±14.59 | 0.558 | -- |
| Preoperative pain | 86.40±11.64 | 81.08±13.56 | 85.29±8.52 | 0.429 | -- |
| Postoperative 1 day pain | 72.60±23.17 | 43.46±25.33 | 50.24±27.02 | 0.009 | 0.806 |
| Postoperative 3 day pain | 41.27±34.82 | 20.38±22.09 | 17.94±20.25 | 0.037 | 0.632 |
| Postoperative 5 day pain | 24.67±31.66 | 15.54±19.64 | 5.88±12.81 | 0.074 | 0.518 |
| Postoperative 7 day pain | 15.60±23.52 | 8.85±16.49 | 1.71±5.33 | 0.071 | 0.525 |
DISCUSSION
Although preoperative administration of analgesics has been found to be effective in reducing postoperative pain (31, 32), there has been no study related to the effect of the preoperative oral administration of antihistamines on postoperative pain. Thus, the purpose of this study was to evaluate the effect of preoperative administration of antihistamine on postoperative pain in molar teeth with symptomatic apical periodontitis as compared to that of analgesic and placebo.
The null hypothesis was that there would be no difference among the antihistamine, analgesic, and placebo groups in terms of postoperative pain. However, the preoperative administration of both antihistamine and analgesic resulted in lower pain levels than did that of a placebo at days 1 and 3. Thus, the null hypothesis was rejected.
Wells et al. (33) found that there were decreases in postoperative pain levels with the preoperative use of ibuprofen, a finding in harmony with ours. Since there have not been any studies on the effect of preoperative administration of antihistamine on postoperative pain, a direct comparison here between present and previous findings here is not possible. The decreased pain levels in the antihistamine group can be explained by the ability of antihistamine to eliminate effects mediated by histamine resulting in sensitization and activation of nociceptive sensory nerve fibers (29).
Nevins et al. (20) locally injected antihistamine preoperatively and compared this to local anesthetics in reducing postoperative endodontic pain. According to the results, there were no significant differences between the two (antihistamine and anesthetic) groups. This finding is inconsistent with the results of the present study. The difference between the results might be due to the different administration types (local and systemic).
An interesting finding in the present study was that while the preoperative administration of antihistamine resulted in less pain than that of a placebo at days 1 through 7, there was no significant difference between analgesic and placebo administration at days 5 and 7 (P>0.05). These findings suggest that the preoperative administration of antihistamine is beneficial in reducing postoperative pain for 1 week.
An interesting paper by Oliveira et al. (30) aimed to investigate the involvement of mast cells in a model of postoperative pain in mice. Plantar surgery produced immense mast cell degranulation, and a pre-treatment with antihistamines decreased postoperative nociception in mice. The findings of the present study are harmonious with those of the Oliveira et al. (30) study.
Patients requiring endodontic treatment were evaluated for the present study. A total of 51 patients met the inclusion and exclusion criteria and were treated for approximately 7 months. Healthy patients undergoing endodontic treatment for symptomatic apical periodontitis were included in this clinical study. Only maxillary molar teeth without anatomical/technical difficulties, periodontal severe disease, or periapical radiolucency more than 3 cm diameter were included in the study.
The present study was a small 3-armed trial of an antihistamine, an analgesic, and a placebo in healthy adults with symptomatic apical periodontitis. One of the strengths of small studies is that they need only a short time for completion (approximately 7 months for this study). In the present study, the patients were randomly divided into groups using a web site. According to the “Levels of Evidence” classification, randomized clinical trials provide the best evidence. The randomization procedure can be viewed as one of the strengths of the present study (31).
The main limitation of the small studies is that they generate underpowered results. In the present study, the results were underpowered, except those obtained on day 1. Thus, a large sample size study should be conducted to confirm the results of the present study.
Post hoc comparisons can be conducted to check all paired comparisons for possible differences. However, this multiple test may produce type 1 error. In the present study, post hoc tests were used to check all paired comparisons, while keeping this limitation in mind.
CONCLUSION
Preoperative administration of an antihistamine can be beneficial in reducing the postoperative pain of endodontic treatments. However, a large sample size study should be conducted to confirm the results of the present study.
Footnotes
Ethical Approval: Ethics committee approval was received for this study from the ethics committee of Erzurum Atatürk University.
Informed Consent: Written informed consent was obtained from patient who participated in this study.
Peer-review: Externally peer-reviewed.
Authorship contributions: Concept - H.A.; Design - H.A.; Supervision - H.A.; Funding – N/A; Materials - E.C.G., M.S.; Data Collection and/or Processing - E.C.G., M.S.; Analysis and/or Interpretation - H.A.; Literature Review - H.A., E.C.G., M.S.; Writer - H.A.; Critical Review - H.A., E.C.G., M.S.
Conflict of interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Cunningham CJ, Mullaney TP. Pain control in endodontics. Dent Clin North Am. 1992;36(2):393–408. [PubMed] [Google Scholar]
- 2.Arias A, de la Macorra JC, Hidalgo JJ, Azabal M. Predictive models of pain following root canal treatment:a prospective clinical study. Int Endod J. 2013;46(8):784–93. doi: 10.1111/iej.12059. [DOI] [PubMed] [Google Scholar]
- 3.Pak JG, White SN. Pain prevalence and severity before, during, and after root canal treatment:a systematic review. J Endod. 2011;37(4):429–38. doi: 10.1016/j.joen.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 4.Seltzer S, Naidorf IJ. Flare-ups in endodontics:I. Etiological factors. J Endod. 1985;11(11):472–8. doi: 10.1016/S0099-2399(85)80220-X. [DOI] [PubMed] [Google Scholar]
- 5.Sathorn C, Parashos P, Messer H. The prevalence of postoperative pain and flare-up in single- and multiple-visit endodontic treatment:a systematic review. Int Endod J. 2008;41(2):91–9. doi: 10.1111/j.1365-2591.2007.01316.x. [DOI] [PubMed] [Google Scholar]
- 6.Andrew JM. Recovery from surgery, with and without preparatory instruction, for three coping styles. J Pers Soc Psychol. 1970;15(3):223–6. doi: 10.1037/h0029442. [DOI] [PubMed] [Google Scholar]
- 7.Parirokh M, Yosefi MH, Nakhaee N, et al. Effect of bupivacaine on postoperative pain for inferior alveolar nerve block anesthesia after single-visit root canal treatment in teeth with irreversible pulpitis. J Endod. 2012;38(8):1035–9. doi: 10.1016/j.joen.2012.04.012. [DOI] [PubMed] [Google Scholar]
- 8.Pasqualini D, Mollo L, Scotti N, et al. Postoperative pain after manual and mechanical glide path:a randomized clinical trial. J Endod. 2012;38(1):32–6. doi: 10.1016/j.joen.2011.09.017. [DOI] [PubMed] [Google Scholar]
- 9.Parirokh M, Rekabi AR, Ashouri R, et al. Effect of occlusal reduction on postoperative pain in teeth with irreversible pulpitis and mild tenderness to percussion. J Endod. 2013;39(1):1–5. doi: 10.1016/j.joen.2012.08.008. [DOI] [PubMed] [Google Scholar]
- 10.Rosenberg PA, Babick PJ, Schertzer L, Leung A. The effect of occlusal reduction on pain after endodontic instrumentation. J Endod. 1998;24(7):492–6. doi: 10.1016/S0099-2399(98)80054-X. [DOI] [PubMed] [Google Scholar]
- 11.Morse DR, Esposito JV, Furst ML. Comparison of prophylactic and on-demand diflunisal for pain management of patients having one-visit endodontic therapy. Oral Surg Oral Med Oral Pathol1990; 69(6):729–36. doi: 10.1016/0030-4220(90)90358-y. [DOI] [PubMed] [Google Scholar]
- 12.Attar S, Bowles WR, Baisden MK, et al. Evaluation of pretreatment analgesia and endodontic treatment for postoperative endodontic pain. J Endod. 2008;34(6):652–5. doi: 10.1016/j.joen.2008.02.017. [DOI] [PubMed] [Google Scholar]
- 13.Menhinick KA, Gutmann JL, Regan JD, et al. The efficacy of pain control following nonsurgical root canal treatment using ibuprofen or a combination of ibuprofen and acetaminophen in a randomized, double-blind, placebo-controlled study. Int Endod J. 2004;37(8):531–41. doi: 10.1111/j.1365-2591.2004.00836.x. [DOI] [PubMed] [Google Scholar]
- 14.Ryan JL, Jureidini B, Hodges JS, et al. Gender differences in analgesia for endodontic pain. J Endod. 2008;34(5):552–6. doi: 10.1016/j.joen.2008.01.021. [DOI] [PubMed] [Google Scholar]
- 15.Morse DR, Furst ML, Koren LZ, et al. Comparison of diflunisal and an aspirin-codeine combination in the management of patients having one-visit endodontic therapy. Clinical therapeutics. 1987;9(5):500–11. [PubMed] [Google Scholar]
- 16.Sadeghein A, Shahidi N, Dehpour AR. A comparison of ketorolac tromethamine and acetaminophen codeine in the management of acute apical periodontitis. J Endod. 1999;25(4):257–9. doi: 10.1016/S0099-2399(99)80154-X. [DOI] [PubMed] [Google Scholar]
- 17.Mehrvarzfar P, Shababi B, Sayyad R, et al. Effect of supraperiosteal injection of dexamethasone on postoperative pain. Australian endodontic journal :the journal of the Australian Society of Endodontology Inc. 2008;34(1):25–9. doi: 10.1111/j.1747-4477.2007.00076.x. [DOI] [PubMed] [Google Scholar]
- 18.Pochapski MT, Santos FA, de Andrade ED, Sydney GB. Effect of pretreatment dexamethasone on postendodontic pain. Oral Surg Oral Med Oral Pathol. 2009;108(5):790–5. doi: 10.1016/j.tripleo.2009.05.014. [DOI] [PubMed] [Google Scholar]
- 19.Stewart GG. An antihistamine-antibiotic compound for root canal medication. Oral Surg Oral Med Oral Pathol. 1953;6(11):1338–47. doi: 10.1016/0030-4220(53)90266-7. [DOI] [PubMed] [Google Scholar]
- 20.Nevins A, Verhelle R, Feldman MJ, Berman D. Local prophylactic benadryl injections in an attempt to reduce postinstrumental pain. J Endod. 1994;20(6):296–8. doi: 10.1016/s0099-2399(06)80820-4. [DOI] [PubMed] [Google Scholar]
- 21.Willett J, Reader A, Drum M, et al. The anesthetic efficacy of diphenhydramine and the combination diphenhydramine/lidocaine for the inferior alveolar nerve block. J Endod. 2008;34(12):1446–50. doi: 10.1016/j.joen.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 22.Becker GL, Cohen S, Borer R. The sequelae of accidentally injecting sodium hypochlorite beyond the root apex. Report of a case. Oral Surg Oral Med Oral Pathol. 1974;38(4):633–8. doi: 10.1016/0030-4220(74)90097-8. [DOI] [PubMed] [Google Scholar]
- 23.Montagnese TA, Setty M. A clinical report of the management of episodic idiopathic pruritus occurring during endodontic therapy. J Endod. 2013;39(3):415–6. doi: 10.1016/j.joen.2012.10.010. [DOI] [PubMed] [Google Scholar]
- 24.Dale HH, Richards AN. The vasodilator action of histamine and of some other substances. J Physiol. 1918;52(2-3):110–65. doi: 10.1113/jphysiol.1918.sp001825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Canonica GW, Blaiss M. Antihistaminic, anti-inflammatory, and antiallergic properties of the nonsedating second-generation antihistamine desloratadine:a review of the evidence. World Allergy Organ J. 2011;4(2):47–53. doi: 10.1097/WOX.0b013e3182093e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Karaman K, Bostanci EB, Aksoy E, et al. Effects of dexamethasone and pheniramine hydrogen maleate on stress response in patients undergoing elective laparoscopic cholecystectomy. Am J Surg. 2013;205(2):213–9. doi: 10.1016/j.amjsurg.2012.05.010. [DOI] [PubMed] [Google Scholar]
- 27.Bender IB. Pulpal pain diagnosis--a review. J Endod. 2000;26(3):175–9. doi: 10.1097/00004770-200003000-00012. [DOI] [PubMed] [Google Scholar]
- 28.Cohen S, Hargreaves KM, Keiser K, LCC MC. Pathways of the Pulp. Mosby. 2010 [Google Scholar]
- 29.Hargreaves KM, Swift JQ, Roszkowski MT, et al. Pharmacology of peripheral neuropeptide and inflammatory mediator release. Oral Surg Oral Med Oral Pathol. 1994;78(4):503–10. doi: 10.1016/0030-4220(94)90045-0. [DOI] [PubMed] [Google Scholar]
- 30.Oliveira SM, Drewes CC, Silva CR, et al. Involvement of mast cells in a mouse model of postoperative pain. Eur J Pharmacol. 2011;672(1-3):88–95. doi: 10.1016/j.ejphar.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 31.Arslan H, Topcuoglu HS, Aladag H. Effectiveness of tenoxicam and ibuprofen for pain prevention following endodontic therapy in comparison to placebo:a randomized double-blind clinical trial. J Oral Sci. 2011;53(2):157–61. doi: 10.2334/josnusd.53.157. [DOI] [PubMed] [Google Scholar]
- 32.Attar S, Bowles WR, Baisden MK, et al. Evaluation of pretreatment analgesia and endodontic treatment for postoperative endodontic pain. J Endod. 2008;34(6):652–5. doi: 10.1016/j.joen.2008.02.017. [DOI] [PubMed] [Google Scholar]
- 33.Wells LK, Drum M, Nusstein J, et al. Efficacy of ibuprofen and ibuprofen/acetaminophen on postoperative pain in symptomatic patients with a pulpal diagnosis of necrosis. J Endod. 2011;37(12):1608–12. doi: 10.1016/j.joen.2011.08.026. [DOI] [PubMed] [Google Scholar]


