On February 21, the first cases of severe acute respiratory syndrome coronavirus 2 infection were diagnosed in hospitalized patients in the Lombardy and Veneto regions of Italy. Immediately, the population was warned by public health authorities to avoid nonurgent visits to the emergency department. During the subsequent days, the number of people affected, and the number of hospital beds occupied by patients with coronavirus disease 2019 (COVID-19) increased exponentially. A lockdown was imposed by the Italian government on March 8. At the same time, the population was warned by public authorities not to misuse the emergency services due to the possible overload of hospital capacity and risk of infection.
We reported the trends in urgent pacemaker implantations in 10 hospitals of the Veneto region of Italy during the six weeks before and after the COVID-19 outbreak started and during the corresponding 2019 period.
The authors declare that all supporting data are available within the article. We evaluated the number of urgent pacemaker implantations in 10 different hospitals of the Veneto region during the 6 weeks before and after February 21, 2020 (day of the first COVID-19 diagnosis in Italy). We also evaluated the corresponding 12 weeks in 2019. Urgent pacemaker implantation was defined as the presence of symptomatic sinus dysfunction or atrioventricular conduction disturbance that required admission to the emergency department and pacemaker implantation within one week. To account for the reduced number of heart surgery and transcatheter aortic valve replacement interventions, we excluded pacemaker implantation for postprocedural atrioventricular block.
In our region, patients evaluated in the outpatient setting that needs urgent pacemaker implantation must be admitted through the emergency department; those who were not deemed severe enough to require urgent admission were excluded.
Data are presented as counts (%) or as median (first–third quartiles). Categorical variables were compared with the χ2 test while continuous data were compared using the the Mann-Whitney U test. Behavior of counts over time has been modeled using a loess function within a Conway-Maxwell Poisson regression allowing for time-induced overdispersion. Analyses were made with the R System X and the COMPoissonReg libraries X. The study was approved by the ethical committee. Because of the type of investigation, consent from patients was waived.
The number of urgent pacemaker implantations (excluding postheart surgery or transcatheter aortic valve replacement atrioventricular blocks) during the 6 weeks before and after February 21, 2020 and during the corresponding period in 2019 are shown in the Figure. Compared with the 6 weeks before the first COVID-19 case, a significant decrease in the number of urgent pacemaker implantations was observed during the 6 weeks after (from 122 to 88, −28%; P=0.02). The decrease appeared particularly evident after the lockdown was imposed by the Italian government on March 8. In 2019, a similar number of pacemaker implantations were performed during the 6 weeks before February 21 compared with 2020 (119 versus 122, +3%; P=0.80). After this date, the number of pacemaker implantations in 2019 remained similar (123) while in 2020 it decreased to 88 (−29%; P=0.02).
Figure.
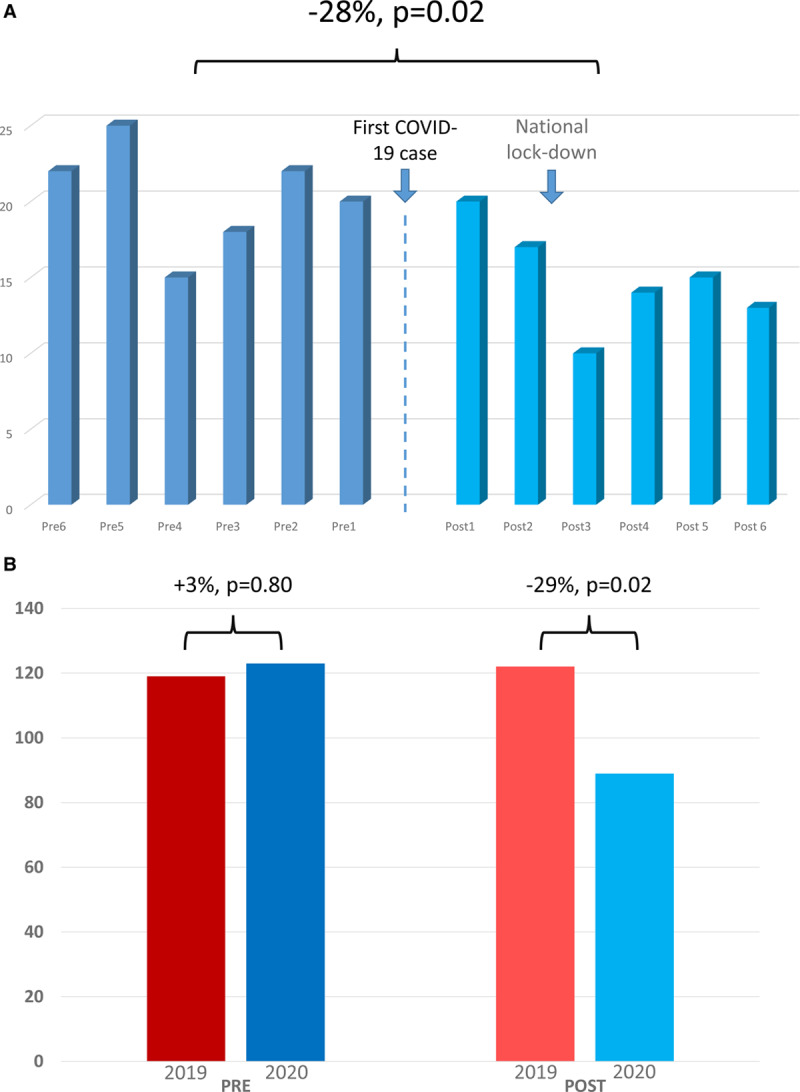
Urgent pacemaker implantations before and during the coronavirus disease 2019 (COVID-19) outbreak. Number of urgent pacemaker implantations (excluding post heart surgery and post trans-aortic valve implantation atrioventricular blocks) in 10 hospitals of the Veneto region of Italy during each of the 6 weeks before (dark color bars) and after (light color bars) the beginning of the COVID-19 outbreak on February 21, 2020 (A). Cumulative number of urgent pacemaker implantation during the 6 wk period before February 21, 2019 (pre 2019); before February 21, 2020 (pre 2020); after February 21, 2019 (post 2019); and after February 21, 2020 (post 2020; B).
In 2020, the proportion of female patients requiring urgent pacemaker decreased after the COVID-19 outbreak from 60/122 (49%) to 30/88 (34%; P=0.03). There were no differences in terms of median age (81 [77–86] versus 82 [75–88], P=0.52), proportion of patients implanted for complete atrioventricular block (44% versus 50%, P=0.41), proportion of patients who presented for syncope (46% versus 53%, P=0.07) and proportion of patients who presented within 24 hours after symptom onset (52% versus 60%, P=0.18) between the 2 study periods.
While cardiology societies are trying to answer the mystery of the missing ST-segment elevation myocardial infarctions during the COVID-19 pandemic, our research group found a reduction in urgent pacemaker implantation rates in the Veneto region of Italy. Although we may advance different hypothesis to explain this finding, we believe that the most likely explanation is that many people, fearing infection, may not seek medical attention even for severe symptoms. The proportion of patients who presented for syncope and within 24-hour after symptoms onset increased after the COVID-19 outbreak started, although the difference was not significant, while the proportion of women significantly decreased. This suggest that particularly patients with less symptomatic bradycardia refrained from seeking medical attention. According to our findings, this behavior appears more frequent among females. Thus, in the next weeks we may expect an increase in the number of patients who are suffering the consequences of this crisis and we may see several complications, including cardiogenic shock, caused by the delayed treatment of these patients. Finally, it is conceivable that part of the deaths occurring during this pandemic may be caused by the absence of otherwise routine medical care rather than COVID-19.
Sources of Funding
None.
Disclosures
None.
Footnotes
Nonstandard Abbreviations and Acronyms
- COVID-19
- coronavirus disease 2019
Drs Migliore and Zorzi contributed equally to this work.
For Sources of Funding and Disclosures, see page 577.


