Supplemental Digital Content is available in the text
Keywords: COVID-19, public perceptions, rapid online surveys, surgery, telemedicine
Abstract
Objective:
This study aims to determine the public's perception of telemedicine surgical consultations, during the COVID-19 pandemic and beyond.
Summary Background Data:
With rapid expansion and uptake of telemedicine during the pandemic, many have posited that virtual visits will endure even as in-person visits are reinstated. The public's perception of telemedicine for an initial surgical consultation has not been previously studied.
Methods:
A 43-question survey assessed respondents’ attitudes toward telemedicine for initial consultations with surgeons, both in the context of COVID-19 and during “normal circumstances.” Participants were recruited through Amazon Mechanical Turk, an online crowd-sourcing marketplace.
Results:
Based on 1827 analyzable responses, we found that a majority (86%) of respondents reported being satisfied (either extremely or somewhat) with telemedicine encounters. Interestingly, preference for in-person versus virtual surgical consultation reflected access to care, with preference for telemedicine decreasing from 72% to 33% when COVID-related social distancing ends. Preferences for virtual visits decreased with increasing complexity of the surgical intervention, even during the pandemic. A majority felt that “establishing trust and comfort” was best accomplished in person, and the vast majority felt it was important to meet their surgeons before the day of surgery.
Conclusions:
The public views telemedicine as an acceptable substitute for in-person visits, especially during the pandemic. However, it seems that an in-person interaction is still preferred when possible for surgical consultations. If telemedicine services are to persist beyond social distancing, further exploration of its impact on the patient-surgeon relationship will be needed.
The COVID-19 pandemic has catalyzed an unprecedented need to deliver care remotely. Within just a few days of widespread advisories for social distancing and shelter-in-place mandates, there was rapid expansion of telemedicine services across specialties and sites to continue to meet patients’ ambulatory care needs. Long touted as an underused, but promising, mode of delivering care, telemedicine has become a putative “game changer” during the pandemic.1,2
As physicians rapidly converted to either televideo or telephonic appointments, many came to realize that nearly all (or all) components of the visit were able to be completed virtually. Many have, albeit anecdotally, reported high levels of both provider and patient satisfaction with telemedicine. Indeed, the development and expansion of platforms for the delivery of virtual services and the resultant increase in capacity and/or readiness to sustain telemedicine may be a positive unintended consequence of population-wide social distancing.3
However, as payers and policymakers make decisions about the future of waivers and temporary/emergent policies around the delivery of telemedicine visits, public perception of and patient satisfaction with virtual visits will be needed to inform decision making. Based on analyses of internet search volumes, it seems that broad interest in telemedicine is increasing.4 However, acceptance of telemedicine in the setting of the pandemic may be a consequence of the perceived risks associated with in-person visits, not to mention the nearly universal suspension of them. On the other hand, ease of access associated with telemedicine may result in sustained changes in care delivery.
We conducted this online, crowd-sourced survey to learn more about the public's willingness to use telemedicine for an initial consultation with a surgeon and to understand how their attitudes are affected by the unique factors posed by the COVID-19 pandemic.
METHODS
Survey Design
A public-facing survey was developed on a Qualtrics (Provo, UT) online platform using a modified Delphi method. A draft of the survey was developed by the investigators and then alpha-tested by 6 volunteer participants. Based on their feedback, an updated version of the survey was beta-tested on 24 volunteer participants via convenience sampling. Beta-version feedback was incorporated at this stage, and a final 43-question version of the survey was created (Appendix 1; http://links.lww.com/SLA/C309). The survey was designed to be completed in 15 minutes or less.
We collected basic demographic information, including data about prior experience with the health care system (either professionally or as a surgical patient) and with telemedicine, specifically focusing on satisfaction and willingness to continue with virtual visits. The first portion of the survey was based on a five-point Likert scale and asked respondents to consider the importance of meeting their surgeon in person before the day of surgery. We also asked respondents whether certain components of an initial appointment with their surgeon would be better accomplished in person, virtually, or either way. Then, to determine if there were differences in preferences for telemedicine under normal circumstances (before or after the pandemic) compared to the limitations imposed by social distancing, 6 different surgical scenarios of varying complexity were used: lipoma, cosmetic rhinoplasty, inguinal hernia, thyroid cancer, pancreatic cancer, and total knee replacement. Finally, survey participants were invited to comment on initial visits with a surgeon and telemedicine in a free text box.
Participant Enrollment
Participants were recruited using Amazon Mechanical Turk, or MTurk, an online crowd-sourcing marketplace which allows people to complete human intelligence tasks for small amounts of money. We restricted participation in our study to those 18 years or older who reside in the United States. We included one attention check question in the middle of the survey and excluded participants who did not answer this question correctly. We paid each participant based on the federal minimum wage for taking this 15-minute survey ($1.75). To maximize demographic representation, and therefore generalizability of the survey results, we targeted enrollment of 2000 participants. The survey was posted on April 21, 2020 and we achieved the targeted number of responses in 4 days.
This study was approved by the Dartmouth-Hitchcock Institutional Review Board (Study 02000435).
RESULTS
Two thousand forty-two people responded to this survey. Seventy-nine were excluded for missing the attention check question, and 142 were excluded for entering invalid responses on questions which would indicate a lack of attentiveness to the survey questions. We therefore included 1827 responses in our final analysis.
Demographics of the respondents are shown in Table 1. The majority of respondents (85%) were under age 50, and 58% were male. Overall, they were well-educated, with 76% reporting at least a college degree; 27% of respondents had some medical background. The survey population tended to be employed (84% working full or part-time) and insured (87% with some form of health insurance). Only 12% of respondents were from a rural area, and most reported that they lived within 30 minutes of both their doctor's office (80%) and the nearest hospital (82%). Almost all reported compliance with social distancing measures, with 94% either not leaving home at all or going out only for essential activities.
TABLE 1.
Characteristics of Survey Respondents (N = 1827)
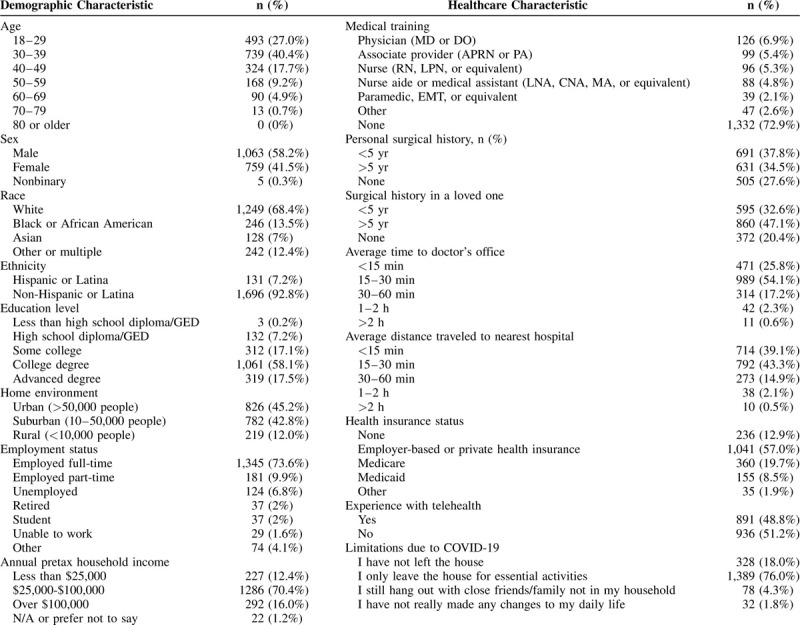
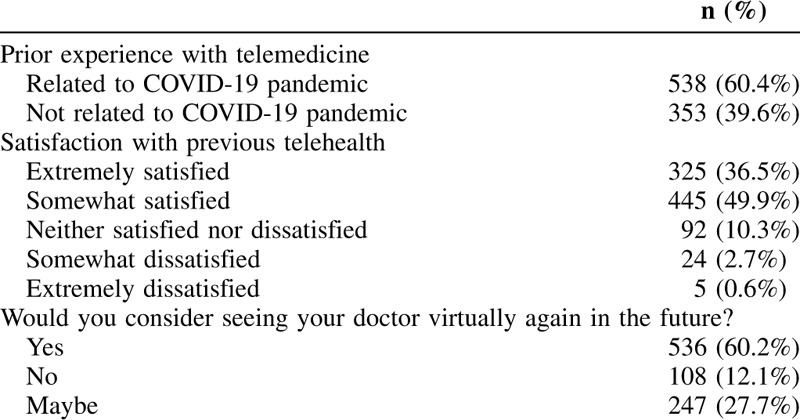
More than two-thirds had prior experience with surgery either as a patient (72% reported having prior surgery) or via experience with a loved one going through surgery (80%). Half of respondents (49%) had experience with telemedicine, and 60% of those experiences were due to the COVID-19 pandemic (Table 2). Of the respondents who had prior experience with telemedicine (n = 891, 49%), most reported being extremely satisfied (36%) or somewhat satisfied (50%) with the encounter(s). Only 12% were unwilling to consider seeing a doctor virtually again.
TABLE 2.
Respondents’ Prior Experience and Satisfaction with Telemedicine (N = 891)
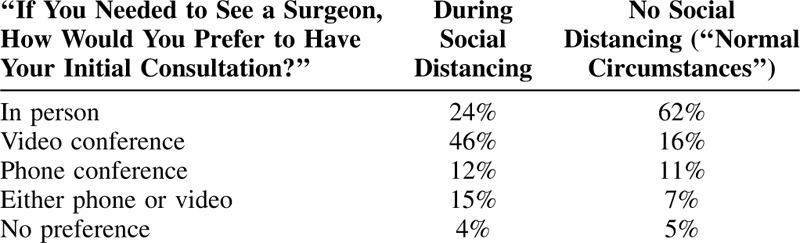
In general, respondents were interested in telemedicine as a means to access the health care system during social distancing related to the pandemic: 79% preferred telemedicine for visits to their primary care providers (PCPs), with only 16% desiring to see their PCP in person. A higher proportion (24%) favored an in-person consultation with a surgeon if necessary during social distancing, but 72% would choose a telemedicine visit. Of the telemedicine modalities, video visits were preferred over telephonic ones. However, without the limitations of social distancing, 62% would prefer an in-person initial consultation with a surgeon, with only 33% choosing telemedicine (Table 3). The majority of respondents (62%) believed a virtual visit should cost less than an in-person visit, whereas 22% thought the visits should be the same cost and only 15% thought that a virtual visit should cost more.
TABLE 3.
Preferences for In Person versus Telemedicine Visits
We sought to understand the perceived importance of in-person meetings between surgeons and potential patients, and the perceived effectiveness of telemedicine to achieve certain elements of an initial surgical consultation. Nearly three-quarters of survey respondents believed it was extremely or very important to meet their surgeon in person beforethe day of surgery (71%) and to be examined by the surgeon before the day of surgery (73%). Further, they did not seem to believe this was as important to the surgeon, with only 56% and 64%, respectively, reporting that they thought it would be extremely or very important to their surgeon to meet them and examine them before the day of surgery (Fig. 1). When considering 8 components of an initial visit to a surgeon (review history/reason for referral; initiate/complete diagnostic work-up; perform a physical exam; discuss treatment options; offer an opinion regarding need for/benefit of surgery; explain the technical components of the surgery; establish trust/comfort; and explain post-operative monitoring), the majority of respondents thought the physical exam (72%) and establishing trust and comfort (55%) could best be done in person. Almost half (44%) reported that initiating/completing a diagnostic workup would also be better in person. For the other 5 elements of the consultation, the majority (57%–67%) thought either an in-person or telemedicine visit would suffice. There were no elements of the initial consultation that respondents thought would be more effective virtually (Fig. 2).
FIGURE 1.
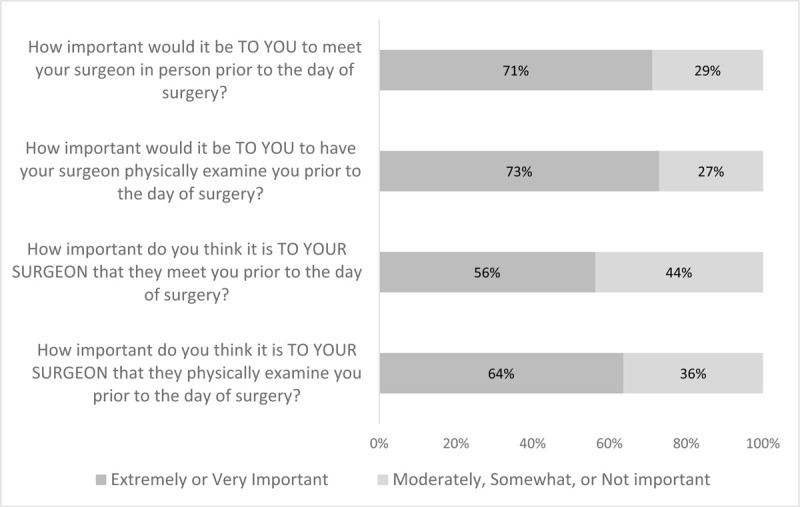
Perceived importance of in-person meetings between patients and surgeons.
FIGURE 2.
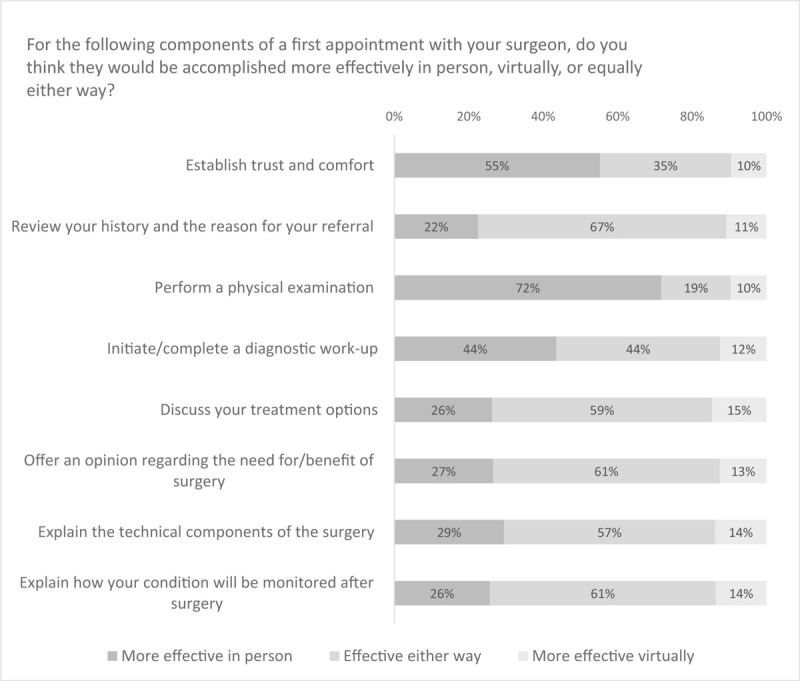
Effectiveness of telehealth on various elements of an initial surgical consultation.
Survey respondents were asked to consider 6 different surgical scenarios: lipoma resection; rhinoplasty; inguinal hernia repair; thyroidectomy for cancer; pancreatic resection for cancer; and total knee replacement for severe knee osteoarthritis. Under “normal circumstances,” most participants would prefer an in-person consultation for all 6 diagnoses, ranging from 64% for lipoma to 79% for pancreatic cancer. During social distancing, most respondents preferred telemedicine; as the diagnoses became relatively more complicated, the preference for in-person consultation increased. For example, only 20% preferred an in-person initial consultation with a surgeon for rhinoplasty during social distancing, but 52% would prefer it for pancreatic cancer. Interestingly, a minority of participants would delay care altogether for any of the diagnoses, with 20% of respondents reporting that they would wait for social distancing to end before consulting with a surgeon regarding rhinoplasty, and only 4% would delay consultation for pancreatic cancer (Fig. 3). Survey respondents were also asked to consider the same 6 scenarios for a loved one (for whom they would be the primary caregiver). There was no difference in their preferences for in person and telemedicine visits when considering their own care versus that of a loved one.
FIGURE 3.

Attitudes toward telehealth under “normal circumstances” versus during social distancing.
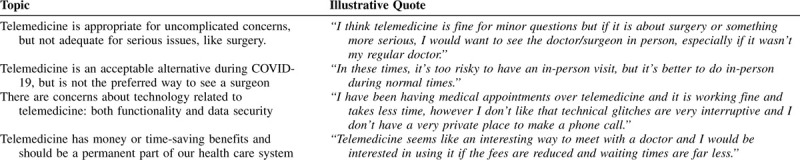
Free text comments were reviewed qualitatively. We were unable to formally analyze the content for themes, but some topics emerged, including perceptions that telemedicine visits are more appropriate for uncomplicated visits, less appropriate for surgical consultation, and viewed relatively more favorably when access is otherwise limited. Some comments reflected concerns with technical difficulties and perceptions that telemedicine visits should be lower cost (Table 4).
TABLE 4.
Common Topics Identified in Participant Free-form Comments
DISCUSSION
This study is the first to report large-scale public attitudes toward obtaining an initial surgical consultation via telemedicine, specifically in the context of social distancing during COVID-19 pandemic, but with consideration for “normal circumstances.” Using a crowd-sourced survey with over 2000 respondents, we confirmed that telemedicine has indeed become more ubiquitous during the pandemic, with approximately half of survey respondents reporting prior experience with telemedicine, noting that 60% of those virtual encounters occurred during COVID-19-related social distancing. A vast majority (86%) of respondents reported being satisfied (either extremely or somewhat) with their telemedicine encounter. Interestingly, preference for in-person versus virtual surgical consultation reflected access to care, with preference for telemedicine decreasing from 72% to 33% when COVID-related social distancing ends. Telemedicine was viewed more favorably for PCP visits than for surgical consultations, with a further decline in preferences for virtual visits with increasing complexity of surgical intervention, even during the pandemic.
Although many have posited that telemedicine will have an enduring presence even as in-person visits are reinstated, surgical consultations require special consideration. Not surprisingly, the vast majority of survey respondents indicated that it was extremely or very important to meet their surgeon and to have their surgeon examine them in person before the day of surgery, which corresponds with our finding that a majority of respondents felt that “establishing trust and comfort” was best accomplished in person. Interestingly, public perception about the converse (how important it was for surgeons to meet and examine patients in person before the day of surgery), demonstrated a slight shift, with a much lower (albeit still majority) opinion about the relative importance of this. Taken together, such perceptions may explain why most respondents felt that telemedicine visits should cost less than an in person one. In this initial exploratory study, we were unable to delve into the reasons behind this perception, but future work will need to explore the impact of the respondents’ insurance status and out-of-pocket costs.
Various prior studies have reported high patient satisfaction with telemedicine in the surgical context, citing benefits of money saved/economic benefit,5,6 reduced missed work,7 reduced trips to hospital,7,8 and preventing additional calls or visits to clinicians.8 However, almost all of this work has been for surgical follow-up visits and not initial consultations, which was the focus of our study.9,10 A few telemedicine studies in limited settings demonstrate and support its feasibility and accuracy for prescreening of patients with common general surgery diagnoses.11–14 Indeed, there is very little in the literature related to using telemedicine in more “elective” settings, especially ones in which there is a consultation requiring more shared decision making. Prior studies in primary care settings suggest that there is less information exchange by patients and physicians during video and telephonic visits when compared with in-person encounters,15 suggesting that patients and physicians may adapt their behavior and expectations based on circumstances, including the relative urgency or severity of presentation and access to care.
Our findings demonstrated the strong effect of telemedicine in alleviating barriers resulting from COVID-related social distancing restrictions to receipt of a surgical consultation. Very few respondents wished to “wait until social distancing ends” even with relatively discretionary and elective procedures such as rhinoplasty and total knee replacement. As a measure of relative sensitivity to mode of care, acceptance of a telemedicine visit, compared to desire for an in-person visit, decreased with relative severity of disease. Even with social distancing in place, over half of respondents wanted an in-person visit for pancreas cancer evaluation, though this was the case in less than a quarter of those with an inguinal hernia and in a fifth of those with a lipoma. Across all 6 scenarios, there were no differences in proportions of respondents who preferred in-person visits regardless of the relative importance they placed on the surgeon meeting patients before the day of surgery, suggesting it was their own desire to interact with the surgeon rather than a perception that it would be critical for the surgeon's decision making.
There was generally slow adoption of telemedicine before the COVID-19 pandemic, related to regulatory barriers and implementation challenges related to technology platforms. However, COVID-related social distancing mandates and the mass suspension of normal ambulatory clinic operations led to the rapid uptake of telemedicine visits, aided by changes in policies around telemedicine visits including broad coverage of services by the Centers for Medicare & Medicaid Services (CMS) on “a temporary and emergency basis.” These CMS waivers will need to be evaluated as the pandemic evolves back to more normal circumstances and our findings may be important to consider as this occurs, especially as it relates to surgical consultations and the value placed on an in-person meeting with a surgeon before surgery.
As noted previously, survey respondents placed great importance in meeting their surgeon in person before the day of surgery. This suggests that if the initial consultation were done virtually, an in-person visit may need to be scheduled before surgery or, at the very least, extra time may need to be built in for discussions on the day of surgery. As such, practical considerations around reimbursement for services (related to multiple and duplicative visits) and health care utilization (efficiency and workflow around surgical schedules) will need to be resolved if telemedicine visits continue to be used in high volumes. Moreover, concern for the depersonalization of care with telemedicine has been described both before and during the COVID-19 pandemic, and the ability to establish rapport virtually is understudied across settings.16
There are several limitations of this study. Participants in a crowd-sourced survey study are selfselected and make up a nonrepresentative cohort. There is no calculable response rate and results may not be generalizable. However, Amazon MTurk is an increasingly credible means of conducting survey research in healthcare.17 In addition, rapid online surveys have been proposed as a highly effective way to assess evolving public perceptions during COVID-19 pandemic.18 Given this methodology, our respondents, by definition, represent a relatively more tech-savvy segment of the population. Although this is another reason our findings may not be generalizable, we hypothesize that people without access to or familiarity with technology would be even less comfortable with telehealth consultations. Another limitation is that this survey relies on the participants’ ability to imagine their response in hypothetical scenarios rather than studying the response of real patients actually facing these diagnoses and decisions. That said, public perception is important to consider since policy changes, as would be the case with CMS waivers and regulations around telemedicine services, should take a broader view into consideration. Nevertheless, early reports demonstrate a high level of patient satisfaction with telemedicine; whether this is solely related to a paucity of choice secondary to the pandemic or reflective of broader views on access to care remain to be seen.
CONCLUSIONS
There is an abundance of enthusiasm for telemedicine from both patients and providers, and it seems that the public views it as an acceptable substitute, especially during the COVID-19 pandemic. However, it may be that an in-person interaction is still preferred when at all possible for initial surgical consultations. If expanded telemedicine services are to persist beyond social distancing, the impact it could have on patient satisfaction and the therapeutic relationship between surgeons and their patients will need to be further explored.
Footnotes
The authors report no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.annalsofsurgery.com).
REFERENCES
- 1.Robbins T, Hudson S, Ray P, et al. COVID-19: a new digital dawn? Digital health 2020; 6:2055207620920083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med 2020; 382:1679–1681. [DOI] [PubMed] [Google Scholar]
- 3.Hakim AA, Kellish AS, Atabek U, et al. Implications for the use of telehealth in surgical patients during the COVID-19 pandemic. Am J Surg 2020; doi:10.1016/j.amjsurg.2020.04.026. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hong Y-R, Lawrence J, Williams D, Jr, et al. Population-level interest and telehealth capacity of US hospitals in response to COVID-19: cross-sectional analysis of google search and national hospital survey data. JMIR Public Heal Surveill 2020; 6:e18961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wood EW, Strauss RA, Janus C, et al. Telemedicine consultations in oral and maxillofacial surgery: a follow-up study. J Oral Maxillofac Surg 2016; 74:262–268. Epub 2015 Oct 3. [DOI] [PubMed] [Google Scholar]
- 6.Urquhart AC, Antoniotti NM, Berg RL. Telemedicine- an efficient and cost-effective approach in parathyroid surgery. Laryngoscope 2011; 121:1422–1425. Epub 2011 Jun 6. [DOI] [PubMed] [Google Scholar]
- 7.Martínez-Ramos C, Cerdán MT, López RS. Mobile phone-based telemedicine system for the home follow-up of patients undergoing ambulatory surgery. Telemed J E Health 2009; 15:531–537. [DOI] [PubMed] [Google Scholar]
- 8.Willard A, Brown E, Masten M, et al. Complex surgical infants benefit from postdischarge telemedicine visits. Adv Neonatal Care 2018; 18:22–30. [DOI] [PubMed] [Google Scholar]
- 9.Nandra K, Koenig G, DelMastro A, et al. Telehealth provides a comprehensive approach to the surgical patient. Am J Surg 2019; 218:476–479. [DOI] [PubMed] [Google Scholar]
- 10.Soegaard Ballester JM, Scott MF, Owei L, et al. Patient preference for time-saving telehealth postoperative visits after routine surgery in an urban setting. Surgery 2018; 163:672–679. [DOI] [PubMed] [Google Scholar]
- 11.Cain SM, Moore R, Sturm L, et al. Clinical assessment and management of general surgery patients via synchronous telehealth. J Telemed Telecare 2017; 23:371–375. [DOI] [PubMed] [Google Scholar]
- 12.Schroeder C. Pilot study of telemedicine for the initial evaluation of general surgery patients in the clinic and hospitalized settings. Surg Open Sci 2019; 1:97–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sudan R, Salter M, Lynch T, et al. Bariatric surgery using a network and teleconferencing to serve remote patients in the Veterans Administration Health Care System: feasibility and results. Am J Surg 2011; 202:71–76. Epub 2011 May 23. [DOI] [PubMed] [Google Scholar]
- 14. Lee S, Broderick TJ, Haynes J, et al. The role of low-bandwidth telemedicine in surgical prescreening. J Pediatr Surg. 2003;38:1281–1283. [DOI] [PubMed] [Google Scholar]
- 15.Hammersley V, Donaghy E, Parker R, et al. Comparing the content and quality of video, telephone, and face-to-face consultations: a non-randomised, quasi-experimental, exploratory study in UK primary care. Br J Gen Pract J R Coll Gen Pract 2019; 69:e595–e604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dickman Portz J, Ford K, Bekelman DB, et al. We’re taking something so human and trying to digitize”: provider recommendations for mHealth in palliative care. J Palliat Med 2020; 23:240–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mortensen K, Hughes TL. Comparing Amazon's mechanical Turk platform to conventional data collection methods in the health and medical research literature. J Gen Intern Med 2018; 33:533–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Geldsetzer P. Use of rapid online surveys to assess people's perceptions during infectious disease outbreaks: a cross-sectional survey on COVID-19. J Med Internet Res 2020; 22:e18790. [DOI] [PMC free article] [PubMed] [Google Scholar]


