Abstract
This report describes a 2-year prospective, longitudinal survey of attending physicians in 3 clinical areas (family medicine, general pediatrics, internal medicine) who experienced a transition from a homegrown electronic health record (EHR) to a vendor EHR. Participants were already highly familiar with using EHRs. Data were collected 1 month before and 3, 6, 13, and 25 months post implementation. Our primary goal was to determine if perceptions followed a J-curve pattern in which they initially dropped but eventually surpassed baseline measures. A J-curve was not found for any measures, including workflow, safety, communication, and satisfaction. Only the reminders and alerts measure dropped and then returned to baseline (U-curve); a few remained flatlined. Most dropped and remained below baseline (L-curve). The only measure that remained above baseline was documenting in the exam room with the patient. This study adds to the literature about current controversies surrounding EHR adoption and physician satisfaction.
Keywords: electronic health records, ambulatory care, physicians, longitudinal studies, survey methods
INTRODUCTION
The United States has experienced substantial growth in the number of hospitals and ambulatory care providers adopting electronic health records (EHRs), in part due to the Health Information Technology for Economic and Clinical Health (HITECH) Act.1–3 The benefits of EHRs have been well described.4–7 Yet EHRs remain controversial with respect to cost,8 productivity and efficiency,9–17 patient-provider communication,10,13,18 and physician job satisfaction.19–23
Recent EHR adoptions provide opportunities to study “second-generation” implementations, in which users switch from legacy electronic systems to newer vendor systems,24–27 and where users have existing familiarity with EHRs. This familiarity is important when judging the impact of an EHR, since the consternation that could arise from “first-generation” implementation, ie, switching from a paper-based to an electronic workflow, should be minimized. Additionally, such users should already be computer literate,28,29 a topic of concern for first-generation implementations.30,31
While there have been multiple studies of EHR and other health IT implementations,19 only some have followed the same providers longitudinally,10,24,30,32–40 and even fewer have measured these changes for 2 or more years.30,37,38,40 Understanding how perceptions about an EHR change over time is important, because single time point measurements cannot reveal trends.
Here we describe a 2-year prospective, longitudinal survey of ambulatory care providers in 3 clinical areas (family medicine, general pediatrics, and internal medicine) where an EHR implementation occurred within a longstanding, mature health information technology environment. The survey assessed perceptions about a second-generation EHR among physicians with experience using an existing homegrown EHR. We tested the hypothesis that perceptions would follow a J-curve pattern, in which measures would initially decrease but then rise to surpass their baseline (pre-implementation) levels. Such a pattern, well described in other settings,41 should signify a successful EHR adoption, even if satisfaction temporarily dropped.
METHODS
Institutional setting
In 1998 the University of Michigan Health System (UMHS) implemented a homegrown EHR, CareWeb, which was used by all clinicians for creating and viewing documentation, as well as viewing test results, vital signs, and other data. CareWeb was integrated with multiple vendor systems, including an outpatient e-prescribing system.
In August 2012, UMHS transitioned all ambulatory providers to a primary vendor system, Epic (Epic Systems, Verona, WI, USA), locally renamed MiChart. Prior to implementation, all physicians received training, and clinical groups had invested substantial resources developing customized content, including order sets, documentation templates, and other anticipated time-saving components.
Survey development
We developed a brief survey with input from physicians in 3 clinical departments: family medicine, pediatrics, and internal medicine. Experts in clinical and health informatics and survey design also provided input. Questions covered themes including data entry, communication, safety, reminders and alerts, workflow and efficiency, job satisfaction, and overall perceptions about the transition from the old to the new EHR (see Appendix). Most questions were based on 5-point attitude scales (“disagree strongly” to “agree strongly”) and 5-point behavioral frequency scales (“never” to “all of the time”). Participants could also leave free-text comments. We used the online survey platform Qualtrics (Provo, UT, USA). This study was reviewed and exempted by our medical school’s institutional review board.
Survey deployment
Attending physicians in the 3 clinical areas were invited by e-mail to take the survey at baseline 1 month before the implementation, and then 3, 6, 13, and 25 months after the implementation, hereafter referred to as −1, +3, +6, +13, and +25 months. Residents (ie, physicians in training) were not included and no incentives were provided. Only those in the cohort invited to participate in the pre-implementation survey were invited to take subsequent surveys, so as to include only those who had experience with both the old and new EHRs.
Data analysis
Only completed surveys were included in our analysis, using the RR1 definition from the American Association for Public Opinion Research.42 For our analysis we used the 2 positive responses for each question (“slightly agree” and “strongly agree”) for the numerator when determining the percentages reported. We calculated 95% binomial confidence intervals with the Pearson-Klopper method, using the “binom” package (v1.1-1) within R v2.15.3. Line graphs depicting responses over time were also made using R. Free-text comments were selected to illustrate various sentiments from the respondents. For internal medicine, results from primary care physicians (eg, general internal medicine) were reported separately from specialty physicians (eg, nephrology) in addition to reporting the aggregate results. The Appendix details the approach for determining curve shapes.
RESULTS
Response rates varied from a high of 76% for general pediatricians at +13 months to a low of 23% for internal medicine specialty physicians at –1 month (Table 1). Longitudinal responses for each group are shown in Table 2, including overall trend lines and curve shape descriptions. The Appendix contains additional analyses demonstrating no evidence of selective attrition among those with positive or negative views at baseline; no difference between the minority of participants who responded at a single time point compared to the majority who responded at multiple time points; and additional longitudinal paired analyses for participants who responded at multiple time points.
Table 1.
Survey response rates, reported as number of responses/total surveys senta (% response rate)
| Clinical Specialty | −1 month | +3 months | +6 months | +13 months | +25 months |
|---|---|---|---|---|---|
| Family Medicine | 36/75 (48) | 44/75 (59) | 40/75 (53) | 27/71 (38) | 36/67 (54) |
| General Pediatrics | 26/44 (59) | 28/43 (65) | 31/42 (74) | 29/38 (76) | 25/35 (71) |
| Internal Medicine | 112/413 (27) | 164/413 (40) | 122/413 (30) | 147/413 (36) | 118/413 (29) |
| Primary Care | 37/85 (44) | 35/85 (41) | 24/85 (28) | 34/85 (40) | 35/85 (41) |
| Specialty | 75/328 (23) | 129/328 (39) | 98/328 (30) | 113/328 (35) | 83/328 (25) |
| Overall | 174/532 (33) | 236/531 (44) | 193/530 (36) | 203/522 (39) | 179/515 (35) |
aThe number of potential respondents in the denominator varied each month for family medicine and pediatrics as faculty left the institution permanently or were out temporarily (eg, maternity leave). Internal medicine was not able to provide data on faculty attrition, and thus the denominator for that group remained unchanged throughout the study period.
Table 2.
Survey responses at 5 time points along the EHR implementation
|
Theme: Data Entry (Location and Timing) | ||||||
|---|---|---|---|---|---|---|
| 1. Physicians entering data into the medical record (including dictation) on clinical workdays in the patient rooms with the patient, often or all of the time | ||||||
| Clinical Specialty | −1 month | + 3 months | + 6 months | + 13 months | + 25 months | |
| Family Medicine | 7 (19) [8-36] | 17 (39) [24-55] | 16 (40) [25-57] | 16 (59) [39-78] | 21 (58) [41-74] | 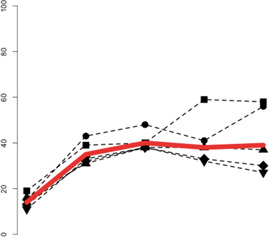 |
| General Pediatrics | 4 (15) [4-35] | 12 (43) [24-63] | 15 (48) [30-67] | 12 (41) [24-61] | 14 (56) [35-76] | |
| Internal Medicine | 14 (13) [7-20] | 53 (32) [25-40] | 46 (38) [29-47] | 49 (33) [26-42] | 35 (30) [22-39] | |
| Primary Care | 6 (16) [6-32] | 11 (31) [17-49] | 9 (38) [19-59] | 13 (38) [22-56] | 13 (37) [21-55] | |
| Specialty | 8 (11) [5-20] | 42 (33) [25-41] | 37 (38) [28-48] | 36 (32) [23-41] | 22 (27) [17-37] | |
| Overall | 25 (14) [10-20] | 82 (35) [29-41] | 77 (40) [33-47] | 77 (38) [32-45] | 70 (39) [32-46] | “inverted L curve” |
| 2. Physicians entering data into the medical record (including dictation) on evenings/nights of clinical workdays, often or all of the time | ||||||
|---|---|---|---|---|---|---|
| Clinical Specialty | −1 month | + 3 months | + 6 months | + 13 months | + 25 months | |
| Family Medicine | 22 (61) [43-77] | 32 (73) [57-85] | 28 (70) [53-83] | 20 (74) [54-89] | 24 (67) [49-81] | 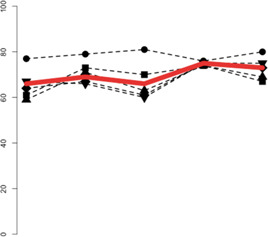 |
| General Pediatrics | 20 (77) [56-91] | 22 (79) [59-92] | 25 (81) [63-93] | 22 (76) [56-90] | 20 (80) [59-93] | |
| Internal Medicine | 72 (64) [55-73] | 110 (67) [59-74] | 74 (61) [51-69] | 110 (75) [67-82] | 86 (73) [64-81] | |
| Primary Care | 22 (59) [42-75] | 25 (71) [54-85] | 15 (63) [41-81] | 25 (74) [56-87] | 24 (69) [51-83] | |
| Specialty | 50 (67) [55-77] | 85 (66) [57-74] | 59 (60) [50-70] | 85 (75) [66-83] | 62 (75) [64-84] | |
| Overall | 114 (66) [58-72] | 164 (69) [63-75] | 127 (66) [59-72] | 152 (75) [68-80] | 130 (73) [66-79] | “flat line” |
| 3. Physicians entering data into the medical record (including dictation) on days off (weekdays or weekends), often or all of the time | ||||||
|---|---|---|---|---|---|---|
| Clinical Specialty | −1 month | + 3 months | + 6 months | + 13 months | + 25 months | |
| Family Medicine | 15 (42) [26-59] | 19 (43) [28-59] | 19 (48) [32-64] | 12 (44) [25-65] | 15 (42) [26-59] | 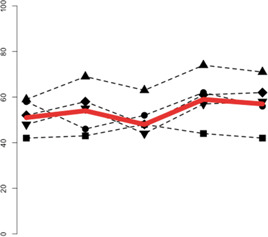 |
| General Pediatrics | 15 (58) [37-77] | 13 (46) [28-66] | 16 (52) [33-70] | 18 (62) [42-79] | 14 (56) [35-76] | |
| Internal Medicine | 58 (52) [42-61] | 95 (58) [50-66] | 58 (48) [38-57] | 89 (61) [52-68] | 73 (62) [52-71] | |
| Primary Care | 22 (59) [42-75] | 24 (69) [51-83] | 15 (63) [41-81] | 25 (74) [56-87] | 25 (71) [54-85] | |
| Specialty | 36 (48) [36-60] | 71 (55) [46-64] | 43 (44) [34-54] | 64 (57) [47-66] | 48 (58) [46-69] | |
| Overall | 88 (51) [43-58] | 127 (54) [47-60] | 93 (48) [41-55] | 119 (59) [52-65] | 102 (57) [50-64] | “flat line” |
|
Theme: Communication | ||||||
|---|---|---|---|---|---|---|
| 4. Physicians who agree that the EHRa enables the creation of high-quality documentation | ||||||
| Clinical Specialty | −1 month | + 3 months | + 6 months | + 13 months | + 25 months | |
| Family Medicine | 35 (97) [85-100] | 9 (20) [10-35] | 8 (20) [9-36] | 10 (37) [19-58] | 7 (19) [8-36] | 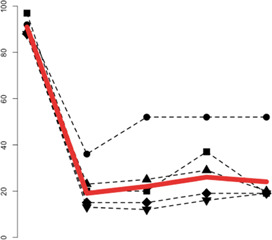 |
| General Pediatrics | 24 (92) [75-99] | 10 (36) [19-56] | 16 (52) [33-70] | 15 (52) [33-71] | 13 (52) [31-72] | |
| Internal Medicine | 99 (88) [81-94] | 25 (15) [10-22] | 18 (15) [9-22] | 28 (19) [13-26] | 23 (19) [13-28] | |
| Primary Care | 33 (89) [75-97] | 8 (23) [10-40] | 6 (25) [10-47] | 10 (29) [15-47] | 7 (20) [8-37] | |
| Specialty | 66 (88) [78-94] | 17 (13) [8-20] | 12 (12) [6-20] | 18 (16) [10-24] | 16 (19) [11-29] | |
| Overall | 158 (91) [86-94] | 44 (19) [14-24] | 42 (22) [17-28] | 53 (26) [21-3] | 43 (24) [18-31] | “L curve” |
| 5. Physicians who agree that the EHRa does not interfere with the ability to have face-to-face contact with patients | ||||||
|---|---|---|---|---|---|---|
| Clinical Specialty | −1 month | + 3 months | + 6 months | + 13 months | + 25 months | |
| Family Medicine | 33 (92) [78-98] | 5 (11) [4-25] | 5 (13) [4-27] | 4 (15) [4-34] | 6 (17) [6-33] | 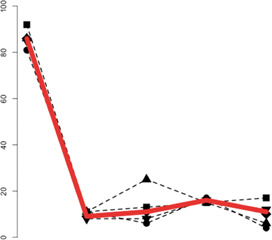 |
| General Pediatrics | 21 (81) [61-93] | 3 (11) [2-28] | 2 (6) [1-21] | 5 (17) [6-36] | 1 (4) [0-20] | |
| Internal Medicine | 96 (86) [78-92] | 14 (9) [5-14] | 14 (11) [6-19] | 23 (16) [10-23] | 12 (10) [5-17] | |
| Primary Care | 32 (86) [71-95] | 4 (11) [3-27] | 6 (25) [10-47] | 5 (15) [5-31] | 2 (6) [1-19] | |
| Specialty | 64 (85) [75-92] | 10 (8) [4-14] | 8 (8) [4-15] | 18 (16) [10-24] | 10 (12) [6-21] | |
| Overall | 150 (86) [80-91] | 22 (9) [6-14] | 21 (11) [7-16] | 32 (16) [11-21] | 19 (11) [7-16] | “L curve” |
| 6. Physicians who agree that the EHRa supports the ability to interact with patients in a meaningful way | ||||||
| Clinical Specialty | −1 month | + 3 months | + 6 months | + 13 months | + 25 months | |
| Family Medicine | 34 (94) [81-99] | 4 (9) [3-22] | 6 (15) [6-30] | 6 (22) [9-42] | 9 (25) [12-42] | 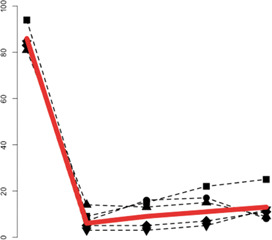 |
| General Pediatrics | 22 (85) [65-96] | 2 (7) [1-24] | 5 (16) [5-34] | 5 (17) [6-36] | 2 (8) [1-26] | |
| Internal Medicine | 93 (83) [75-89] | 9 (5) [3-10] | 6 (5) [2-10] | 11 (7) [4-13] | 13 (11) [6-18] | |
| Primary Care | 30 (81) [65-92] | 5 (14) [5-30] | 3 (13) [3-32] | 5 (15) [5-31] | 3 (9) [2-23] | |
| Specialty | 63 (84) [74-91] | 4 (3) [1-8] | 3 (3) [1-9] | 6 (5) [2-11] | 10 (12) [6-21] | |
| Overall | 149 (86) [80-90] | 15 (6) [4-10] | 17 (9) [6-14] | 22 (11) [7-16] | 24 (13) [9-19] | “L curve” |
|
Theme: Safety | ||||||
|---|---|---|---|---|---|---|
| 7. Physicians who agree that the EHRa has improved patient safety by helping to avoid problems or mistakes | ||||||
| Clinical Specialty | −1 month | + 3 months | + 6 months | + 13 months | + 25 months | |
| Family Medicine | 20 (56) [38-72] | 6 (14) [5-27] | 7 (18) [7-33] | 7 (26) [11-46] | 15 (42) [26-59] | 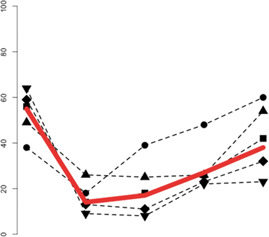 |
| General Pediatrics | 10 (38) [20-59] | 5 (18) [6-37] | 12 (39) [22-58] | 14 (48) [29-67] | 15 (60) [39-79] | |
| Internal Medicine | 66 (59) [49-68] | 21 (13) [8-19] | 14 (11) [6-19] | 34 (23) [17-31] | 38 (32) [24-41] | |
| Primary Care | 18 (49) [32-66] | 9 (26) [12-43] | 6 (25) [10-47] | 9 (26) [13-44] | 19 (54) [37-71] | |
| Specialty | 48 (64) [52-75] | 12 (9) [5-16] | 8 (8) [4-15] | 25 (22) [15-31] | 19 (23) [14-33] | |
| Overall | 96 (55) [48-62] | 32 (14) [8-19] | 33 (17) [12-23] | 55 (27) [21-34] | 68 (38) [31-45] | “L curve” |
|
Theme: Reminders and Alerts | ||||||
|---|---|---|---|---|---|---|
| 8. Physicians who agree that the EHRa provides reminders about important actions or items (eg, labs, studies, procedures, vaccines, documentation) for which the patient is due that might have otherwise been forgotten or overlooked | ||||||
| Clinical Specialty | −1 month | + 3 months | + 6 months | + 13 months | + 25 months | |
| Family Medicine | 30 (83) [67-94] | 14 (32) [19-48] | 12 (30) [17-47] | 14 (52) [32-71] | 26 (72) [55-86] | 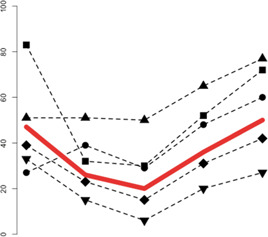 |
| General Pediatrics | 7 (27) [12-48] | 11 (39) [22-59] | 9 (29) [14-48] | 14 (48) [29-67] | 15 (60) [39-79] | |
| Internal Medicine | 44 (39) [30-49] | 37 (23) [16-30] | 18 (15) [9-22] | 45 (31) [23-39] | 49 (42) [33-51] | |
| Primary Care | 19 (51) [34-68] | 18 (51) [34-69] | 12 (50) [29-71] | 22 (65) [46-80] | 27 (77) [60-90] | |
| Specialty | 25 (33) [23-45] | 19 (15) [9-22] | 6 (6) [2-13] | 23 (20) [13-29] | 22 (27) [17-37] | |
| Overall | 81 (47) [39-54] | 62 (26) [21-32] | 39 (20) [15-26] | 73 (36) [30-43] | 90 (50) [43-58] | “U curve” |
| Theme: Workflow and Efficiency | ||||||
|
9. Physicians who agree that the EHRa enables the completion of documentation in a timely manner | ||||||
| Clinical Specialty | −1 month | + 3 months | + 6 months | + 13 months | + 25 months | |
| Family Medicine | 23 (64) [46-79] | 15 (34) [20-50] | 10 (25) [13-41] | 13 (48) [29-68] | 16 (44) [28-62] | 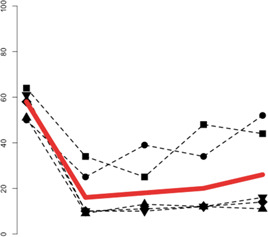 |
| General Pediatrics | 13 (50) [30-70] | 7 (25) [11-45] | 12 (39) [22-58] | 10 (34) [18-54] | 13 (52) [31-72] | |
| Internal Medicine | 65 (58) [48-67] | 16 (10) [6-15] | 13 (11) [6-18] | 18 (12) [7-19] | 17 (14) [9-22] | |
| Primary Care | 19 (51) [34-68] | 3 (9) [2-23] | 3 (13) [3-32] | 4 (12) [3-27] | 4 (11) [3-27] | |
| Specialty | 46 (61) [49-72] | 13 (10) [5-17] | 10 (10) [5-18] | 14 (12) [7-20] | 13 (16) [9-25] | |
| Overall | 101 (58) [51-65] | 38 (16) [12-21] | 35 (18) [13-24] | 41 (20) [15-26] | 46 (26) [20-33] | “L curve” |
|
10. Physicians who agree that the EHRa has eliminated work that they used to have to do | ||||||
|---|---|---|---|---|---|---|
| Clinical Specialty | −1 month | + 3 months | + 6 months | + 13 months | + 25 months | |
| Family Medicine | N/A | 9 (20) [10-35] | 8 (20) [9-36] | 10 (37) [19-58] | 7 (19) [8-36] | 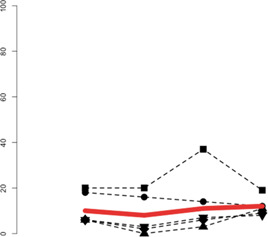 |
| General Pediatrics | N/A | 5 (18) [6-37] | 5 (16) [5-34] | 4 (14) [4-32] | 3 (12) [3-31] | |
| Internal Medicine | N/A | 10 (6) [3-11] | 3 (2) [1-7] | 9 (6) [3-11] | 11 (9) [5-16] | |
| Primary Care | N/A | 2 (6) [1-19] | 0 (0) [0-14] | 1 (3) [0-15] | 4 (11) [3-27] | |
| Specialty | N/A | 8 (6) [3-12] | 3 (3) [1-9] | 8 (7) [3-13] | 7 (8) [3-17] | |
| Overall | N/A | 24 (10) [7-15] | 16 (8) [5-13] | 23 (11) [8-16] | 21 (12) [8-17] | “flat line” |
| 11. Physicians who agree that the EHRa has created new work that they now must do | ||||||
| Clinical Specialty | −1 month | + 3 months | + 6 months | + 13 months | + 25 months | |
| Family Medicine | N/A | 42 (95) [85-99] | 40 (100) [91-100] | 27 (100) [87-100] | 36 (100) [90-100] | 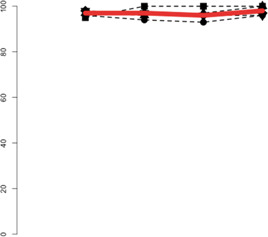 |
| General Pediatrics | N/A | 27 (96) [82-100] | 29 (94) [79-99] | 27 (93) [77-99] | 24 (96) [80-100] | |
| Internal Medicine | N/A | 160 (98) [94-99] | 118 (97) [92-99] | 141 (96) [91-98] | 115 (97) [93-99] | |
| Primary Care | N/A | 34 (97) [85-100] | 23 (96) [79-100] | 33 (97) [85-100] | 35 (100) [90-100] | |
| Specialty | N/A | 126 (98) [93-100] | 95 (97) [91-99] | 108 (96) [90-99] | 80 (96) [90-99] | |
| Overall | N/A | 229 (97) [94-99] | 187 (97) [93-99] | 195 (96) [92-98] | 175 (98) [94-99] | “flat line” |
|
Theme: Job Satisfaction | ||||||
|---|---|---|---|---|---|---|
| 12. Physicians who report being satisfied with their overall job | ||||||
| Clinical Specialty | −1 month | + 3 months | + 6 months | + 13 months | + 25 months | |
| Family Medicine | 33 (92) [78-98] | 18 (41) [26-57] | 22 (55) [38-71] | 13 (48) [29-68] | 22 (61) [43-77] | 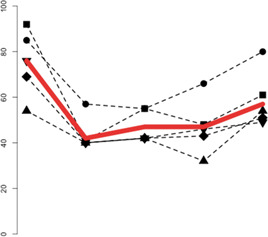 |
| General Pediatrics | 22 (85) [65-96] | 16 (57) [37-76] | 17 (55) [36-73] | 19 (66) [46-82] | 20 (80) [59-93] | |
| Internal Medicine | 77 (69) [59-77] | 66 (40) [33-48] | 51 (42) [33-51] | 63 (43) [35-51] | 60 (51) [41-60] | |
| Primary Care | 20 (54) [37-71] | 14 (40) [24-58] | 10 (42) [22-63] | 11 (32) [17-51] | 19 (54) [37-71] | |
| Specialty | 57 (76) [65-85] | 52 (40) [32-49] | 41 (42) [32-52] | 52 (46) [37-56] | 41 (49) [38-61] | |
| Overall | 132 (76) [69-82] | 100 (42) [36-49] | 90 (47) [40-54] | 95 (47) [40-54] | 102 (57) [50-64] | “L curve” |
| 13. Physicians who report that the EHRa has had a positive impact on their job satisfaction | ||||||
|---|---|---|---|---|---|---|
| Clinical Specialty | −1 month | + 3 months | + 6 months | + 13 months | + 25 months | |
| Family Medicine | 23 (64) [46-79] | 5 (11) [4-25] | 2 (5) [1-17] | 5 (19) [6-38] | 4 (11) [3-26] | 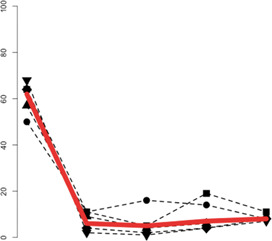 |
| General Pediatrics | 13 (50) [30-70] | 3 (11) [2-28] | 5 (16) [5-34] | 4 (14) [4-32] | 2 (8) [1-26] | |
| Internal Medicine | 72 (64) [55-73] | 6 (4) [1-8] | 2 (2) [0-6] | 6 (4) [2-9] | 9 (8) [4-14] | |
| Primary Care | 21 (57) [39-73] | 3 (9) [2-23] | 1 (4) [0-21] | 2 (6) [1-20] | 3 (9) [2-23] | |
| Specialty | 51 (68) [56-78] | 3 (2) [0-7] | 1 (1) [0-6] | 4 (4) [1-9] | 6 (7) [3-15] | |
| Overall | 108 (62) [55-69] | 14 (6) [4-10] | 9 (5) [2-9] | 15 (7) [5-12] | 15 (8) [5-13] | “L curve” |
|
Theme: Looking Forward | ||||||
|---|---|---|---|---|---|---|
| 14. Physicians who agree that MiChart will allow them to provide better care for their patients than CareWeb | ||||||
| Clinical Specialty | −1 month | + 3 months | + 6 months | + 13 months | + 25 months | |
| Family Medicine | 14 (39) [23-57] | 6 (14) [5-27] | 6 (15) [6-30] | 8 (30) [14-50] | 9 (25) [12-42] | 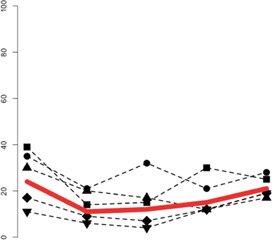 |
| General Pediatrics | 9 (35) [17-56] | 6 (21) [8-41] | 10 (32) [17-51] | 6 (21) [8-40] | 7 (28) [12-49] | |
| Internal Medicine | 19 (17) [11-25] | 15 (9) [5-15] | 8 (7) [3-13] | 17 (12) [7-18] | 22 (19) [12-27] | |
| Primary Care | 11 (30) [16-47] | 7 (20) [8-37] | 4 (17) [5-37] | 4 (12) [3-27] | 6 (17) [7-34] | |
| Specialty | 8 (11) [5-20] | 8 (6) [3-12] | 4 (4) [1-10] | 13 (12) [6-19] | 16 (19) [11-29] | |
| Overall | 42 (24) [18-31] | 27 (11) [8-16] | 24 (12) [9-18] | 31 (15) [11-21] | 38 (21) [16-28] | “flat line” |
All responses are reported as No. (%) [95% CI]. The line graphs to the right are visualizations of the positive responses for each question; the y-axis shows the percentage of positive responses from 0 to 100, whereas the x-axis represents the time points. Below each line graph is the curve shape, as described in the Appendix. Note that the time points on the x-axis are shown at equal intervals although the actual study time intervals varied. Larger versions of each line graph can be found in the Appendix.
N/A: Not asked in this phase. aCareWeb in the pre-implementation phase and MiChart in the post-implementation phases. Filled square: family medicine. filled circle: general pediatrics; filled rhombus: internal medicine; filled triangle: internal medicine, primary care; filled inverted triangle: internal medicine, specialty.
For the data entry theme, the frequency of entering data while in the examination room with the patient increased (Q1), but respondents noted little change in the frequency of entering data during clinical workday evenings or on days off (Q2–3). Whereas most physicians agreed that the prior EHR supported various aspects of communication, there was a large drop in these measures across all groups that persisted 2 years post implementation (Q4–6).
Regarding safety (Q7), positive perceptions dropped substantially for about the first 6 months, then began to rise. While the overall graph displays an L-curve (remaining below baseline), a U-curve (return to baseline) was observed for family medicine, pediatrics, and primary care internal medicine. A drop and subsequent rise back to baseline was observed for the reminders and alerts measure (Q8).
For workflow and efficiency (Q9–11), 58% of respondents believed that the prior EHR allowed them to complete their documentation in a timely manner (Q9), which ultimately dropped to 26% with the new system. Across all specialties, few reported that the new EHR eliminated work they used to have to do (Q10), and nearly everyone reported that the new EHR created new work (Q11), a sentiment that remained stable over the study period.
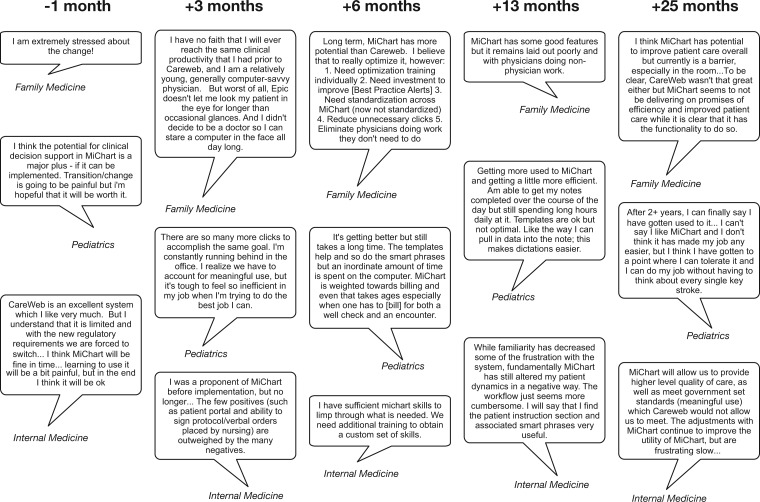
Overall job satisfaction (Q12) dropped after the implementation. While it did rise slightly over time, it never reached baseline levels by +25 months. When participants were asked about the EHR’s contribution to their job satisfaction (Q13), positive views dropped from a high of 62% with the prior EHR to 8% with the new EHR. At no point did a majority of respondents believe that the new EHR would allow them to provide better care than the original EHR (Q14). A subset of the 559 comments left by the physicians is shown in Figure 1.
Figure 1.
Illustrative quotes representing sentiments expressed at the different time points during the longitudinal survey. These were drawn from 559 comments left by the respondents, totaling 56 303 words. Quotes from the same specialty are not necessarily from the same physicians each time. Note that CareWeb was the legacy homegrown EHR used from 1998 to 2012, and MiChart is the local name for the replacement vendor EHR.
DISCUSSION
Overall, we did not find evidence for J-curve patterns up to 2 years post EHR implementation. The only significant increase over baseline 2 years post implementation was for documenting while in exam rooms with patients. Most measures fell and remained below baseline, and only 1 (reminders and alerts) returned to baseline. These findings are worth discussing in the context of similar work. Some EHR implementation studies have shown improvements in productivity,32,33 quality of care,32 safety,37 and overall perceptions,34 but others have had mixed results.19 Differences of opinion among providers exist: a recent survey found that 38% of family medicine physicians, 36% of primary care internal medicine physicians, and 29% of specialists felt that their EHR improved care, but higher percentages of physicians in each group thought it worsened care.43 An older study from 2004 found lower satisfaction among internal medicine physicians compared to pediatricians who used an EHR within the same institution.44 This raises questions about how well EHRs meet the diverse needs of various specialties.45
A 2014 survey of providers revealed that many measures of EHR perception improved over time.38 However, some measures did not improve, including patient engagement and care coordination. Even after 2 years, 27% felt that the EHR was not meeting their practice’s needs. Another EHR implementation study in a pediatric emergency department found multiple metrics returning to baseline as early as 3 months.39
The variable time frames reported in prior studies make comparisons difficult. Experts have concluded that a “ramp-up” period33 or a “shakedown phase”46 is needed to achieve routine EHR use, lasting from 6 to 12 months. Our results suggest that even if routine use occurs by 12 months, perceptions can continue to change.
Three months remains a common duration before post-implementation studies began,9,27,28 but that may be too early for perceptions to stabilize. Longitudinal assessments, therefore, are important for capturing changing patterns. Studies lasting less than a year may show decreases in some measures28,47 that may increase after the study period.35 One study reported the opposite; that is, productivity “gains” found at 3 months post implementation did not persist.48 Several studies have observed that it may require 2 years before significant benefits from and satisfaction with an EHR are achieved.6,49 One report suggested that 5 years may be needed for benefits to be observed,50 whereas another study found EHR concerns persisting beyond 5 years.18 One thing is certain: “The optimal time period for assessment of time efficiencies post-implementation of EHRs remains a challenge and will require further research.”48
Physicians in our study had increasing data capture and documentation requirements51 (eg, Meaningful Use)52 that coincided with the EHR implementation. Our prior EHR had fewer capabilities than its replacement, so it may be that physicians’ perceptions about increased work was due to the fact that they were accomplishing more.53 One study found that physicians using an EHR with many functions, such as the one we implemented, had higher stress and time pressures, perhaps “trying to balance an increase in tasks with no increases in time allotted.”54
Simpler EHRs may be perceived more positively by clinicians eager to spend more time with their patients and less with their computers.55–58 There may also be differences between organizational and clinical needs for an EHR.59 Strategies have been proposed to improve satisfaction with EHRs.60,61 Major changes can be emotional for physicians,62 and our institution has ongoing efforts to improve physician efficiency and satisfaction. Additional surveys should clarify if satisfaction and perceptions continue to improve.
While our study was conducted at a single center, we surveyed 3 distinct clinical groups. We did not capture demographics, but age and gender may not be significant predictors of EHR satisfaction44 or, as in earlier times, computer anxiety.63 We also acknowledge that some of our response rates were low, but it is worth noting that for multiple measures the low response rate groups tracked closely with the high response rate groups, and that low response rates for physicians does not necessarily introduce bias.64–69 Physicians with the lowest satisfaction may have chosen to leave,12,70 and therefore may not have completed the surveys, resulting in a positive bias. Alternatively, unhappy users may have been motivated to respond. Despite these opposing possibilities, we did not observe differences in survey attrition rates among those responding positively vs negatively at baseline. Even if we are unable to generalize to the entire physician population, a substantial minority had persistent concerns even 2 years post implementation, and this should be considered in the context of an “emerging EHR monoculture.”71
CONCLUSION
In this prospective, longitudinal survey of physicians lasting 2 years post EHR implementation, we did not find evidence for a J-curve pattern with respect to positive perceptions eventually exceeding baseline measures. Some measures followed a U-curve (returned to baseline), or flatlined, while most followed an L-curve (fell and remained below baseline). Future research is warranted to determine if positive perceptions eventually surpass baseline, and what interventions can help physicians use EHRs more effectively.
Supplementary Material
ACKNOWLEDGMENTS
We would like to thank the physicians who took time out of their busy schedules to complete the surveys and provide feedback during the multiple phases of this study.
CONFLICT OF INTEREST
The authors have no conflicts of interest to report.
CONTRIBUTORS
David Hanauer: Conception and design of the study, analysis, and interpretation of the data, drafting the manuscript
Greta Branford: Conception and design of the study, survey lead for internal medicine
Grant Greenberg: Conception and design of the study, survey lead for family medicine, drafting the manuscript
Sharon Kileny: Conception and design of the study, survey lead for general pediatrics
Mick Couper: Conception and design of the study, analysis and interpretation of the data, drafting the manuscript
Kai Zheng: Conception and design of the study
Sung Choi: Analysis and interpretation of the data, drafting the manuscript
All authors approved the final version to be published and agree to be accountable for all aspects of the work.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
REFERENCES
- 1. Office of the National Coordinator for Health Information Technology. Office-based Physician Electronic Health Record Adoption: 2004-2014. Health IT. Quick-Stat #50. http://dashboard.healthit.gov/quickstats/pages/physician-ehr-adoption-trends.php. Accessed on February 28, 2016.
- 2. Charles D, Gabriel M, Searcy T. Adoption of electronic health record systems among U.S. non-federal acute care hospitals: 2008-2014. ONC Data Brief, no. 23. Office of the National Coordinator for Health Information Technology: Washington, DC; 2015. [Google Scholar]
- 3. Joseph S, Sow M, Furukawa MF, et al. HITECH spurs EHR vendor competition and innovation, resulting in increased adoption. Am J Manag Care. 2014;209:734–740. [PubMed] [Google Scholar]
- 4. Burke HB, Sessums LL, Hoang A, et al. Electronic health records improve clinical note quality. J Am Med Inform Assoc. 2015;221:199–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chaudhry B, Wang J, Wu S, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006;14410:742–752. [DOI] [PubMed] [Google Scholar]
- 6. King J, Patel V, Jamoom EW, et al. Clinical benefits of electronic health record use: national findings. Health Serv Res. 2014;49(1 Pt 2):392–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zlabek JA, Wickus JW, Mathiason MA. Early cost and safety benefits of an inpatient electronic health record. J Am Med Inform Assoc. 2011;182:169–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Adler-Milstein J, Green CE, Bates DW. A survey analysis suggests that electronic health records will yield revenue gains for some practices and losses for many. Health Aff (Millwood). 2013;323:562–570. [DOI] [PubMed] [Google Scholar]
- 9. Benda NC, Meadors ML, Zachary Hettinger A, et al. Emergency physician task switching increases with the introduction of a commercial electronic health record. Ann Emerg Med. 2015. [DOI] [PubMed] [Google Scholar]
- 10. Bloom MV, Huntington MK. Faculty, resident, and clinic staff's evaluation of the effects of EHR implementation. Family Med. 2010;428:562–566. [PubMed] [Google Scholar]
- 11. Hirsch IB. Ranting in 2016: a medical system in crisis. Diabetes Technol Ther. 2016;182:110–112. [DOI] [PubMed] [Google Scholar]
- 12. Howard J, Clark EC, Friedman A, et al. Electronic health record impact on work burden in small, unaffiliated, community-based primary care practices. J Gen Intern Med. 2013;281:107–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kane L, Chesanow N. Medscape EHR Report 2014. http://www.medscape.com/features/slideshow/public/ehr2014. Accessed on October 5, 2015. [Google Scholar]
- 14. Leu MG, O'Connor KG, Marshall R, et al. Pediatricians' use of health information technology: a national survey. Pediatrics. 2012;1306:e1441–e1446. [DOI] [PubMed] [Google Scholar]
- 15. McAlearney AS, Robbins J, Hirsch A, et al. Perceived efficiency impacts following electronic health record implementation: an exploratory study of an urban community health center network. Int J Med Inform. 2010;7912:807–816. [DOI] [PubMed] [Google Scholar]
- 16. McDonald CJ, Callaghan FM, Weissman A, et al. Use of internists’ free time by ambulatory care Electronic Medical Record systems. JAMA Int Med. 2014;17411:1860–1863. [DOI] [PubMed] [Google Scholar]
- 17. Woolhandler S, Himmelstein DU. Administrative work consumes one-sixth of U.S. physicians' working hours and lowers their career satisfaction. Int J Health Services. 2014;444:635–642. [DOI] [PubMed] [Google Scholar]
- 18. Makam AN, Lanham HJ, Batchelor K, et al. The good, the bad and the early adopters: providers' attitudes about a common, commercial EHR. J Eval Clin Pract. 2014;201:36–42. [DOI] [PubMed] [Google Scholar]
- 19. Nguyen L, Bellucci E, Nguyen LT. Electronic health records implementation: an evaluation of information system impact and contingency factors. Int J Med Inform. 2014;8311:779–796. [DOI] [PubMed] [Google Scholar]
- 20. American College of Physicians. Survey of Clinicians: User Satisfaction with Electronic Health Records Has Decreased Since 2010. https://www.acponline.org/newsroom/ehrs_survey.htm. Accessed on October, 2015.
- 21. Rosenbaum L. Transitional Chaos or Enduring Harm? The EHR and the Disruption of Medicine. N Engl J Med. 2015;37317:1585–1588. [DOI] [PubMed] [Google Scholar]
- 22. Wylie MC, Baier RR, Gardner RL. Perceptions of electronic health record implementation: a statewide survey of physicians in Rhode Island. Am J Med. 2014;12710:1010. e21–e27. [DOI] [PubMed] [Google Scholar]
- 23. Let Doctors Be Doctors. http://www.letdoctorsbedoctors.com/pdfs/LDBD_Infographic.pdf. Accessed on February 28, 2016.
- 24. Abramson EL, Malhotra S, Fischer K, et al. Transitioning between electronic health records: effects on ambulatory prescribing safety. J Gen Intern Med. 2011;268:868–874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Abramson EL, Patel V, Malhotra S, et al. Physician experiences transitioning between an older versus newer electronic health record for electronic prescribing. Int J Med Inform. 2012;818:539–548. [DOI] [PubMed] [Google Scholar]
- 26. Gettinger A, Csatari A. Transitioning from a legacy EHR to a commercial, vendor-supplied EHR: one academic health system's experience. Appl Clin Inform. 2012;34:367–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pfoh ER, Abramson E, Zandieh S, et al. Satisfaction after the transition between electronic health record systems at six ambulatory practices. J Eval Clin Pract. 2012;186:1133–1139. [DOI] [PubMed] [Google Scholar]
- 28. Zandieh SO, Abramson EL, Pfoh ER, et al. Transitioning between ambulatory EHRs: a study of practitioners' perspectives. J Am Med Inform Assoc. 2012;193:401–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Zandieh SO, Yoon-Flannery K, Kuperman GJ, et al. Challenges to EHR implementation in electronic- versus paper-based office practices. J Gen Intern Med. 2008;236:755–761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Terry AL, Brown JB, Bestard Denomme L, et al. Perspectives on electronic medical record implementation after two years of use in primary health care practice. J AmBoard Family Med. 2012;254:522–527. [DOI] [PubMed] [Google Scholar]
- 31. Terry AL, Giles G, Brown JB, et al. Adoption of electronic medical records in family practice: the providers' perspective. Fam Med. 2009;417:508–512. [PubMed] [Google Scholar]
- 32. Brotzman GL, Guse CE, Fay DL, et al. Implementing an electronic medical record at a residency site: physicians' perceived effects on quality of care, documentation, and productivity. WMJ. 2009;1082:99–103. [PubMed] [Google Scholar]
- 33. Cheriff AD, Kapur AG, Qiu M, et al. Physician productivity and the ambulatory EHR in a large academic multi-specialty physician group. Int J Med Inform. 2010Jul;797:492–500. [DOI] [PubMed] [Google Scholar]
- 34. Chisolm DJ, Purnell TS, Cohen DM, et al. Clinician perceptions of an electronic medical record during the first year of implementaton in emergency services. Pediatric Emergency Care. 2010;262:107–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. El-Kareh R, Gandhi TK, Poon EG, et al. Trends in primary care clinician perceptions of a new electronic health record. J Gen Intern Med. 2009;244:464–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hoonakker PL, Carayon P, Brown RL, et al. Changes in end-user satisfaction with Computerized Provider Order Entry over time among nurses and providers in intensive care units. J Am Med Inform Assoc. 2013;202:252–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. McGuire MJ, Noronha G, Samal L, et al. Patient safety perceptions of primary care providers after implementation of an electronic medical record system. J Gen Intern Med. 2013;282:184–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ryan MS, Shih SC, Winther CH, et al. Does it get easier to use an EHR? Report from an urban regional extension center. J Gen Intern Med. 2014;2910:1341–1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Spellman Kennebeck S, Timm N, Farrell MK, et al. Impact of electronic health record implementation on patient flow metrics in a pediatric emergency department. J Am Med Inform Assoc. 2012;193:443–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Vishwanath A, Singh SR, Winkelstein P. The impact of electronic medical record systems on outpatient workflows: a longitudinal evaluation of its workflow effects. Int J Med Inform. 2010;7911:778–791. [DOI] [PubMed] [Google Scholar]
- 41. Elrod PD, Tippett DD. The “death valley” of change. J Organizational Change Manag. 2002;153:273–291. [Google Scholar]
- 42. The American Association For Public Opinion Research. Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys. 2015. https://www.aapor.org/AAPOR_Main/media/MainSiteFiles/Standard-Definitions2015_8thEd.pdf. Accessed on February 27, 2016. [Google Scholar]
- 43. Verdon DR. Physician outcry on EHR functionality, cost will shake the health information technology sector. February 10, 2014. http://medicaleconomics.modernmedicine.com/medical-economics/content/tags/ehr/physician-outcry-ehr-functionality-cost-will-shake-health-informa. Accessed on October 5, 2015. [Google Scholar]
- 44. O'Connell RT, Cho C, Shah N, et al. Take note(s): differential EHR satisfaction with two implementations under one roof. J Am Med Inform Assoc. 2004;111:43–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Spooner SA. We are still waiting for fully supportive electronic health records in pediatrics. Pediatrics. 2012;1306:e1674–e1676. [DOI] [PubMed] [Google Scholar]
- 46. Sykes TA, Venkatesh V, Rai A. Explaining physicians' use of EMR systems and performance in the shakedown phase. J Am Med Inform Assoc. 2011;182:125–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Mohan MK, Bishop RO, Mallows JL. Effect of an electronic medical record information system on emergency department performance. Med J Aust. 2013;1984:201–204. [DOI] [PubMed] [Google Scholar]
- 48. Poissant L, Pereira J, Tamblyn R, et al. The impact of electronic health records on time efficiency of physicians and nurses: a systematic review. J Am Med Inform Assoc. 2005;125:505–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Menachemi N, Powers T, Au DW, et al. Predictors of physician satisfaction among electronic health record system users. J Healthcare Qual. 2010;321:35–41. [DOI] [PubMed] [Google Scholar]
- 50. Brookstone A. HIMSS13 — EHR Satisfaction Diminishing. March 6, 2013. http://www.americanehr.com/blog/2013/03/himss13-ehr-satisfaction-diminishing/. Accessed on October 5, 2015. [Google Scholar]
- 51. Cusack CM, Hripcsak G, Bloomrosen M, et al. The future state of clinical data capture and documentation: a report from AMIA's 2011 Policy Meeting. J Am Med Inform Assoc. 2013;201:134–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Slight SP, Berner ES, Galanter W, et al. Meaningful use of electronic health records: experiences from the field and future opportunities. JMIR Med Inform. 2015;33:e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Rand CM, Blumkin A, Szilagyi PG. Electronic health record use and preventive counseling for US children and adolescents. J Am Med Inform Assoc. 2014;21(e1):e152–e156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Babbott S, Manwell LB, Brown R, et al. Electronic medical records and physician stress in primary care: results from the MEMO Study. J Am Med Inform Assoc. 2014;21(e1):e100–e106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Frankel RM. Computers in the Examination Room. JAMA Int Med. 2016;1761:128–129. [DOI] [PubMed] [Google Scholar]
- 56. Montague E, Asan O. Dynamic modeling of patient and physician eye gaze to understand the effects of electronic health records on doctor-patient communication and attention. Int J Med Inform. 2014;833:225–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Ratanawongsa N, Barton JL, Lyles CR, et al. Association between clinician computer use and communication with patients in safety-net clinics. JAMA Int Med. 2016;1761:125–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Toll E. A piece of my mind. The cost of technology. JAMA. 2012;30723:2497–2498. [DOI] [PubMed] [Google Scholar]
- 59. Mandl KD, Kohane IS. Escaping the EHR trap—the future of health IT. N Engl J Med. 2012;36624:2240–2242. [DOI] [PubMed] [Google Scholar]
- 60. Sinsky CA, Willard-Grace R, Schutzbank AM, et al. In search of joy in practice: a report of 23 high-functioning primary care practices. Ann Fam Med. 2013;113:272–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Zhang J, Chen Y, Ashfaq S, et al. Strategizing EHR use to achieve patient-centered care in exam rooms: a qualitative study on primary care providers. J Am Med Inform Assoc. 2016;231:137–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Shoolin JS. Change management—recommendations for successful electronic medical records implementation. Appl Clin Inform. 2010;13:286–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Brown SH, Coney RD. Changes in physicians' computer anxiety and attitudes related to clinical information system use. J Am Med Inform Assoc. 1994;15:381–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Bjertnaes OA, Garratt A, Botten G. Nonresponse bias and cost-effectiveness in a Norwegian survey of family physicians. Eval Health Professions. 2008;311:65–80. [DOI] [PubMed] [Google Scholar]
- 65. Cull WL, O'Connor KG, Sharp S, et al. Response rates and response bias for 50 surveys of pediatricians. Health Serv Res. 2005;401:213–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Flanigan TS, McFarlane E, Cook S. Conducting survey research among physicians and other medical professionals: a review of current literature. Proc Survey Res Methods Section, Am Stat Assoc. 2008;2008:4136–4147. [Google Scholar]
- 67. Kellerman SE, Herold J. Physician response to surveys. A review of the literature. Am J Prev Med. 2001;201:61–67. [DOI] [PubMed] [Google Scholar]
- 68. McFarlane E, Olmsted MG, Murphy J, et al. Nonresponse bias in a mail survey of physicians. Eval Health Professions. 2007;302:170–185. [DOI] [PubMed] [Google Scholar]
- 69. Menachemi N, Hikmet N, Stutzman M, et al. Investigating response bias in an information technology survey of physicians. J Med Syst. 2006;304:277–282. [DOI] [PubMed] [Google Scholar]
- 70. Crowson MG, Vail C, Eapen RJ. Influence of electronic medical record implementation on provider retirement at a major academic medical centre. J Eval Clin Pract. 2015;222:222–226. [DOI] [PubMed] [Google Scholar]
- 71. Koppel R, Lehmann CU. Implications of an emerging EHR monoculture for hospitals and healthcare systems. J Am Med Inform Assoc. 2015;222:465–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.