Abstract
Background:
Nurses suffer from Compassion Fatigue (CF) when exposed to chronic stress while caring for patients. Depression and anxiety disorders can develop following CF and intervention at the earliest is essential. The present study aimed to evaluate the effectiveness of the Accelerated Recovery Program (ARP) on CF among nurses.
Materials and Methods:
The present experimental study was carried out with a pretest posttest design and control group among 120 nurses working in Narayana Medical College Hospital, India. The nurses selected through simple random sampling were divided into two groups: intervention and control (every 60 nurses). Data were collected using the Professional Quality of Life Scale: Compassion Satisfaction and Fatigue Version 5 (ProQOL) (Stamm, 2010) which consists of the three subscales of Compassion Satisfaction (CS), Burnout (BO), and Secondary Traumatic Stress (STS). The pretest was conducted at day 1, and posttests I, II, III, IV, and V were conducted at 5th week, 3rd month, 6th month, 9th month, and 12th month, respectively using ProQOL. ARP and routine care were implemented for 5 weeks in the intervention group, and routine activities were implemented in the control group. Data were analyzed using descriptive and inferential statistics.
Results:
There was a statistically significant difference in the ProQOL score between the intervention and control groups, which demonstrated a significant difference between the groups in terms of CS (F1,118= 120.10, p < 0.001), BO (F1,118 = 123., p < 0.001), and STS (F1,118 = 205.18, p < 0.001).
Conclusion:
In conclusion, ARP has a significant impact on ProQOL, resulting in an improvement in CS, and a decrease in BO and STS.
Keywords: Burnout, compassion fatigue, nurses, psychological
Introduction
Nursing is an exceptionally challenging but gratifying profession. It necessitates the physical, psychological, emotional, and spiritual involvement of the nurse.[1] Nurses are in contact with patients in every phase of treatment, and support them and give them the confidence to fight the illness. Being a facilitator, nurses undergo painful experiences during their career.[2] Caring has positive and negative effects on the Professional Quality of Life (ProQOL) of the nurses. Factors such as work environment, competency in caregiving, designation, nature of job, beliefs, and perception influence the ProQOL score.[3] ProQOL has two components, namely, Compassion Satisfaction (CS), and Compassion Fatigue (CF). CS is an optimistic feeling resulting from helping individuals to overcome distressing events.[4] Figley states that CF, also termed vicarious trauma or Secondary Traumatic Stress (STS), occurs when an individual is exposed to chronic stress in caring for patients due to experiencing misery, catastrophe, and grief.[5]
CF comprises CS, Burnout (BO), and STS.[5] BO is defined as a mental pattern that involves a lengthened reaction to persistent interpersonal stressors on the job (Jan Beckstrand, 2017).[6] STS is a situation portrayed by an enduring decrease in compassion for a long period. BO and STS are interrelated as the former is the outcome of ecological stressors, and the latter is the result of the experience of caring for patients.[7] According to the World Health Organization (WHO) (2012), the information from the National Institute for Occupational Safety and Health (NIOSH) revealed that “healthcare workers have higher rates of substance abuse and suicide than other professions and high rates of depression and anxiety linked to job stress.”[7] Previous studies have reported that 79% of nurses suffer from BO,[8] and 42% of palliative professionals and 64% of emergency nurses had STS.[9] Another study reported that 17% of nurses working in a hospice and palliative care had CF.[10] In the study by Kelly et al., 60% of healthcare workers reported feeling burned out by their jobs, 34% planned for a new job, and 45% were looking forward to a job change over the next 2 years.[11] Nolte stated that CF has not been labeled as a psychiatric disorder, but it can lead to depression and anxiety disorders.[12] Various research studies have been conducted on the prevalence of stress, BO, Post-Traumatic Stress Disorder (PTSD), and CF. Some studies conducted have proved that interventions such as guided imagery, mindfulness training, educational programs, and resiliency programs are effective on combating stress, BO, PTSD, and CF. A holistic program is vital in managing the problem of CF and in bringing out the optimal personal and professional potentials of an individual.
An Accelerated Recovery Program (ARP)[13] is an interventional package that includes guided imagery, Neuro-Linguistic Programming (NLP), Thought Field Therapy (TFT), self-management plan, and self-analysis which can augment the clinical competencies and enrich the personal well-being of nurses. The literature search by the investigator also revealed that very few studies have been carried out on CF and the effectiveness of ARP on CF. Thus, the present study aimed to evaluate the impact of ARP on CF among nurses.
Materials and Methods
An experimental study with a pretest-posttest design and control group was conducted from April 2015 to March 2017 in Narayana Medical College Hospital, Nellore, Andhra Pradesh, India. The sample size was calculated using power analysis (Z1α/2 = 1.96; Zβ1 = 0.85; S = 1.82; d = 1.60), and 120 nurses from ICUs and emergency wards were recruited for the study through simple random sampling using lottery method. The nurses were randomly assigned to the intervention (60 nurses) and control groups (60 nurses). The study inclusion criteria were being a nurse and a CS score of less than 22, and BO and STS scores of higher than 42. Nurses who underwent any training program related to stress management, cognitive-behavioural therapy (CBT) and NLP were excluded from the study. Data was collected using the ProQOL Scale: Compassion Satisfaction and Fatigue Version 5 (Stamm, 2010).[14] The 30-item ProQOL Scale consists of the 3 subscales of CS, BO, and STS, each containing 10 items that are scored on a 5-point Likert scale. All subscales have a minimum score of 10 and a maximum score of 50. The ProQOL score is interpreted as high if the CS score is high, BO score is low, and STS score is average, as average if the score of all subscales is average, and as low if the CS score is low, BO score is high, and STS score is average.
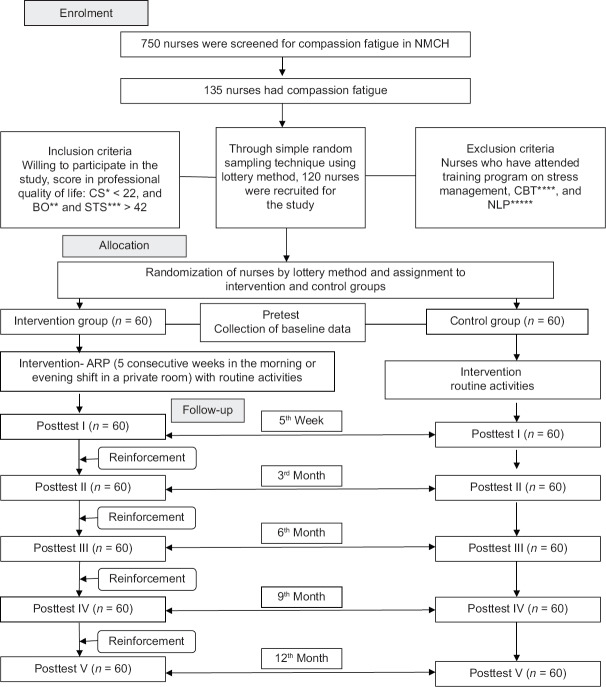
Content validity was obtained with the help of experts in the field of psychology and psychiatric nursing. Spearman-Brown prophecy formula was used to check the reliability of the tool; the reliability of the CS, BO, and STS subscales were 0.88, 0.75, and 0.81, respectively. Pretest data were collected at day 1, and posttest I, II, III, IV, V data were collected at 5th week, 3rd month, 6th month, 9th month, and 12th month using the ProQOL Scale [Figure 1].
Figure 1.
SPIRIT Flow chart of the Study (CS* Compassion satisfaction, BO**Burnout, STS***Secondary traumatic stress, CBT**** Cognitive-behavioural therapy, NLP***** Neuro-linguistic programming)
ARP is a consecutive 5-week program based on an individualized standard treatment protocol in 5 sessions, each lasting 90–120 min. The program involves didactic and experiential training along with audios. Session 1 focuses on the assessment of condition, life goals, conflicts, followed self-care strategies, stressors. The participants practice the guided imagery with the “retirement party visualization” script for 30 min. Session 2 focuses on developing a personal and professional time-line telling a story in which the participants narrate the achievement have had and hurdles have overcome in their life. Session 3 emphasizes a review of graphic time-line review and constructing the target/trigger list. Based on this, individualized self-management plans were developed and trained. In TFT, the troubling memories of participants were identified and tapping was conducted 5–8 times on the eyebrows, under the eye, beneath the armpit, on the collarbone, and the gamut series point located just above, and between the little and ring finger knuckles. In the NLP, safety and competency anchors were created, the negative anchors I and II were identified, and negative anchors were released through desensitization and reprocessing. Session 4 focuses on supervising the self; the “Letter from the Great Supervisor” is read and reread repeatedly, and then, introspected. Session 5 highlights the evaluation of program goals and addressing pathways for recovery.[15,16] The sessions were held once a week either in the morning or evening in a private room. The collected data were coded, grouped, and analyzed using the SPSS software (version 15; SPSS Inc., Chicago, IL, USA). Descriptive statistics including frequency, percentage, Mean (M), and Standard Deviation (SD), and the nonparametric Chi-square test, Wilcoxon signed-rank test, Mann-Whitney U test, and repeated measures ANOVA were used for analysis.
Ethical considerations
Permission to conduct the study was obtained from the Institutional Ethics Committee (IEC-NMCH-23/12/2013), Narayana Medical College, Director, Medical Superintendent, and Nursing Dean of Narayana Medical College Hospital. The nature and purpose of the study were explained to nurses and informed consent was obtained from all participants. Nurses in the intervention group received the 5-week intervention along with routine activities and received continuous reinforcement through telephone calls until the 12th month, whereas the control group only received routine activities.
Results
In both groups, nurses were in the age group of 21–30 years. Moreover, 80% of nurses were women, 71.70% were single, 56.70% had less than 1 year of experience, and 85% worked as a staff nurse. Furthermore, 58.30% of nurses lived in rural areas, 63.30% received support from their family, 48.30% listened to music as a coping strategy, 98.30% did not have a history of physical illness, 60% had dependent parents, and 96.70% had no history of recent loss.
Wilcoxon signed-rank test showed a statistically significant difference in mean CS, BO, and STS scores after the intervention in the intervention group compared to the control group [CS: (intervention group: p < 0.001), (control group: p < 0.01)], [BO: (intervention group: p < 0.001), (control group: p < 0.01)], [(STS: (intervention group: p < 0.001), (control group: p < 0.01)]. Mann-Whitney U test showed a statistically significant difference between the two groups after the intervention in terms of the CS, BO, and STS scores [(CS: p < 0.001), (BO: p < 0.001), (STS: p < 0.001)]. The effect of the intervention up to a period of 1 year was analyzed using repeated-measures ANOVA, which revealed a statistically significant difference within the intervention (p < 0.001) and control (p < 0.01) groups (CS: F1,59 = 125.96, 3.138), (BO: F1,59 = 178.37, 30.749), (STS: F1,59=389.09, 10.413) (and between the intervention and control groups (CS: F1,118=120.10, p < 0.001) (BO: F1,118=123.11, p < 0.001) (STS: F1,118=205.18, p < 0.001) [Tables 1–3].
Table 1.
Comparison of professional quality of life (compassion satisfaction) between the intervention and control groups (n=120)
| Duration of the study | Mean (SD*) |
MD** | Z*** | p | F****, p | |
|---|---|---|---|---|---|---|
| Intervention group (n=60) | Control group (n=60) | |||||
| Pretest | 20.67 (1.99) | 20.28 (1.51) | 0.39 | 0.85 | 0.390 | |
| Posttest I | 34.30 (7.66) | 19.85 (1.62) | 14.45 | 9.06 | 0.001 | |
| Posttest II | 35.87 (5.43) | 20.17 (1.25) | 15.70 | 9.08 | 0.001 | 120.102 |
| Posttest III | 37.37 (2.83) | 19.65 (1.49) | 17.72 | 9.59 | 0.001 | 0.001 |
| Posttest IV | 36.47 (2.82) | 19.53 (1.58) | 16.94 | 9.57 | 0.001 | |
| Posttest V | 35.50 (2.81) | 19.37 (1.77) | 16.13 | 9.61 | 0.001 | |
*SD: Standard deviation, **MD: Mean difference, ***Z: Wilcoxon signed-rank test, ****F: RM ANOVA
Table 3.
Comparison of professional quality of life (secondary traumatic stress) between the intervention and control groups (n=120)
| Duration of the study | Mean (SD) |
MD | Z | p | F, p | |
|---|---|---|---|---|---|---|
| Intervention group (n=60) | Control group (n=60) | |||||
| Pretest | 46.57 (1.69) | 45.97 (1.93) | -0.47 | 1.61 | 0.107 | |
| Posttest I | 35.40 (2.30) | 44.67 (1.83) | -9.27 | 9.59 | 0.001 | |
| Posttest II | 30.27 (3.78) | 45.03 (2.31) | -14.76 | 9.57 | 0.001 | |
| Posttest III | 32.82 (1.96) | 45.13 (0.87) | -12.31 | 9.6 | 0.001 | 205.17 |
| Posttest IV | 33.27 (2.31) | 44.50 (2.07) | -11.23 | 9.53 | 0.001 | 0.001 |
| Posttest V | 35.57 (1.60) | 43.68 (1.33) | -8.11 | 9.64 | 0.001 | |
Table 2.
Comparison of professional quality of life (burnout) between the intervention and control groups (n=120)
| Duration of the study | Mean (SD) |
MD | Z | p | F, p | |
|---|---|---|---|---|---|---|
| Intervention group (n=60) | Control group (n=60) | |||||
| Pretest | 45.72 (1.53) | 45.72 (1.53) | 0 | 0 | >0.999 | |
| Posttest I | 33.92 (2.78) | 43.57 (2.18) | -9.65 | 9.30 | 0.001 | |
| Posttest II | 36.08 (2.06) | 46.57 (1.69) | -10.49 | 9.53 | 0.001 | 123.11 |
| Posttest III | 35.65 (2.71) | 46.95 (1.76) | -11.30 | 9.61 | 0.001 | 0.001 |
| Posttest IV | 36.88 (3.08) | 46.13 (1.26) | -9.25 | 9.54 | 0.001 | |
| Posttest V | 35.6 (2.55) | 46.38 (1.47) | -10.78 | 9.56 | 0.001 | |
Discussion
The study findings indicate that the mean score of BO and STS significantly decreased and CS increased in the intervention group compared to the control group. ARP helps increase CS and reduce CF among nurses. The present study findings are consistent with that of the study conducted by Scarlet et al. on the effects of compassion cultivation training (CCT) (self-compassion skills, psycho-education, and 20 min of guided meditations) on BO and job satisfaction. They reported significant improvements in participants' self-compassion, mindfulness, and interpersonal conflict scores.[17] Daxesh et al. also reported that guided imagery is effective in reducing BO.[18] Bazarko et al. examined the effect of a novel telephone-adapted mindfulness stress reduction (MBSR) program on the health and well-being of nurses and reported an improvement in health, decrease in stress, decrease in work BO, and progress in other areas.[19]
Moreover, a 4-hour group seminar in educating and preventing CF was helpful for nurses working in the oncology unit as reported in Flarity et al. study. They found a statistically significant increase in CS (p = 0.004), decrease in BO (p = 0.001), and decrease in STS symptoms (p = 0.001) after the implementation of a multifaceted education program.[20] In a pilot study, Potter et al. found a CF resiliency program to be effective in lessening STS and improving job satisfaction. A 5-week (90 min) didactic program was found to be effective in reducing CF.[21] In the present study, the comparison of the mean scores between the intervention and control groups showed a statistically significant difference in CS (p < 0.050), BO (p < 0.010), and STS (p < 0.001). This could be due to the personality type of the nurses; they may have a natural inbuilt capacity to withstand the amount of stress and BO they undergo and effectively overcome it by using their coping mechanisms.
In the current study, there was a continuous follow-up until the end of 1 year, which proves that uninterrupted reinforcement and follow-up helps nurses to combat CF. A model program comprising of self-regulation, intentionality, and CF interventions seemed to be efficient in decreasing the symptoms of CF in the posttest at 3 and 6 months.[22] Several research reviews have studied only one intervention for the prevention and management of CF; however, the present study offers an intervention package for managing CF. The present study had some limitations. One limitation was that although it adopted an intervention package, the effect of each intervention was not assessed. Moreover, the researchers had no control over the support and counselling received from superiors, colleagues, and families. The control group also had an equal opportunity to receive support from others. This might have influenced the outcome of the study. Additional researches need to be conducted on larger populations to prove the efficacy of the ARP.
Conclusion
Regular practice of ARP can enhance CS and thus, reduce CF. A professional obligation exists for nurses to strengthen their CS and to prevent, recognize, and combat CF so that they can continue their work with the presence it deserves.
Financial support and sponsorship
Nil.
Conflicts of interest
Nothing to declare.
Acknowledgments
This article was derived from the thesis, with the Registration Number 4413030 of MAHER, Meenakshi University, Chennai, India. We greatly appreciate the cooperation of the authorities and the participation of nurses of Narayana Medical College Hospital, Andhra Pradesh, India, and the assistance of all those who helped us in this research.
References
- 1.Lombardo B, Eyre C. Compassion fatigue: A nurse's primer. Online J Issues Nurs. 2011;16:1–3. doi: 10.3912/OJIN.Vol16No01Man03. [DOI] [PubMed] [Google Scholar]
- 2.Yılmaz G, Ustun B. Professional quality of life in nurses: Compassion satisfaction and compassion fatigue. J Psychiatric Nurs. 2018;9:205–11. [Google Scholar]
- 3.Figley CR, Lovre C, Figley KR. Post-Traumatic Syndromes in Childhood and Adolescence: A Handbook of Research and Practice. London: Wiley-Blackwell; 2011. Compassion Fatigue, Vulnerability, and Resilience and in Practitioners Working with Traumatized Children; pp. 1–17. [Google Scholar]
- 4.Sacco TL, Ciurzynski SM, Harvey ME, Ingersoll GL. Compassion satisfaction and compassion fatigue among critical care nurses. Crit Care Nurse. 2015;35:32–42. doi: 10.4037/ccn2015392. [DOI] [PubMed] [Google Scholar]
- 5.Figley CR. Florida State University Traumatology Institute, Tallahassee, Florida. 2013. [Last accessed on 2019 Apr 10]. Available from: https://www.irest.us/
- 6.Beckstrand J, Yanchus N, Osatuke K. Only one burnout estimator is consistently associated with health care providers' perceptions of job demand and resource problems. Psychology. 2017;7:7. [Google Scholar]
- 7.Abendroth M, Flannery J. Predicting the risk of compassion fatigue: A study of hospice nurses. J Hosp Palliat Nurs. 2006;8:346–56. [Google Scholar]
- 8.Lee HF, Yen M. Nurse Burn out in Taiwan. J Nursing and Women's Healthcare. 2017:2. [Google Scholar]
- 9.Sean O'Mahony, James I Gerhart, Johanna Grosse, Ira Abrams, Mitchell M Levy. Posttraumatic stress symptoms in palliative care professionals seeking mindfulness training: Prevalence and vulnerability. Palliat Med. 2015;30:189–92. doi: 10.1177/0269216315596459. [DOI] [PubMed] [Google Scholar]
- 10.Melvin CS. Professional compassion fatigue: What is the true cost of nurses caring for the dying? Int J Palliat Nurs. 2012;18:606–11. doi: 10.12968/ijpn.2012.18.12.606. [DOI] [PubMed] [Google Scholar]
- 11.Kelly D, Kutney-Lee A, Lake ET, Aiken LH. The critical care work environment and nurse-reported health care-associated infections. Am J Crit Care. 2013;22:482–8. doi: 10.4037/ajcc2013298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nolte AG, Downing C, Temane A, Hastings-Tolsma M. Compassion fatigue in nurses: A meta synthesis. J Clin Nurs. 2017;26:4364–78. doi: 10.1111/jocn.13766. [DOI] [PubMed] [Google Scholar]
- 13.Smart D, English A, James J, Wilson M, Daratha KB, Childers B, et al. Compassion fatigue and satisfaction: A cross-sectional survey among US healthcare workers. Nurs Health Sci. 2014;16:3–10. doi: 10.1111/nhs.12068. [DOI] [PubMed] [Google Scholar]
- 14.Stamm BH. The Concise ProQOL Manual. 2nd ed. Sidran Press: Pocatello; 2010. pp. 1–55. [Google Scholar]
- 15.Baranowsky AB, Eric Gentry J. CFST Treatment Manual. 5th ed. Canada: Traumatology Institute; 2010. [Last accessed on 2013 Jan 02]. pp. 1–91. Available from http://www.psychink.com . [Google Scholar]
- 16.Baranowsky AB, Eric Gentry J. CFST Client Manual. 4th ed. Canada: Traumatology Institute; 2010. [Last accessed on 2013 Jan 02]. pp. 1–63. Available from: http://www.psychink.com . [Google Scholar]
- 17.Scarlet J, Altmeyer N, Knier S, Harpin RE. The effects of compassion cultivation training (CCT) on healthcare workers. Clin Psychol. 2017;21:116–24. [Google Scholar]
- 18.Patel DK, Suresh V., Mr Effectiveness of guided imagery on burnout syndrome among staff nurses working in Dhiraj General Hospital at Piparia, Vadodara. Int J Nurs Educ Res. 2016;4:764–5. [Google Scholar]
- 19.Bazarko D, Cate RA, Azocar F, Kreitzer MJ. The impact of an innovative mindfulness-based stress reduction program on the health and well-being of nurses employed in a corporate setting. J Workplace Behav Health. 2013;28:107–33. doi: 10.1080/15555240.2013.779518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Flarity K, Gentry JE, Mesnikoff N. The effectiveness of an educational program on preventing and treating compassion fatigue in emergency nurses. Adv Emerg Nurs J. 2013;35:247–58. doi: 10.1097/TME.0b013e31829b726f. [DOI] [PubMed] [Google Scholar]
- 21.Potter P, Deshields T, Berger JA, Clarke M, Olsen S, Chen L. Evaluation of a compassion fatigue resiliency program for oncology nurses. Oncol Nurs Forum. 2013;40:180–7. doi: 10.1188/13.ONF.180-187. [DOI] [PubMed] [Google Scholar]
- 22.National Hospice and Palliative Care Organization. Hospice action network. 2015. [Last accessed on 2019 Feb 15]. Available from: http://www.nhpco.org/sites/default/files/public/communications/Outreach/The_Medicare_Hospice_Benefit.pdf .