Abstract
Background:
Preterm birth is increasing as a major cause of perinatal complications and mortality in Iran. The present study aimed to investigate the effect of prenatal self-care based on Orem's theory on preterm birth occurrence in women at risk for preterm birth.
Materials and Methods:
The present clinical trial was conducted on 176 pregnant women at 24–26 weeks at risk for preterm birth in Mashhad, Iran, from December 2015 to October 2016. A multistage sampling method was used in this study. The intervention group (88 pregnant women) received individual self-care education but the control group (88 pregnant women) received only common prenatal care.
Results:
There was a statistically significant difference between intervention and control groups in terms of preterm birth occurrence (6.80% vs 20.50%) (χ2 = 6.90, df = 1,p = 0.008). The incidence of preterm birth in the intervention group was approximately three times higher than that in the control group.
Conclusions:
Given that educational interventions could reduce the incidence of preterm birth, it is suggested that the women at risk for preterm birth are trained for prenatal self-care.
Keywords: Iran, premature birth, self care
Introduction
According to the World Health Organization (WHO), preterm labor is defined as giving birth before 37 weeks (259 days) from the 1st day of the last menstruation.[1] Preterm birth affects approximately 11% of births worldwide.[2] Preterm birth has increased in Iran from 6.7% in 1996 to 12.1% in 2000 and 16.4% in 2003.[3] Preterm birth is a major cause of perinatal morbidity and mortality.[4] According to the findings of various studies, the poverty, maternal age of under 20 and over 36 years, short interval between pregnancies, preeclampsia, addiction, some drugs,[5] malnutrition,[6] hyperemesis gravidarum,[7] infection, inflammation,[8] and maternal body mass index affect the incidence of preterm birth.[9] The social support, relationships, and self-care have also been considered as factors involved in the incidence of preterm birth.[10] The self-care program for pregnant women is an effective way to prevent preterm birth and is recommended for all pregnant women.[11] Self-care is the care undertaken by individuals to improve life, health, and well-being.[12,13] Orem's self-care theory is one of the most important theories on self-care education.[14] There are three types of self-care requisites including universal self-care requisites, developmental self-care requisites, and health deviation self-care requisites.[13,15] Universal self-care requisites are found in all humans and are associated with processes of individuals' lives and general welfare.[16] Universal self-care deficits in pregnancy include malnutrition in pregnancy,[6] alcohol usage, drug use, inadequate intake of healthy air in situations where there is smoking,[17] ambient poisons,[5] sulfur dioxide,[18] imbalance between activity and rest such as prolonged standing and walking,[19] intense physical activity and night work,[20] occupational tiredness,[10] risks for pregnant women during pregnancy such as hitting,[21] anxiety,[22] depression,[23] stress, and lack of social support and relationships.[5] These cases are among the predisposing factors for the incidence of preterm birth. Developmental self-care requisites emerge at different stages of life including adolescence, pregnancy, and aging.[16] Developmental self-care deficits during pregnancy include short interval between pregnancies,[3] number of pregnancies, inappropriate weight gain during the pregnancy, and lack of adequate prenatal care which are associated with an increased risk of preterm birth.[5] Health deviation self-care requisites occur due to diseases, genetic and physical defects, and structural and functional deviations in humans.[16] Health deviation self-care deficits in pregnancy include medical and obstetric diseases including bacterial vaginosis,[24] anemia,[25] short cervical length,[26] pyelonephritis, preeclampsia, oligohydramnios, polyhydramnios, placenta previa, third-trimester hemorrhage, anatomic abnormality of uterus, diabetes mellitus, thyroid dysfunction, and cardiac disease of mothers,[5] which could also be associated with preterm birth. Evidence shows that pregnant women's lifestyles including their self-care could be related to the preterm birth occurrence.[10] Therefore, it seems that teaching self-care to mothers who are at risk for preterm birth can reduce the incidence of preterm birth.[27] However, there are some other reports that do not confirm the significant relationship between lifestyle and prenatal care with preterm birth.[28] This controversy suggests the need for further studies on the impact of self-care on the incidence of preterm birth.
Given the importance of preterm birth as well as the significance of self-care in pregnant mothers and the lack of access to available evidence about the effect of self-care behaviors on the incidence of preterm birth in Iran, this study sought to investigate the effect of prenatal self-care based on Orem's theory on preterm birth occurrence in Iranian women at risk for preterm birth.
Materials and Methods
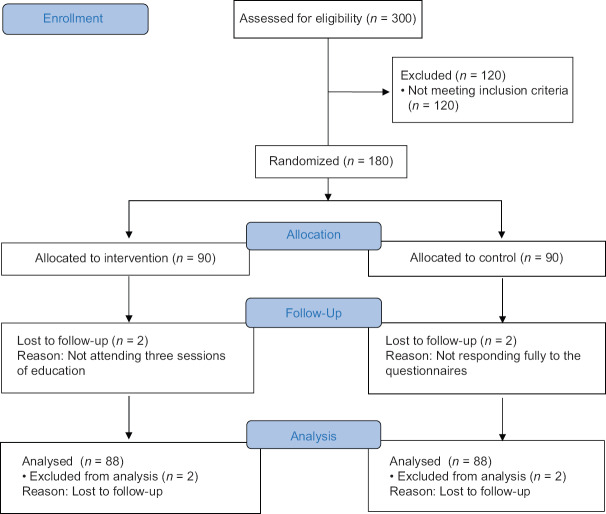
The present clinical trial study (IRCT2015122225659N1) was derived from a master thesis in Midwifery and it was performed on 176 pregnant women at risk for preterm birth (88 participants in the intervention group and 88 participants in the control group) in Mashhad, Iran, from December 2015 to October 2016. The participants consisted of all pregnant women at risk for preterm birth referring to health centers affiliated to Mashhad University of Medical Sciences, Mashhad, Iran. The inclusion criteria included: being Iranian and resident of Mashhad; having at least reading and writing literacy for understanding and answering the questions; willingness to participate in the study; gestational age of 24–26 weeks based on the accurate and reliable Last Menstrual Period (LMP) or ultrasound results at the first 3 months of pregnancy; score 10 or more in Holbrook's preterm delivery screening questionnaire; no speech, hearing, or accent disorder which prevent communication with the researcher; and previous or current incidence of psychological problems. Exclusion criteria at the end of the study were as follows: not attending three sessions of education and not responding fully to the questionnaires. Results of the pilot study on 30 pregnant women (15 participants in each group) and a formula for comparing means were used at 95% confidence interval, 80% test power, Z1-α/2=1.96, Z1-β=0.84, X1=38, X2=37, S1=1 and S2=3 in order to estimate sample size due to the lack of similar study. The sample size was 78 in each group and 156 in total. The final sample size was determined by adding 15% (90 participants in each group and 180 in total) to compensate for dropout [Figure 1]. A multistage sampling method was used in this study. The five main urban health centers and 180 smaller subsidiary health centers were determined as the sampling frame. The five main urban health centers were selected using stratified random sampling, and then subsidiary health centers were selected using cluster sampling. In each center, the subjects were selected conveniently. A total of 24 health centers were selected, from which 12 centers were assigned to the intervention group and 12 ones to the control group.
Figure 1.
CONSORT flow diagram
The data collection instruments included a questionnaire for demographic and obstetric characteristics, the Holbrook's preterm delivery screening questionnaire, and the Hart Prenatal Care Actions Scale (HPCAS). The questionnaire for demographic and obstetric characteristics included 26 questions that were completed by the subjects at the beginning of the study. The Holbrook's preterm delivery screening questionnaire included three sections: risk factors, sub-risk factors, and underlying risk factors. The first section consisted of 14 questions, the second section includes 14 questions, and the third section comprised 12 questions. The first section questions receive score 10, the second section receives score 5, and the third section receives score 2.5. If individuals scored 10 or more, they were considered as a high-risk group, and if they scored lower than 10, they were considered as a low-risk group for the preterm birth.[27] HPCAS was developed by Hart. HPCAS consisted of 41 items that were derived from the universal self-care requisites and articulate the guidelines for prenatal care.[21] HPCAS is a Likert type scale with five responses ranging from “never” to “always.” Scores can range from 41 to 205 with a higher score indicating increased engagement in prenatal care actions.[21] The validity of this questionnaire was approved by Sea-han.[29] The Farsi version of HPCAS (passing the translation and back-translation process by professional translators) was also validated through the content validity in the present study. The reliability of HPCAS was confirmed with a Cronbach's alpha of 80% by Sae-han.[29] The reliability of the Farsi HPCAS was estimated to be 76.20% using Cronbach's alpha formula.
The entire sampling process lasted 11 months. To recruit the participants, firstly, objectives and methods of the study and the issue of confidentiality were explained to the participants. Written consent was also obtained from the participants before taking part in the study. Then, eligible participants completed the preterm labor screening questionnaire and those scoring 10 or higher were allocated to the intervention group (mothers at risk of preterm birth undergoing self-care education) and control group (mothers at risk of preterm birth undergoing common prenatal care during pregnancy). In the next step, the personal and midwifery characteristics questionnaire and HPCAS were completed by them. Educational needs of the intervention group were evaluated based on the HPCAS, and then the necessary training was provided in three 45–60-minute sessions in 3 consecutive weeks individually and face-to-face. After the training, training cards were given to the subjects in the intervention group based on each individual's needs. Educational content was designed based on the Orem's self-care theory. It contained universal self-care requisites including adequate nutrition, fluid intake, drinking milk, avoidance of drinking coffee and alcohol, healthy air intake, avoidance of smoking, balance between activity and rest, enough sleeping, physical risk prevention, avoiding of stress, anxiety and depression, social support and relationships of pregnant women at risk for preterm labor. Also it contained developmental self-care requisites including regular visits to health centers or physicians for prenatal care, proper weight gain in pregnancy, intake of prescribed prenatal vitamins and iron tablets; and health deviation self-care requisites including bleeding in pregnancy, premature uterine contractions, pyelonephritis, periodontitis, bacterial vaginosis, preeclampsia, oligohydramnios, polyhydramnios, diabetes, placenta previa, anatomic abnormality of uterus and history of organic disorder (cardiac, renal, thyroid), risk factors for pregnancy and their relationships with preterm birth. Participants were given two HPCASs to complete before the second and third sessions of the training based on their self-care behaviors during the last week and hand it over to the researcher. At the end of the third session, the general content of education was given to them as pamphlets. The control group received only the usual prenatal care by the midwife of the health center. The control group also completed HPCAS for 2 consecutive weeks and delivered it to the researcher. Until the 40th week, the researcher contacted the intervention and control groups via telephone to inform them about the process of pregnancy, delivery, or lack of delivery. The researcher's phone number was given to all participants and all (those in intervention and control groups) were requested to contact the researcher if they went to the hospital and were hospitalized for delivery. The researcher then asked the participants in the postpartum period to come to health centers and again complete HPCAS. Finally, the educational content was also provided to the control group. Data analysis were done using statistical software (version 18 SPSS Inc, Chicago, IL, USA). In order to investigate the homogeneity of the two groups, Chi-square and exact Chi-square tests were used. The independent samples t-test and Mann-Whitney U test were used to compare the intervention and control groups in terms of length of pregnancy. Chi-square was used to estimate the effect of prenatal self-care on preterm birth occurrence. Statistical significance was set at p ≤ 0.05.
Ethical considerations
The present research was conducted after gaining approval by the research deputy as well as the Ethics Committee of Mashhad University of Medical Sciences, Mashhad, Iran and obtaining a letter of recommendation from the Faculty of Nursing and Midwifery of Mashhad and presenting it to the authorities of health centers. The approved code of the ethics committee was IR.MUMS.REC.1394.448.
Results
The mean (SD) age of participants was 28.61 (6.21) years in the intervention group and 28.38 (6.62) years in the control group, but there was no significant difference between the two groups (p = 0.861). With regard to the education level, 38 (43.20%) women in the intervention group and 39 (44.30%) in the control group had a high school diploma and the difference between the two groups was not statistically significant (p = 0.68). Furthermore, most of the subjects in the intervention 62 (70.50%) and control group 61 (69.30%) had sufficient income (p = 1.00). The mean age, husband's age and length of marriage based on results of the independent t-test, and the frequency of husband's education, occupation, husband's job, family income, insurance, insurance type, and housing status based on results of the Chi-square test were not significantly different in between the two groups (p > 0.05). There was no statistically significant difference between the two groups in term of number of pregnancies, number of deliveries, number of abortions, number of preterm deliveries, number of live children, number of dead children, number of stillbirths, and interval of current and previous pregnancy (p > 0.05) [Table 1]. Most of the participants in the intervention 57 (64.80%) and control 50 (56.80%) groups had no history of self-care education in pregnancy (p = 0.28). Also, most of the participants (59 [67.00%]) in the intervention and 57 (64.80%) control groups had little information about preterm birth and self-care activities during pregnancy (p = 0.596). There was no significant difference between two groups in terms of the history of self-care education in pregnancy, self-care education resources, information on preterm birth and self-care activities, and interest in learning about complications of preterm birth (p > 0.05). But, there were significant differences between the two groups in terms of interest in learning about symptoms of preterm birth and self-care activities (χ2 = 9.94, df = 2, p < 0.05). Therefore, comparisons between the intervention and control groups in terms of interest in learning about symptoms of preterm birth and self-care activities were carried out using analysis of covariance. The results showed that removing these variables does not change the outcome of the study, and yet significant differences existed between the two groups (p < 0.001). There was no statistically significant difference between the two groups in terms of self-care during pregnancy before the intervention (p = 0.899).
Table 1.
Comparison of mean scores midwifery characteristics between two groups
| Intervention group mean (SD) | Control group mean (SD) | t | df | p | |
|---|---|---|---|---|---|
| Number of pregnancies | 2.60 (1.67) | 2.48 (1.41) | 0.39 | 174 | 0.93 |
| Number of deliveries | 1.00 (1.13) | 0.86 (0.88) | 0.51 | 174 | 0.98 |
| Number of abortions | 0.60 (0.97) | 0.59 (0.90) | 0.00 | 174 | 0.89 |
| Number of preterm labor | 0.21 (0.49) | 0.28 (0.47) | -1.05 | 174 | 0.20 |
| Number of live children | 0.75 (0.93) | 0.70 (0.82) | 0.65 | 174 | 0.77 |
| Number of dead children | 0.07 (0.31) | 0.15 (0.45) | -0.76 | 174 | 0.47 |
| Number of stillbirths | 0.05 (0.23) | 0.02 (0.14) | 1.15 | 174 | 0.24 |
| Interval of current and previous pregnancy (year) | 5.25 (3.91) | 3.95 (4.40) | 0.40 | 119 | 0.61 |
Based on the independent samples t-test, the length of pregnancy was significantly different between the two groups (t174 =2.18, p = 0.03). In other words, the duration of pregnancy was significantly longer in the intervention group [Table 2].
Table 2.
Comparison of mean scores of length of pregnancy between two groups
| Intervention group mean (SD) | Control group mean (SD) | t | df | p | |
|---|---|---|---|---|---|
| Duration of pregnancy (week) | 38.97 (1.45) | 38.27 (2.61) | 2.18 | 174 | 0.030 |
According to Chi-square test, there was a significant difference between two groups in the prevalence of preterm birth (χ2 = 6.94, df = 1, p = 0.008); six cases (6.80%) in the intervention group and 18 cases (20.50%) in the control group had a preterm birth. Furthermore, 82 (93.20%) women in the intervention group and 70 (79.50%) in the control group didn't have preterm birth [Table 3]. Also, based on the results of multiple linear regression test to investigate the role of demographic and obstetric characteristics (age of mothers, education, income, job, husbands job, housing status, insurance type, number of pregnancies, number of deliveries, number of abortions, number of preterm births, number of alive children, number of dead children, number of stillbirths, interval of current and previous pregnancy, history of self-care education, interest in learning about complications of preterm birth, interest in learning about symptoms of preterm birth, and self-care activities) on the effect of prenatal self-care education based on Orem's theory on preterm birth occurrence, none of them had significant linear regression with preterm birth (p > 0.05) [Table 4].
Table 3.
Frequency of preterm birth incidence in two groups
| Intervention group n (%) | Control group n (%) | Total n (%) | χ2 | Chi-square df | p | |
|---|---|---|---|---|---|---|
| Preterm birth | ||||||
| Yes | 6 (6.80%) | 18 (20.50%) | 24 (13.60%) | 6.94 | 1 | 0.008 |
| No | 82 (93.20%) | 70 (79.50%) | 152 (86.40%) | |||
| Total | 88 (100.00%) | 88 (100.00%) | 176 (100.00%) |
Table 4.
Role of demographic and obstetric characteristics on the effect of prenatal self-care based on Orem’s theory on preterm birth occurrence in women at risk for preterm birth
| Beta | Std. Error | Linear regression t | p | |
|---|---|---|---|---|
| Constant | 2.90 | 490 | 5.93 | <0.001 |
| Age of mothers | −0.01 | 0.00 | −1.46 | 0.14 |
| Education | −0.02 | 0.03 | −0.72 | 0.47 |
| Income | 0.04 | 0.08 | −0.58 | 0.55 |
| Job | 0.06 | 0.06 | 0.99 | 0.32 |
| Husbands job | 0.00 | 0.04 | 0.00 | 0.99 |
| Insurance type | −0.31 | 0.16 | −1.87 | 0.06 |
| Housing status | −0.01 | 0.02 | −0.48 | 0.62 |
| Number of pregnancies | −0.07 | 0.37 | −0.19 | 0.84 |
| Number of deliveries | −0.19 | 0.43 | −0.44 | 0.66 |
| Number of abortions | 0.09 | 0.37 | 0.24 | 0.80 |
| Number of preterm labor | −0.04 | 0.07 | −0.61 | 0.54 |
| Number of alive children | 0.34 | 0.57 | 0.59 | 0.55 |
| Number of dead children | 0.31 | 0.56 | 0.56 | 0.57 |
| Number of stillbirths | 0.38 | 0.54 | 0.71 | 0.47 |
| Interval of current and previous pregnancy (Year) | −0.02 | 0.05 | −0.74 | 0.38 |
| History of self-care education | −0.08 | 0.06 | −1.31 | 0.19 |
| Interest in learning about complications of preterm birth | 0.06 | 0.07 | 0.80 | 0.42 |
| Interest in learning about symptoms of preterm birth and self-care activities | −0.09 | 0.07 | −1.23 | 0.22 |
Discussion
The results of the study showed that using self-care education based on Orem's theory leads to the increased length of pregnancy and proximity of delivery to the term and in fact, reduced incidence of preterm birth. In other words, the incidence of preterm birth in the control group was approximately three times higher than that in the intervention group. In terms of the effect of self-care on the preterm birth, results of the present study were consistent with studies by Rajaeefard et al.,[27] Avelyn,[12] Kamalifard et al.,[10] and Bostani-Khalesi et al.[30] Rajaeifard et al. (2010) conducted a study to determine the risk factors of preterm delivery and the effects of education on its prevention on 1,117 pregnant women with less than 37 weeks of pregnancy referring to maternal and child health units in 36 health centers of Shiraz, Iran. They could reduce the incidence of preterm labor by identifying pregnant women at risk for preterm labor through Holbrook's preterm delivery screening and teaching them the importance, symptoms, and principles of preterm labor prevention during the pregnancy.[27] Results of research by Bostani-Khales et al. (2013) with the aim of studying “the relationship between prenatal care utilization index and neonatal outcomes” on 205 pregnant women referring to health care centers of Rasht, Iran indicated that the greater prenatal care and subsequently educating pregnant mothers to decrease the incidence of preterm labor.[30] Kamalifard et al. (2010) investigated the effect of lifestyle on the rate of preterm birth in 132 women with a history of preterm labor and 264 women without any history of preterm labor. They studied the lifestyle variables including nutrition, smoking, consumption of alcohol and invalid drugs, social relationships, stress, and self-care and concluded that women with term delivery had a better lifestyle than those with preterm labor.[10] Finally, Avelyn (2012) investigated the relationship between prenatal self-care practices during pregnancy and birth outcomes among 80 young mothers aged 16–24 at Gweru maternity hospital of Zimbabwe and found that self-care during the pregnancy based on Orem's theory increases the duration of pregnancy and reduces the preterm labor.[12]
According to Orem's educational support system, when a patient has the capacity but needs help for learning or doing things, decision-making, selecting methods, and using specific knowledge or skills, nurses take on the role of counselor to help the patients do the self-care activities.[16] Therefore, the researcher, as a counselor, taught self-care activities during pregnancy and dependent-care activities (fetus) to pregnant mothers at risk for preterm birth based on mother's self-care requisites and the dependent-care requisites (fetus). According to Orem's assumptions, humans have the power to think, reason, and take responsibility, and they can take care of themselves and have acceptable performance. As a result, mothers at risk for preterm birth considered themselves self-care agents and dependent-care agents for their fetus to promote self-care behaviors[31] and improve pregnancy outcomes for their fetuses (increase the length of pregnancy and reduce the incidence of preterm birth and its complications) after becoming aware of self-care behavior and dependent-care activities (fetus) associated with preterm birth. Finally, it led to an increase in the length of pregnancy and a decrease in the incidence of preterm birth in the intervention group compared to the control group.
However, the results of the present study were inconsistent with the results of a study by Lotfalizadeh et al. (2005) on the effect of self-care on the duration of pregnancy and preterm birth. They conducted a cross-sectional study to measure the prevalence and risk factors of preterm labor in 600 participants (300 with preterm deliveries and 300 with term deliveries) at Imam Reza Hospital, Mashhad, Iran. Results of their study showed that smoking, maternal medical status, and type of prenatal care are significantly related to preterm labor.[28] Tobacco use is a variable of Orem's universal self-care requisites during pregnancy; the prenatal care method is a variable of Orem's developmental self-care requisites during pregnancy, and the maternal medical status is a variable of Orem's health deviation self-care requisites in the pregnancy. According to Lotfalizadeh, none of the above variables were associated with the preterm labor, and thus their research was inconsistent with the present study. The reason for different effects of prenatal care on the length of pregnancy and the incidence of preterm labor could be due to differences in types of data collection instruments, design of the study, and their implementation methods between studies. In a study by Lotfalizadeh, type of pregnancy care measured based on interview and patient records did not show any significant relationship with preterm labor. However, the current study showed that self-care, assessed using the HPCAS, had a significant relationship with the length of pregnancy and preterm labor. The differences in designs of studies could be the main reason for the difference between the results of the study by Lotfalizadeh and the present study.
The advantage of this study was that it was based on Orem's self-care theory, which is one of the most important theories. This study focused on all universal, developmental, and health deviation self-care requisites during pregnancy to reduce the incidence of preterm birth. Also, according to the first HPCAS, the educational needs of each mother were evaluated and the researcher emphasized their needs and in the following weeks, based on how to respond in this questionnaire, the researcher determined whether the training had been able to meet the mother's need. In this study, mothers were taught how each of the factors affecting the incidence of preterm labor can lead to preterm birth. Finally, mothers gained the awareness that how they can take care of themselves in order to prevent preterm birth. The present study faced limitations such as ignoring the individual differences and mental status of the participants. Not being able to closely monitor on self-care activities and to use HPCAS as a self-report that was trusted to the research units' responses. Some of the factors affecting preterm birth, including racial-ethnic differences and genetic factors, were out of the control of the researcher.
Conclusion
Given the effect of prenatal self-care based on Orem's theory on preterm birth occurrence in women at risk for preterm birth, it is suggested pregnant women at risk for preterm birth are identified and provided with them self-care education in health care centers in order to increase the length of pregnancy and reduce the incidence of preterm birth.
Financial support and sponsorship
Mashhad University of Medical Sciences, Mashhad, Iran
Conflicts of interest
Nothing to declare.
Acknowledgments
The present paper was extracted from a master thesis in Midwifery in Mashhad University of Medical Sciences, Mashhad, Iran with the identification number of 940364. We are deeply grateful to the research deputy of Mashhad University of Medical Sciences for sponsoring the project. We also thank the authorities of healthcare centers affiliated to Mashhad University of Medical Sciences and all the participants for their cooperation.
References
- 1.Romero R, Dey SK, Fisher SJ. Preterm labor: One syndrome, many causes. Science. 2014;345:760–5. doi: 10.1126/science.1251816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vogel J, Chawanpaiboon S, Moller A, Watananirun K, Bonet M, Lumbiganon P. The global epidemiology of preterm birth. Best Pract Res Clin Obstet Gynaecol. 2018;52:3–12. doi: 10.1016/j.bpobgyn.2018.04.003. [DOI] [PubMed] [Google Scholar]
- 3.Mehran N, Abbaszadeh F, Bagheri A. Relationship physical activity with preterm labor. Qom Univ Med Sci J. 2012;6:17–22. [Google Scholar]
- 4.Wu W, Witherspoon DJ, Fraser A, Clark EA, Rogers A, Stoddard GJ, et al. The heritability of gestational age in a two-million member cohort: Implications for spontaneous preterm birth. Hum Genet. 2015;134:803–8. doi: 10.1007/s00439-015-1558-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nabavizadeh SH, Ghaffarian Shirazi HR, Ghaffari P, Karshenas N, Zoladi M. Retrospective study of factors related to preterm labor in Yasuj, Iran. IJGM. 2012;5:1013–7. doi: 10.2147/IJGM.S33385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Triunfo S, Lanzone A. Impact of maternal under nutrition on obstetric outcomes. J. Endocrinol. 2015;38:31–8. doi: 10.1007/s40618-014-0168-4. [DOI] [PubMed] [Google Scholar]
- 7.Da Silva Lopes K, Ota E, Shakya P, Dagvadorj A, Balogun O, Pena-Rosas J, et al. Effect of nutrition interventions during pregnancy on low birth weight: An overview of systematic reviews. BMJ Glob Health. 2017;2:e000389. doi: 10.1136/bmjgh-2017-000389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peled Y, Melamed N, Hiersch L, Pardo J, Wiznitzer A, Yogev Y. The impact of total parenteral nutrition support on pregnancy outcome in women with hyperemesis gravidarum. J Matern Fetal Neonatal Med. 2014;27:1146–50. doi: 10.3109/14767058.2013.851187. [DOI] [PubMed] [Google Scholar]
- 9.Agrawal V, Jaiswal MK, Mallers T, Katara GK, Gilman-Sachs A, Beaman KD, et al. Altered autophagic flux enhances inflammatory responses during inflammation-induced preterm labor. Sci Rep. 2015;5:9410. doi: 10.1038/srep09410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kamali Fard M, Alizadeh R, Sehati Shafaei F, Gojazadeh M. The effect of lifestyle on the rate of preterm birth. J Ardabil Univ Med Sci. 2010;10:55–63. [Google Scholar]
- 11.Saling E, Drager M. Program for prevention of a considerable number of premature births. DSJUOG. 2008;2:48–56. [Google Scholar]
- 12.Avelyn G. The relationship between prenatal self- care practices during pregnancy and birth outcomes among young mothers aged 16 to 24 years delivering at Gweru Maternity hospital, MD Dissertation, Health Sciences Faculty of University of Zimbabwe. 2012 [Google Scholar]
- 13.Nazik E, Eryilmaz G. The prevention and reduction of post partum complications: Orem's model. Nurs Sci Q. 2013;26:360–4. [Google Scholar]
- 14.Rafieefar Sh AM, Ahmadzadeh Asl M. Comprehensive System of Empowering People to Take Care of their Health. 1st ed. Tehran: Mehrravash; 2006. pp. 30–40.pp. 57–84. Persian. [Google Scholar]
- 15.Rezaeean SM, Abedian Z, Latifnejad Roudsari R, Mazloom SR, Dadgar S. The relationship of prenatal self-care behaviors with stress, anxiety and depression in women at risk of preterm delivery. IJOGI. 2017;20:68–76. [Google Scholar]
- 16.Meleis A. Theoretical Nursing Development and Progress. 5th ed. Pennsylvania: Wolters Kluwer Health | Lippincott Williams and Wilkins; 2012. pp. 207–28. [Google Scholar]
- 17.Mahmoudzadeh Zarandi F, Raiesifar A, Ebadi A. The effect of Orem's self-care model on quality of life in patients with migraine: A randomized clinical trial. Acta Med Iran. 2016;54:159–64. [PubMed] [Google Scholar]
- 18.Mei-Dan E, Walfisch A, Weisz B, Hallak M, Brown R, Shrim A. The unborn smoker: Association between smoking during pregnancy and adverse perinatal outcomes. J Perinat Med. 2015;43:553–8. doi: 10.1515/jpm-2014-0299. [DOI] [PubMed] [Google Scholar]
- 19.Mivane F, Entezari A, Khadem N, Shojaee T. Modeling the seasonal pattern of preterm labors. IJOGI. 2016;18:12–20. [Google Scholar]
- 20.Dalili M, Karimzadeh Meybodi MA, Ghaforzadeh M, Farajkhoda T, Molavi-E Vardanjani H. Screening of preterm labor in Yazd city: Transvaginal ultrasound assessment of the length of cervix in the second trimester. Iran J Reprod Med. 2013;11:279–84. [PMC free article] [PubMed] [Google Scholar]
- 21.Hart MA. Orem's self-care deficit theory: Research with pregnant women. Nurs Sci Q. 1995;8:120–6. doi: 10.1177/089431849500800307. [DOI] [PubMed] [Google Scholar]
- 22.Neshat R, Majlesi F, Rahimi A, Shariat M, Poorreza A. Relationship between preterm birth with anxiety, stress and depression during pregnancy referring to health centers in the city Dorud in1389. IJOGI. 2013;16:16–24. [Google Scholar]
- 23.Staneva A, Bogossian F, Pritchard M, Wittkowski A. The effects of maternal depression, anxiety, and perceived stress during pregnancy on preterm birth: A systematic review. Women Birth. 2015;28:179–93. doi: 10.1016/j.wombi.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 24.Tavana Z, Zolghadri Zh, Hadaegh MJ, Pourdast T. The effect of treatment of bacterial vaginosis on pregnancy outcome. IJOGI. 2010;13:1–7. [Google Scholar]
- 25.Seifi M, Farshbaf Khalili A, Aghayi H, Poorzinali S. The relationship of iron deficiency anemia with preterm delivery in pregnant women referred to health centers of Tabriz. IJOGI. 2015;18:8–17. [Google Scholar]
- 26.Di Renzo GC, Roura LC, Facchinetti F, Antsaklis A, Breborowicz G, Gratacos E, et al. Guidelines for the management of spontaneous preterm labor: Identification of spontaneous preterm labor, diagnosis of preterm premature rupture of membranes, and preventive tools for preterm birth. J Matern Fetal Neonatal Med. 2011;24:659–67. doi: 10.3109/14767058.2011.553694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rajaee Fard A, Mohammadi BA, Mohammadi M, Jolaee H, Alipour H. Evaluation of risk factors in preterm delivery and impact of education in its prevention. Sci Res J Shahed Univ. 2010;17:1–9. [Google Scholar]
- 28.Lotfalizadeh M, Mohamadzadeh A, Kamandi Sh, Bagheri S. Prevalence and risk factors of preterm labor in Imam Reza hospital. IJOGI. 2005;8:93–100. [Google Scholar]
- 29.Sea-han CH. Effects of depression on learned resourcefulness and prenatal self-care practices in pregnant women with and without HIV seropositivity in Thailand, PHD Dissertation, Nursing Faculty of Case Western Reserve University. 2002 [Google Scholar]
- 30.Bostani Khalesi Z, Rafat F. Relationship between adequacy of prenatal care utilization index and neonatal outcomes. Holistic Nurs Midwifery J. 2015;25:8–15. [Google Scholar]
- 31.Rezaeean SM, Abedian Z, Latifnejad Roudsari R, Mazloom SR, Dadgar S. Application of Orem's theory for promotion of self-care behaviors of pregnant women at risk for preterm delivery: A clinical trial. IJOGI. 2017;20:68–77. [Google Scholar]