Abstract
Purpose
Traditional critical care dogma regarding the benefits of early tracheostomy during invasive ventilation has had to be revisited due to the risk of COVID-19 to patients and healthcare staff. Standard practises that have evolved to minimise the risks associated with tracheostomy must be comprehensively reviewed in light of the numerous potential episodes for aerosol generating procedures. We meet the urgent need for safe practise standards by presenting the experience of two major London teaching hospitals, and synthesise our findings into an evidence-based guideline for multidisciplinary care of the tracheostomy patient.
Methods
This is a narrative review presenting the extensive experience of over 120 patients with tracheostomy, with a pragmatic analysis of currently available evidence for safe tracheostomy care in COVID-19 patients.
Results
Tracheostomy care involves many potentially aerosol generating procedures which may pose a risk of viral transmission to staff and patients. We make a series of recommendations to ameliorate this risk through infection control strategies, equipment modification, and individualised decannulation protocols. In addition, we discuss the multidisciplinary collaboration that is absolutely fundamental to safe and effective practise.
Conclusion
COVID-19 requires a radical rethink of many tenets of tracheostomy care, and controversy continues to exist regarding the optimal techniques to minimise risk to patients and healthcare workers. Safe practise requires a coordinated multidisciplinary team approach to infection control, weaning and decannulation, with integrated processes for continuous prospective data collection and audit.
Keywords: Tracheostomy care, COVID, Multidisciplinary, Novel coronavirus
Introduction
The COVID-19 pandemic has resulted in unprecedented numbers of patients being admitted to intensive care units (ICUs) with additional capacity created in many hospitals all over the world to meet this overwhelming demand [1]. Approximately 70% of patients admitted to ICU require mechanical ventilation with a median length of stay of 13 days (IQR 7–19 days) [2]. Tracheostomy is often performed by critical care physicians to facilitate ventilatory wean when mechanical ventilation is prolonged (7–10 days) [3, 4]. A significant number of patients admitted with COVID-19 are therefore expected to require tracheostomies as a result of this pandemic [5, 6].
The benefits of tracheostomy include the ability to wean sedation, facilitate gradual reduction in ventilatory support, improve communication, participate in rehabilitation, reduce dead space, facilitate bronchial toilet, and potentially reduce long-term complications such as vocal cord granuloma formation, subglottic stenosis and scarring [7, 8]. However, there are also recognised complications and risks to the procedure which may be more challenging to manage in the current pandemic situation.
COVID-19 spreads primarily through contact and droplet routes so careful attention to infection control during tracheostomy management is of paramount importance to prevent cross-contamination between patients and medical staff. The risk of transmission may be increased by aerosolisation of particles [9, 10]. Airway management by healthcare workers (HCW) involves manoeuvres which are recognised as aerosol generating procedures (AGPs), and as such may present a significant risk of COVID-19 transmission [10]. Recognised AGPs related to tracheostomy care are summarised in Table 1 [9–14].
Table 1.
Aerosol generating procedures in tracheostomy care
| Aerosol generating procedures related to tracheostomy care |
|---|
| Open suction of the respiratory tract |
| Tracheostomy-related insertion, decannulation and care procedures |
| Induction of sputum |
| Fiberoptic examination of the nasal cavity and upper respiratory tract |
| Bronchoscopy |
| Tracheostomy tube changes |
| Cycling between ventilator-free and supportive mechanical ventilation during weaning |
| Changing heat and moisture exchange filters |
Despite the increasing demand, there has been little time and experience to develop a robust evidence-based guide to the indications, timing, technique and delivery of tracheostomy care for patients with COVID-19. Such guidance is essential to provide the best standard of care, particularly as health care professionals re-deployed into ICU to manage the surge in patient volumes may lack relevant expertise.
We respond to this urgent need by presenting our experience of caring for newly tracheotomised patients treated for COVID-19 pneumonitis, with emphasis in the tracheostomy care and the process of weaning and decannulation. This represents the cumulative experience of the two largest South London tertiary referral teaching hospitals at the epicentre of the COVID-19 pandemic, serving a population of over 4 million people in the UK. The aim of this paper is to review our early experience, provide evidence and the rationale underpinning our approach, and ultimately provide a clinical practice guideline to optimise patient care in newly tracheotomised patient as a result of COVID-19 infection.
Infection risk
Awareness of the risk of harm to HCW has developed since the COVID-19 pandemic began in Wuhan at the end of 2019. A detailed analysis of COVID-19 infection rates in HCW will surely follow in the near future, but early reports from Italy suggest that HCW have been disproportionately affected (HCW alone account for 8.4% of all cases in this country [15]) and similar rates have also recently been reported by Chou et al. [16]. The coronavirus is not considered to be an airborne virus so airborne precautions are not routinely necessary [17]. However, certain procedures particularly those associated with airway management can create aerosols containing virus that linger in the air and therefore risk transmission over distances beyond 2 metres. The risk of COVID-19 infection with AGP’s is such that healthcare organisations around the world have been clear in their guidance that precautions must be followed to protect HCW. This includes the use of personal protective equipment (PPE) such as disposable gloves, fluid-repellent gown, filtering face piece respirator and eye/face protection. When possible, AGPs should be carried out in a single room with negative pressure airflow (preferably HEPA filtered) with the doors closed and the minimum number of HCW’s present. Full PPE would need to be worn to enter the room for a period of time after the AGP depending on the air change rate; in the absence of a negative pressure room, this room isolation period would need extending.
In the hospital environment, room ventilation ensures quick viral aerosol clearance. One air exchange removes ~63% of the virus [18]. After five air exchanges in the room, there is < 1% of the original viral load. Five exchanges take ~25 min in most clinical environments. However, in ICU or operating room, the air exchange is more frequent and five exchanges will take 12 min. While negative pressure rooms are recommended for aerosol generating procedures, our experience has shown that such settings are infrequently available. In some locations, engineering modifications can change a positive pressure room or entire ward to negative pressure. We would suggest that having a room with good ventilation and a high rate of air exchanges, is likely to be more important than whether it is positive or negative pressure [19].
The sequelae of COVID-19 infection can be potentially devastating, and the sensitivity of COVID-19 testing does not yet approach 100%. Therefore, caring for a patient with a negative swab result does not preclude the need for full PPE [17]. Furthermore, patients with a tracheostomy may be infectious for longer than the average COVID-19 patient. This is because tracheostomy patients will, by definition, have been critically ill during their COVID-19 episode and this is associated with the delayed clearance of viral RNA [20]. The increased sensitivity of COVID-19 RNA detection in blind endotracheal aspirates compared to saliva tests and oropharyngeal swabs suggests that viral load is greater in the lower respiratory tract [21]. Tracheostomy is thought to pose a particular threat to HCW through exposure to these endobronchial secretions and the performance of multiple AGPs during routine care. These factors, combined with the putative peak viral load in early illness lend weight to the consensus for later tracheostomy in COVID-19 patients [6, 22, 23].
Basic tracheostomy care
The same basic principles of care should apply to a tracheostomy patient with suspected or diagnosed COVID-19 infection as for any other tracheotomised patient in hospital. These include clear display of vital information at the bedside; tracheostomy emergency protocols [24]; infection control; stoma care; humidification; cuff management; secretion management and oral hygiene; as well as ongoing quality assurance and improvement processes that deliver and disseminate best practice.
As a patient begins to recover from the insult that led to ICU admission, there begins a process of rehabilitation that encompasses facilitating communication, swallowing, weaning and, ideally, eventual decannulation [25, 26]. Collaboration across specialties is critical to deliver safe and effective care, and we are unified in commending the benefits of a multidisciplinary tracheostomy team who work together in synchronous ward rounds, with standardised protocols/guidelines, interdisciplinary education, patient and family involvement, and quality improvement processes [27].
The following proposed measures (Table 2), although not eliminating the possibility of aerosolisation, should minimise droplet production and therefore protect HCW. This will not preclude the need for PPE as per current guidance.
Table 2.
Key recommendations for tracheostomy care during COVID-19 pandemic
| Function | Potential for AGP | Key steps | |
|---|---|---|---|
| Basic principles | Ensure best possible patient care | N/A |
Bedhead information signs Emergency protocols and equipment Multidisciplinary treatment Patient/family involvement Audit |
| Cuff management |
Provide closed circuit Protect airway and decreases aspiration |
Yes |
Whilst ventilated, keep pressure on upper limit (25–30 cm H20) to decrease cuff leak Decrease cuff pressure when self-ventilating Check pressure at the beginning of each shift Avoid unnecessary checks |
| Humidification/mucolytics (including nebulisers) |
Reduce secretions viscosity Maintain tube patency |
Controversial |
Start with HME circuit Use regular saline nebulisers Add mucolytic if necessary Consider change to “wet” circuit |
| Suctioning | Remove retained secretions to ensure airway patency and maintain gas exchange | Yes | Consider closed in-line suction minimize suctioning without compromising airway |
| Inner cannula | Reduce risk of tube occlusion | Yes |
When patient ventilated, do not break circuit to change Change when circuit has to be broken for other reasons or if clinical signs Encourage self-ventilating patient to do for themselves when able |
| Subglottic aspiration ports | Removal of secretion load on top of the cuff | Yes |
Decide on a case by case basis Consider with high secretions |
| Cuff deflation trials |
Restore upper respiratory tract Facilitate communication |
Yes |
Balance initiate as soon as possible vs. waiting until patient able to maintain self-ventilation for 24 h FNE/FEES after MDT agreement Consider surgical mask for the patient during cuff down |
| One way valves |
Facilitate verbal communication Rehabilitation |
Potential | Use humidification bib and apply surgical mask to the patient |
Emergency situations
Early recognition and rapid management of emergency situations are essential for all tracheostomy care, however this is even more critical in the context of COVID-19, where infection control procedures can impact on the speed of response. It is essential that regular observations and basic maintenance procedures happen in a timely fashion to avert impending emergencies [24]. Cohorted care of “positive” patients may help to reduce risk from delays in donning and doffing PPE. Otherwise, the location of patients in side rooms with doors shut may be a communication hindrance and may delay access to equipment. It is therefore essential that this extra time is factored in when staffing areas with tracheostomy patients.
Locally agreed resuscitation guidance in COVID-19 patients dictates that no airway-related procedures are performed unless all staff present are wearing PPE. This means that a first responder needs to enter the area in full PPE. In circumstances where the staff present are not wearing appropriate PPE, modified mechanisms to support emergency care need to be adopted whilst other staff are preparing to attend the emergency in full PPE. Additional equipment may need to be provided as standard and other mechanisms for enhanced team communication should be considered.
Cuff management
An inflated cuff during ventilation should provide a closed system and is therefore likely to prevent cross-contamination from patients to staff, equipment and other patients. When inflated, cuff pressure should be monitored using a manometer and maintained between 25 and 30 cm H2O to decrease the risk of cuff leak [28]. The cuff pressure should be checked at the beginning of each nursing shift and re-checked whenever a cuff leak has been identified or when the cuff or tracheostomy tube has been manipulated [29]. HCW should be aware that all methods of cuff measurement are inherently inefficient and using a cuff manometer will cause some cuff deflation [30] and possible aerosol generation due to a cuff leak; PPE should therefore be worn whenever the cuff is checked. Once the patient is liberated from the ventilator, the cuff pressure should be dropped to values of ~20–25 cm H2O to prevent tracheal tissue damage through ischaemia. Where available, automatic tracheostomy cuff pressure monitoring devices will minimise these risks.
Humidification
Warm humidification is a fundamental aspect of tracheostomy care. The tracheostomy bypasses the normal upper airway mechanisms for humidification, filtration, and warming of inspired gases [25]. Therefore, there must be a 24 h humidification strategy in place for all patients with a tracheostomy. Mechanical ventilation ideally requires humidification and this can be achieved through different methods with no distinct advantages of one against the other [31]. Concerns were raised early on in the UK’s pandemic experience regarding the potential for “wet” circuits to generate virus-laden aerosols at times of disconnection. Recommendations were made that ventilated patients should have a heat and moisture exchanger (HME) in the circuit [19] set in conjunction with in-line nebulised saline every 4–6 h. Subsequently, there have been counter-arguments that this strategy was associated with inadequate humidification and that “wet” circuit protocol should be adopted where full PPE and adequate isolation or cohorting measures are in use. We do not recommend one against the other provided appropriate PPE is used.
Similarly, in self-ventilating patients, a fitted HME cartridge is preferable to the looser fitting bib type, provided secretion volumes do not place the patient at risk of tube occlusion.
Nebulisers
In many settings, nebulised saline is used routinely to maintain tracheostomy tube patency, especially in the absence of heated humidification systems (such as when self-ventilating on room air) [32]. Current advice in COVID-19 suggests avoidance of nebulisers where possible, using spacer devices and metered dose inhalers to deliver inhaled mediations such as bronchodilators [33]. However, in tracheotomised patients without physiological mechanisms for humidification through the upper airway, saline/mucolytic nebulisers would still be beneficial. There is debate over whether nebuliser administration is aerosol generating with conflicting advice by the World Health Organisation (WHO) [34] and Public Health England/New and Emerging Respiratory Virus Threats Advisory Group (PHE/NERVTAG) [14] guidance. However, as in the case of many of the unknowns surrounding COVID-19 transmission, it would be advisable to take a risk reduction approach such as the use of expiratory filters.
Secretion management
Critically ill tracheotomised patients often produce copious volumes of respiratory secretions due to the altered dynamics of the upper aerodigestive tract, effects of medication-induced paralysis/sedation, airway inflammation, and secondary infections. This secretion load may require tracheal suctioning for removal, to ensure ongoing airway patency and gas exchange. To reduce aerosol spread during suctioning, the use of closed in-line suction is recommended for all COVID-19 patients [35]—this is particularly useful for maintaining a closed circuit in patients requiring high positive end-expiratory pressure (PEEP). However, to reduce tracheal injury, indiscriminate suctioning should be avoided: the patient should be assessed for signs of sputum in the airway, and where the patient can cough secretions independently into the top of the tracheostomy tube, these secretions should be removed using the in-line suction catheter, avoiding its insertion into the trachea. Overly aggressive tracheal suctioning risks damage to the trachea that may result in bleeding, granulation and ultimately tracheal stenosis. These risks must be balanced against ineffective suctioning and inadequate secretion clearance, with subsequent risk of pneumonia and tracheitis.
Several methods have been developed to achieve a filtered circuit in self-ventilated patients although there is no compelling evidence to favour any one method. An example is represented in Fig. 1. The use of an HME with closed suction apparatus reduces aerosolisation during suction. It has been observed that the weight of this may inadvertently alter tracheostomy position and risk causing tracheal or stomal trauma. In these circumstances, where appropriate external support is possible, this would be recommended to avoid this complication. Otherwise, in-line suction systems can be used intermittently provided that safe closed storage arrangements are in place between suctions and appropriate closing of the otherwise open airway takes place in between (e.g., HME cartridge, bib). No evidence currently exists comparing the amount of environmental contamination with intermittent closed suction versus open suction or spontaneous coughing with either a HME or bib.
Fig. 1.
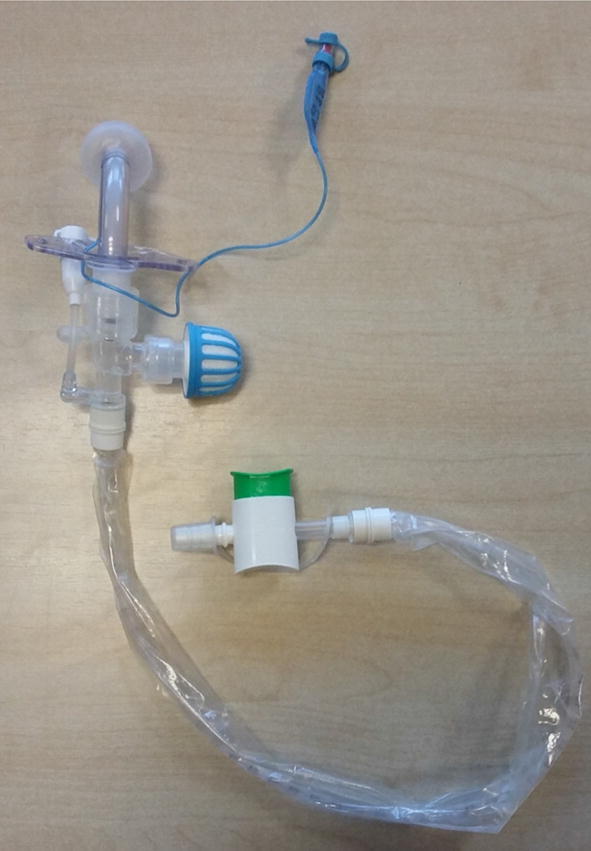
In-line suctioning with HME attached
Naso-oral hygiene
Tracheotomised patients also require effective naso-oropharyngeal secretion clearance to reduce the risk of build-up and loading of the upper respiratory tract, with associated risk of aspiration and ventilator-associated pneumonia (VAP) [36]. Patients able to participate in self clearance of secretions should be encouraged to adhere to heightened infection control advice (such as immediate disposal of tissues) and provided with their own hand sanitiser.
Inner cannula
Inner cannulas are commonly used to safeguard against tube occlusion. At least one clean, dry spare non-fenestrated inner cannula should be kept at the bedside at all times. There is very little published evidence specifically regarding the management of inner cannulas for COVID-19 patient, but after balancing the risk of occlusion versus the risk to HCW we recommend that for the period that a patient is ventilated, the inner cannula should not be changed routinely; but instead changed opportunistically when the circuit has to be broken for other reasons or when there are signs of increased ventilation pressure.
For self-ventilating patients, wherever possible, consider teaching the patient to change the inner cannula (e.g., every 2–4 h) to ensure timely secretion management and reduce the risk of tube blockage whilst minimising any unnecessary aerosol exposure to the HCW.
When cleaning the inner tube, we would recommend that all materials are stored, used, and disposed of at the bedside to avoid contamination of common areas. For that reason, use of disposable inner cannulas has been recommended for COVID-19 patients by Goldman et al. [37] although cost-effectiveness has yet to be proven.
Subglottic aspiration ports
Tracheostomy tubes with subglottic aspiration ports are commonly used in the ICU setting to allow removal of the secretions that can accumulate around and above of the cuff. There is evidence in orotracheal intubation that this may help to decrease the incidence of VAP [38], although there is ongoing debate as to whether this can be extrapolated to their use in tracheostomy care. There is, however, the potential of aerosol generation during subglottic aspiration (by triggering cough). Therefore, its use should be decided on a case-by-case basis but primarily used in those patients with high oral or oropharyngeal secretion load. When they are utilised, an appropriately sized tube with a sufficiently large cuff is required to ensure effectiveness. Where cost or availability issues preclude their use, it should not be a reason to delay or avoid tracheostomy.
Cuff deflation trials
Controversy exists regarding when to start cuff deflation and the balance between HCW safety and expediting weaning. In one of our units, cuff deflation is only commenced once the patient is able to maintain adequate gas exchange and is self-ventilating for 24 h with moderate to low levels of supplemental oxygen. Once a patient meets this criterion, speech and language therapy and physiotherapy assessments may commence to assess suitability for cuff deflation trials. The usual considerations should be made including assessment of alertness, sensation, secretion management, effective cough, and capacity for physical function [39]. In the other unit contributing to this guide, short ventilator-free breathing trials are combined with cuff down time and in line one way valve (Fig. 2) to initiate weaning despite an ongoing need for intermittent mechanical ventilation.
Fig. 2.
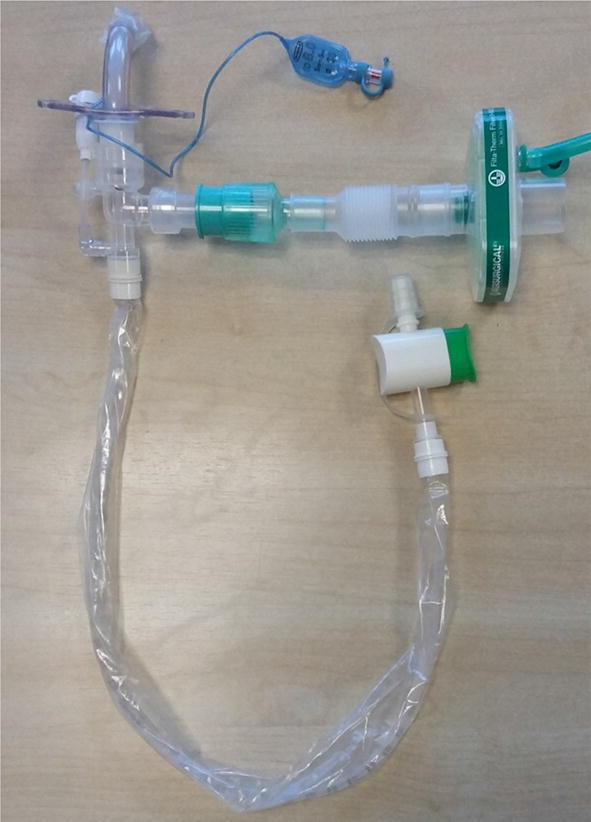
Example of system to initiate cuff deflation during ventilator support weaning
Additional considerations may be required to guide an individualised weaning strategy. Factors such as the mode and duration of mechanical ventilation, medicated paralysis/sedation, proning, and previous failed extubations should be considered as possible markers of ICU acquired myopathy and residual laryngeal oedema or trauma [40].
Once the cuff is deflated, the usual clinical assessment of upper airway patency can be performed through a brief digital occlusion of the tracheostomy tube. Swallowing should be assessed by a speech and language therapist due to the high risk of silent aspiration and the need to identify rehabilitative strategies to promote airway protection. Instrumental assessments routinely performed such as fibreoptic nasolaryngoscopy and fibreoptic endoscopic evaluation of swallowing assessments are considered non-mandatory due to their status as AGPs [35]. The Royal College of Speech and Language Therapy (RCSLT) guidance has only recently allowed a staged return to therapist-led endoscopy for urgent and essential cases with multidisciplinary team (MDT) approval [41]. Despite the reduced access to instrumental assessments, the goal of bedside swallowing assessments remains to reinstate oral intake as quickly and safely as possible. Cuff deflation trials should progress as clinically indicated with time built up as tolerated using clinical criteria to guide trial duration and a patient-worn surgical mask during these trials is a low-cost strategy that may further decrease aerosolisation.
One way valves
One way valves are a useful tool in tracheostomy weaning. Through their use, dead space of the upper airway can be partially reinstated (at expiration), training the patient to regain control of the upper respiratory tract and promoting airway protection. In addition, they may facilitate phonation and therefore verbal communication, which has been associated with improved mood, outlook and sense of recovery [42]. Due to friends and family being unable to visit patient with COVID-19, reinstating voice enables communication by phone/video link, therefore reconnecting them to their loved ones. Furthermore, facilitating any means of communication (either verbal or non-verbal) is essential for psychological and emotional wellbeing and may help reduce delirium [43], which we have observed frequently in this patient group. This can and should be used with in-line suction where appropriate. Wearing a humidification bib over the valve will help to add a layer of filtration to inspired room air to further protect the patient.
Capping
This is not routinely done at our centres and any use is based on individualised clinical grounds. There has been debate about any change in need for this with the COVID-19 population, but no change to practice has been indicated thus far.
COVID-19 special situations and needs
As indicated, full PPE is paramount while performing any of the previously mentioned steps. Another relevant consideration regarding these patients is that a positive COVID-19 status should not detract from the tracheostomy weaning process where possible.
Prone positioning for these patients is relatively rare as this is mostly done during the early stages of the disease according to our experience. However, it is possible to prone patients with a tracheostomy using extra chest and head support to provide good neck access. Suctioning becomes more complicated in these situations and this must be considered when planning the proning regime if the secretion load is high.
Advanced planning for managing tracheotomised COVID-19 patients
Setting and location
Successful and prompt weaning requires experienced multidisciplinary staff; it would therefore be ideal to cohort recovering tracheostomised patients to facilitate efficient input. However, it is unclear whether patients who have been discharged from ICU yet still return positive swabs for COVID-19 viral RNA remain infectious [41]. Regardless, site-specific measures dependant on ward ergonomics and ventilation are required to effectively segregate COVID-19 positive and negative patients.
In our units thus far, capacity and patient status has been such that the majority of patients have progressed to decannulation whilst still in cohorted “COVID-19 positive” level 3 care (data to be published).
Tracheostomy management simulation training
HCW have been redeployed in large numbers to intensive care units and designated COVID-19 wards. For many, this has led to the need to contribute to caring for patients with unfamiliar needs including tracheostomy management. Simulation therefore has a vital role [42] to train staff in both the procedure and the subsequent management of tracheostomies. Examples of procedural simulation include, cadaver-based training to teach the percutaneous technique of tracheostomies to surgeons. Examples of ward-based care simulations include a dedicated rehearsal of clinically based scenarios with high fidelity mannequins. Training sessions can use a variety of teaching methods to develop skills and reduce risk. Devising a program that incorporates a combination of didactic teaching and hands-on simulation has proved popular. Sessions include all relevant members of the multi-disciplinary team to ensure scenarios are as realistic as possible. Advanced patient simulators can be used with scenarios based on real complications and played out in real time. Non-technical skills such as communication, team-working, and decision-making can also be rehearsed although it is recognised that it can be difficult to accurately recreate complex clinical scenarios in a non-clinical setting.
Weaning and decannulation process
One of the key goals of tracheostomy is to facilitate weaning from ventilation support. Tracheostomy weaning will restore physiological breathing, with its advantages of filtering, warming and humidifying inhaled air. Weaning is achieved with progressive reductions in pressure support. Prior to COVID-19, regular periods of cuff deflation, use of vocalisation strategies through one way valves, swallowing rehabilitation, and promotion of coughing to the mouth. However, all these steps have the potential of both droplet and aerosol generation when on a ventilator, hence the decannulation process should be modified to only move through these stages once the patient can tolerate self-ventilation. Although downsizing of tracheostomy tubes is not routine practice, it could be required to facilitate weaning for patients that are not progressing. However, appropriate risk management of this will be required as tracheostomy tube removal and insertion are AGPs. This sequence of events leads towards the final step; tracheostomy decannulation. Each institution should to have its own well-honed decannulation protocol reflecting local expertise, experience and resources.
During these unprecedented times, every effort must be made to expedite the safe decannulation of patients once ventilator support is no longer required. This facilitates effective patient care and decreases the pressure on our stretched healthcare systems.
A unified and experienced tracheostomy team comprising tracheostomy nurses, speech and language therapists, respiratory physiotherapists, critical care specialists, respiratory physicians and head and neck surgeons is fundamental to achieving this, particularly when leading redeployed staff.
Conclusion
The healthcare response to COVID-19 pandemic is likely to generate an increased number of tracheotomised patients in our hospitals. There are still many controversial aspects in the management of patients with COVID-19 as researchers struggle to keep pace with the rapidly evolving disease paradigm. Randomised control trials comparing patients with different care strategies or equipment usage, whilst providing robust evidence, require time and resources that are not reasonable in the environment of a global pandemic. We therefore propose a pragmatic approach to tracheotomised patient care, weaning and decannulation. This is based on the highest quality evidence available and interpreted in light of our experience of COVID-19 patients. It is clearly of utmost importance to ensure the safety of patients and staff. This requires a single multidisciplinary team for all patients who require a tracheostomy during their recovery from COVID-19. Finally, we recommend continuous prospective data collection and audit to refine future practise.
Compliance with ethical standard
Conflict of interest
None of the authors declare any conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Phua J, et al. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir. 2020;8(5):506–517. doi: 10.1016/S2213-2600(20)30161-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Intensive Care National Audit and Research Centre (2020). ICNARC report on COVID-19 in critical care. https://www.icnarc.org/Our-Audit/Audits/Cmp/Reports. Accessed 7 May 2020
- 3.Griffiths J, et al. Systematic review and meta-analysis of studies of the timing of tracheostomy in adult patients undergoing artificial ventilation. BMJ. 2005;330(7502):1243. doi: 10.1136/bmj.38467.485671.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adly A, Youssef TA, El-Begermy MM, et al. Timing of tracheostomy in patients with prolonged endotracheal intubation:a systematic review. Eur Arch Otorhinolaryngol. 2018;275:679–690. doi: 10.1007/s00405-017-4838-7. [DOI] [PubMed] [Google Scholar]
- 5.Angel L, et al. Novel percutaneous tracheostomy for critically ill patients with COVID-19. Ann Thorac Surg. 2020 doi: 10.1016/j.athoracsur.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Takhar A, et al. Recommendation of a practical guideline for safe tracheostomy. Eur Arch Otorhinolaryngol. 2020 doi: 10.1007/s00405-020-05993-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barry BN, Bodenham AR. The role of tracheostomy in ICU. Anaesth Intensive Care Med. 2004;5(11):375–378. doi: 10.1383/anes.5.11.375.53408. [DOI] [Google Scholar]
- 8.Shinn JR, et al. Incidence and outcomes of acute laryngeal injury after prolonged mechanical ventilation. Crit Care Med. 2019;47(12):1699–1706. doi: 10.1097/CCM.0000000000004015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chan JYK, Wong EWY, Lam W. Practical aspects of otolaryngologic clinical services during the 2019 novel coronavirus epidemic: an experience in Hong Kong [published online March 20, 2020] JAMA Otolaryngol Neck Surg. 2020 doi: 10.1001/jamaoto.2020.0488. [DOI] [PubMed] [Google Scholar]
- 10.Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS ONE. 2012;7(4):e35797. doi: 10.1371/journal.pone.0035797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thamboo A, et al. Clinical evidence based review and recommendations of aerosol generating medical procedures in otolaryngology—head and neck surgery during the COVID-19 pandemic. J Otolaryngol Head Neck Surg. 2020;49(1):28. doi: 10.1186/s40463-020-00425-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chung FF, et al. Aerosol distribution during open suctioning and long-term surveillance of air quality in a respiratory care center within a medical center. Respir Care. 2015;60(1):30–37. doi: 10.4187/respcare.03310. [DOI] [PubMed] [Google Scholar]
- 13.Thompson KA, et al. Influenza aerosols in UK hospitals during the H1N1 (2009) pandemic—the risk of aerosol generation during medical procedures. PLoS ONE. 2013;8(2):e56278. doi: 10.1371/journal.pone.0056278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.COVID-19 personal protective equipment (PPE). https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control/covid-19-personal-protective-equipment-ppe. Accessed 7 May 2020 [DOI] [PMC free article] [PubMed]
- 15.Lazzerini M, Putoto G. COVID-19 in Italy: momentous decisions and many uncertainties. Lancet Glob Health. 2020;8(5):e641–e642. doi: 10.1016/S2214-109X(20)30110-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chou R, et al. Epidemiology of and risk factors for coronavirus infection in health care workers: a living rapid review. Ann Intern Med. 2020 doi: 10.7326/M20-1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.COVID-19: Infection prevention and control (IPC) www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control. Accessed 7 May 2020
- 18.Coia J, et al. Guidance on the use of respiratory and facial protection equipment. J Hosp Infect. 2013;85(170–82):31. doi: 10.1016/j.jhin.2013.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cook TM, et al. Consensus guidelines for managing the airway in patients with COVID-19: guidelines from the difficult airway society, the association of anaesthetists the intensive care society, the faculty of intensive care medicine and the Royal College of Anaesthetists. Anaesthesia. 2020;75(6):785–799. doi: 10.1111/anae.15054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xu K, et al. Factors associated with prolonged viral RNA shedding in patients with COVID-19. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang W, et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA J Am Med Assoc. 2020 doi: 10.1001/jama.2020.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.American Academy of Otolaryngology and Head and Neck Surgery (2020) AAO position statement: tracheotomy recommendations during the COVID-19 pandemic. https://www.entnet.org/content/aao-position-statement-tracheotomy-recommendations-during-covid-19-pandemic. Accessed 7 May 2020
- 23.Canadian Society of Otolaryngology-Head and Neck Surgery (2020) Recommendations from the CSO-HNS taskforce on performance of tracheotomy during the COVID-19 pandemic. https://www.entcanada.org/wp-content/uploads/COVID-19-Guidelines-CSOHNS-Task-Force-Mar-23-2020.pdf. Accessed 7 May 2020 [DOI] [PMC free article] [PubMed]
- 24.McGrath BA, et al. Multidisciplinary guidelines for the management of tracheostomy and laryngectomy airway emergencies. Anaesthesia. 2012;67(9):1025–1041. doi: 10.1111/j.1365-2044.2012.07217.x. [DOI] [PubMed] [Google Scholar]
- 25.Dawson D. Essential principles: tracheostomy care in the adult patient. Nurs Crit Care. 2014;19(2):63–72. doi: 10.1111/nicc.12076. [DOI] [PubMed] [Google Scholar]
- 26.Kutsukutsa J, et al. Tracheostomy decannulation methods and procedures for assessing readiness for decannulation in adults: a systematic scoping review. Int J Evid Based Healthc. 2019;17(2):74–91. doi: 10.1097/XEB.0000000000000166. [DOI] [PubMed] [Google Scholar]
- 27.Bedwell JR, et al. Multidisciplinary tracheostomy care: how collaboratives drive quality improvement. Otolaryngol Clin North Am. 2019;52(1):135–147. doi: 10.1016/j.otc.2018.08.006. [DOI] [PubMed] [Google Scholar]
- 28.Respiratory Care Committee of Chinese Thoracic Society Expert consensus on preventing nosocomial transmission during respiratory care for critically ill patients infected by 2019 novel coronavirus pneumonia. Zhonghua Jie He He Hu Xi Za Zhi. 2020;43(4):288–296. doi: 10.3760/cma.j.cn112147-20200304-00239. [DOI] [PubMed] [Google Scholar]
- 29.Hess DR. Tracheostomy tubes and related appliances. Resp Care. 2005;50(4):497–510. [PubMed] [Google Scholar]
- 30.Rose L, Rendl L. Survey of cuff management practies in intensive care units in Australia and New Zealand. Am J Crit Care. 2008;17(5):428–435. doi: 10.4037/ajcc2008.17.5.428. [DOI] [PubMed] [Google Scholar]
- 31.Vargas M. Heat and moisture exchangers (HMEs) and heated humidifiers (HHs) in adult critically ill patients: a systematic review, meta-analysis and meta-regression of randomized controlled trials. Crit Care. 2017;21(1):123. doi: 10.1186/s13054-017-1710-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Day-to-day management of Tracheostomies and Laryngectomies. Tracheostomy.org.uk/storage/files/HumidificationNew.pdf. Accessed 8 May 2020
- 33.Thomas P, et al. (2020) Physiotherapy management for COVID-19 in the acute hospital setting: clinical practice recommendations. J Physiother. 2020;66(2):73–82. doi: 10.1016/j.jphys.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations. https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations. Accessed 8 May 2020.
- 35.ENT-UK (2020) COVID-19 Tracheostomy guidance. https://www.entuk.org/sites/default/files/files/COVID%2520tracheostomy%2520guidancecompressed.pdf
- 36.Hua F, et al. Oral hygiene care for critically ill patients to prevent ventilator-associated pneumonia. Cochrane Database Sys Rev. 2016;10:CD008367. doi: 10.1002/14651858.CD008367.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Goldman RA, et al. Tracheostomy management during the COVID-19 pandemic. Otolaryngol Head Neck Surg. 2020 doi: 10.1177/0194599820923632. [DOI] [PubMed] [Google Scholar]
- 38.Mao Z. Subglottic secretion suction for preventing ventilator-associated pneumonia: an updated meta-analysis and trial sequential analysis. Crit Care. 2016;20(1):353. doi: 10.1186/s13054-016-1527-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Singh RK, Saran S, Baronia AK. The practice of tracheostomy decannulation—a systematic review. J Intensive Care. 2017;5:38. doi: 10.1186/s40560-017-0234-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dres M, et al. Critical Illness-associated diaphragm weakness. Intensive Care Med. 2017;43:1441–1452. doi: 10.1007/s00134-017-4928-4. [DOI] [PubMed] [Google Scholar]
- 41.RCSLT Guidance. Speech and language therapist-led endoscopic procedures in the COVID-19 pandemic. https://www.rcslt.org/-/media/docs/Covid/RCSLT-COVID-19-SLT-led-endoscopic-procedure-guidance_FINAL-(2).PDF?la=en&hash=8101575091FE8F1ABA41B4B472387DAFB023A39D. Accessed 10 May 2020
- 42.Freeman-Sanderson AL, et al. Quality of life improves for tracheostomy patients with return of voice: a mixed methods evaluation of the patient experience across the care continuum. Intensive Crit Care Nurs. 2018;46:10–16. doi: 10.1016/j.iccn.2018.02.004. [DOI] [PubMed] [Google Scholar]
- 43.Tembo AC, et al. The experience of communication difficulties in critically ill patients in and beyond intensive care: findings from a larger phenomenological study. Intensive Crit Care Nurs. 2015;31(3):171–178. doi: 10.1016/j.iccn.2014.10.004. [DOI] [PubMed] [Google Scholar]
- 44.Wölfel R, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020 doi: 10.1038/s41586-020-2196-x. [DOI] [PubMed] [Google Scholar]
- 45.Musbahi O, et al. Current role of simulation in otolaryngology: a systematic review. J Surg Educ. 2017;74(2):203–215. doi: 10.1016/j.jsurg.2016.09.007. [DOI] [PubMed] [Google Scholar]
- 46.de Montbrun SL, Macrae H. Simulation in surgical education. Clin Colon Rectal Surg. 2012;25(3):156–165. doi: 10.1055/s-0032-1322553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bannon R. Non-technical skills and otolaryngology: systematic review. J Laryngol Otol. 2020;8:1–4. doi: 10.1017/S0022215120000900. [DOI] [PubMed] [Google Scholar]


