Abstract
Introduction
Neurological conditions are a major and increasing cause of hospitalisation among children and young people, but little is known about the impact of neurological conditions on hospital services in England, nor the factors that influence length of stay and bed days per year.
Objectives
To quantify the hospital usage in children and young people related to neurological conditions, trends over time and variation by ethnicity and deprivation status.
Methods
An ICD10 coding framework identified a cohort of individuals aged 0-19 years with neurological conditions from linked routinely collected healthcare data from England (The Hospital Episode Statistics Admitted Patient Care dataset), from 1 April 2003 to 31 March 2015. Linked outpatient and accident and emergency data were used to supplement missing demographic data. Length of stay and bed days per year per person were calculated. These were separately modelled using random intercept multivariable negative binomial regressions with gender, age, ethnic group, diagnostic group, region of residence and deprivation category as predictors.
Results
524,442 individuals were identified over the study period, increasing from 49,928 in 2003/04 to 102,840 in 2014/15. Neurological conditions account for 8.8% of inpatient bed days in the 0-14 year old age group. Length of stay and bed days per year vary primarily by age group – e.g. Under 1 year olds had 1.85 times (95%CI 1.83-1.86%) longer stays and over double (2.36 times, 95%CI 2.34-2.37 times) the number of bed days per person per year compared to 5 to 9 year olds – and main diagnostic group, with smaller variations by ethnic group, deprivation and region.
Conclusions
Neurological conditions in children and young people have a significant and increasing impact on the NHS in England. Falls in length of stay and bed days per person are more than offset by increasing numbers of children and young people with neurological diagnoses. Variations in length of stay and bed days per year by diagnostic group, ethnic group, age group, deprivation category and region should be taken into account in resource planning
Introduction
Neurological conditions, such as cerebral palsy, epilepsy and neuromuscular conditions, are a major and increasing [1] cause of hospitalisation among children and young people, accounting for between 5% and 10% of their admissions, around 20% of costs and 14% of bed days in the United States (US)[1,2]. Among children and young people in the US, those with neurological conditions had nearly three times greater intensive care unit (ICU) use than those with other conditions and accounted for nearly half of deaths[2].
In the UK, neurological conditions account for 30-40% of deaths in children and young people aged 1-19 years[3] and are the third most common primary reason for paediatric ICU (PICU) admission[4]. However the only study which has assessed data on hospital usage for children with neurological conditions in the UK was a single centre study in London[5]. Although there are studies which have tracked neurological outcomes for preterm babies[6] and regional disease specific registers e.g. north east cerebral palsy register[7], there are no good quality, national level data sources for the incidence of these neurological conditions in children in the UK. Given the demographic differences between London and the rest of England, there is value in a national level study. This study aimed to quantify the hospital usage (admissions, length of stay and bed pays per year) in children and young people related to neurological conditions, trends over time and variation by ethnicity and deprivation status.
Methods
Participants
Cohort identification
An International Classification of Diseases version 10 (ICD10)[8] coding framework for neurological conditions (supplementary material) was developed by a consultant paediatric neurologist (JL) and reviewed by LF. This coding framework aimed to identify all children with a neurological diagnosis who, depending on severity of their condition, may require to be seen by a paediatric neurologist e.g. epilepsy, cerebral palsy, Duchenne muscular dystrophy, Batten disease.
The study cohort included all individuals (0-19 years) who had at least one episode in the Hospital Episode Statistics (HES) admitted patient care (APC – containing hospital inpatient episodes) dataset with one of the neurological codes recorded between 1/4/2003 – 31/3/2015.
Datasets
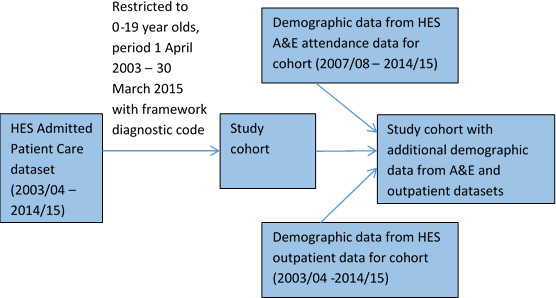
The HES data are national records of NHS hospital use in England [9]. A request was made to NHS Digital for all HES APC (1/4/2003 -31/3/2015), outpatient (1/4/2003-31/3/2015) and Accident and Emergency (A&E) records (1/4/2007-31/3/2015) for individuals matching the cohort definition. The outpatient and A&E data were used only to supplement missing demographic information in the inpatient data (Figure 1). NHS Digital linked the data across the APC, A&E and outpatient datasets using patient HESID (determined based on NHS number, date of birth, gender, postcode, provider code and local patient ID)[10].
Figure 1: Construction of the cohort and datasets used. ‘HES’ refers to Hospital Episode Statistics; ‘A&E’ refers to Accident and Emergency.
Data management
The datasets were arranged in financial years (e.g. financial year 2003/04 covers the period from 1 April 2003 to 31 March 2004).
Ethnicity was first assigned to one of eight groups in each record: White, Indian, Pakistani, Bangladeshi, Black, Chinese, Mixed or Other. Each individual’s ethnic group was then set as the most commonly recorded in the APC dataset, excluding missing values (the APC dataset was preferred as these data were more complete than in the A&E or outpatient datasets). Where ethnic group could not be determined from the APC dataset, data from the outpatient and A&E datasets were used.
Gender was set as the most commonly recorded, again excluding any missing values and preferring the APC dataset, using the outpatient and A&E datasets only where gender was not defined in the APC dataset.
Age, Government Office Region of residence (GOR), and deprivation score (Index of Multiple Deprivation (IMD) 2004)[11] could change over time. The first recorded value was used in each financial year (again, preferring APC data, supplementing with A&E and outpatient data where missing in APC). Deprivation scores were assigned to categories (with approximately 20% of the population of England in each) using published populations[12] and IMD 2004 rankings[13] for Lower Super Output Areas (a small-scale geographical area of approximately 1500 people).
Seven diagnostic groups were used, based on the ICD10 chapters: malignant neoplasms (C), benign neoplasms (D), metabolic conditions (E), mental or behavioural conditions (F), nervous system conditions (G), congenital conditions (Q) and other conditions (R). Each record was assigned one or more diagnostic groups based on all the diagnoses present (primary and secondary diagnoses). Each individual was also assigned a main diagnostic group. This was the most common diagnostic group recorded in records for that individual over the study period, using all the diagnosis fields. If there was no most common diagnostic group, the most common diagnostic group associated with primary diagnoses was used. If there was still no most common diagnostic group, records were progressively ignored (starting with the oldest on the basis that diagnoses should become more certain over time) until a most common diagnostic group could be determined.
Finally, continuous inpatient spells (‘admissions’) were constructed for each cohort member per year[14]. Each admission represents a continuous period of inpatient care, often a single finished consultant episode (FCE, a period of care under one consultant) although they may contain multiple FCEs. In creating admissions, FCEs that were separated by less than 2 days (i.e. those with discharge and admission on the same or consecutive days) and within the same hospital were combined (considered part of a single admission).
Statistical analyses
All data analyses were performed using Stata V.14 (StataCorp. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP, 2015).
Descriptive analyses
Each year, the number of individuals aged 0-19 years with at least one inpatient admission that year with one of the neurological codes was recorded, as was the number with a primary neurological diagnosis.
Length of stay (number of nights in hospital) was calculated for each admission and the number of bed days (length of stay plus one for each admission) was calculated for each cohort member per year. In each year, the analysis was limited to cohort members with an inpatient admission (or part of an inpatient admission) in that year. This ensured that the analysed group was similar in each year. Otherwise, if the whole cohort was analysed each year from first inclusion, then in later years there would be an increasing proportion of ‘inactive’ cohort members who had an identified condition, had previously had an inpatient admission but were not in that year in need of inpatient care. When admissions spanned a year boundary, they were considered part of the year of admission for analysis of length of stay. For analysis of bed days, these admissions were split at the year boundary and the bed days assigned to the year in which they took place.
Some validation was performed on length of stay: negative length of stay, lengths of stay that were longer than the age of the patient plus one year (to allow for patients that had almost reached their next birthday), and lengths of stay where admission or discharge dates were outside the study period were set to missing. If any length of stay for an individual was missing in a year then the bed days for the individual in that year were also set to missing.
Analyses of length of stay and bed days were split by year, age group, diagnostic group, ethnic group, deprivation category and GOR.
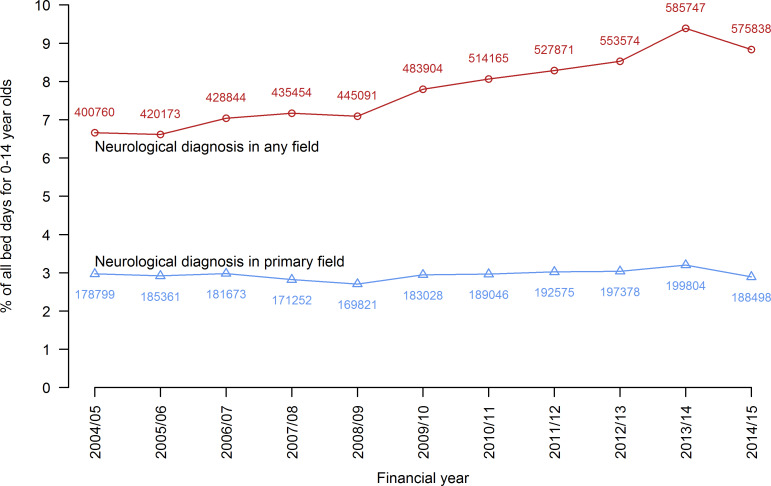
The proportion of inpatient bed days in England attributable to neurological patients was determined, both for admissions with a neurological diagnosis in any field and only for admissions with a primary neurological diagnosis. Aggregate HES data on bed days were only available for the 0-14 year old age group[15] so, for this analysis alone, only 0-14 year old cohort members were included.
Multivariate models
Length of stay and bed days were modelled separately for the whole cohort (0-19 years) using the same strategy. In each year, only cohort members with an admission or part of an admission in that year were included. A two level (random intercept) multivariate negative binomial regression was used. The random intercept accounted for clustering in the data due to dependence in length of stay among multiple admissions and bed days per year among multiple years for a single individual. The following predictors were included: at level 1 (admission level for length of stay; year level for bed days per year) year of admission, age group, primary diagnostic group, deprivation category and GOR; at level 2 (individual level) gender and ethnic group. Interaction terms were included if they decreased the Bayesian Information Criterion (BIC)[16] by more than 2[17]. For the model of bed days, time at risk was included in the model, calculated using year and month of birth provided in the data (day of birth was set to the 15th of the month, except for those admitted as neonates, for whom age in days was provided and so date of birth could be determined exactly) and date of death (only available for those who died in hospital).
Individuals with missing data were excluded from the models for the years in which data were missing. For ethnic group a sensitivity analysis was performed modelling only years 2009/10 onwards where data were more complete.
Results
There were 524,442 cohort members in total; 272,250 had a primary neurological diagnosis. 49,928 had an admission with a neurological diagnosis in 2003/04, rising to 102,840 in 2014/15 (Table 1). There were 1,665,575 admissions (7,431,723 bed days) with a neurological diagnosis, 651,357 of which (2,971,390 bed days) had a primary neurological diagnosis. Children (0-14 years) with neurological conditions accounted for an increasing percentage of bed days (2003/04: 6.66%, 95%CI 6.64-6.68%; 2014/15: 8.83%, 95%CI 8.81-8.86%) but for primary diagnoses the share was relatively static (around 3%, Figure 2).
Table 1: Characteristics of the cohort and its hospital use, by year.
| Financial years | ||||
|---|---|---|---|---|
| 2003/04-2006/07 | 2007/08-2010/11 | 2011/12-2014/15 | Overall in cohort | |
| Persons with an inpatient admission | ||||
|
| ||||
| any neur. diagnosis | 213991 | 278696 | 371965 | 524442 |
| primary neur. diagnosis | 109634 | 131469 | 155535 | 272250 |
| Inpatient admissions | ||||
|
| ||||
| any neur. diagnosis | 438642 | 536496 | 690437 | 1665575 |
| primary neur. diagnosis | 196508 | 214514 | 240335 | 651357 |
| Bed days | ||||
|
| ||||
| any neur. diagnosis | 2103226 | 2449850 | 2878647 | 7431723 |
| primary neur. diagnosis | 955387 | 977225 | 1038778 | 2971390 |
| Persons with unknown bed days in year | 522 | 656 | 753 | N/A |
0.2% |
0.2% |
0.2% |
N/A | |
| Persons with an inpatient admission by gender | ||||
|
| ||||
| Male | 121089 | 158992 | 213864 | 300236 |
56.6% |
57.0% |
57.5% |
57.2% |
|
| Female | 92861 | 119633 | 158013 | 224006 |
43.4% |
42.9% |
42.5% |
42.7% |
|
| Unknown | 41 | 71 | 88 | 200 |
0.0% |
0.0% |
0.0% |
0.0% |
|
| Persons with an inpatient admission by ethnic group | ||||
|
| ||||
| White | 166151 | 217309 | 283097 | 398781 |
77.6% |
78.0% |
76.1% |
76.0% |
|
| Indian | 3880 | 5658 | 7829 | 10485 |
1.8% |
2.0% |
2.1% |
2.0% |
|
| Pakistani | 9204 | 13640 | 19056 | 21372 |
4.3% |
4.9% |
5.1% |
4.1% |
|
| Bangladeshi | 2358 | 3535 | 5124 | 6379 |
1.1% |
1.3% |
1.4% |
1.2% |
|
| Black | 8661 | 13910 | 21351 | 27648 |
4.0% |
5.0% |
5.7% |
5.3% |
|
| Chinese | 429 | 700 | 1038 | 1348 |
0.2% |
0.3% |
0.3% |
0.3% |
|
| Mixed ethnicity | 4320 | 7701 | 12787 | 15477 |
2.0% |
2.8% |
3.4% |
3.0% |
|
| Other ethnicity | 5643 | 9530 | 15672 | 19476 |
2.6% |
3.4% |
4.2% |
3.7% |
|
| Unknown | 13345 | 6713 | 6011 | 23476 |
6.2% |
2.4% |
1.6% |
4.5% |
|
| Persons with an inpatient admission by age group | ||||
|
| ||||
| Under 1 | 30080 | 41469 | 53162 | N/A |
14.1% |
14.9% |
14.3% |
N/A |
|
| 1-4 | 50270 | 67766 | 98312 | N/A |
23.5% |
24.3% |
26.4% |
N/A |
|
| 5-9 | 47664 | 58598 | 81228 | N/A |
22.3% |
21.0% |
21.8% |
N/A |
|
| 10-14 | 45115 | 55777 | 69365 | N/A |
21.1% |
20.0% |
18.6% |
N/A | |
| 15-19 | 40862 | 55086 | 69898 | N/A |
19.1% |
19.8% |
18.8% |
N/A |
|
| Persons with an inpatient admission by diagnostic group | ||||
|
| ||||
| Malignant neoplasms (C) | 3876 | 4397 | 4401 | N/A |
1.8% |
1.6% |
1.2% |
N/A |
|
| Benign neoplasms (D) | 521 | 634 | 743 | N/A |
0.2% |
0.2% |
0.2% |
N/A |
|
| Metabolic (E) | 4665 | 6062 | 6828 | N/A |
2.2% |
2.2% |
1.8% |
N/A |
|
| Mental/behavioural (F) | 43150 | 66505 | 116996 | N/A |
20.2% |
23.9% |
31.5% |
N/A |
|
| Nervous system (G) | 136018 | 167785 | 213273 | N/A |
63.6% |
60.2% |
57.3% |
N/A |
|
| Congenital (Q) | 43246 | 57135 | 71826 | N/A |
20.2% |
20.5% |
19.3% |
N/A |
|
| Other (R) | 17685 | 27598 | 42013 | N/A |
8.3% |
9.9% |
11.3% |
N/A |
|
| Persons with an inpatient admission by main diagnostic group | ||||
|
| ||||
| Malignant neoplasms (C) | 3515 | 3993 | 3846 | 4360 |
1.6% |
1.4% |
1.0% |
0.8% |
|
| Benign neoplasms (D) | 297 | 347 | 405 | 666 |
0.1% |
0.1% |
0.1% |
0.1% |
|
| Metabolic (E) | 4179 | 5263 | 5913 | 5598 |
2.0% |
1.9% |
1.6% |
1.1% |
|
| Mental/behavioural (F) | 30089 | 45083 | 77749 | 103058 |
14.1% |
16.2% |
20.9% |
19.7% |
|
| Nervous system (G) | 127542 | 155656 | 191688 | 284879 |
59.6% |
55.9% |
51.5% |
54.3% |
|
| Congenital (Q) | 34239 | 45998 | 57933 | 58941 |
16.0% |
16.5% |
15.6% |
11.2% |
|
| Other (R) | 14130 | 22356 | 34431 | 66940 |
6.6% |
8.0% |
9.3% |
12.8% |
|
| Persons with an inpatient admission by deprivation category | ||||
|
| ||||
| 1 (most deprived) | 62767 | 81488 | 109895 | N/A |
29.3% |
29.2% |
29.5% |
N/A |
|
| 2 | 45559 | 59414 | 82435 | N/A |
21.3% |
21.3% |
22.2% |
N/A | |
| 3 | 38091 | 48932 | 67762 | N/A |
17.8% |
17.6% |
18.2% |
N/A | |
| 4 | 34545 | 43475 | 57211 | N/A |
16.1% |
15.6% |
15.4% |
N/A | |
| 5 (least deprived) | 32925 | 42119 | 54636 | N/A |
15.4% |
15.1% |
14.7% |
N/A | |
| Unknown | 104 | 3268 | 26 | N/A |
0.0% |
1.2% |
0.0% |
N/A |
|
| Persons with an inpatient admission by Government Office Region of residence | ||||
|
| ||||
| North East | 13019 | 16441 | 20038 | N/A |
6.1% |
5.9% |
5.4% |
N/A |
|
| North West | 33430 | 44040 | 55140 | N/A |
15.6% |
15.8% |
14.8% |
N/A |
|
| Yorkshire and Humber | 21295 | 27026 | 36615 | N/A |
10.0% |
9.7% |
9.8% |
N/A |
|
| East Midlands | 18339 | 22639 | 27332 | N/A |
8.6% |
8.1% |
7.3% |
N/A |
|
| West Midlands | 24361 | 32165 | 43138 | N/A |
11.4% |
11.5% |
11.6% |
N/A |
|
| East of England | 20550 | 27093 | 38036 | N/A |
9.6% |
9.7% |
10.2% |
N/A |
|
| London | 29304 | 40389 | 60829 | N/A |
13.7% |
14.5% |
16.4% |
N/A |
|
| South East | 32112 | 41994 | 56273 | N/A |
15.0% |
15.1% |
15.1% |
N/A | |
| South West | 21581 | 26909 | 34564 | N/A |
10.1% |
9.7% |
9.3% |
N/A |
|
Figure 2: The proportion of inpatient bed days for 0-14 year olds in England in admissions that either had a neurological condition among diagnoses or a neurological condition as the primary diagnosis.
The data were largely complete: apart from ethnic group (8.7% missing in 2003/04, dropping to 2.0% in 2014/15), only bed days (≤0.3% in all years), length of stay (≤0.2%) gender (<0.05% in all years) and deprivation category (1.4% in 2008/09 to 2010/11; ≤0.5% in other years) had missing data.
There were more males (300,326) than females (224,006) in the cohort. White individuals made up the largest group (398,781 individuals, 76%); individuals in the Pakistani and Black ethnic groups were over-represented (respectively, 5% and 6% of the cohort in 2011/12 compared to 2% of population for each in 2011)[18]. 1 to 4 year olds were the largest group (27,494 in 2014/25), but <1 year olds were proportionately more likely to have inpatient admissions (14,789 in 2014/15). Overall, the most common diagnoses were epilepsy (26% of admissions), cerebral palsy (14%) and developmental disorders of scholastic skills (10%). The most deprived category contained approximately double the number of individuals compared to the least deprived (30,373 versus 15,013 in 2014/15). The North West had the largest number of admissions in most years (2014/15: 15,142); the North East had the fewest (2014/15: 5,349).
Length of stay
Admissions shortened over the study period – those with no overnight stay increased from 35.5% (95%CI 35.2-35.8%) to 50% (supplemental Table S1). Admissions longer than 14 days decreased from 4.3% (95%CI 4.2-4.4%) to 3.5% (95%CI 3.4-3.6%). Between 38 and 62 individuals each year had admissions longer than one year.
Minority ethnic groups had more stays over 14 days – over 5% of admissions for all groups except Mixed (4.4%), unknown (3.8%) and White (3.8%). Children <1 year showed variable admission length, with 31% in the 0 day group, but 22% in the 2 to 4 day group and 12% staying over 14 days. For all other age groups, 0 days was the largest group (>50% of admissions).
Admissions with no overnight stay were most common for individuals with a malignant central nervous system (CNS) tumour; other diagnostic groups had more overnight stays (42% to 59%, compared to 29% for malignant CNS tumours).
The least deprived had more admissions with no overnight stay than the most deprived (47.3%, 95%CI 47.1-47.5% compared to 45.2%, 95%CI 45.1-45.3%) and fewer admissions over 14 days (3.6%, 95%CI 3.5-3.7% compared to 4.6%, 95%CI 4.5-4.7%). There were small differences by GOR: admissions over 14 days were more common in London (5.1%) than other regions (3.0% to 4.5%).
Bed days
The number of bed days per person per year has decreased over the study period (supplemental Table S2). 27.0% (95%CI 26.6-27.4%) of individuals (13,235) had a single bed day in 2003/04 compared to 35.1% (95%CI 34.8-35.4%) (36,080) in 2014/15. The proportion having more than 14 bed days fell from 14.4% (95%CI 14.1-14.7%) to 9.4% (95%CI 9.2-9.6%).
White individuals were most likely to have only 1 bed day per year (33%), while Black individuals were most likely to have 2 to 4 (35%). Under 1 year olds were most likely to have more bed days (26% had over 14) while 5 to 9 year olds were most likely (40%) to have only 1 bed day.
Individuals with a malignant CNS tumour were most likely to have over 14 bed days per year (41%) compared to other main diagnoses (all <24%). Those with mental or behavioural disorders were most likely to have only 1 bed day per year (49%).
The least deprived were slightly more likely to have only 1 bed day (33.3%, 95%CI 33.0-33.6% versus 32.1%, 95%CI 31.9-32.3%) and less likely to have over 14 bed days (11.1%, 95%CI 10.9-11.3% versus 12.3%, 95%CI 12.2-12.4%) than the most deprived. There were only minor variations between GORs.
Multivariate models
Length of stay
There was a decrease in length of stay over the study period, by 4% per year (Table 2). Length of stay for females was 2% (95%CI 2-3%) higher than for males. Individuals in the black (by 5%, 95% CI 4-6%) and Mixed (by 4%, 95%CI 2-6%) had longer stays than those in the White group. The Indian (by 6%, 95CI4-7%), Pakistani (1%, 95%CI 0-3%) and Chinese (by 13%, 95%CI 9-18%) ethnic groups had shorter length of stay than those in the White group. <1 year olds had stays nearly twice (1.85 times, 95%CI 1.83-1.86) as long as 5 to 9 year olds. Older groups also had longer stays: 24% (95%CI 23-25%) longer for 10 to 14 year olds and 39% (95%CI 38-41%) longer for 15 to 19 year olds than 5 to 9 year olds. 1 to 4 year olds had stays 3% shorter (95% CI 2-4%) than 5 to 9 year olds.
Table 2: Two level random intercept negative binomial regression models for length of stay and bed days per person per year. IRR is incidence rate ratio compared to the reference category – the ratio of expected length of stay or number of bed days.
| Length of Stay | Bed days per year | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| IRR | 95% CI | P value | IRR | 95% CI | P value | |||
| Financial year | ||||||||
| Change per year | 0.96 | 0.96 | 0.96 | <0.01 | 0.98 | 0.98 | 0.98 | <0.01 |
| Gender | ||||||||
| Male | 1 (ref) | 1 (ref) | ||||||
| Female | 1.02 | 1.02 | 1.03 | <0.01 | 1.01 | 1 | 1.01 | 0.02 |
| Ethnic group | ||||||||
| White | 1 (ref) | 1 (ref) | ||||||
| Indian | 0.94 | 0.93 | 0.96 | <0.01 | 1.03 | 1.02 | 1.05 | <0.01 |
| Pakistani | 0.99 | 0.97 | 1 | 0.03 | 1.04 | 1.02 | 1.05 | <0.01 |
| Bangladeshi | 1.01 | 0.98 | 1.03 | 0.58 | 1.02 | 1 | 1.04 | 0.12 |
| Black | 1.05 | 1.04 | 1.06 | <0.01 | 1.03 | 1.02 | 1.04 | <0.01 |
| Chinese | 0.87 | 0.82 | 0.91 | <0.01 | 1.01 | 0.97 | 1.06 | 0.6 |
| Mixed | 1.04 | 1.02 | 1.06 | <0.01 | 1 | 0.99 | 1.02 | 0.74 |
| Other | 1 | 0.99 | 1.02 | 0.52 | 1.05 | 1.03 | 1.06 | <0.01 |
| Age group | ||||||||
| Under 1 | 1.85 | 1.83 | 1.86 | <0.01 | 2.36 | 2.34 | 2.37 | <0.01 |
| 1 to 4 | 0.97 | 0.96 | 0.98 | <0.01 | 1.05 | 1.04 | 1.05 | <0.01 |
| 5 to 9 | 1 (ref) | 1 (ref) | ||||||
| 10 to 14 | 1.24 | 1.23 | 1.25 | <0.01 | 1.13 | 1.12 | 1.13 | <0.01 |
| 15 to 19 | 1.39 | 1.38 | 1.41 | <0.01 | 1.22 | 1.22 | 1.23 | <0.01 |
| Main diagnostic group | ||||||||
| Malignant neoplasms (C) | 0.37 | 0.36 | 0.37 | <0.01 | 1.24 | 1.21 | 1.27 | <0.01 |
| Benign neoplasms (D) | 0.74 | 0.68 | 0.8 | <0.01 | 1.17 | 1.09 | 1.25 | <0.01 |
| Metabolic (E) | 0.83 | 0.81 | 0.84 | <0.01 | 1.13 | 1.11 | 1.15 | <0.01 |
| Mental/behavioural (F) | 0.95 | 0.95 | 0.96 | <0.01 | 0.87 | 0.87 | 0.88 | <0.01 |
| Nervous system (G) | 1 (ref) | 1 (ref) | ||||||
| Congenital (Q) | 0.82 | 0.81 | 0.83 | <0.01 | 0.98 | 0.98 | 0.99 | <0.01 |
| Other (R) | 0.99 | 0.98 | 1.01 | 0.29 | 0.74 | 0.73 | 0.74 | <0.01 |
| Deprivation category | ||||||||
| 1 (most deprived) | 1(ref) | 1 (ref) | ||||||
| 2 | 1.01 | 1 | 1.02 | 0.03 | 0.99 | 0.99 | 1 | 0.01 |
| 3 | 1.03 | 1.02 | 1.04 | <0.01 | 0.99 | 0.98 | 1 | 0.01 |
| 4 | 0.98 | 0.98 | 0.99 | <0.01 | 0.98 | 0.97 | 0.99 | <0.01 |
| 5 (least deprived) | 0.97 | 0.96 | 0.98 | <0.01 | 0.98 | 0.97 | 0.99 | <0.01 |
| Government Office Region of Residence | ||||||||
| North East | 1.15 | 1.14 | 1.17 | <0.01 | 1 | 0.99 | 1.01 | 0.75 |
| North West | 1 (ref) | 1 (ref) | ||||||
| Yorkshire and Humber | 1.21 | 1.2 | 1.23 | <0.01 | 1.02 | 1.01 | 1.03 | <0.01 |
| East Midlands | 1.21 | 1.19 | 1.22 | <0.01 | 1.04 | 1.03 | 1.05 | <0.01 |
| West Midlands | 1.21 | 1.2 | 1.23 | <0.01 | 1.01 | 1 | 1.02 | 0.04 |
| East of England | 1.15 | 1.14 | 1.16 | <0.01 | 1.03 | 1.02 | 1.04 | <0.01 |
| London | 1.06 | 1.05 | 1.08 | <0.01 | 1.03 | 1.02 | 1.04 | <0.01 |
| South East | 1.21 | 1.2 | 1.23 | <0.01 | 1.03 | 1.02 | 1.04 | <0.01 |
| South West | 1.07 | 1.06 | 1.08 | <0.01 | 1 | 0.99 | 1.01 | 0.97 |
| Model parameters | ||||||||
| Degrees of freedom | 34 | 34 | ||||||
| Log likelihood | -3072235 | -2379091 | ||||||
| BIC | 6144956 | 4758646 | ||||||
Compared to nervous system conditions, all other groups had shorter stays – by 63% for those with malignant neoplasms (95%CI 63-64%), 26% for benign neoplasms (95%CI 20-32%), 17% for metabolic disorders (95%CI 16-19%), 5% for mental or behavioural conditions (95%CI 4-5%), 18% for congenital conditions (95%CI 17-19%) – or were not significantly different (Other conditions).
There was some observed variation in length of stay with deprivation: the least deprived had 3% (95%CI 2-4%) shorter stays than the most deprived, however those in the middle deprivation category had 3% (95%CI 2-4%) longer stays than the most deprived. There were variations by GOR with up to 21% longer stays (Yorkshire & Humber, East Midlands, West Midlands and South East) compared to the North West.
To put these variations in context, in 2010/11 the mean expected length of stay for a White girl aged <1 year old, with a nervous system condition, living in an area in the most deprived category in the East Midlands was 6.6 days. A boy, in the Indian ethnic group, aged 5 years, also with a nervous system condition, living in an area in the least deprived category in the North West, had a mean expected length of stay of 2.6 days, a difference of 4.0 days.
Bed days per person per year
There was a decrease in bed days per person per year over the period, by 2% per year. Females had 1% (95%CI 0-1%) more bed days than males (Table 2). Individuals in the Indian, Pakistani, Black and Other (largest difference, 5%, 95%CI 3-6%) ethnic groups had more bed days than White individuals. <1 year olds had 2.36 (95%CI 2.34-2.37) times as many bed days as 5 to 9 year olds. Older groups also had more bed days: 13% (95%CI 12-13%) more for 10 to 14 year olds and 22% (95%CI 22-23%) more for 15 to 19 year olds compared to 5 to 9 year olds. 1 to 4 year olds had 5% more bed days (95%CI 4-5%) than 5 to 9 year olds.
Compared to nervous system conditions, three groups had more bed days: malignant CNS tumours (by 24%, 95%CI 21-27%), benign CNS tumours (17%, 95%CI 9-25%) and metabolic disorders (13%, 95%CI 11-15%). Three groups had fewer bed days than nervous system conditions: mental or behavioural conditions (by 13%, 95%CI 12-13%), congenital conditions (2%, 95%CI 1-2%) and ‘Other’ conditions (26%, 95%CI 26-27%).
There was a small gradient in bed days with deprivation: the least deprived had 2% (95%CI 1-3%) fewer bed days than the most deprived. There were minor variations by GOR, with up to 4% more bed days (East Midlands, 95%CI 3-5%) compared to the North West.
Illustrating these differences, in 2007/08 a girl in the Pakistani ethnic group, aged <1 year, with a malignant CNS tumour, living in an area in the most deprived category in the East Midlands had a mean expected total of 17.3 bed days per year. A White boy, aged 7 years, also with a malignant CNS tumour, living in an area in the least deprived category in the North East had a mean expected total of 6.6 bed days per year, a difference of 10.7 days.
Discussion
There are growing numbers of children and young people with neurological conditions being admitted to hospitals in England, representing a growing proportion of the inpatient population. The distribution of length of stay has changed over the study period with half of all admissions being day-cases. However approximately 6,500 cohort members had hospital stays of longer than 14 days in 2014/15.
8.8% of inpatient bed days for 0-14 year olds in England in 2014/15 were for children with a neurological condition (among any of their diagnoses). This figure lies between the results of two studies from the US which showed neurological diagnoses or impairment accounted for 5.2% [1] and 10.3% [2] of child hospital admissions but is lower than the only other UK study which was a single centre study in London[5]. This study found that children with neurological diagnoses accounted for 15.3% of all inpatients and 17.7% of all inpatient admission episodes. It is not clear whether day case patients were included in this study or not which may account for the difference[5]. The increasing use of resources by children with neurological conditions mirrors that of the US study which assessed trends[1]. These trends are important in terms both of recruitment and retention of clinical paediatric neurological specialists but also in terms of designing services.
The commonest diagnoses were epilepsy (26%) and cerebral palsy (14%). Again these are similar to those identified by the US study[1], but the London study found that children with genetic, chromosomal and syndromic conditions had the highest number of hospital admissions followed by children with epilepsy[5]. There is some evidence that cerebral palsy prevalence is increasing in the UK[19] which would fit with our results. However, there is evidence that, within primary care in the UK, the incidence of epilepsy in children is decreasing over time[20]. Our results may therefore be showing that GPs are not involved in the care of children with epilepsy or that families simply bypass GPs straight to hospital.
It is unfortunately not possible within the HES data to make any assessment of changes in severity of these neurological conditions over time. The coded data included in the HES data did not allow us to assign these admissions as avoidable or not, nor assess whether they could have been managed by primary care or other community services. However some non-emergency day-case admissions may have the potential to be treated in the non-acute hospital setting – there is some evidence that hospital admissions can be reduced through care plans[21]. There may also be variations over time in clinical coding, with incentives to more accurately record neurological comorbidities (this is supported by the increasing proportion of all admissions that include a neurological diagnosis, but the static proportion that have a primary neurological diagnosis). However, as the survival of these children improves over time due to increasing use of medical technologies and aggressive treatment of complications, these results may demonstrate a genuine increase in admissions for comorbid conditions.
There were large differences by age group, with <1 year olds having admissions lasting 1.9 times as long as 5 to 9 year olds and having over twice as many bed days per year. Older children and young people also had longer stays (24% longer and 39% longer for 10-14 and 15-19 year olds compared to 5-9 year olds) and more bed days per year (13% more and 22% more for 10-14 and 15-19 year olds respectively compared to 5-9 year olds). These differences may reflect disease progression in older children and young people and increased severity or risk of complications in the very young (extremely premature babies commonly have neurological conditions)[22].
The different patterns of healthcare usage by children and young people with different underlying conditions are to be expected. For example, multiple day-case stays but higher numbers of bed days over the year would be expected in a child receiving treatment for a malignant CNS tumour.
The variations seen by ethnicity are more difficult to explain. Many non-white ethnic groups had higher numbers of bed-days than the white population (at p < 0.01, although effect sizes were small at 2-4%). These may be explained by different conditions between ethnic groups (within the broad diagnostic groups used in the model) or differences in severity within the same condition (which are not reflected in the data used). They may also represent different health seeking behaviours. Interestingly these results differ from a previous study in the UK in which South Asian children were more likely to use GP services but less likely to use hospital services than white children[23]. Changes in primary and secondary healthcare in the England in the intervening time period could partly explain these differences.
There is variation with deprivation for both length of stay and bed days – the least deprived have shorter stays (3% shorter for least deprived compared to most deprived group) and fewer bed days per year (2% lower for least deprived compared to most deprived group). This may be due to variations in healthcare provision and practices in different geographical areas or may be linked to different conditions within different deprivation categories. The differences are small for individuals, but larger when aggregated. For example, if bed days per person per year for the most deprived could be reduced to the level of the least deprived, the model suggests over 31 thousand bed days (over 84 bed years) could have been saved over the study period.
There are also geographical differences, with length of stay up to 21% longer (Yorkshire & Humber, East Midlands, West Midlands and South East) than the reference region (North West). The East Midlands also had 5% more bed days per person per year than the North West. There may be geographical variation in conditions (within the diagnostic groups included in the model). There may be differences in outreach or other community services affecting decisions on when to admit to hospital and when to discharge. While the observed geographical differences may not be clinically significant at the individual level, at the population level they represent larger variations in hospital use. For example, if the bed days per person per year in the East Midlands were reduced to the level of the North West then the model suggests over 17,000 bed days (over 47 bed years) could have been saved over the study period.
Strengths and limitations
This study utilised routinely collected, national level healthcare data. The coding framework was developed with a consultant paediatric neurologist, but the ICD10 coding system does not always provide sufficient granularity to isolate all diagnoses. For the analyses, diagnoses have been grouped by ICD10 chapter, but diagnoses within a chapter may have very different care needs, affecting length of stay and bed days per year.
Missing data are few for most variables, but recording of ethnic group is poor in earlier years, of possible concern for the results regarding ethnicity. A sensitivity analysis was performed (supplementary Table S3), repeating the length of stay and bed day models only for data from 2009/10 to 2014/15 where ethnicity data were more complete (≤2.1% missing). This supports the observation that non-White groups had similar or more bed days per person per year than White individuals. The HES data are provided by individual care providers and there are concerns about the accuracy of clinical coding and variations between suppliers[24]. Linkage between datasets is also imperfect[25]. It is possible that this may have an impact on variations observed over time or between geographical areas. Further, increasing use of electronic health records and changes in numbers of diagnoses recorded may explain some of the increase in bed days for individuals with neurology diagnoses observed over the study period. Individuals were only known to have died if they died in hospital. This may have some impact on the modelling of bed days as time at risk may be overestimated for those who died out of hospital.
Conclusions
Neurological conditions account for significant and growing share of inpatient bed days for 0-14 year olds in England. Reductions in length of stay and bed days per person are more than offset by increasing numbers of CYP with neurological diagnoses. Length of stay and bed days per year vary by diagnostic group, ethnic group, age group, deprivation category and by region. These variations should be taken into account in future resource planning for this growing hospital population.
Supplementary Appendices
Acknowledgements
This paper is independent research arising from a Postdoctoral Fellowship (LF) supported by the National Institute for Health Research. The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health.
Abbreviations
| A&E | Accident and Emergency |
| APC | Admitted Patient Care |
| BIC | Bayesian Information Criterion |
| CNS | Central nervous system |
| FCE | Finished consultant episode |
| GOR | Government Office Region |
| HES | Hospital Episode Statistics |
| HESID | Hospital Episode Statistics Identifier |
| ICU | intensive care unit |
| ICD10 | International Classification of Diseases, 10th Edition |
| IMD2004 | Index of Multiple Deprivation 2004 |
| IRR | Incidence rate ratio |
References
- 1. Berry JG, Poduri A, Bonkowsky JL, et al. Trends in Resource Utilization by Children with Neurological Impairment in the United States Inpatient Health Care System: A Repeat Cross-Sectional Study. PLOS Med. 2012; 9: e1001158 10.1371/journal.pmed.1001158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Moreau JF, Fink EL, Hartman ME, et al. Hospitalizations of children with neurological disorders in the United States. Pediatr Crit Care Med. 2013; 14: 801-10. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3795828/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hardelid P, Dattani N, Davey J, Pribramska I and Gilbert R. Overview of child deaths in the four UK countries. Child Health Reviews - UK. London: Royal College of Paediatrics and Child Health, 2013 http://www.rcpch.ac.uk/system/files/protected/page/CHRUK_Module%20A%20low%20res%20(2).pdf [Google Scholar]
- 4. PICANet. PICANet 2015 Annual Report. 2015 http://www.picanet.org.uk/Audit/Annual-Reporting/
- 5. Yuan JX, McGowan M, Hadjikoumi I, et al. Do children with neurological disabilities use more inpatient resources: an observational study. Emerging Themes in Epidemiology. 2017; 14 10.1186/s12982-017-0059-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Moore T, Hennessy EM, Myles J, et al. Neurological and developmental outcome in extremely preterm children born in England in 1995 and 2006: the EPICure studies. Bmj-British Medical Journal. 2012; 345 10.1136/bmj.e7961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Glinianaia SV, Rankin J, Colver A, et al. Cerebral palsy rates by birth weight, gestation and severity in North of England, 1991-2000 singleton births. Archives of disease in childhood. 2011; 96: 180-185. 10.1136/adc.2010.183939 [DOI] [PubMed] [Google Scholar]
- 8. World Health Organisation. International Statistical Classification of Diseases and Related Health Problems. 10 ed. Geneva, Switzerland: World Health Organisation, 1992 http://apps.who.int/classifications/icd10/browse/2016/en [Google Scholar]
- 9. NHS Digital. Hospital Episode Statistics. 2018 http://content.digital.nhs.uk/hes
- 10. Health & Social Care Information Centre. Methodology for creation of the HES Patient ID (HESID). 2014 http://content.digital.nhs.uk/media/1370/HES-Hospital-Episode-Statistics-Replacement-of-the-HES-patient-ID/pdf/HESID_Methodology.pdf
- 11.Noble M, Wright G, Dibben C, et al. The English Indices of Deprivation 2004. London: ODPM Publications, 2003. [Google Scholar]
- 12. Department for Communities and Local Government. SOA level 2001 population estimates - rounded. London: Department for Communities and Local Government, 2004 http://webarchive.nationalarchives.gov.uk/20100410180038/http://www.communities.gov.uk/archived/general-content/communities/indicesofdeprivation/216309/ [Google Scholar]
- 13. Department for Communities and Local Government. SOA level ID 2004. London: , 2004 http://webarchive.nationalarchives.gov.uk/20100410180038/ http://www.communities.gov.uk/archived/general-content/communities/indicesofdeprivation/216309/ [Google Scholar]
- 14. Health & Social Care Information Centre. Methodology to create provider and CIP spells from HES APC data. 2014 http://content.digital.nhs.uk/media/11859/Provider-Spells-Methodology/pdf/Spells_Methodology.pdf
- 15. Health & Social Care Information Centre. Hospital Episode Statistics - Admitted Patient Care - 2014-15. 2015 http://content.digital.nhs.uk/catalogue/PUB19124
- 16. Schwarz G. Estimating the dimension of a model. Ann Stat. 1978; 6: 461-464. https://projecteuclid.org/euclid.aos/1176344136 [Google Scholar]
- 17. Kass RE and Raftery AE. Bayes factors. J Am Stat Assoc. 1995; 90: 773-795. http://www.jstor.org/stable/2291091 [Google Scholar]
- 18. NOMIS. Census 2011 - Ethnic group by sex by age. NOMIS, 2013 https://www.nomisweb.co.uk/census/2011/dc2101ew [Google Scholar]
- 19. Glinianaia SV, Best KE, Lingam R, et al. Predicting the prevalence of cerebral palsy by severity level in children aged 3 to 15 years across England and Wales by 2020. Developmental Medicine and Child Neurology. 2017; 59: 864-+ 10.1111/dmcn.13475 [DOI] [PubMed] [Google Scholar]
- 20. Meeraus WH, Petersen I, Chin RF, et al. Childhood epilepsy recorded in primary care in the UK. Archives of disease in childhood. 2013; 98: 195-202. 10.1136/archdischild-2012-302237 [DOI] [PubMed] [Google Scholar]
- 21. Newton A, Sarker SJ, Parfitt A, Henderson K, Jaye P and Drake N. Individual care plans can reduce hospital admission rate for patients who frequently attend the emergency department. Emerg Med J. 2011; 28: 654. http://emj.bmj.com/content/28/8/654.abstract [DOI] [PubMed] [Google Scholar]
- 22. Wood NS, Marlow N, Costeloe K, Gibson AT and Wilkinson AR. Neurologic and Developmental Disability after Extremely Preterm Birth. N Engl J Med. 2000; 343: 378-384. 10.1056/NEJM200008103430601 [DOI] [PubMed] [Google Scholar]
- 23. Cooper H, Smaje C and Arber S. Use of health services by children and young people according to ethnicity and social class: secondary analysis of a national survey. Br Med J. 1998; 317: 1047-1051. http://www.bmj.com/content/317/7165/1047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Capita Health and Wellbing Limited. The quality of clinical coding in the NHS. 2014 https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/364476/The_quality_of_clinical_coding_in_the_NHS.pdf
- 25. Hagger-Johnson G, Harron K, Fleming T, et al. Data linkage errors in hospital administrative data when applying a pseudonymisation algorithm to paediatric intensive care records. BMJ open. 2015; 5 10.1136/bmjopen-2015-008118 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- NHS Digital. Hospital Episode Statistics. 2018 http://content.digital.nhs.uk/hes
- Health & Social Care Information Centre. Hospital Episode Statistics - Admitted Patient Care - 2014-15. 2015 http://content.digital.nhs.uk/catalogue/PUB19124