Abstract
Background
The COVID-19 crisis has brought many unique challenges to the healthcare system. Across the United States, social distancing measures have been put in place, including stay-at-home orders (SAH), to combat the spread of this infection. This has impacted the type and volume of traumatic injuries sustained during this time. Meanwhile, steps have been taken in our healthcare system to assure that adequate resources are available to maintain a high standard of patient care while recognizing the importance of protecting healthcare providers. Using comparative data, we aim to describe the trends in traumatic injuries managed by our Plastic Surgery service and detail the changes in consultation policies made to minimize provider exposure.
Methods
A retrospective chart review was performed of all plastic surgery emergencies at our institution during the 3 weeks preceding the issuance of SAH orders in Chicago and the 3 weeks following. The electronic medical record was queried for patient age, type and mechanism of injury, location where injury was sustained, presence of domestic violence, length of inpatient hospital stays and treatment rendered. The two 3-week periods were then comparatively analyzed to determine differences and trends in these variables. and treatment rendered. The two periods were then comparatively analyzed to determine differences and trends in these variables.
Results
There was a significant decrease in trauma consults since issuance of SAH (88 pre-SAH vs 62 post-SAH) with a marked decrease in trauma related hand injuries. There was an increase in the percentage of assault-related injuries including those associated with domestic violence, while there was an overall decrease in motor vehicle collisions. There was no notable change in the location where injuries were sustained. Significantly fewer patients were seen by house staff in the emergency room, while those requiring surgical intervention were able to receive care without delay.
Conclusion
Stay-at-home orders in Chicago have impacted traumatic injury patterns seen by the Section of Plastic and Reconstructive Surgery at a Level I Trauma Center. Safe and timely care can continue to be provided with thorough communication, vigilance and guidance from our colleagues.
Introduction
On March 13, 2020, the United States declared a National Emergency in response to the outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative virus of coronavirus disease (COVID-19). Shortly thereafter, many states issued stay-at-home orders (SAH) to curtail the interactions of people in an effort to prevent the spread of the virus. Schools and non-essential businesses across the country were closed, major sporting and entertainment events were cancelled or postponed.
Social distancing has dramatically changed the way people interact and has decreased the number of people aggregating in public spaces on an unprecedented scale, not seen in recent times. Working from home has obviated the need to commute for many people, which has resulted in a significant decrease in highway traffic in major US cities.1 Restricting the mobility within a population has the potential to impact common sources of traumatic injuries.
While strict adherence to stay at home orders could, in theory, reduce the incidence of certain mechanisms of trauma (e.g. motor vehicle collisions), it also has the potential to create new mechanisms or exacerbate existing ones. According to media reports, the incidence of domestic violence has surged since SAH were put into place. In Chicago, Illinois, specifically, the domestic violence hotline experienced a 12.1% increase in domestic violence calls in the week after Governor Pritzker issued the SAH from March 23 to 29, 2020 compared to the same week in March 2019.2
The impact of COVID-19 on affected healthcare systems around the world has been well documented in the media. Hospital resources are being redistributed to deal with the additional burden presented by the surge of critically ill patients. Non-essential or elective surgeries are being postponed to allow for allocation of personal protective equipment (PPE) to healthcare workers directly treating patients afflicted with COVID-19. What is less well documented is the impact of the virus on the type and volume of traumatic injuries usually treated at the hospital. In addition, few consensus guidelines exist for the protection of healthcare workers managing trauma patients whose infection status is unknown.
Plastic surgeons have an integral role in an urban Level I Trauma Center.3 At the University of Chicago, the Section of Plastic and Reconstructive Surgery receives an average of more than 50 hand and face-related trauma consults per month. These range from simple lacerations to high acuity ballistic and blunt injuries from gunshot wounds and motor vehicle collisions, respectively. The aims of this study are to describe the changes in consultation patterns for plastic surgery traumatic injuries since the issuance of SAH and to describe the steps that have been taken to minimize potential provider exposure.
Methods
We performed a retrospective review of all trauma patients receiving consultation for plastic surgery emergencies, excluding burn consultations, at the University of Chicago Medical Center and the Comer Children’s Hospital from March 1, 2020 through April 11, 2020. Patients presenting with mainly burn injuries were excluded. This six-week period of interest was broken up into two separate three-week groups. The first three-week group, March 1 – 21, represents the time period before SAH were implemented. The second three-week group, March 22 – April 11, represents the time following the initiation of the official SAH in Illinois on March 21, 2020 at 5:00 PM.
The electronic medical record was queried for patient age, gender, race, type of injury, mechanism of injury, location where injury was sustained, presence of domestic violence, length of inpatient hospital stay, and treatment rendered. Data collected for admission and length of stay was not exclusively based on injuries managed solely by the Plastic Surgery service. Patients with hand and facial trauma often have sustained additional injuries that affect their length of stay. Some patients sustained both hand and facial trauma, which were counted as separate injuries. Patient consultations were included even in the rare situation where they were found to be without pathologic diagnosis. Comparisons were made between the first three-week time period and the second three-week period. Data was comparatively analyzed to determine differences and trends in these variables across weeks.
The study was conducted at the University of Chicago Medical Center and was reviewed and approved by the Institutional Review Board of the University of Chicago.
Protocols
Resident Schedule & Routine Modification
The PRS resident schedules were modified in order to ensure adequate availability of residents and providers in the event of exposure and illness. Two separate teams of residents were created with Junior and Senior level representation. Each team worked alternate weeks. In the event that a member or whole team were to become ill, the second team would act as a back-up and fill in as needed. Additional back-up residents were assigned as a level of redundancy.
Daily rounding was modified such that the team no longer rounded together, but rather that a single provider (senior resident or attending) would see each patient as needed. Following rounds, sign-out was given to other members of the team via phone call or video conference. In person communication was limited as much as possible to ensure social distancing within the team. Throughout the day, communication was a point of emphasis given potential issues with team members operating from a distance, and residents and attendings were encouraged to discuss patients virtually as a group at a minimum of two times per day.
Emergency Department Protocols
Consultation policies were amended in order to minimize time in the Emergency Department (ED) and limit potential staff and patient exposure to infection. Whenever possible, a single resident was assigned to see a consultation. Residents were encouraged to plan ahead for any potential procedures. Pictures were requested of any complex wound which may require closure in order to bring materials (sutures, local anesthetic, splint materials etc.) and prevent multiple visits to, and minimize time in the emergency room.
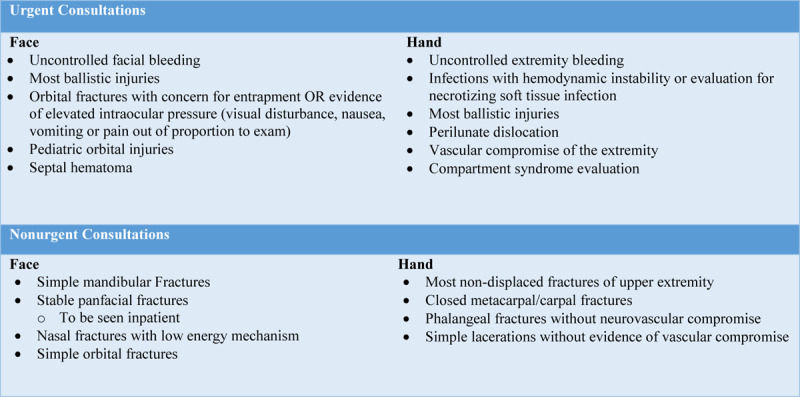
Consults were triaged by protocols established by consensus within the Section of Plastic and Reconstructive Surgery. These protocols were created with consideration for patient safety and provider security, as well as conservation of PPE. Traumatic injuries range widely in acuity and not all require immediate attention by a PRS provider. All non-urgent consultations which eventually require admission to the hospital were seen once the patient arrives in their unit. Urgent consultations, which were to be seen immediately, are summarized in Table 1. Injuries deemed nonurgent were triaged to the outpatient clinic or seen during inpatient hospital admission. Any discrepancies or questions were handled by the attending on call for the day in conjunction with the ED provider.
Table 1.
Summary of urgent consultations seen in the Emergency Department and nonurgent consultations which can be triaged to either outpatient clinics or be seen during inpatient hospital admission.
COVID-19 PATIENTS & PATIENT UNDER INVESTIGATION (PUI) PROTOCOLS
While all trauma consultations are routinely triaged at a high level of care, consultations with patients who are either known COVID-19 positive or patients under investigation (PUI) are treated with particular care. Any consultation in this patient group was discussed with the senior resident with frequent involvement of the attending on call. Specifically, the team and the consulting service together determined if the patient could be triaged remotely. A discussion followed regarding the patient’s ability to undergo surgical intervention. If it is determined that a surgical intervention would not benefit the patient or would not likely change the clinical outcome in the acute setting, the in-person consult would be deferred until after the patient recovered from the illness.
Results
A total of 150 hand and facial trauma consults were received between March 1 and April 11, 2020. Of those, 88 were received during the 3 weeks preceding the implementation of SAH in Illinois on March 21, and 62 were received in the 3 weeks following. This represents a decrease in average per day consults of 4.2 to 2.9 or a 29.5% overall decrease on volume (Table 2). There was a decrease in hand injuries (54 vs. 28), while the number of facial trauma injuries remained almost unchanged (37 vs. 33). There was no significant change in the percentage of trauma patients transferred to the University of Chicago Medical Center from outside hospitals for higher level of care (11 vs. 8). The percentage of patients admitted to the hospital did not change, but the average length of inpatient hospital stay decreased from 6.7 to 3.1 days. No differences were noted in the urine toxicology (Utox) results between groups, however data was collected inconsistently.
Table 2.
General characteristics of consultations before and after stay at home (SAH) order for each 3-week period.
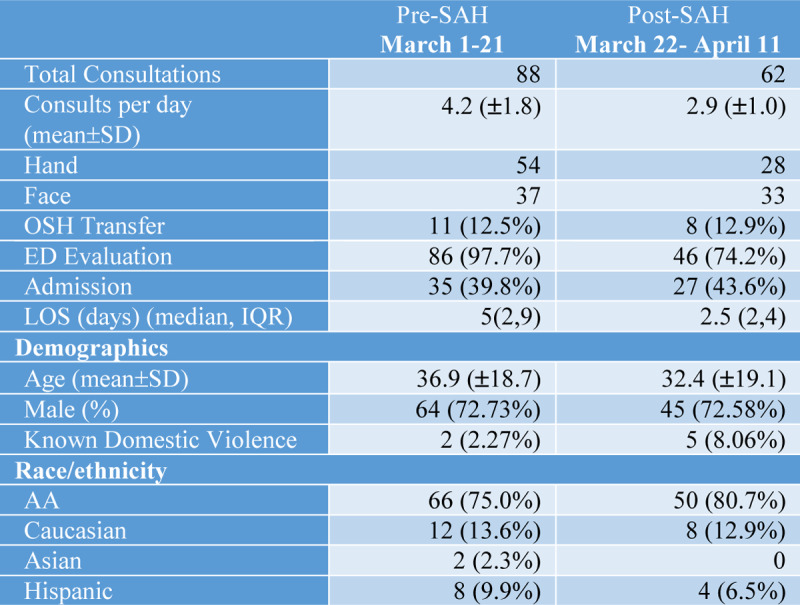
Demographics
The average age of patients seen prior to SAH was 36.9 ± 18.8 compared to 32.4 ± 18.9 following SAH. There was no difference in the gender of patients; 73% of trauma patients presenting before and after SAH were male, compared to 27% female. The ethnic background of patients seen pre SAH consisted of 75% African American, 2% Asian, 14% Caucasian and 9% Hispanic. In the 3 weeks following SAH, 81% of patients seen were African American, 0% Asian, 13% Caucasian and 6% Hispanic (Table 2).
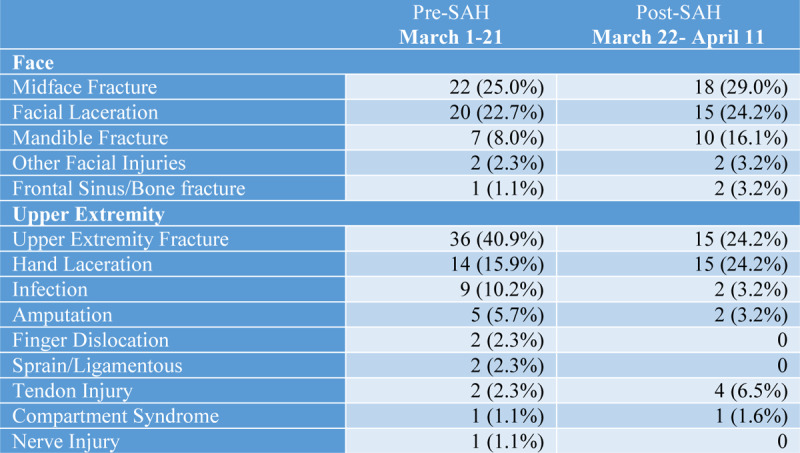
Types of injury
In regard to facial trauma, there was a slight increase in the number of mandibular fractures otherwise were no notable differences in facial trauma pre-SAH compared to post-SAH. (Table 3) For hand trauma, the number of fractures decreased from 36 in the pre-SAH group to 15 in the post-SAH group, which represents a decrease from 50% to 38.5% of all trauma-related injuries over those two time periods (Table 3). The number of hand infections (paronychia, felon, cellulitis) decreased in the post-SAH group (9 vs 2). The number of lacerations to the hand were equal across the two groups but increased as the percentage of total trauma-related injuries in the post-SAH group (19.4% vs 38.5%).
Table 3.
Patient location and mechanism of injury for each 3-week period.
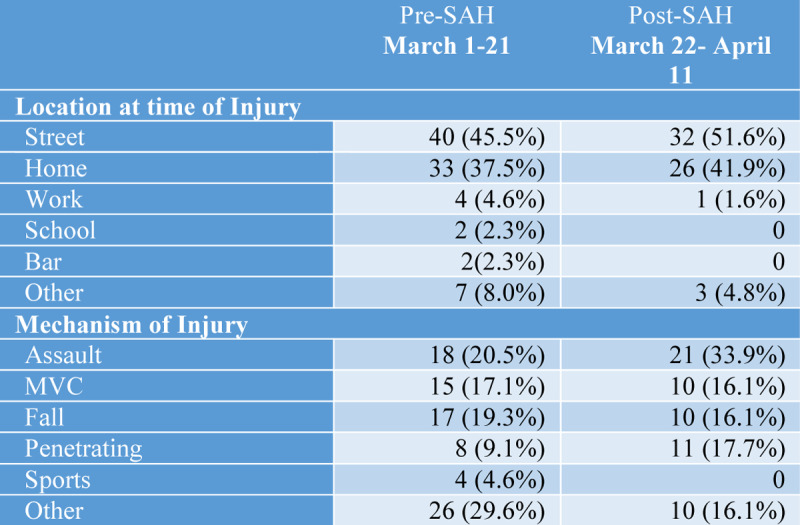
Mechanism of injury
The number and percentage of assault-related injuries increased in the post-SAH group. Eighteen injuries (20.5%) sustained pre-SAH were the result of assault compared to 21 (33.9%) post-SAH. Penetrating trauma, gunshot wounds and stabbings, also increased from 8 to 11 following SAH, which nearly doubled in relative proportion of type of injuries for the time period. The majority of the increase was secondary to an increase gunshot wounds. Of those, 2 were the result of domestic violence in the pre-SAH group compared to 5 in the post-SAH group. The total number of injuries related to motor vehicle collisions (MVC) decreased in the post-SAH group (15 vs 10), but MVC-related injuries as a percentage of all traumas remained the same (17.1% vs 16.1%). There were no sports-related injuries in the post-SAH group (Table 4).
Table 4.
Types of traumatic hand and facial injuries reported as percentage of patients having that type of injury.
Location at time of injury
The percentage of injuries that occurred at home increased slightly from 37.5% to 41.9% in the post- SAH group. At the same time, the percentage of injuries that occurred on the street outside of the home also increased from 45.5% to 51.6%. There were no injuries sustained at school or the bar in the post-SAH group and work-related injuries also decreased (Table 4).
Interventions
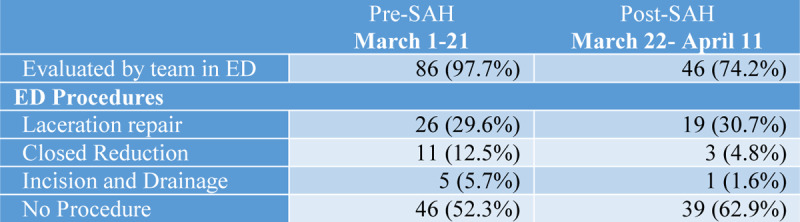
There was a decrease in the percentage of patients evaluated in the emergency room from 97.73% pre-SAH to 74.19% post-SAH. The percentage of hand laceration repairs remained the same while the number of closed reductions of fractures decreased. (Table 5) There was no change in operative volume. Twelve injuries required operative management pre-SAH compared to 11 post-SAH. However, given the overall decrease in trauma consults post-SAH, this represented a higher percentage of total injuries that met operative indications (13.6% vs 17.7%).
Table 5.
Evaluations and procedures performed in the ED.
Discussion
Social distancing policies have profound social, economic and psychological consequences. The purpose of these policies is to reduce the physical interaction of people and thereby limit the propagation of disease. We hypothesized that the issuance of SAH on March 21, 2020 in Chicago, Illinois would have a significant impact on hand and facial trauma seen within the communities served by the University of Chicago Medical Center. Several interesting trends were noted in our data. Notably, the average number of daily consultations received decreased from 4.2 to 2.9 following the SAH. This suggests that social distancing policies may have been effective in reducing the potential for certain types trauma. Notably at our institution there wasn’t a decline in overall trauma activations, there was actually a slight increase in the number of activations. This discordance may represent a decrease in nonurgent consultations originating from the trauma or service, or just a decrease in the number of isolated or lower acuity injuries visiting the ED to avoid the possibility of being exposed in the hospital.
Interestingly, the reduction in the total number of trauma consults was attributed to a decrease in hand trauma consults, while the incidence of facial trauma has remained relatively unchanged. There was a decrease in fractures and infections of the hand. This could be explained, in part, by the suspension of organized sporting activities and workplace closures, which under normal circumstances present a common source of hand injuries.
The demographics of our trauma population changed slightly with social distancing measures. The average age of patients has decreased from 36.9 to 32.4 years. There are several potential explanations for this, which may be related to non-uniform adherence to SAH. It is possible that older people recognize their increased vulnerability to COVID-19 and are more compliant with minimizing their daily activities, thus reducing their injury potential. Meanwhile, reports throughout the country suggest that younger people are not strictly obeying SAH. School closures have also increased the number of children with more unstructured time at home. However, our analysis did not reveal any difference in the number of school-aged children (6-18 years old) presenting with traumatic injuries to the ED as a consequence of SAH.
The majority of trauma patients were African American, which is consistent with the patient population we serve and our general trauma experience. There was a slight increase in the percentage of African American patients from 75% to 80% following SAH. This slight increase is troubling given the disproportionate mortality amongst African Americans noted in Illinois.4 This patient population is traditionally underserved in our communities with socioeconomic disadvantages that make it most vulnerable during a prolonged quarantine. We did not witness any increase in the percentage of Asian Americans presenting with traumatic injuries. The media has reported of a spike in xenophobia directed at this patient population since the spread of COVID-19 in the United States, at times erupting in both verbal and physical violence.5,6 The absence of any traumatic injuries to Asian Americans seen at our institution over the last 3 weeks, should not dismiss possibility of potential physical or verbal abuse that may be directed at this patient population.
The adherence to social distancing is perhaps best reflected in the location (i.e. the house, the outdoors) and the mechanism by which traumatic injuries are sustained. Surprisingly, our data reveals only a slight increase in the percentage of injuries occurring at home (37.5% vs 41.9%), while also noting a slight increase in injuries occurring outside (45.5% vs 51.6%). The lack of injuries occurring in places usually frequented by people, including bars, schools and work partially account for this change. These findings are consistent with trends seen in Anhui, China at the peak of the pandemic. In a retrospective analysis of all trauma patients seen at 2 regional trauma centers, the authors noted a slight but insignificant decrease in injuries occurring outdoors, while the number of injuries occurring at home remained unchanged. 7
Another study from the same region examines changes to the mechanism of traumatic injuries. Comparing data from a 4-week period during the height of the pandemic to the same period over the past 5 years, authors note a significant decrease in traumatic traffic injuries and falls.8 These findings correlate with reports from NASA indicating that air pollution has dropped by as much as 30% in the Northeast region of the United States and 25-40% globally in countries that have implemented stay at home orders.9,10 We noted a similar trend over the 3 weeks following implementation of SAH with an overall decrease in the number of MVC-related injuries.
The potential impact of a lockdown on domestic violence was a major concern preceding its implementation. Unemployment, reduced income, limited social support and alcohol abuse are commonly reported risk factors for family violence.11 We found that these concerns were warranted. Our analysis showed that the percentage of traumatic injuries resulting from domestic disputes increased from 2.3% to 8.1% in the 3-week period after SAH-orders were put in place. This is consistent with trends published in the media nationwide. In Chicago, specifically, the domestic violence hotline has experienced a 12.1% increase in distress calls,2 while Britain has reported a 25% surge.12 This is likely due to increased exposure to domestic partners at home and exacerbated by daily stressors inherent to the pandemic.2
Assaults in general constituted a larger number and percentage of injuries seen in the post-SAH group compared to earlier in the month. This trend was seen in particular with penetrating injuries consisting of stabbings and gunshot wounds. Penetrating injuries increased following the stay at home order (n=11 to n=8), and this trauma mechanism was responsible for nearly double the percentage of injuries in that time period, 17.7% to 9.1%. The majority of these injuries occurred outside of the home. This is an unexpected trend and suggests poor compliance with SAH. It is unclear whether this trend is related to COVID-19. According to government data, the United States has seen a record-breaking number of gun purchases. More than 3.7 million total firearm background checks were conducted through the FBI’s background check system in March 2020, representing an 80% increase compared to March 2019. However, it is difficult to link this trend directly to a slight increase in gunshot wounds seen at our institution.
It is also possible that increases in alcohol sales since the beginning of the crisis have contributed to the increase in assaults over this period.4 We did not see any difference in the percentage of trauma patients presenting to the ED intoxicated as confirmed by a Utox urine toxicology (Utox) screen. However, a Utox was not consistently obtained and documentation was not sufficient to make any conclusions about the trend in alcohol or other drugs use among trauma patients. Additionally, the intoxication of the patient provides no information about the presence of drugs as an influencing agent on the assailant’s actions. The trend more likely reflects the unfortunate reality of our community that frequently deals with assault-related injuries even in the face of a pandemic and strict SAH.
While the total number of hospital admissions has decreased following the SAH, the percentage of total consults being admitted has remained relatively unchanged from 39.78% to 43.55%. This suggests that the acuity of injuries has not changed significantly. Instead, patients suffering minor injuries may be electing to stay at home rather than presenting to the emergency room given the higher risk of exposure. Regardless, the finding that social distancing and SAH appear to have only a minor impact on the incidence of high acuity trauma is troubling and should make us reflect on how to help our patients avoid such situations.
Management of the trauma patient during a pandemic presents unique challenges for the healthcare provider. Under ideal circumstances, the patient would be able to disclose any symptoms of illness to the provider prior to an examination. However, frequently trauma patients arrive in critical condition and their infection status is unknown. This presents significant risk to the healthcare provider, especially when managing complex craniofacial trauma where a comprehensive examination relies on close proximity to the patient’s nose and mouth. These injuries present exposure to open sources of virus in the nasopharynx and sinus.13 In order to ensure self-protection, the provider must therefore operate under the assumption that the patient has the virus and use proper PPE. At the same time, it is important to practice responsible resource allocation given reports in the media regarding critical shortages of PPE around the world.
These conflicting challenges were used as guiding principles in the development of ED protocols for managing trauma consults, namely to 1) protect the healthcare provider, 2) practice responsible resource utilization and to 3) maintain a high level of care. These are similar to guidelines published by a multidisciplinary team at Michigan Medicine who manage maxillofacial trauma14 and reflect the same priorities used by Orthopedic and Trauma Surgery programs in the UK to reconstruct their trauma services .15,16
Following our guidelines, we physically saw fewer patients in the emergency room (97.7% pre-SAH vs 74.2% post-SAH). When the patient was being admitted for other related injuries, we would wait to see the patient until they were transferred to the inpatient unit whenever the acuity of the injury permitted. Nonetheless, we performed procedures in the ER whenever indicated. In fact, the percentage of laceration repairs performed in the ER increased after SAH were implemented. Furthermore, we were able to continue to perform operative interventions when indicated without delay in care. In total, fewer number of patients were evaluated in the ED or admitted, and those admitted had a shorter length of stay, consistent with guidelines aimed at maintaining hospital resources during the crisis.
There are numerous factors to consider when considering trends in consultation across a trauma center. The most significant factor that we frequently note is correlation of penetrating trauma with warmer weather, which we did not account for in our data. The area we serve is also particularly susceptible to retaliatory violence, which can create a cycle of increasing trauma from a single inciting event. While we analyzed the changes in the amount of trauma in the context of SAH, it is important to note that any changes cannot be definitively attributed to the SAH.
Few studies to date have assessed the impact of stay at home orders and COVID-19 on consultation patterns within the United States. Within the Section of Plastic and Reconstructive Surgery at the University of Chicago, we have seen a relative decrease in the volume of plastic surgery emergencies. However, major traumas continue to occur at a relatively high rate within our community. These consultations highlight the need for continued surgical availability within our hospital. As more areas are impacted, we anticipate that similar patterns may be seen across other metropolitan areas. Safe and timely care can continue to be provided with thorough communication, vigilance and guidance from our colleagues.
Footnotes
*Both authors contributed equally to this work.
The authors received no funding for the following manuscript, they have no relevant financial disclosures to report.
References
- 1.Plumer B, Popovich N. Traffic and Pollution Plummet as U.S. Cities Shut Down for Coronavirus. The New York Times. Available from: https://www.nytimes.com/interactive/2020/03/22/climate/coronavirus-usa-traffic.html. 2020. Accessed April 17, 2020.
- 2.Assad S, Hickey M. Chicago Sees An Uptick In Domestic Violence Calls During Coronavirus Outbreak. WBBM-TV CBS2-Chicago. Available from: https://chicago.cbslocal.com/video/4510850-chicago-sees-an-uptick-in-domestic-violence-calls-during-coronavirus-outbreak/. 2020. Accessed April 15, 2020.
- 3.Peterson SL, Moore EE. The integral role of the plastic surgeon at a level I trauma center. Plast Reconstr Surg. 2003;112:1371–1375. [DOI] [PubMed] [Google Scholar]
- 4.IDPH COVID-19 Statistics Available from: https://www.dph.illinois.gov/covid19/covid19-statistics. 2020. Accessed April 15, 2020.
- 5.Coates M. Covid-19 and the rise of racism. BMJ. 2020;369:m1384–m1384. [DOI] [PubMed] [Google Scholar]
- 6.Blanding S, Solomon D. The Coronavirus Pandemic Is Fueling Fear and Hate Across America. Center for American Progress. Available from: https://www.americanprogress.org/issues/race/news/2020/03/30/482407/coronavirus-pandemic-fueling-fear-hate-across-america/. 2020. Accessed April 17, 2020. [Google Scholar]
- 7.Zhu W, Li X, Wu Y, et al. Community quarantine strategy against coronavirus disease 2019 in Anhui: an evaluation based on trauma center patients. Int J Infect Dis. Epub ahead of print April 2020 DOI: 10.1016/j.ijid.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhu W, Yang J, Xu L, et al. A plunge in the number of traumatic traffic injuries in an emergency center in Anhui province, China. American Journal of Emergency Medicine. Epub ahead of print March 20, 2020 DOI: 10.1016/j.ajem.2020.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hauser J, Jackson A. NASA images show a decrease in China’s pollution related to coronavirus. CNN. Available from: https://www.cnn.com/2020/03/01/world/nasa-china-pollution-coronavirus-trnd-scn/index.html. 2020. Accessed April 17, 2020. [Google Scholar]
- 10.He G, Pan Y, Tanaka T. COVID-19, City Lockdown, and Air Pollution: Evidence from China. medRxiv. 2020;2020.03.29.20046649. [Google Scholar]
- 11.Campbell AM. An Increasing Risk of Family Violence during the Covid-19 Pandemic: Strengthening Community Collaborations to Save Lives. Forensic Sci Int Reports. 2020;100089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grierson J. UK domestic abuse helplines report surge in calls during lockdown. The Guardian. Available from: https://www.theguardian.com/society/2020/apr/09/uk-domestic-abuse-helplines-report-surge-in-calls-during-lockdown. 2020. Accessed April 17, 2020.
- 13.Holmes S, Bhatti N, Bhandari R, et al. Toward a consensus view in the management of acute facial injuries during the Covid-19 pandemic. Br J Oral Maxillofac Surg. Epub ahead of print April 2020 DOI: 10.1016/j.bjoms.2020.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Edwards SP, Kasten S, Nelson C, et al. Maxillofacial Trauma Management During COVID-19: Multidisciplinary Recommendations. Facial Plast Surg aesthetic Med. Epub ahead of print April 3, 2020 DOI: 10.1089/fpsam.2020.0158. [DOI] [PubMed] [Google Scholar]
- 15.Morgan C, Ahluwalia AK, Aframian A, et al. The impact of the novel coronavirus on trauma and orthopaedics in the UK. Br J Hosp Med. 2020;1–6. [DOI] [PubMed] [Google Scholar]
- 16.Ashford RU, Nichols JS, Mangwani J. Annotation: The COVID-19 Pandemic and Clinical Orthopaedic and Trauma Surgery. J Clin Orthop Trauma. Epub ahead of print April 2020 DOI: 10.1016/j.jcot.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]


