Appeals have been made to deliver uninterrupted electroconvulsive therapy (ECT) services during the COVID-19 outbreak as the pandemic is likely to increase the mental health burden1,2. A recent report highlighted a bad outcome when the service had to be suspended halfway during a treatment course3. The need for ECT can be classified as elective, essential and urgent/emergency. Elective means that ECT is indicated if the patient is not at significant risk if ECT is not given: e.g. treatment resistant depression without the risk of suicide. Essential ECT is indicated when the patient is at significant risk if ECT is not given: e.g. depression with significant suicide risk or maintenance ECT when the patient is likely to relapse quickly when ECT is withdrawn. Urgent or emergency ECT is indicated when the patient is at high risk if ECT is not given: e.g. severe and or psychotic depression with dehydration and cachexia, malignant catatonia and manic delirium2,4. Anesthesiologists may either encounter known/suspected COVID-19 cases, or ward-nursed unsuspected patients who happen to be in close proximity to a positive case. Such a scenario has been recently described3. Aerosol/droplet dispersion is likely during the peri-ictal phase from airway manipulation, bag mask ventilation (BMV), cough and motor seizures. We highlight airway management principles for ECT in suspected as well as unsuspected COVID-19 patients, based on current guidelines and our practice adaptations.
Known or suspected cases should be performed with full personal protective equipment precautions (as per local guidelines) in a negative pressure room if available. Patients should be briefed about the procedure and the attire worn by the staff to prevent an overwhelming impression. For co-operative patients, a surgical facemask should be applied during transfer. A dedicated anesthetic machine with a viral filter at the expiratory limb is preferable. Open anesthetic circuits such as the Bain’s modification of Mapleson D without viral filters is a common practice in resource-poor settings and are best avoided.
BMV is generally discouraged for known/suspected COVID patients considering the possibility of a poor airway seal increasing the risk of aerosolization5. Also, it leaves the respiratory track and the upper airway open during the ictal phase. While tracheal intubation can achieve a near complete seal and limit aerosolization, the intubation and extubation process together with bucking on the endotracheal tube and maneuvers such as suctioning can increase the risk of aerosol and droplet dispersion. The latest expert opinion supports the use of supraglottic airways (SGAs) in known/suspected COVID patients when it is indicated6. Currently, evidence is lacking to support one device (SGA vs tracheal tubes) over the other during this pandemic6. SGA insertion and removal may be less aerosol generating than during tracheal intubation and extubation, and tracheal intubation is the procedure most associated with virus transmission6. These devices offer better seal pressure during assisted ventilation compared to the first generation devices, and may reduce aerosolization of viral particles5,7. For these reasons, a second generation SGA such as the i-gel® (taking due care to ensure a leak-free seal) may be a better option for airway management than standard practice in known/suspected COVID cases for ECT. The technique has many favorable features. First, a well-fitting device can offer a near complete seal of the oropharynx. Second, it negates the requirement for BMV, and can reduce proximity of the staff to the airway. Third, a closed circuit can be established (without disconnection) and maintained throughout the stimulus and seizure phase. Fourth, it facilitates smooth emergence. The gastric channel can be taped to prevent any droplet dispersion.
Preoxygenation (< 6 L min -1) with a two-hand mask holding technique should commence using an anaesthetic face mask with a viral filter. An antisialagogue would help to reduce the secretions and droplet spread. Induction should be followed by administration of 1.5 mg/kg of succinylcholine, and a SGA should be inserted when appropriate. Gentle BMV prior to SGA insertion should be restricted only for hypoxia. Gentle positive pressure ventilation should commence after ensuring leak-free seal and establishing a closed circuit system. It may be better to avoid ventilation during facsiculations due to high esophageal pressures. During electro-stimulus application and seizure activity, a firm bite block should remain in-place; circuit should remain connected, adjustable pressure relief valve opened to zero, and ventilation ceased at end-expiration. Anaesthetic induction, SGA insertion and stimulus delivery can be done under a clear plastic tent, firmly encircled over the head and chest areas (Figure). This method may reduce aerosol/droplet dispersion and allows unobstructed monitoring of motor seizures. Synchronized ventilation should be commenced when appropriate and extubation performed under the tent and transitioned to oxygen delivering devices. Many patients who receive ECT feel claustrophobic and could become anxious if covered by sheets/tents. Special COVID intubating negative pressure chambers have been discussed on online/social media platforms. These chambers are transparent with a big surface area and projects away from the face and torso, and likely to be less disturbing to the patients.
Figure 1.
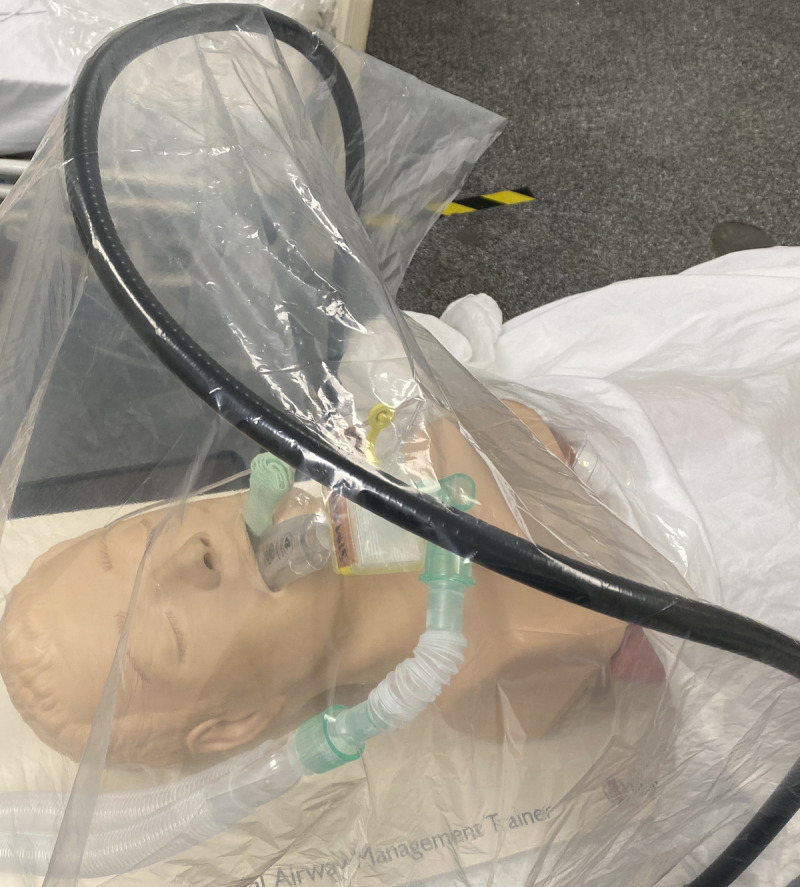
Supraglottic airway (i-gel®) with a viral filter and bite block in place and a clear plastic tent covering the airway and upper part of chest.
The service is provided without any interruption at our (AD) institution, located in the state with highest prevalence of COVID-19 in the country at the time of this writing. There are suggestions that viral transmission is feasible through asymptomatic carriers, and viral loads could be similar between symptomatic and asymptomatic patients8. In areas with high prevalence, opinion from infectious disease experts should be considered in choosing an optimal technique. A practice change has been implemented for our routine cases. This involves airway management with i-gel® (with a viral filter), a second generation SGA device. Author’s preference of bite block is tightly rolled gauzes about 2 cm diameter.
Antiemetics are warranted as post-ictal nausea can manifest in up to 25% of patients9. Self-limiting post-ictal agitation (with potential for droplets spread) can affect up to 10% of patients. In severe cases, small doses of benzodiazepines, propofol or dexmedetomidine can be used10. Policy makers must appreciate the role of ECT in reinstating quality of life for patients during the pandemic. As guidelines and clinical updates in the management of COVID-19 patients continue to evolve, locally adapted and updated recommendations are often the best resource.
Acknowledgments
Author Contributions:
Venkatesan Thiruvenkatarajan: main author conceptualised the review, drafting and review of the manuscript.
Ashok Dharmalingam: manuscript writing, editing and critical review
Allysan Armstrong-Brown: critical review and expert opinion
Alan Weiss: critical review and expert opinion
Susan Waite: critical review and expert opinion
Roelof Van Wijk: critical review, editing and expert opinion
Footnotes
Conflict of interests: Nil
Funding sources: Nothing to declare
References
- 1.Espinoza RT, Kellner CH, McCall WV. ECT: An Essential Medical Procedure. J ECT 2020; published online Mar 31 Doi; 10.1097/YCT.00000000000089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.ECT is an essential treatment and can save lives during COVID-19. The Royal Australian and New Zealand College of Psychiatrists. https://www.ranzcp.org/news-policy/news/ect-is-an-essential-treatment-and-can-save-lives-d (accessed Apr 16, 2020).
- 3.Tor PC, Phu AHH, Koh DSH, Mok YM. ECT in a time of COVID-19. J ECT 2020; published online Mar 31 Doi; 10.1097/YCT.00000000000690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baghai TC, Möller HJ. Electroconvulsive therapy and its different indications. Dialogues Clin Neurosci 2008; 10: 105–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brewster DJ, Chrimes NC, Do TBT, et al. Consensus statement: Safe Airway Society principles of airway management and tracheal intubation specific to the COVID-19 adult patient group. [published online ahead of print, 2020 May 1]. Med J Aust. 2020;10.5694/mja2.50598.doi: 10.5694/mja2.50598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The Faculty of Intensive Care Medicine Use supraglottic airways during the COVID-19 pandemic. ICM Anaesthesia COVID-19. Available from: https://icmanaesthesiacovid-19.org/use-of-supraglottic-airways-during-the-covid-19-pandemic. Published 7 May 2020. Accessed 8 may 2020.
- 7.Cheung JC, Ho LT, Cheng JV, Cham EYK, Lam KN. Staff safety during emergency airway management for COVID-19 in Hong Kong. Lancet Respir Med 2020. Apr; 8:e19. doi: 10.1016/S2213-2600(20)30084-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lui RN, Wong SH, Sánchez-Luna SA, Pellino G, Bollipo S, Wong MY, Chiu PW, Sung JJ. Overview of guidance for endoscopy during the coronavirus disease 2019 (COVID-19) pandemic. J Gastroenterol Hepatol 2020; published online Mar 31. doi: 10.1111/jgh.15053. [DOI] [PubMed] [Google Scholar]
- 9.Bryson EO, Aloysi AS, Farber KG, Kellner CH. Individualized anesthetic management for patients undergoing electroconvulsive therapy: a review of current practice. Anesthesia & Analgesia 2017; 124: 1943–56. [DOI] [PubMed] [Google Scholar]
- 10.Mizrak A, Koruk S, Ganidagli S, Bulut M, Oner U. Premedication with dexmedetomidine and midazolam attenuates agitation after electroconvulsive therapy. Journal of anesthesia 2009; 23: 6–10. [DOI] [PubMed] [Google Scholar]


