Purpose of review
The Covid-19 pandemic has daunted the world with its enormous impact on healthcare, economic recession, and psychological distress. Nutrition is an integral part of every person life care, and should also be mandatorily integrated to patient care under the Covid-19 pandemic. It is crucial to understand how the Covid-19 does develop and which risk factors are associated with negative outcomes and death. Therefore, it is of utmost importance to have studies that respect the basic tenets of the scientific method in order to be trusted. The goal of this review is to discuss the deluge of scientific data and how it might influence clinical reasoning and practice.
Recent findings
A large number of scientific manuscripts are daily published worldwide, and the Covid-19 makes no exception. Up to now, data on Covid-19 have come from countries initially affected by the disease and mostly pertain either epidemiological observations or opinion papers. Many of them do not fulfil the essential principles characterizing the adequate scientific method.
Summary
It is crucial to be able to critical appraise the scientific literature, in order to provide adequate nutrition therapy to patients, and in particular, to Covid-19 infected individuals.
Keywords: covid-19, nutrition, quality
KEY POINTS
Under the Covid-19 pandemic many studies have not fulfilled basic tenets of scientific methodology
The importance of nutrition therapy for Covid-19 patients has seldom been the topic of most published studies, despite its utmost relevancy in the holistic approach of any individual
The best patient care should mingle clinical reasoning and scientific knowledge
Massive deluge of publications may not necessarily mean good quality science
THE COVID-19 AND THE DELUGE OF PUBLICATIONS
The Covid-19 pandemic, began in late 2019, in Wuhan, China, followed by a rapid spread worldwide. This has daunted the world with an enormous impact on healthcare, economic recession, psychological distress, and many associated adverse events. Adequate nutrition is an integral part of every person care and should be integrated to the care of patients suffering from Covid-19. It is crucial to understand how the disease develops and what risk factors are associated with negative outcomes and death. Therefore, in order to reach conclusions, it is of utmost importance to carry out studies that respect the basic tenets of the scientific method, while being able to trust their results.
In the last years, the scientific community has been exposed to a huge increase in health scientific publications. Overall, nearly 20 million manuscripts have been reported in PubMed, with about one million defined as ‘clinical trials’ and almost two million as ‘reviews’, of which about 10% are systematic reviews [1]. This has not been different for the Covid-19 pandemic. As of today (April 13, 2020), a search in PubMed for the key word ‘covid-19’ provided 3810 results [2]; remarkably, none of them was classified as a clinical trial. When the word ‘nutrition’ was added, the results fell to 30. Considering that there are many intertwined cause/effects variables that may interfere with outcomes, which in statistics may imply collinearity, it is even more challenging for clinicians to interpret results.
RISK FACTORS, STATISTICS, AND ACCURATE RESULTS
Collinearity is a condition in which some of the independent variables are highly correlated, a situation that will eventually inflate the variance of at least one estimated regression coefficient, thus generating potential flawed or inflated results [3]. In regard to Covid-19 patients, it is known that death rates are increased among the elderly, as shown in particular in Italy [4]. Is this observation related to age alone? Or is it because this group of individuals have increased comorbidities, with polypharmacy as a rule which, together with social isolation make them more vulnerable to nutrition deficiencies? Adding to the confusion, smoking is still highly prevalent among the Chinese, Italian, and Iranian old people. On the other hand, smoking is not so prevalent in the United States of America where the disease has currently outnumbered other countries, with a reasonable number of young patients [5]. Could the U.S. pandemic and death rates among younger Americans be explained by the high obesity prevalence in that country [6]? Obesity is a chronic inflammatory state that may interfere with the acute immunologic response to the virus. Little is known about each one of the afore mentioned potential risk factors, and what role they play on individual populations.
A few years ago, John Ioannidis in a pivotal provocative paper – ‘How to survive he medical misinformation mess’ – addressed the deluge of scientific information [7], which affects not only physicians but also those in the healthcare field who should be thriving to adopt the best evidence practices in order to improve patient care. It is interesting to highlight that Ioannidis’ concerns about the quality of the scientific publications date back to 15 years ago, when he courageously stated that conclusions of most published research findings were false [8]. According to him, the majority of studies lacked methodological quality and were biased because of the absence of statistic power. He also depicted that most study designs and settings were flawed. Therefore, many research claims were more likely to be false than true. More recently, Ioannidis raised awareness to crucial topics that might interfere with the analysis of data pertaining to the Covid-19 pandemic [9▪]. In his opinion, data collected on how many people have been infected are unreliable because of the limiting testing, and death rates are flawed because of this limitation.
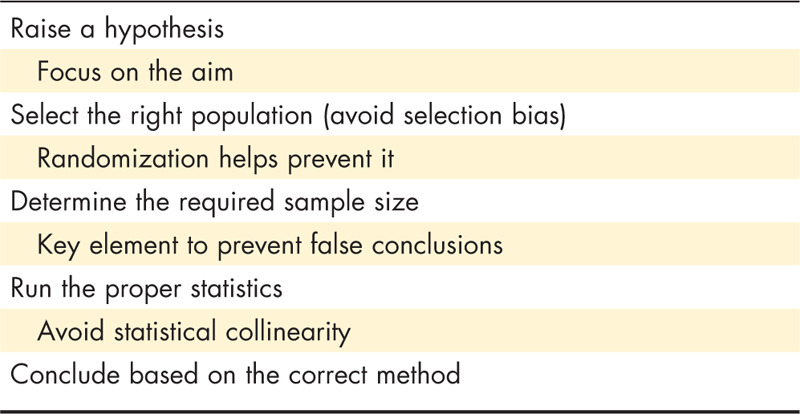
Under the Covid-19 pandemic, there has not been a random sample study to correctly indicate the disease prevalence, and the same applies to most studies pertaining interventions. In fact, sample size calculation, a key methodological principle, has not been regularly addressed by many authors, and the same flaw is the rule in most of the published papers regarding the Covid-19 disease. One may understand and even accept that such important requirement may not be fulfilled under the current pandemic as most data come from observational studies. Yet, it is mandatory to either calculate it a posteriori (post hoc) or to indicate the limitations because of its absence. The methodological quality of research is mandatory, and there are no excuses not to follow it. In fact, adequate sample size has been a major drawback when assessing clinical trials, which may lead to type II statistical errors. Because of this, many authors and institutions have relied on metanalysis to draw conclusions, which is also challenging considering the appropriateness and quality of such studies [1,10▪] (Table 1). Furthermore, significant concern has recently emerged: are clinical practitioners able to adequately read and critically appraise the scientific method, and thus the results and conclusions of the studies [11–13]?
Table 1.
The basic/adequate scientific method
THE COVID-19 AND NUTRITION
In the context of the Covid-19 pandemic, most patients suffering mild signs and symptoms, are treated at home, require symptomatic therapies, and a good healthy diet is recommended as it should be common practice for any individual based on the percepts of healthy living habits. Nonetheless, if the Covid-19 patients are at risk of malnutrition or malnourished, commonly among the elderly, nutrition supplements may help improve the nutritional status, similarly to at risk-patients with other diseases [14]. A minority of patients do require hospitalization, and less than 5% are admitted in the intensive care units. For these individuals, nutrition therapy should be integrated to the whole therapeutic approach, as for any critical care patient [15,16▪].
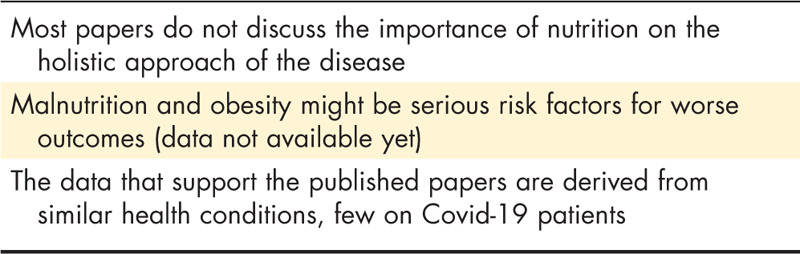
Some authors have published papers addressing nutrition care for Covid-19 patients [16▪,17,18,19▪▪,20,21], but with one exception [19▪▪], these are either editorials or based on information derived from different disease states. On the other hand and importantly, the majority of published manuscripts on Covid-19 do not mention the role of nutrition as an integral part of patient care, and the risks of associated burdens, such as obesity. The role of previous inadequate nutrition habits and behavior, two well known risk factors associated with malnutrition, which are also highly prevalent among the elderly, may cause significant impact on the outcomes of the Covid-19 patients. The latter in association with the many other risk factors, including the genetic background lead to excessive inflammation which increases morbidity and mortality (Table 2).
Table 2.
Covid-19 and nutrition
Rundle et al. [20] raise awareness to the possibility of long-term effect on children's health, because of the increased risk of obesity while schools are shut down. Luzi et al., on the basis of influenza derived data, advocate that overweight and obese individuals might have an increased risk of complications, because of the permanent inflammatory status as currently seen in the United States. Also, according to these authors, the appearance of a virulent viral strain maybe associated to obesity, and they indicate mild caloric restricted diets and weight loss, and AMPK activators and PPARγ activators as therapeutic approaches for obese and diabetic individuals [21]. On the other hand, such interventions may increase the risk of nutrition deficiencies because many obese people are hidden malnourished individuals [22]. Caccialanza et al. [16▪] present a pragmatic protocol for early nutrition supplementation of noncritically ill hospitalized patients; this is supported by the Italian observations that these patients, present with severe inflammation and anorexia, at admission, which cause drastic decrease of food intake, further impacted by olfactory and gustatory dysfunctions. In this regard, Lechien et al. [19▪▪] assessed 417 European patients with mild-to-moderate Covid-19 disease, and indicated that 85.6 and 88.0% of them reported olfactory and gustatory dysfunctions, respectively. Laviano et al. [18], in an editorial, raise attention to how nutrition is a determinant of health, and part of the treatment for acute and chronic diseases. They refer to the Ebola virus outbreak in 2014–2016, in Africa, for which immediate supportive care significantly reduced case fatalities. All these papers add numbers to the massive deluge of information; once again, most of them are experts’ opinions based on previous observations.
HOW TO INTERPRET THE DELUGE OF DATA?
Machine learning techniques, for example, random forests or decision trees, might be able to approach the diversity of data and predict outcomes as it has been seen for other disease conditions [23,24▪▪,25▪▪,26,27]. In the current pandemic, artificial intelligence has also been used [28,29]. Nonetheless, no matter how crucial these new data analyses may help solve controversies in healthcare sciences, it is important to highlight that numbers alone should not replace medical wisdom. It is of utmost importance to understand the biology and physiology behind the data, and namely, to have substantial experience with patients, and not only with numbers. On the other hand, the single use of experts’ opinions, even if supported by some evidence as those in guidelines, may be problematic [30]. However, one must acknowledge that the art of Medicine has been supported by the millennial use of aphorisms. One of Latham's aphorisms summarizes where lines cross between good science and the art of practicing medicine (or any other healthcare specialty):
’Medicine is a strange mixture of speculation and action. We have to cultivate science and exercise art. The calls of science are upon our leisure and our choice; the calls of practice are of daily emergence and necessity.’ [31]
Thus, clinical experience together with methodological knowledge are key to interpret research evidence and reach conclusions to be used into practice. The excellency of patient care requires practice by the bedside and knowledge to interpret data. Unfortunately, even guidelines (which many clinicians rely on to take decisions) do not fully acknowledge the poor quality of the data on which they are based, not to mention that sometimes, different recommendations are given within the same guideline [7]. Furthermore, many clinicians (and also guidelines) rely on meta-analyses, considered the highest level of evidence studies, to determine recommendations. Unfortunately, as previously mentioned such studies are also at risk of poor methodological control and quality [32▪▪,33▪▪,34,35].
Barnard et al. [36] have proposed that because meta-analyses, particularly those involving nutrition, influence health policies, and are frequently used by the media, with the potential to do more harm than good, the peer-review process should go beyond the meta-analytic method and include a series of quality control techniques. It is important to highlight that nutrition science novelties, either from epidemiological, experimental or clinical studies, are commonly favorite topics used by the lay media to attract attention, in ways that may jeopardize peoples’ health; this has not been different under the Covid-19 pandemic. Mostly, such news confers the benefits of miraculous treatments or discoveries, many not yet proven. The majority of medical articles in the lay media are based on inaccurate criteria, either maximizing benefits, while avoiding to mention potential harms [37].
THE LAY MEDIA AND SCIENCE
A group of reviewers from HealthNewsReview.org, many of whom physicians, assessed news reported by organizations in the United States of America regarding new medical treatments, tests, products, and procedures. The reviewers evaluated almost 2000 documents, of which 43% were newspaper articles, 30% wire or new services stories, 15% online material, and 12% network television stories. Most articles were rated unsatisfactory on five of 10 review criteria: costs, benefits, harms, quality of the evidence, and comparison of the new approach with alternatives. It is noteworthy that medical devices, medications, and other interventions were usually reported positively, while potential harms were minimized, and costs not indicated [37]; similar patterns are found in some of the proposed Covid-19 treatments [38]. In fact, the overwhelming number of scientific publications has created a similar awkward situation in healthcare sciences, which is further powered by the boom of scientific journals, questionable review processes, and inadequate metrics [39–41]. Has this resulted in increased wisdom? Unfortunately, not!
THE PRACTICE OF MEDICINE AND SCIENCE
The importance of individualized medicine, the abidance by ethical principles, and the art of diagnostics, together with realistic prognostication, have their roots in the Hippocratic tradition, which seems to have been neglected in the modern era (Fig. 1). And, by the way, one of the many Hippocrates aphorisms regarded weight loss and cognitive impairment as death predictors [31,42], which are two well known risk factors for malnutrition [43,44]. Therefore, the best patient care should mingle clinical reasoning and scientific knowledge, and the latter requires adequate methods. In summary: raise an hypothesis; present its rationale; thoroughly describe the methods (as a cake recipe), include the sample size that will allow the proper interpretation of the results; present the findings (results) with details and not as mere numbers but with logic statistical significance; and then focus on the discussion of what was found, comparing it to data from other authors, leaving room for limitations and perspectives.
FIGURE 1.
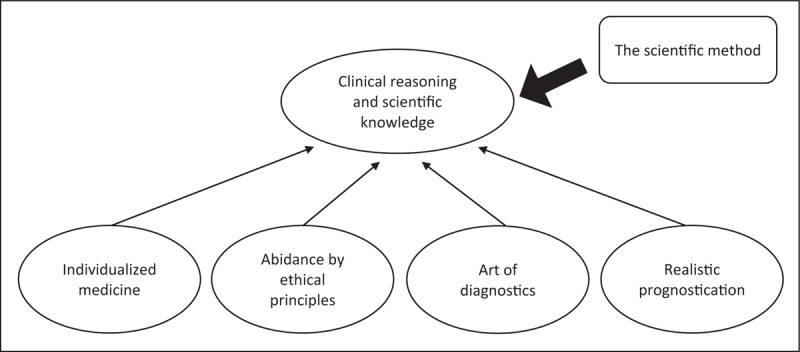
The practice of medicine and science.
CONCLUSION
Finally, it is commonly believed that under critical situations there is a potential for the emergence of a better future. In this regard, raising awareness to the need for adequate scientific methods, and, for better-quality report and assessment might improve messages delivered by science and potentially impact patient care. Afterall, the science of ‘guesswork’ was long ago challenged by Descartes.
Acknowledgements
None.
Financial support and sponsorship
None.
Conflicts of interest
None.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Ioannidis JP. The mass production of redundant, misleading, and conflicted systematic reviews and meta-analyses. Milbank Q 2016; 94:485–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pubmed.gov [Internet]. 2020. https://www.ncbi.nlm.nih.gov/pubmed/?term=%22covid-19%22.
- 3.Ardalan ZS, Sparrow MP, Muir JG, Gibson PR. Dietary fat and the faecal microbiome: where collinearity may lead to incorrect attribution of effects to fat. Gut 2019; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 4.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020; 395:1054–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Control CfD. Coronavirus Disease 2019 (COVID-19) – cases in the US 2020 [updated April, 15, 2020]. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html.
- 6.Hales CM, Fryar CD, Carroll MD, et al. Trends in obesity and severe obesity prevalence in us youth and adults by sex and age, 2007–2008. JAMA 2018; 319:1723–1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ioannidis JPA, Stuart ME, Brownlee S, Strite SA. How to survive the medical misinformation mess. Eur J Clin Invest 2017; 47:795–802. [DOI] [PubMed] [Google Scholar]
- 8.Ioannidis JP. Why most published research findings are false. PLoS Med 2005; 2:e124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9▪.Ioannidis JPA. A fiasco in the making? As the coronavirus pandemic takes hold, we are making decisions without reliable data Statnew: Boston Globe; 2020. https://www.statnews.com/2020/03/17/a-fiasco-in-the-making-as-the-coronavirus-pandemic-takes-hold-we-are-making-decisions-without-reliable-data/?fbclid=IwAR0r5W-fu7C4Qi19bUdiW_ekgbTu6HpP98xx5BBaZjL1bZn5QjIvaVbm3yc.; The authors challenges data pertaining the current pandemic.
- 10▪.Correia M. Are we capable of separating the wheat from the chaff when assessing meta-analyses? Clin Nutr 2020; 39:705–707. [DOI] [PubMed] [Google Scholar]; A critical appraisal of meta-analyzes.
- 11.Bellomo R, Bagshaw SM. Evidence-based medicine: classifying the evidence from clinical trials--the need to consider other dimensions. Crit Care 2006; 10:232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ioannidis JPA. Hijacked evidence-based medicine: stay the course and throw the pirates overboard. J Clin Epidemiol 2017; 84:11–13. [DOI] [PubMed] [Google Scholar]
- 13.Ioannidis JPA. Randomized controlled trials: often flawed, mostly useless, clearly indispensable: a commentary on Deaton and Cartwright. Soc Sci Med 2018; 210:53–56. [DOI] [PubMed] [Google Scholar]
- 14.Waitzberg DL, De Aguilar-Nascimento JE, Dias MCG, et al. Hospital and homecare malnutrition and nutritional therapy in Brazil. Strategies for alleviating it: a position paper. Nutr Hosp 2017; 34:969–975. [DOI] [PubMed] [Google Scholar]
- 15.Singer P, Blaser AR, Berger MM, et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nutr 2019; 38:48–79. [DOI] [PubMed] [Google Scholar]
- 16▪.Caccialanza R, Laviano A, Lobascio F, et al. Early nutritional supplementation in noncritically ill patients hospitalized for the 2019 novel coronavirus disease (COVID-19): Rationale and feasibility of a shared pragmatic protocol. Nutrition 2020; 110835.[Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]; Indications for noncritical Covid-19 patients based on previous disease states.
- 17.Joob B, Wiwanitkit V. COVID-19, school closings and weight gain. Obesity (Silver Spring) 2020; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 18.Laviano A, Koverech A, Zanetti M. Nutrition support in the time of SARS-CoV-2 (COVID-19). Nutrition 2020; 110834.[Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19▪▪.Lechien JR, Chiesa-Estomba CM, De Siati DR, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Otorhinolaryngol 2020; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]; Observational study with Covid-19 assessing olfactory and gustatory dysfunction.
- 20.Rundle AG, Park Y, Herbstman JB, et al. COVID-19 related school closings and risk of weight gain among children. Obesity (Silver Spring) 2020; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Luzi L, Radaelli MG. Influenza and obesity: its odd relationship and the lessons for COVID-19 pandemic. Acta Diabetol 2020; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gonzalez MC, Correia M, Heymsfield SB. A requiem for BMI in the clinical setting. Curr Opin Clin Nutr Metab Care 2017; 20:314–321. [DOI] [PubMed] [Google Scholar]
- 23.Lundberg SM, Nair B, Vavilala MS, et al. Explainable machine-learning predictions for the prevention of hypoxaemia during surgery. Nat Biomed Eng 2018; 2:749–760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24▪▪.Panaretos D, Koloverou E, Dimopoulos AC, et al. A comparison of statistical and machine-learning techniques in evaluating the association between dietary patterns and 10-year cardiometabolic risk (2002-2012): the ATTICA study. Br J Nutr 2018; 120:326–334. [DOI] [PubMed] [Google Scholar]; A machine learning model to assess the risk of hypoxemia while undergoing anesthesia.
- 25▪▪.Cobb AN, Daungjaiboon W, Brownlee SA, et al. Seeing the forest beyond the trees: predicting survival in burn patients with machine learning. Am J Surg 2018; 215:411–416. [DOI] [PMC free article] [PubMed] [Google Scholar]; A machine learning statistical model to compare the association between dietary patterns and a 10-year risk of cardiometabolic risk.
- 26.Ribeiro M, Guestrin C, Singh S. Are Red Roses Red? Evaluating consistency of question-answering models. Association for Computational Linguistics:Florence, Italy:2019. [Google Scholar]
- 27.Mortazavi BJ, Bucholz EM, Desai NR, et al. Comparison of machine learning methods with national cardiovascular data registry models for prediction of risk of bleeding after percutaneous coronary intervention. JAMA Netw Open 2019; 2:e196835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alimadadi A, Aryal S, Manandhar I, et al. Artificial intelligence and machine learning to fight COVID-19. Physiol Genom 2020; 52:200–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tarnok A. Machine Learning, COVID-19 (2019-nCoV), and multi-OMICS. Cytometry A 2020; 97:215–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.[30] Rada G. What is the best evidence and how to find it?: BMJ Best Practice. https://bestpractice.bmj.com/info/toolkit/discuss-ebm/what-is-the-best-evidence-and-how-to-find-it/.
- 31.Chandler ET, Bloomfield RL. Aphorisms: wisdom for all seasons. South Med J 1987; 80:84–89. [DOI] [PubMed] [Google Scholar]
- 32▪▪.Flegal KM, Ioannidis JPA, Doehner W. Flawed methods and inappropriate conclusions for health policy on overweight and obesity: the Global BMI Mortality Collaboration meta-analysis. J Cachexia Sarcopenia Muscle 2019; 10:9–13. [DOI] [PMC free article] [PubMed] [Google Scholar]; The authors discuss the flawed and inappropriate methods that have been used to address health policy on overweight and obesity regarding mortality
- 33▪▪.Schuit E, Li AH, Ioannidis JPA. How often can meta-analyses of individual-level data individualize treatment? A meta-epidemiologic study. Int J Epidemiol 2019; 48:596–608. [DOI] [PubMed] [Google Scholar]; This is a meta-epidemiologic study to indicate how often meta-analyzes can be used for individualize treatments
- 34.Siontis KC, Ioannidis JPA. Replication, duplication, and waste in a quarter million systematic reviews and meta-analyses. Circ Cardiovasc Qual Outcomes 2018; 11:e005212. [DOI] [PubMed] [Google Scholar]
- 35.Moller MH, Ioannidis JPA, Darmon M. Are systematic reviews and meta-analyses still useful research? We are not sure. Intensive Care Med 2018; 44:518–520. [DOI] [PubMed] [Google Scholar]
- 36.Barnard ND, Willett WC, Ding EL. The misuse of meta-analysis in nutrition research. JAMA 2017; 318:1435–1436. [DOI] [PubMed] [Google Scholar]
- 37.Schwitzer G. A guide to reading healthcare news stories. JAMA Intern Med 2014; 174:1183–1186. [DOI] [PubMed] [Google Scholar]
- 38.Zhang L, Liu Y. Potential interventions for novel coronavirus in China: a systematic review. J Med Virol 2020; 92:479–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Diamandis EP. The Journal Impact Factor is under attack - use the CAPCI factor instead. BMC Med 2017; 15:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gasparyan AY, Nurmashev B, Yessirkepov M, et al. The journal impact factor: moving toward an alternative and combined scientometric approach. J Korean Med Sci 2017; 32:173–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Karabulut N. Inaccurate citations in biomedical journalism: effect on the impact factor of the American Journal of Roentgenology. AJR Am J Roentgenol 2017; 208:472–474. [DOI] [PubMed] [Google Scholar]
- 42.St John PD, Montgomery PR. Utility of Hippocrates’ prognostic aphorism to predict death in the modern era: prospective cohort study. BMJ 2014; 349:g7390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cederholm T, Jensen GL, Correia M, et al. GLIM criteria for the diagnosis of malnutrition – a consensus report from the global clinical nutrition community. Clin Nutr 2019; 38:1–9. [DOI] [PubMed] [Google Scholar]
- 44.Correia M, Perman MI, Waitzberg DL. Hospital malnutrition in Latin America: a systematic review. Clin Nutr 2017; 36:958–967. [DOI] [PubMed] [Google Scholar]


