Abstract
Background:
Overburdened systems and concerns of adverse outcomes have resulted in deferred cancer surgeries with devastating consequences. In this COVID pandemic, the decision to continue elective cancer surgeries, and their subsequent outcomes, are sparsely reported from hotspots.
Methods:
A prospective database of the Department of Surgical Oncology was analysed from March 23rd to April 30th, 2020.
Findings:
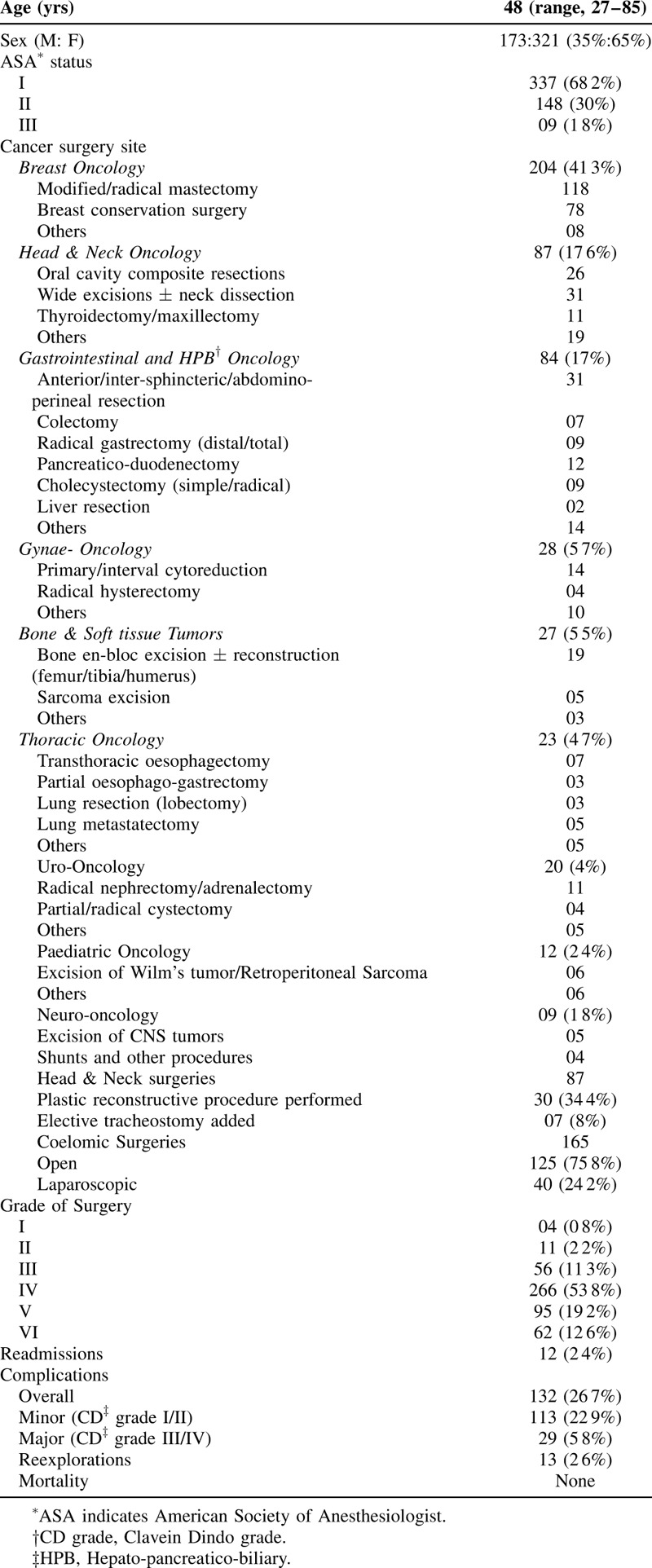
Four hundred ninety-four elective surgeries were performed (377 untested and 117 tested for Covid 19 before surgery). Median age was 48 years with 13% (n = 64) above the age of 60 years. Sixty-eight percent patients were American Society of Anaesthesiology (ASA) grade I. As per surgical complexity grading, 71 (14·4%) cases were lower grade (I-III) and 423 (85.6%) were higher grade complex surgeries (IV – VI).
Clavien-Dindo ≥ grade III complications were 5.6% (n = 28) and there were no postoperative deaths. Patients >60 years documented 9.3% major complications compared to 5.2% in <60 years (P = 0.169). The median hospital stay was 1 to 9 days across specialties.
Postoperatively, 26 patients were tested for COVID 19 and 6 tested positive. They all had higher grade surgeries but none required escalated or intensive care treatment related to COVID infection.
Interpretation:
A combination of scientific and administrative rationale contributed to favorable outcomes after major elective cancer surgeries. These results support the continuation of elective major cancer surgery in regions with Covid 19 trends similar to India.
Keywords: cancer care, cancer surgery, Covid 19, oncologic surgery, outcomes, pandemic
Health systems have been under duress due to pandemic caused by SARS coronavirus 2 (SARS-CoV-2). Based on information suggesting that India was faring better compared to the west1 and that oncology patients were likely to get deferred care with significant implications,2 the department of surgical oncology took a conscious decision to continue offering elective cancer surgeries albeit deescalated by approximately 50% (and continues to do so till date of submission of manuscript). Outcome data of elective cancer resections are sparsely reported from Covid hotspots around the world. We aimed to analyze and report outcomes of 494 elective cancer surgeries and discuss the implications of our decision.
METHODS
A prospective database of the Department of Surgical Oncology was analysed from March 23rd to April 30th, 2020.
Screening and Selection of Patients for Surgery
Patients likely to benefit from potentially curative cancer surgery were given the highest priority. Younger patients with fewer comorbidities were preferred.
Asymptomatic patients were not tested preoperatively for COVID 19 unless there was history of contact or international travel in the initial part of the study (23rd March – 18th April 2020). In the last 2 weeks of the study (19th – 30th April) with increasing concern of community spread, routine preoperative COVID 19 testing was instituted. The test was performed on nasopharyngeal and the oropharyngeal swabs by TaqMan probe-based real-time reverse transcriptase polymerase chain reaction (RT-PCR) method. Irrespective of preoperative testing, all patients were considered as COVID positive and the operating room staff had to adhere to full precautions.
Data Recording and Analysis
The electronic clinical data were reviewed and documented. Surgeries were graded (grade I - grade VI) with increasing surgical complexity. All perioperative parameters were documented in detail. Statistical analyses was performed using Statistical Product and Service Solutions (SPSS), IBM Corp, for Windows version 21·0, (SPSS Inc, Armonk, NY). Descriptive analysis was performed to identify distribution of variables under study and continuous variables were presented as median with interquartile range.
The study was approved by the Institutional Ethics Committee.
RESULTS
During the study period, 520 surgeries were performed of which 494 (95%) cases were elective surgeries whereas 26 (5%) were emergency surgeries. Demographic and operative outcomes are provided in Table 1.
TABLE 1.
Patient Characteristics, Surgical Procedures, and Overall Postoperative Outcomes (n = 494)
Of all patients undergoing elective surgery, 181 (36 6%) were residents of Mumbai or Maharashtra state and rest from other parts of India (63.4%).
As per the surgical complexity grading, 71 (14 4%) cases were of lower grade (I-III) and 423 (85 6%) were higher grade surgeries (IV–VI). Breast cancer surgeries constituted 41.3% (n = 205), followed by head and neck (87 cases; 17.6%) and GI cancer surgeries (84 cases; 17%). Plastic reconstructive procedures were required in 34.4% of the Head & Neck resections. Postoperative major morbidity (Clavein Dindo grade ≥III) occurred in 28 (5 6%) patients and there were no deaths. Perioperative outcomes across cancer sites are presented in Table 2. Sixty-four patients were above 60 years age, of which 9.3% developed major complications compared to 5.2% in <60 years (P value =0.169). Grade IV to VI surgeries accounted for more than 85% of cases in both groups.
TABLE 2.
Perioperative Details and Outcomes According to Cancer Site
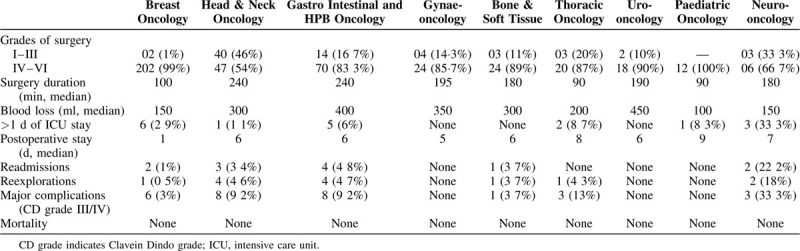
None of the patients undergoing surgery had clinical suspicion for COVID 19, based on symptoms or contact history, and initial 377 surgeries were performed without any testing. One hundred seventeen surgeries were carried out after testing for subclinical COVID 19 infection. Postoperatively, 26 patients were tested in view of specific symptoms or contact history from the community (to patients or their kins) and 6 tested positive. All these patients had undergone grade IV to VI surgeries (Buccal mucosa composite resection - 3, total thyroidectomy with neck dissection - 1, pancreatico-duodenectomy - 1, distal femur resection with total knee replacement - 1). None of these patients required escalated or intensive care treatment related to COVID infection. All of them recovered well from surgery and COVID infection.
DISCUSSION
The reasons for our decision to continue elective major cancer surgery were not easy. Mumbai, is currently rated as a COVID 19 hotspot. The population of Mumbai is approximately 21 million with a population density of 21,000 people per square kilometre.3 It is pertinent to note that despite good testing rates (1221/million, the mortality rate in Mumbai is 4.24/million population.4 There are about one million new cancer cases in India,5 of which around 0.2 million will require surgery. In the absence of surgery, most patients will experience disease progression with resultant mortality. Given that death due to COVID-19 in India is 0.99 per million of population with case fatality rate of about 3%,1 the cancer mortality in absence of definitive surgery will far exceed the mortality due to infection with COVID-19.
These observations, coupled with patients prebooked for surgery - a number of them from outside of Mumbai under national lockdown – was compelling enough to continue elective major cancer surgeries.6
Decisions for individual patients were made by balancing the risk that patients will contract Covid-19 because of hospitalization and subsequent cancer surgery and their potential for associated complications, with the benefits of receiving potentially curative cancer surgery.
Our results reflect a cautious approach adopted initially that has gradually widened in scope with increasing confidence. Breast cancer surgeries, gastrointestinal cancer resections, and head and neck surgeries accounted for over 76 percent of our resections. Head and neck cancer surgeries, traditionally registering the highest number of resections, recorded a modest number once again reflecting a safety first approach. The service is now scaling up their efforts with increasing availability of operating rooms and increasing confidence of operating room teams with specialized protection and stringent standard operating procedures compared to other services.
The median age of 48 years, the majority with American Society of Anaesthesiology (ASA) grades 1 and 2, confirm our policy decision of offering elective cancer surgeries to “low risk” patients as far as possible. However, there was no difference in morbidity and mortality when patients over 60 years were compared to those younger than 60 years of age.
Our low rates of major complications and zero mortality in this series 494 resections over 5 weeks not only reflects our “‘Covid 19 centric policy” of case selection, adopting best surgical practices and having the best operating teams (average age 40 years) led by senior consultants (with an average age of 48 years) but also confirm that there were no deviations from earlier benchmarks established by the various surgical specialties in the pre-Covid era.7–10
Also, all 6 patients detected with COVID infection in the postoperative period, did not develop any major complication with uneventful recovery. Although a small number, all of them had undergone major resections. Thus magnitude of surgery did not affect their recovery in the presence of a potentially sinister infection.
The various overall outcome measures – specifically intensive care unit stay, major morbidity and mortality – seem to validate our scientific and administrative rationale for continuing elective cancer surgeries in a referral centre.
Our strategy may well be applicable to regions where mortality is less than 10/million population (such as China, Japan, Russia, South Korea, Australia, Saudi Arabia, Singapore etc) but may not be applicable for countries like USA with high number of COVID-19 cases (3498 per million) and a high death rate.
Although our results possibly represent the largest series published on elective cancer surgeries during the ongoing pandemic, there are certain limitations to this study. Not all patients and the staff associated with their treatment delivery were tested preoperatively. The possibility of asymptomatic carriers remains a concern; however all have been monitored closely even after discharge from the hospital and outcome measures for patients and staff alike have been very encouraging. The applicability of our experience to the larger population of patients, especially the elderly and those with comorbidities is yet to be fully established. Finally, the prevalence of COVID-19 in India could have been truncated to a large extent by the national lockdown, and the trajectory of infection rates after restrictions are lifted is as yet, unknown.
CONCLUSIONS AND FUTURE PERSPECTIVES
Cancer surgeons are currently facing a dilemma. Whereas world awaits definitive treatment options, new information about the virus will continue to impact decisions.11 Our results would not only serve as a springboard for a good action plan for nations with a pandemic profile similar to that of India, but also help resolve the conundrum of continuing cancer surgeries in health systems worldwide. We believe this would ultimately result in development of guidelines for continuation of elective major cancer surgery in a world that may well have to learn to live with COVID 19. The philosophy that regardless of COVID 19, cancer centres and specialists are available to care for their patients, should gain ground as we attempt to move ahead in this pandemic.12
ACKNOWLEDGMENTS
Dr. Rajesh Dikshit, Director, Centre for Cancer Epidemiology, Mrs. Swapna Joshi, Professor and Nursing Superintendent, Mrs. Sindhu Nair, Assistant Nursing Superintendent, Sister Veena Prakash Thorat, Operating Theatre in charge, Mr. Mangesh Kadam, CSSD (Central Sterile Supply Department), Mrs. Nishu Goel and her team of Kevats (patient navigators) and all our fearless and dedicated operating room, intensive care staff and resident doctors of the Tata Memorial Centre, Mumbai.
Footnotes
The authors report no conflicts of interest.Each author has contributed sufficiently for construction of this manuscript.
Shrikhande SV - Conception and design, interpretation of data, drafting the article or revising it critically, final approval of the version.
Pai PS, Bhandare MS, Bakshi G, Chaukar DA, Chaturvedi P, Goel M, Gulia A, Qureshi SS, Maheshwari A, Moiyadi AA, Nair S, Nair NS, Karimundackal George, Saklani AP, Shankhadhar VK, Parmar V, Divatia JV, Pramesh CS, Puri A - Interpretation of data, drafting the article or revising it critically.
Badwe RA - interpretation of data, drafting the article or revising it critically, final approval of the version.
∗Collaborators (48): Ajay Puri1, Aliasgar Moiyadi1, Amita Maheshwari1, Ashish Gulia1, Ashwin deSouza1, Avanish Saklani1, Deepa Nair1, Devayani Niyogi1, Devendra Chaukar1, Shylasree TS1, Anuja Deshmukh1, Prathamesh S. Pai1, Dushyant Jaiswal1, Gagan Prakash1, Ganesh Bakshi1, Garvit Chitkara1, George Karimundackal1, Gouri Pantvaidya1, Jitender Rohila1, Mahendra Pal1, Mahesh Goel1, Manish Bhandare1, Mayur Mantri1, Nita Nair1, Pabashi Poddar1, Pankaj Chaturvedi1, Poonam Joshi1, Prakash Nayak1, Prakash Shetty1, Pramesh CS1, Purvi Thakkar1, Rajendra A. Badwe1, Richa Vaish Mahajan1, Sabita Jiwnani1, Sajid S. Qureshi1, Saumya Mathews1, Shailesh V. Shrikhande1, Shalaka Joshi1, Shiva Kumar1, Shraddha Patkar1, Sudhir Nair1, Vani Parmar1, Vidisha Tuljapurkar1, Vikas Singh1, Vikram A. Chaudhari1, Vinay Kant Shankhdhar1, Virendra Tiwari1, Vijaya P. Patil2.
1Department of Surgical Oncology, Tata Memorial Hospital, Homi Bhabha National Institute, Ernest Borges Marg, Parel, Mumbai 400012, India.
2Department of Anaesthesiology, Critical Care and Pain, Tata Memorial Hospital, Homi Bhabha National Institute, Ernest Borges Marg, Parel, Mumbai 400012, India.
REFERENCES
- 1. Retrieved from http://www.emedinexus.com/post/17753/. [Accessed May 7, 2020] [Google Scholar]
- 2. The Lancet Oncology. COVID-19: global consequences for oncology. Lancet Oncol. 2020;21:467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Retrieved from https://indiapopulation2020.in/population-of-mumbai-2020.html. [Accessed May 7, 2020] [Google Scholar]
- 4. Retrieved from https://www.covid19india.org/state/MH. [Accessed May 7, 2020] [Google Scholar]
- 5.Dhillon PK, Mathur P, Nandakumar A, et al. The burden of cancers and their variations across the states of India: the Global Burden of Disease Study 1990-2016. Lancet Oncol 2018; 19:1289–1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pramesh CS, Badwe RA. Cancer management in India during Covid-19. N Engl J Med 2020; 382:e61.doi:10.1056/NEJMc2011595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gupta S, Maheshwari A, Parab P, et al. Neoadjuvant chemotherapy followed by radical surgery versus concomitant chemotherapy and radiotherapy in patients with stage IB2, IIA, or IIB squamous cervical cancer: a randomized controlled trial. J Clin Oncol 2018; 36:1548–1555. [DOI] [PubMed] [Google Scholar]
- 8.Shrikhande SV, Shinde RS, Chaudhari VA, et al. Twelve hundred consecutive pancreato-duodenectomies from single centre: impact of centre of excellence on pancreatic cancer surgery across India. World J Surg 2019; doi: 10.1007/s00268-019-05235-0. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 9.D’Cruz AK, Vaish R, Kapre N, et al. Elective versus therapeutic neck dissection in node-negative oral cancer. N Engl J Med 2015; 373:521–529. [DOI] [PubMed] [Google Scholar]
- 10.Puri A, Byregowda S, Gulia A, et al. A study of 853 high grade osteosarcomas from a single institution—are outcomes in Indian patients different? J Surg Oncol 2018; 117:299–306. [DOI] [PubMed] [Google Scholar]
- 11. Coccolini F, Tartaglia D, Puglisi A, Lodato M, Chiarugi M. SARS-CoV-2 is present in peritoneal fluid in COVID-19 patients. Annals of Surgery. Retrieved from https://journals.lww.com/annalsofsurgery/Documents/SARS-CoV-2%20is%20present%20in%20peritoneal%20fluid%20in%20COVID-19%20patients.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosenbaum L. The untold toll—the pandemic's effects on patients without Covid-19. N Engl J Med 2020; (published online April 17.). [DOI] [PubMed] [Google Scholar]


