Abstract
Objectives
To identify and characterise a subgroup of patients with early rheumatoid arthritis (RA) reporting not feeling well 1 year after treatment initiation despite achieving optimal disease control according to current treatment standards.
Methods
This observational study included participants of the Care in early RA trial with a rapid and sustained response (DAS28CRP<2.6) from week 16 until year 1 after starting the first RA treatment. Feeling well was assessed at year 1, using five patient-reported outcomes (PROs): pain, fatigue, physical functioning, RA-related quality of life and sleep quality. K-means clustering assigned patients to a cluster based on these PROs. Cohen’s d effect size estimated cluster differences at treatment initiation and week 16, for the five clustering PROs, coping behaviour, illness perceptions and social support.
Results
Analyses revealed three clusters. Of 140 patients, 77.9% were assigned to the ‘concordant to disease activity’ cluster, 9.3% to the ‘dominant fatigue’ cluster and 12.9% to the ‘dominant pain and fatigue’ cluster. Large differences in pain and fatigue reporting were found at week 16 when comparing the ‘concordant’ with the ‘dominant pain and fatigue’ or the ‘dominant fatigue’ cluster. Small differences in reporting were found for the other PROs. Illness perceptions and coping style also differed in the ‘concordant’ cluster.
Conclusions
Although most patients reported PRO scores in concordance with their well-controlled disease activity, one in five persistent treatment responders reported not feeling well at year 1. These patients reported higher pain and fatigue, and different illness perceptions and coping strategies early in the disease course.
Keywords: rheumatoid arthritis, cluster analysis, pain, fatigue, patient-reported outcomes, unmet needs
INTRODUCTION
In the past two decades, major progress has been achieved in the treatment of rheumatoid arthritis (RA), leading to a new generation of patients who experience rapid disease control and are spared from critical joint destructions and disability.1 Hence, patients treated in the current era could be expected to report feeling well. In contrast, it has been observed that the way patients with RA report about their health does not necessarily match with the biomedical evaluation of their disease. For example, patients continue to report moderate-to-high levels of pain and fatigue despite low levels of inflammation.2 3 Likewise, a literature review concluded that many patients with RA continue to report unacceptable levels of pain and fatigue and problems with physical and mental function despite ongoing RA treatment.4
Key messages.
What is already known about this subject?
Some patients with rheumatoid arthritis (RA) report unacceptable levels of pain and fatigue and impaired physical and mental functioning despite ongoing effective treatment.
What does this study add?
Despite the increased interest for unmet needs in RA, limited research focuses on patient-perceived well-being in the early stage of the disease.
This study found that of patients with early RA achieving optimal disease control according to current treatment standards, one in five treatment responders reported not feeling well after 1 year of first RA treatment, mainly because of high fatigue reporting.
These patients are possibly identifiable in the first 4 months of treatment, by including their pain and fatigue levels in the evaluation and considering their beliefs about RA and coping strategies.
How might this impact on clinical practice or future developments?
Attention to this mismatch between disease control and well-being early in the disease could be key in further optimising the clinical course of newly diagnosed patients with RA.
This discrepancy was also demonstrated in the early stage of the disease. Steunebrink and colleagues showed that more than one-third of patients with early RA perceived their health as not improving at all after 1 year of treatment, even despite a good clinical response.5 How patients view and interpret their disease is, however, particularly important early in the disease course, as adequate illness beliefs might help patients in adjusting to their chronic illness.6 Additionally, it has been found that patients’ perceptions about their disease contribute more to their level of pain and functioning than the actual disease status in RA.7
Altogether, these prior observations show that controlling joint inflammation and improving patient-reported outcomes (PROs) are different concepts in RA, both requiring attention from care providers.8 In order to optimise the clinical course of newly diagnosed patients with early RA, we need to better understand why, after optimal pharmacological treatment, some of them still feel unwell, whereas their RA is clinically well controlled. We hypothesised that patients who report signs of poor well-being early in the disease course, despite a rapid and persistent clinical response to initial treatment, are at risk of feeling persistently unwell. This assumption was confirmed by our patient researcher. First, we aimed to identify among patients with early RA, with a well-controlled disease from 4 months of initial treatment onwards, subgroups reporting not feeling well after 1 year. Second, we aimed to investigate if these subgroups can be recognised already early in the disease course based on PRO parameters.
PATIENTS AND METHODS
Setting
The present observational study used data of patients with early RA (diagnosed with RA, as defined by the American College of Rheumatology 1987 revised criteria, ≤1 year ago), who started first disease-modifying antirheumatic drug treatment within the Care in early RA (CareRA) trial between January 2009 and May 2013. CareRA is a prospective 2-year randomised open-label pragmatic trial across 13 rheumatology centres in Flanders, Belgium. Different treatment regimens based on the original COBRA (Combination therapy for early RA) strategy were evaluated in CareRA participants in a treat-to-target setting. Alongside the traditional disease evaluation measures, a set of PROs was prospectively collected in the first 2 years of RA treatment. The ethics committee of the University Hospitals Leuven granted approval after consulting the ethics committees of participating centers. All participants gave written informed consent. Details about the protocol and the 2-year results are reported elsewhere.9
Patients
Of the 379 randomised patients in the CareRA trial, only those who completed the first treatment year, who had a DAS28CRP score available at week 16 and who completed PROs at least once throughout the study were considered (n=333/379). Participants of the present study were selected if they had a rapid and sustained treatment response in the first year of treatment, defined as DAS28CRP<2.6 from week 16 after treatment initiation (baseline) until year 1 (week 52).
Measurements
Clinical and demographic measurements included disease activity (DAS28CRP), age, sex, symptom duration and comorbidities. Together with our patient researcher, we selected the PROs and chose the timepoints for evaluation. Patient-reported measurements evaluated at baseline, week 16 and week 52 were pain and fatigue measured by a Visual Analogue Scale (VAS), physical functioning measured by the Health Assessment Questionnaire (HAQ)10 and health-related quality of life measured by the Rheumatoid Arthritis Quality of Life Questionnaire (RAQoL).11 Sleep quality was assessed using the total score of the Pittsburgh Sleep Quality Index (PSQI) that includes seven sleep dimensions: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medications and daytime dysfunction.12 Higher scores indicate worse pain, worse fatigue, more functional loss, worse health-related quality of life and worse sleep quality.
The following additional PROs were evaluated at week 16. Coping was assessed using the Utrecht Coping List, which measures seven coping strategies: active tackling, seeking social support, expressing emotions, fostering reassuring thoughts, avoidance, passive reacting, and palliative response. A higher score indicates more use of a coping strategy.13 Illness perceptions were evaluated by the nine dimensions of the Revised Illness Perception Questionnaire (IPQ-R): identity, consequences, timeline acute/chronic, personal control, treatment control, illness coherence, timeline cyclical, emotional representations, and causes subdivided into psychological attributions, risk factors, immunity, accident, and chance.14 High scores on the identity, consequences, and timeline dimensions indicate strongly held beliefs about the number of symptoms attributed to RA, the negative consequences of RA, and its chronicity and cyclical nature. High scores on the control and coherence dimensions represent positive beliefs about the controllability of RA and a personal understanding of the disease.15 Perceived social support was measured using four scales of the Social Support List Interactions/Discrepancies. Higher scores indicate a stronger experience of either supportive or negative interactions, and of either excessive or insufficient social support (ie, in discrepancy with the desired level of support).16
Statistical analysis
Descriptive data were reported as absolute numbers and proportions for categorical variables, or as means with SD and medians with 25th percentile and 75th percentile for continuous variables.
To identify the profile of patients feeling well or not based on PRO data after 1 year of treatment, we conducted cluster analyses without applying a priori assumptions. First, we selected five PRO measures to evaluate well-being. Hence, the clusters are based upon: week 52 VAS pain, week 52 VAS fatigue, week 52 HAQ, week 52 RAQoL and week 52 PSQI. We applied the Two-Step clustering method that uses the log-likelihood as a distance measure in step 1, and the Akaike information criteria to select the optimal number of clusters in step 2. Second, patients were grouped to this number of clusters by k-means clustering. Sensitivity analyses by hierarchical clustering using the median method with squared Euclidean distance were done to account for skewness in the cluster data.
After clustering, Cohen’s d was calculated to determine the between-cluster difference in scoring for the following PROs: baseline and week 16 pain, fatigue, physical functioning, RA-related quality of life and sleep quality; week 16 coping strategies; week 16 illness perceptions; week 16 perceived social support. Cohen’s d is an effect size (ES), defined as the difference between 2 means divided by a pooled SD. To evaluate the magnitude or size of this difference, we interpreted Cohen’s d values as follows: small effect=0.2–0.5; medium effect=0.5–0.8; large effect≥0.8.17
To deal with missing data, we first applied the manual instructions of the questionnaires, if available. Subsequently, we applied the Expectation–Maximization algorithm provided in SPSS software to impute the remaining missing PRO scores.18 These missing scores were imputed per questionnaire using all available scores at baseline, week 16, week 52 and week 104 for the total CareRA sample (n=379). Missing baseline PRO scores (0.9–10.1%) were not imputed. We performed a sensitivity analysis including only those patients who had complete PRO data available for the cluster analysis.
Data were analysed using IBM SPSS Statistics for Windows, version 25 (Armonk, NY: IBM Corp.). Data interpretation was performed by an interdisciplinary team consisting of a patient researcher, rheumatologists, nurses and clinical researchers with expertise in the field of RA.
This study is reported following the STROBE statement (checklist in Supplementary file 1).19
rmdopen-2019-001146s001.pdf (554.7KB, pdf)
RESULTS
Within the group of patients eligible for this study (n=333), 140 (42%) could be categorised as early and persistent clinical responders. Among these 140 patients, Two-Step cluster analysis yielded three clusters of patients as the optimal cluster solution when looking at pain, fatigue, physical functioning, quality of life and sleep quality as clustering variables for well-being at year 1. Regarding these five PROs used to cluster patients, the proportion of missingness that was imputed at year 1 was 2.1% for pain, 2.9% for fatigue, 2.1% for physical functioning, 15.7% for RA quality of life and 21.4% for sleep quality. Cluster membership remained stable between imputed and not imputed datasets and between k-means clustering and hierarchical median clustering (Supplementary file 2).
rmdopen-2019-001146s002.pdf (531.8KB, pdf)
The largest cluster (n=109) comprised patients with a low level of pain and fatigue, a good physical functioning and RA-related quality of life and a relatively good sleep quality (table 1). Since the PROs of these patients are in line with the clinical disease activity characteristics, we labelled this cluster the ‘concordant to disease activity’ cluster. Around 20% of the patients (n=31) were allocated to one of two ‘discordant’ clusters with diverging scores, mainly because of their pain and fatigue reporting. The first discordant cluster, comprising 13 patients, was labelled the ‘dominant fatigue’ cluster as these patients mainly reported a high fatigue level at year 1. The second discordant cluster, including 18 patients, was called the ‘dominant pain and fatigue’ cluster, because these patients reported both pain and fatigue at considerable levels at year 1. Compared with the ‘concordant to disease activity’ cluster, patients assigned to the ‘dominant fatigue’ and the ‘dominant pain and fatigue’ clusters reported a more functional loss and a worse RA-related quality of life. Sleep quality seemed less of a discriminating variable for cluster allocation. Table 1 presents the average scores at year 1 of the five PROs used to assign patients to a cluster. Baseline patient characteristics and PROs of the three clusters are shown in table 2.
Table 1.
Average scores of the five patient-reported outcomes after 1 year of RA treatment used to assign patients with an early and persistent treatment response to a cluster (n=140)
| Clusters | |||
|---|---|---|---|
| PRO scores at year 1 | Concordant to disease activity n=109 (77.9%) | Dominant fatigue n=13 (9.3%) | Dominant pain and fatigue n=18 (12.9%) |
| Pain (0–100) | |||
| mean±SD | 7.3±7.5 | 14.5±8.9 | 45.1±14.6 |
| median (Q1–Q3) | 5 (2–3) | 15 (10–20) | 51 (48–68) |
| Fatigue (0–100) | |||
| mean±SD | 10.0±9.9 | 69.6±14.3 | 42.4±14.0 |
| median (Q1–Q3) | 10 (2–20) | 70 (60–80) | 51 (45–60) |
| Physical functioning (0–3) | |||
| mean±SD | 0.1±0.1 | 0.2±0.3 | 0.3±0.3 |
| median (Q1–Q3) | 0 (0–0.1) | 0.1 (0–0.4) | 0.1 (0–0.5) |
| RA-related quality of life (0–30) | |||
| mean±SD | 3.9±4.9 | 6.2±2.4 | 5.6±5.0 |
| median (Q1–Q3) | 2.9 (1–5) | 7 (4–8) | 3 (2.2–8.1) |
| Sleep quality (0–21) | |||
| mean±SD | 5.0±3.0 | 6.0±1.9 | 5.4±2.6 |
| median (Q1–Q3) | 4 (3–6) | 6 (5–7) | 5 (4–6) |
Higher scores indicate worse pain, worse fatigue, more functional loss, worse health-related quality of life and worse sleep quality. Early and persistent response was defined as a DAS28CRP<2.6 at week 16, sustained between week 16 and week 52. PRO, patient-reported outcome; Q1, quartile 1 (25th percentile); Q3, quartile 3 (75th percentile); RA, rheumatoid arthritis.
Table 2.
Baseline patient characteristics and patient-reported outcomes organised for each cluster
| Baseline variables | Concordant to disease activity cluster (n=109) | Dominant fatigue cluster (n=13) | Dominant pain and fatigue cluster (n=18) |
|---|---|---|---|
| Women, n(%) | 76 (69.7) | 9 (69.2) | 10 (55.6) |
| Age (years) | |||
| mean±SD | 52.5±13.3 | 52.2±11.4 | 54.2±15.4 |
| median (Q1–Q3) | 54 (44–62) | 55 (51–60) | 47 (44–64) |
| DAS28CRP (0–9.4) | |||
| mean±SD | 4.5±1.2 | 4.3±1.0 | 4.5±0.9 |
| median (Q1–Q3) | 4.41 (3.7–5.4) | 4.10 (3.8–4.7) | 4.6 (3.7–5.0) |
| Pain (0–100) | |||
| mean±SD | 50.8±25.2 | 53.7±17.6 | 53.4±19.2 |
| median (Q1–Q3) | 50 (30–70) | 53 (46–60) | 60 (37–68) |
| Fatigue (0–100) | |||
| mean±SD | 40.4±24.6† | 53.6±23.8 | 49.9±16.1 |
| median (Q1–Q3) | 42 (20–57) | 52 (46–60) | 51 (41–75) |
| Physical functioning (0–3) | |||
| mean±SD | 0.9±0.7 | 0.7±0.4 | 0.8±0.6 |
| median (Q1–Q3) | 0.8 (0.4–1.3) | 0.6 (0.5–0.8) | 0.6 (0.4–0.9) |
| RA quality of life (0–30) | |||
| mean±SD | 9.1±6.8† | 8.0±4.5 | 10.6±7.7 |
| median (Q1–Q3) | 8 (4–13) | 9 (5–14) | 7 (5–10.3) |
| Sleep quality (0–21) | |||
| mean±SD | 7.9±4.3† | 8.3±3.5† | 8.2±3.6 |
| median (Q1–Q3) | 7 (5–11) | 7 (5–8) | 9 (5–11) |
| Symptom duration (weeks) | |||
| mean±SD | 30.3±30.4 | 29.4±37.7 | 34.7±27.1 |
| median (Q1–Q3) | 22 (13–36) | 38 (26–52) | 14 (13–19) |
| Comorbidities (present), n(%) | 72 (66.1) | 10 (76.9) | 16 (88.9) |
| IPQ-R treatment control* (5–25) | |||
| mean±SD | 19.1±2.2 | 17.9±2.1 | 18.5±2.2 |
| median (Q1-Q3) | 19 (18–21) | 18 (18–19) | 18 (18–19) |
*Patients’ belief in the effectiveness of treatment to control RA at treatment initiation.
†Missingness for patient-reported outcomes: 0.9% (pain; fatigue), 4.6% (RA quality of life), 7.7% (sleep quality, ‘dominant fatigue’ cluster), 10.1% (sleep quality, ‘concordant’ cluster).
comorbidities, number of patients having at least one comorbidity at trial screening; DAS28CRP, 28-joint disease activity score using C-reactive protein level; IPQ-R, Revised Illness Perception Questionnaire; Q1, quartile 1 (25th percentile); Q3, quartile 3 (75th percentile); RA, rheumatoid arthritis
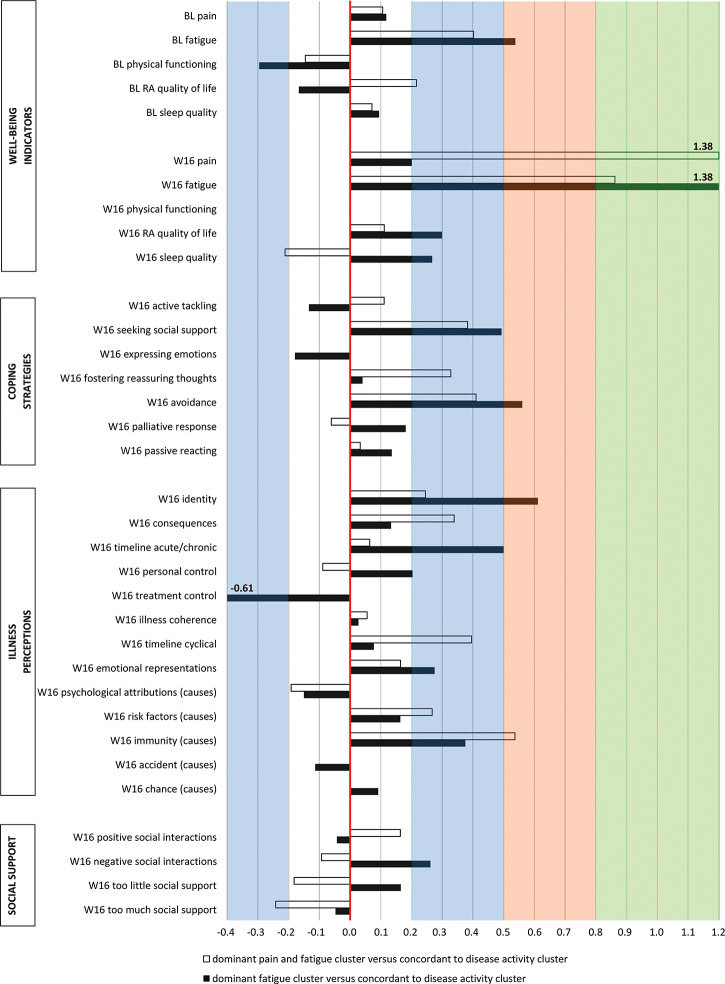
The differences in self-reporting between patients in the ‘discordant’ clusters and those in the ‘concordant to disease activity’ cluster are depicted in figure 1: small (blue shading), medium (orange shading) and large (green shading) effect sizes (ESs) were found for PROs at baseline and week 16. First, the differences in reporting with patients in the ‘concordant’ cluster were small; however, patients in the ‘dominant fatigue’ cluster reported at week 16 more pain (ES=0.20), worse RA quality of life (ES=0.30), worse sleep quality (ES=0.27), more social support seeking (ES=0.49), more personal control (ES=0.20), more negative emotions about the disease (ES=0.28) and more negative social interactions (ES=0.26). Furthermore, their physical functioning was slightly better at baseline (ES=−0.30). A moderately higher fatigue at baseline (ES=0.54), more avoidant coping at week 16 (ES=0.56), a stronger belief that the symptoms are part of RA at week 16 (ES=0.61), a higher belief in chronicity of RA at week 16 (ES=0.50) and a lower belief in the effectiveness of treatment to control RA at week 16 (ES=−0.61) were observed in the ‘dominant fatigue’ cluster. A large difference in effect size was found for fatigue at week 16 (ES=1.38), with more fatigue reported by patients in the ‘dominant fatigue’ cluster compared with patients in the ‘concordant’ cluster.
Figure 1.
Effect sizes of patient-reported outcomes at baseline and week 16 when comparing the ‘dominant pain and fatigue’ cluster with the ‘concordant to disease activity’ cluster and the ‘dominant fatigue cluster’ cluster with the ‘concordant to disease activity’ cluster. The red line represents no effect: patients in the ‘discordant’ clusters gave the same score as patients in the ‘concordant to disease activity’ cluster. The area on the left of this line represents the negative ESs: patients in the ‘discordant’ clusters reported a lower score. The area on the right represents the positive ES: patients in the ‘discordant’ clusters reported a higher score. White area: no meaningful effect (Cohen’s d 0–0.2); blue area: small effects (Cohen’s d 0.2–0.5), orange area: medium effects (Cohen’s d 0.5–0.8), green area: large effects (Cohen’s d≥0.8). BL: Baseline; W16: week 16 of treatment.
Second, when comparing the ‘dominant pain and fatigue’ cluster with the ‘concordant to disease activity’ cluster, a slightly higher level of fatigue at baseline (ES=0.40), worse RA quality of life at baseline (ES=0.22), better sleep quality at week 16 (ES=−0.21), more social support seeking at week 16 (ES=0.38), more fostering of reassuring thoughts at week 16 (ES=0.33), more avoidant coping at week 16 (ES=0.41), a stronger belief that the symptoms are part of RA at week 16 (ES=0.25), more negative beliefs about the consequences of RA at week 16 (ES=0.34), a higher belief in a variable nature of the disease at week 16 (ES=0.40), a stronger belief in risk factors as disease cause at week 16 (ES=0.27) and less perceived excessive social support at week 16 (ES=−0.24) were seen. A moderate difference in reporting between clusters was found for patients’ belief in immunity as disease cause, with a stronger belief reported by patients in the ‘dominant pain and fatigue’ cluster at week 16 (ES=0.54). Large differences between clusters were found for pain and fatigue reporting at week 16, with higher pain (ES=1.38) and fatigue (ES=0.86) scores in the ‘dominant pain and fatigue cluster’ compared with the ‘concordant’ cluster.
The mean scores ±SD of PROs at week 16 are presented in Supplementary file 3.
rmdopen-2019-001146s003.pdf (518.3KB, pdf)
DISCUSSION
We identified three distinct clusters in patients with early RA, who had a rapid and sustained first treatment response. Patients in the largest cluster reported PROs in concordance with the disease activity trajectory after 1 year of treatment. However, one in five patients continued to report signs of poor well-being, despite having enjoyed a favourable treatment response. One cluster showed excessive fatigue, and the other cluster had increased levels of both pain and fatigue. Patients of those two ‘discordant’ clusters reported higher pain and fatigue levels already early in the disease course. Apart from that, patients with a ‘discordant’ PRO profile after 1 year also seem to have different illness perceptions and coping strategies early in the disease course.
Patients reporting not feeling well were all affected by fatigue in our study. Fatigue has already been proposed as an important outcome for patients with RA.20 However, it appears to be a challenging symptom to manage because of its multidimensionality.21 Basu et al found distinct fatigue subtypes among patients with RA reporting severe fatigue, demonstrating the complex nature of this symptom.22 As patients with RA experience different types of fatigue, and the optimal intervention targets are still to be established,23 further research is needed to explore how fatigue evaluation and management could correspond better to patients’ experience of fatigue. Besides fatigue reporting in our study, also pain was reported at a relatively high level despite control of disease activity, in accordance with the current literature summarised by Taylor et al.4 A clinically relevant message of our study is to take patients reporting remaining pain and fatigue seriously already in the early stage of RA, as the results indicate that this can be associated with how patients perceive their RA later on. The perspective of these patients should be further explored using qualitative research methodology to get more insight into this symptom reporting and to identify clues for specific interventions that could prevent the occurrence of secondary fibromyalgia or depression in this patient group.
Patients who are feeling unwell despite good disease control should be identified earlier, to prevent both escalation of perceived disease impact as well as increased medical costs due to overtreatment of non-inflammatory symptoms by immunosuppressive drugs.24 Our results suggest that this early detection might already be achievable in the first 4 months of treatment. Patients` illness perceptions and coping style at week 16, including an avoidant coping strategy and a stronger belief that the experienced symptoms were part of RA, were more prominent in the ‘discordant’ clusters compared with the ‘concordant’ cluster at these early time points. Additionally, the IPQ-R subscale ‘timeline cyclical’ was scored higher by these patients, indicating that they experienced the disease as more fluctuating, which can result in more uncertainty. Attention to such patient factors early in the disease could be a missing link to further optimize the clinical course both short and long term of newly diagnosed patients with RA.25
Inadequate illness representations could be countered by investing in timely education and by reserving time to increase patients’ illness awareness throughout the first months after diagnosis, which is the task of healthcare professionals of different disciplines (eg, physicians, physiotherapists, occupational therapists, psychologists). Nurses could play a specific role in this field as patient education and health promotion are core aspects of their role in disease management.26 Moreover, a recent systematic review in RA showed that psychological interventions can also have a significant effect on coping and self-management behaviours.27 Dures et al found that patients perceive psychological support from rheumatology clinicians and general practitioners as a positive option.28 Hence, it should be investigated whether non-psychologically trained health professionals could deliver such interventions.27 It has been demonstrated that rheumatology clinicians were able to learn and implement interventions such as cognitive behavioural techniques.29 Another option to influence patients` behaviour could be peer mentorship,30 although in general most non-pharmacological interventions to support patients with RA need further study.
Some methodological considerations need to be addressed. First, a disadvantage of k-means clustering is that data should be normally distributed, and that data only contains numerical data. However, sensitivity analyses using hierarchical median clustering showed similar results as the k-means clustering which underlines the robustness of our analysis. However, we utilised HAQ and VAS as numerical variables, but research has shown that caution should be taken using these variables in such a way.31 Second, the number of clusters depended entirely on the variables in the analysis. However, we selected five PROs that reflect typical aspects being communicated by patients during a routine consultation as a reflection of their well-being, including pain, fatigue, sleep and functional problems. Patients’ health-related quality of life was added to further strengthen the face validity of the cluster analysis. As the selected instruments are frequently used in daily practice, our findings could also stimulate the integration of cluster definitions into practice. Third, PRO scores were clustered after 1 year of treatment, while another time point could have resulted in other cluster solutions. However, according to our patient researcher, newly diagnosed patients need time to ‘recover’ and find a new balance, and therefore, improvement in PROs could be delayed. The year 1 time point in the CareRA trial should reflect a more stable disease stage, with most clinically well-controlled patients on methotrexate monotherapy and already off glucocorticoids for 4 months. We also assumed that patients who report signs of poor well-being after 1 year despite a well-controlled disease from 4 months onwards are at risk of feeling persistently unwell. Therefore, we chose year 1 as our endpoint. Fourth, we considered the calculation of ESs more appropriate than p values because of the rather small sample size with risk of multiple testing in this explorative study. However, we acknowledge that our findings need validation in a larger patient population with early RA. Still, the clusters showed a high face validity. Finally, we cannot exclude that there might also have been participants who did not feel well but did not report this as such. Hence, patient questionnaires are a very useful tool, but cannot replace direct communication and interaction with patients. A major strength of this study is that patients were part of a pragmatic clinical trial with a standardised collection of both PROs and disease markers. Another strength is that in this study on the patient perspective, a patient researcher was involved in each research phase: setting up the research question, selection of measurements and evaluation points, interpretation of the cluster solution and differences between clusters, discussion of the results and manuscript writing.
In conclusion, this study identified three clusters of well-being in patients with early RA who enjoyed a rapid and persistent initial treatment response, based on five clinically relevant PROs reported after 1 year of treatment. Although most patients reported very low pain and fatigue levels in concordance with their well-controlled disease activity, one in five persistent responders displayed additional, non-pharmacological needs already in the early disease stage. Patients prone to persistently feeling unwell reported higher pain and fatigue levels already early in the disease course. Evaluated coping and illness perceptions provide opportunities for early intervention with appropriate education and counselling.
Acknowledgments
We are very grateful to all patients, who were willing to complete the questionnaires during a crucial period of their disease. Furthermore, we would like to thank the local rheumatology staff for data collection and the CareRA team for data monitoring.
Footnotes
Contributors: KE, RW, PV, PM, DC and AG made substantial contributions to the conception or design of the study. DC performed statistical analysis in collaboration with KE. All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be submitted for publication.
Funding: The CareRA trial (EudraCT number: 2008-007225-39) was funded by a Flemish governmental grant (Agency for Innovation by Science and Technology [IWT]). Patrick Verschueren holds the Pfizer chair for early rheumatoid arthritis management at the KU Leuven.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: The ethics committee of the University Hospitals Leuven.
Data sharing statement: All data relevant to the study are included in the article or uploaded as supplementary information.
Provenance and peer review: Not commissioned; externally peer reviewed.
REFERENCES
- 1.Smolen JS, Aletaha D, Barton A, et al. Rheumatoid arthritis. Nat Rev Dis Primers 2018;4:18001 10.1038/nrdp.2018.1. [DOI] [PubMed] [Google Scholar]
- 2.Lee YC, Frits ML, Iannaccone CK, et al. Subgrouping of patients with rheumatoid arthritis based on pain, fatigue, inflammation, and psychosocial factors. Arthritis Rheumatol 2014;66:2006–14 10.1002/art.v66.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Druce KL, Bhattacharya Y, Jones GT, et al. Most patients who reach disease remission following anti-TNF therapy continue to report fatigue: results from the British Society for Rheumatology Biologics Register for Rheumatoid Arthritis. Rheumatology (Oxford) 2016;55:1786–90 10.1093/rheumatology/kew241. [DOI] [PubMed] [Google Scholar]
- 4.Taylor PC, Moore A, Vasilescu R, et al. A structured literature review of the burden of illness and unmet needs in patients with rheumatoid arthritis: a current perspective. Rheumatol Int 2016;36:685–95 10.1007/s00296-015-3415-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Steunebrink LMM, Oude Voshaar MAH, Taal E, et al. Determinants of perceived health nonimprovement in early rheumatoid arthritis patients with favorable treatment outcomes. Arthritis Care Res 2018;70:510–15 10.1002/acr.23305. [DOI] [PubMed] [Google Scholar]
- 6.Petrie KJ, Jago LA, Devcich DA. The role of illness perceptions in patients with medical conditions. Curr Opin Psychiatry 2007;20:163–7 10.1097/YCO.0b013e328014a871. [DOI] [PubMed] [Google Scholar]
- 7.Groarke A, Curtis R, Coughlan R, et al. The role of perceived and actual disease status in adjustment to rheumatoid arthritis. Rheumatology (Oxford) 2004;43:1142–9 10.1093/rheumatology/keh262. [DOI] [PubMed] [Google Scholar]
- 8.Ferreira RJO, Duarte C, Ndosi M, et al. Suppressing inflammation in rheumatoid arthritis: does patient global assessment blur the target? A practice-based call for a paradigm change. Arthritis Care Res 2018;70:369–78 10.1002/acr.v70.3. [DOI] [PubMed] [Google Scholar]
- 9.Stouten V, Westhovens R, Pazmino S, et al. Effectiveness of different combinations of DMARDs and glucocorticoid bridging in early rheumatoid arthritis: two-year results of CareRA. Rheumatology (Oxford) 2019;58:2284–94 10.1093/rheumatology/kez213. [DOI] [PubMed] [Google Scholar]
- 10.Bruce B, Fries JF. The Stanford health assessment questionnaire: dimensions and practical applications. Health Qual Life Outcomes 2003;1:20. 10.1186/1477-7525-1-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.de Jong Z, van der Heijde D, McKenna SP, et al. The reliability and construct validity of the RAQoL: a rheumatoid arthritis-specific quality of life instrument. Br J Rheumatol 1997;36:878–83 10.1093/rheumatology/36.8.878. [DOI] [PubMed] [Google Scholar]
- 12.Buysse DJ, Reynolds CF 3rd, Monk TH, et al. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193–213 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 13.Schreurs P, Tellegen B, Vanderwillige G. Health, stress and coping - the development of the utrechtse coping scale. Gedrag-Tijdschr Voor Psychol 1984;12:101–17. [Google Scholar]
- 14.Moss-Morris RWJ, Petrie KJ, Horne R, et al. The revised illness perception questionnaire (IPQ-R). Psychol Health 2002;17:1–16 10.1080/08870440290001494. [DOI] [Google Scholar]
- 15.Hill S. The illness perceptions questionnaire-revised (IPQ-R). J Physiother 2010;56:280. 10.1016/S1836-9553(10)70062-X. [DOI] [PubMed] [Google Scholar]
- 16.Van Sonderen E. Het meten van sociale steun met de Sociale Steun Lijst-Interacties (SLL-I) en Sociale Steun Lijst: Discrepanties (SSL-D): een handleiding. Groningen: Noordelijk Centrum voor Gezondheidsvraagstukken, Rijksuniversiteit Groningen, 1993. [Google Scholar]
- 17.Cohen J. Statistical power analysis for the behavioral sciences. 2nd edn. Mahwah, New Jersey, United States of America: Lawrence Erlbaum Associates,1988. [Google Scholar]
- 18.Dempster APLN, Rubin DB. Maximum likelihood from incomplete data via the EM algorithm. J R Stat Soc 1977;39:1–38. [Google Scholar]
- 19.von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 2008;61:344–9 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 20.Kirwan JR, Minnock P, Adebajo A, et al. Patient perspective: fatigue as a recommended patient centered outcome measure in rheumatoid arthritis. J Rheumatol 2007;34:1174–7. [PubMed] [Google Scholar]
- 21.Lampa J. Fatigue: the heavy backpack of many rheumatoid arthritis patients. Rheumatology (Oxford) 2015;54:962–3 10.1093/rheumatology/kev020. [DOI] [PubMed] [Google Scholar]
- 22.Basu N, Jones GT, Macfarlane GJ, et al. Identification and validation of clinically relevant clusters of severe fatigue in rheumatoid arthritis. Psychosom Med 2017;79:1051–8 10.1097/PSY.0000000000000498. [DOI] [PubMed] [Google Scholar]
- 23.Cramp F, Hewlett S, Almeida C, et al. Non-pharmacological interventions for fatigue in rheumatoid arthritis. Cochrane Database Syst Rev 2013;Aug 23; (8):CD008322. [DOI] [PubMed] [Google Scholar]
- 24.Landewe RBM. Overdiagnosis and overtreatment in rheumatology: a little caution is in order. Ann Rheum Dis 2018;77:1394–6. [DOI] [PubMed] [Google Scholar]
- 25.Evers AW, Kraaimaat FW, Geenen R, et al. Pain coping and social support as predictors of long-term functional disability and pain in early rheumatoid arthritis. Behav Res Ther 2003;41:1295–310 10.1016/S0005-7967(03)00036-6. [DOI] [PubMed] [Google Scholar]
- 26.van Eijk-hustings Y, van Tubergen A, Bostrom C, et al. EULAR recommendations for the role of the nurse in the management of chronic inflammatory arthritis. Ann Rheum Dis 2012;71:13–19 10.1136/annrheumdis-2011-200185. [DOI] [PubMed] [Google Scholar]
- 27.Prothero L, Barley E, Galloway J, et al. The evidence base for psychological interventions for rheumatoid arthritis: a systematic review of reviews. Int J Nurs Stud 2018;82:20–9 10.1016/j.ijnurstu.2018.03.008. [DOI] [PubMed] [Google Scholar]
- 28.Dures E, Almeida C, Caesley J, et al. Patient preferences for psychological support in inflammatory arthritis: a multicentre survey. Ann Rheum Dis 2016;75:142–7 10.1136/annrheumdis-2014-205636. [DOI] [PubMed] [Google Scholar]
- 29.Dures E, Hewlett S, Ambler N, et al. Rheumatology clinicians’ experiences of brief training and implementation of skills to support patient self-management. BMC Musculoskelet Disord 2014;15:108 10.1186/1471-2474-15-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sandhu S, Veinot P, Embuldeniya G, et al. Peer-to-peer mentoring for individuals with early inflammatory arthritis: feasibility pilot. BMJ Open 2013;3:3 10.1136/bmjopen-2012-002267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kersten P, Kucukdeveci AA, Tennant A. The use of the visual analogue scale (VAS) in rehabilitation outcomes. J Rehabil Med 2012;44:609–10 10.2340/16501977-0999. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
rmdopen-2019-001146s001.pdf (554.7KB, pdf)
rmdopen-2019-001146s002.pdf (531.8KB, pdf)
rmdopen-2019-001146s003.pdf (518.3KB, pdf)