INTRODUCTION
To address the unprecedented challenges posed by coronavirus disease 2019 (COVID-19), our healthcare system has appropriately shifted attention and resources to a rapidly growing population of affected patients. Hospitals, in order to expand capacity, have postponed elective surgical cases in order to avail additional beds, ventilators, and personal protective equipment.1 However, this delay has unintended consequences on the health of patients with indications for surgical procedures currently deemed “non-essential,” which may reverberate through our health system for years to come.
Patients with degenerative, traumatic, and oncological spinal pathologies represent a rapidly growing population, with rates of lumbar spinal fusions nearly quadrupling over three decades.2,3 With recent restrictions on “elective procedures,” many of these patients are currently living with unaddressed or under-addressed disease processes, which is associated with increased long-term morbidity and mortality.4 For patients with spinal cord injuries, unstable spinal fractures, or oncological compression, who may exist in a nebulous “gray zone” that falls short of the threshold of emergent cases, this means enduring severe myelopathy, radiculopathy, and chronic pain without appropriate intervention. As of the drafting of this article, there are over 690,000 confirmed COVID-19 cases in the United States, among a global burden of 2.27 million cases, with hospitalization demand projected by some to far exceed available capacity despite the aforementioned measures.5,6 Under these circumstances, the resumption of non-emergent surgeries may be months away. Here, we present pre- and post-restriction spinal case volume in the 5200-bed Schoen Clinic, the largest family-owned (i.e. under the equity ownership and management of a member of a single family since its inception) hospital group in Germany, which may provide insight into the extent of the growing queue of patients affected by surgical delay.
METHODS
A retrospective analysis was conducted on elective spine cases performed at seven Schoen Clinic hospitals throughout Germany during the first 15 calendar weeks of 2019 and 2020. Weekly case volumes were compared across years using pairwise two-tailed t-tests, first on weeks 1–12 of both years to evaluate baseline differences, followed by weeks 13–15 to evaluate the effects of elective surgery restrictions on this endpoint. All statistical analyses and visualization were conducted using GraphPad Prism 8 (GraphPad Software, San Diego, CA). Because no patient data was involved, this investigation was exempt from review by our institutional review board (IRB).
RESULTS
During the first 12 weeks of the calendar year, total weekly spine cases were similar to those of 2019 (249.8 ± 66.7 versus 244.5 ± 54.5 weekly cases, P = .39). However, following the cessation of non-emergent cases from week 13 onward, weekly cases in 2020 became significantly less frequent compared to the same calendar weeks in 2019 (103.7 ± 6.7 vs. 283.0 ± 29.5, P = .01). These results are summarized in Table 1. In the immediate aftermath of restrictions on elective surgery, spine cases fell 64.4% below baseline (2019) expected levels, a trough that has persisted for the remaining weeks of the year to date. These trends are depicted in Figure 1.
TABLE 1.
Pair-wise comparison of spine cases per calendar week
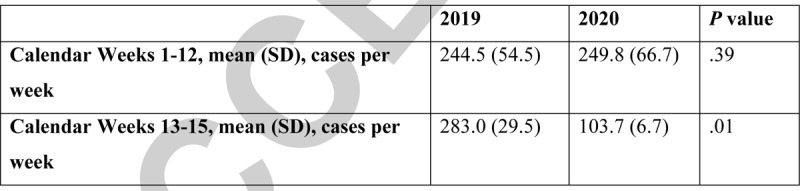
Figure 1.
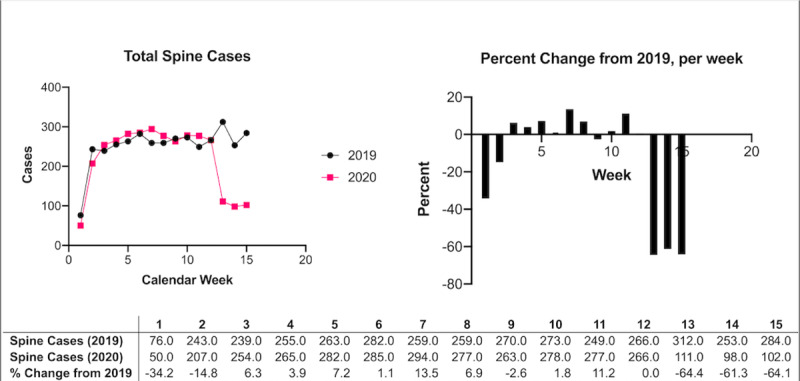
Spine cases performed at Schoen Clinic locations in 2019 and 2020.
DISCUSSION
While the diversion of hospital resources during this time may be warranted, it is important to understand the possible unintended ramifications of such actions that may later necessitate rectification. The reduction in “elective” spine procedures witnessed in the largest family owned hospital system in Germany illustrates the potential impact of surgical delay measures on this patient population, affecting over 60% of patients in this series who would have otherwise undergone necessary surgical intervention. Because patients with protracted symptom duration have been shown to have worse outcomes, in addition to higher complication, reoperation and readmission rates, the halt of these procedures for many months to come may result in tremendous additional costs for the healthcare system once restrictions are lifted.4 Moreover, the increased backlog of patients that results from the postponement of these surgeries may further increase wait times and duration of unresolved symptoms, even when restrictions are lifted. Patients may also be initially reluctant to return to the clinic or hospital setting, which may still carry COVID-19 patients, despite an availability of operating rooms.
The findings herein, however, are not without their limitations. Firstly, this is a single-center experience of a family-owned and managed institution, and thus may be parochial or clustered to this particular practice and may not fully generalizable to a larger German or international experience. We therefore caution against over-extrapolating the results of our analysis. Furthermore, at the time of publication, the world is still in the midst of the COVID-19 pandemic, in which daily changes in the prevalence of disease, and the policies that result, can often be sudden and unpredictable.
Footnotes
The manuscript submitted does not contain information about medical device(s)/drug(s).
No funds were received in support of this work.
No relevant financial activities outside the submitted work.
References
- 1.Givi B, Schiff BA, Chinn SB, et al. Safety Recommendations for Evaluation and Surgery of the Head and Neck During the COVID-19 Pandemic. JAMA Otolaryngol Neck Surg 2020; doi:10.1001/jamaoto.2020.0780. [DOI] [PubMed] [Google Scholar]
- 2.Martin BI, Mirza SK, Spina N, Spiker WR, Lawrence B, Brodke DS. Trends in Lumbar Fusion Procedure Rates and Associated Hospital Costs for Degenerative Spinal Diseases in the United States, 2004 to 2015. Spine 2019; 44 (5):369–376. doi:10.1097/BRS.0000000000002822. [DOI] [PubMed] [Google Scholar]
- 3.Cowan JA, Dimick JB, Wainess R, Upchurch GR, Chandler WF, La Marca F. Changes in the utilization of spinal fusion in the United States. Neurosurgery 2006; 59 (1):15–20. discussion 15-20. doi:10.1227/01.NEU.0000219836.54861.CD. [DOI] [PubMed] [Google Scholar]
- 4.Wagner SC, Butler JS, Kaye ID, Sebastian AS, Morrissey PB, Kepler CK. Risk Factors for and Complications After Surgical Delay in Elective Single-Level Lumbar Fusion. Spine 2018; 43 (3):228–233. doi:10.1097/BRS.0000000000002282. [DOI] [PubMed] [Google Scholar]
- 5.CDC. Coronavirus Disease 2019 (COVID-19) in the U.S. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html. Published April 17, 2020. Accessed April 19, 2020.
- 6.Weissman GE, Crane-Droesch A, Chivers C, et al. Locally Informed Simulation to Predict Hospital Capacity Needs During the COVID-19 Pandemic. Ann Intern Med 2020; doi:10.7326/M20-1260. [DOI] [PubMed] [Google Scholar]


