INTRODUCTION
The COVID-19 pandemic crisis has had a staggering impact worldwide. Confirmed cases have increased exponentially and the number of infected individuals has since exceeded a million [1]. It is however important to realize that with limitations in testing, true infection rates may in fact be much higher [2]. In addition, presymptomatic transmission of infected individuals has been documented in China and lately confirmed in Singapore [3-5]. Our local data suggests that this can occur in 6.4% of patients but has been reported to be as high as 30% in other studies [6,7].
Safe surgery has emerged as a topic of immense interest. As colorectal surgery accounts for a significant proportion of General Surgery workload [8], the COVID-19 pandemic thus has immense implications for many general and colorectal surgeons. In this current juncture of the pandemic with dangers of viral transmission, surgeons need to achieve a balance between surgical safety and judicious consumption of personal protective equipment (PPE). While deferment of nonurgent cases may be an initial strategy, this approach is impractical in the long run. The COVID-19 pandemic will likely have a protracted course and the resultant backlog of cases from indiscriminate deferment may overwhelm surgical capacity in the near future and compromise clinical care [9]. This is particular pertinent for common and time-sensitive pathologies like colorectal cancer.
In Singapore, COVID-19 management has been one of prompt contact tracing and isolation to prevent transmission. Curtailment of travel as well as safe distancing measures at work and social areas have all been imposed. Nonetheless, there have been a large number of imported cases with resultant community spread. In the authors’ hospital, there have been 290 (latest figures as of 23/4/20) positive COVIDs to date.
While there has been a gradual reduction of elective workload over the last 2 months since the onset of the disease outbreak in Singapore, there continues to be a reasonable volume of cases performed. In this article, we share our colorectal unit’s workflow (Fig. 1) and recommendations (Table 1) for safe practice in the COVID-19 era.
Fig. 1.
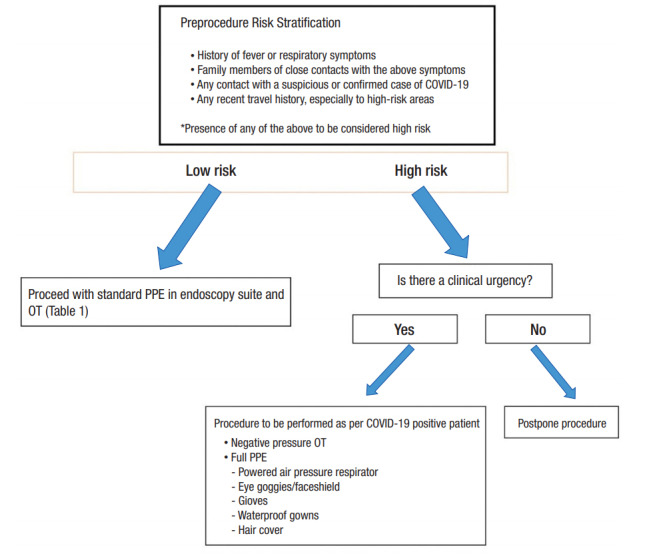
Proposed workflow for patients undergoing Endoscopy or Surgery in the COVID-19 era. PPE, personal protective equipment; OT, operating theater.
Table 1.
Proposed personal protective equipment (PPE) and safety measures for colorectal procedures
| Procedure | PPE recommendations | Other safety measures |
|---|---|---|
| Endoscopy procedures | Face shields/eye goggles | Minimize use of energy during procedures |
| N95 respirator masks | Avoid procedures like EMR/ESD which may require additional insufflation | |
| Gloves | ||
| Waterproof gown | ||
| Open colorectal resections | Face shields/eye goggles | Electrocautery set to the lowest possible settings |
| Hair cover | Minimize use of ultrasonic dissectors or advanced bipolar devices | |
| N95 respirator mask | Diathermy pencils with attached smoke evacuators encouraged | |
| Gloves | ||
| Waterproof gown | ||
| Laparoscopic colorectal resections | Face shields/eye goggles | Minimize port incisions to prevent leakage |
| Hair cover | Consider use of smoke evacuation system | |
| N95 respirator mask | Pneumoperitoneum to be safely evacuated using filtration system or suction device prior to specimen extraction or port removal | |
| Gloves | ||
| Waterproof gown |
EMR, endoscopic mucosal resection; ESD, endoscopic submucosal dissection.
Workflow for patients undergoing elective colorectal procedures in the COVID-19 era:
Our workflow for evaluating patients scheduled for procedures (Endoscopy or Surgery) is illustrated in Fig. 1. Preprocedure risk stratification is done for all patients at 3 stages. At the initial anesthetist assessment 1–2 weeks preoperatively a chest X-ray or computed tomography thorax for cancer cases will be obtained to assess for consolidative changes in the lungs. Three days prior to the surgery date, our admission team will contact the patient to obtain a travel declaration and to inquire if there are new flu-like symptoms. On day of admission, this process is repeated with a formal declaration form signed by the patient.
Patients who have any travel history within 14 days, or has contact with any member of the public who is positive for COVID-19 or on home quarantine, or has new onset of flu-like symptoms will be advised on postponement of procedure. The procedure would be postponed by 2 to 4 weeks to allow infected patients who may be within the incubation period of COIVD-19 to declare themselves.
If there is clinical urgency, the procedure may proceed with precautions taken as per a presumed COVID-19 positive patient (Fig. 1). Clinical urgency refers to cases which necessitate intervention within 2 weeks. These include colorectal cancer cases with impending obstruction or with overt bleeding resulting in significant transfusion requirements. Postoperatively, such patients will undergo COVID-19 testing and will be nursed in isolation until their test results clear them from COVID-19 infection.
At the current moment, universal COVID-19 testing for all patients undergoing surgery is not performed. We only perform testing for patients who meet the suspect case definition stipulated by the Ministry of Health, Singapore. As of 16 April 2020, the case definition is as follows:
(1) A person with clinical signs and symptoms suggestive of Community-Acquired Pneumonia or community-acquired severe respiratory infection with breathlessness.
(2) A person with an acute respiratory illness of any degree of severity (e.g., symptoms of cough, sore throat, runny nose, anosmia), with or without fever, who, within 14 days before onset of illness had: (a) Travelled abroad (outside Singapore); (b) Close contact with a case of COVID-19 infection.
PROCEDURAL CONSIDERATIONS
Endoscopy
Endoscopy carries an increased risk of COVID-19 infection from droplets inhalation, conjunctival contact and fomite contamination. Upper gastrointestinal (GI) endoscopy is recognized to be a high risk aerosol-generating procedure (AGP) [10]. However, it is important to highlight that colonoscopy may also pose significant risks. The 2019-nCoV has been consistently isolated in stool samples and fecal oral transmission is recognized [11-13]. It remains unknown if gas insufflation during colonoscopy may be considered an AGP. In our unit, we adopt the same PPE measures for colonoscopy as for a gastroduodenoscopy. A summary of our PPE recommendations for endoscopy is summarized in Table 1.
Colorectal surgery
Minimally invasive surgery
There is scant evidence regarding the risks of virus transmission of minimally invasive surgery (MIS) or open surgery. However, data does indicate that laparoscopy can lead to aerosolization of blood borne viruses, although it remains unknown if this applies to COVID-19 [14, 15].
As such, while we still perform MIS procedures, surgeons are recommended to adopt the necessary PPE precautions. (Table 1) Filtration systems applied to trocars for smoke evacuation and safe evacuation of pneumoperitoneum may be considered but the efficacy of such measures remains unknown.
The risks of transanal MIS procedures (taTME - transanal total mesorectal excision, TAMIS-transanal minimally invasive surgery) remains unknown in the COVID-19 era. However, the 2019-nCoV has been demonstrated in stool samples, and with the strong potential risks while evacuating air per-anally, these procedures should be performed with extreme caution in the current climate [11-13,16].
Open surgery
Smoke from electrocautery during open surgery can harbor virus particles [17]. Unlike MIS, the exposure of the surgeon to smoke inhalation is likely higher in open surgery which raises the possibility of COVID-19 transmission. Measures to mitigate risks of transmission should thus be adopted. These, together with our proposed PPE for open surgery, are summarized in Table 1.
Operating room management during surgery
Most operating room (ORs) have an average of 15–40 air exchanges per hour. To ensure clean air in the OR, 14–18 minutes is thus required [18]. In our institution, an intubation-extubation protocol has been in practice since the COVID-19 outbreak. In this protocol, a 5-minute pause has been mandated during intubation and extubation, with only the anesthetists and assistant in OR wearing full PPE. This ensures at least 2 gas exchanges of the OR, and enhances safety in the scenario that surgeons are operating on an undiagnosed COVID-19 case. To address the concerns of laparoscopy, an additional 15 minutes has been factored in, which commences on evacuation of the pneumoperitoneum. This allows a complete 20 minutes of air exchange on completion of surgery and extubation [19].
For COVID-19 cases, surgery is performed in a dedicated negative pressure OR. In the negative pressure OR, the induction and scrub room is maintained at a pressure of -2.5 Pascals relative to the exterior to prevent dissemination of aerosolized virus particles. Fig. 2 illustrates the setup of our negative pressure OR.
Fig. 2.
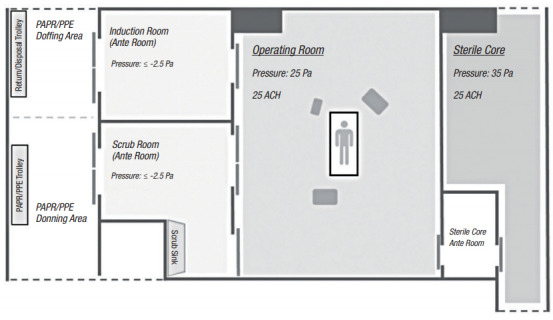
Negative pressure OR setup. PAPR, positive air pressure respiratory; PPE, personal protective equipment; ACH, air exchanges per hour.
The COVID-19 pandemic is likely to run a protracted course and has immense implications on colorectal practice. Various academic societies have provided guidance for clinical practice and these are summarized in Table 2 [10, 20-23]. While the measures we have in place have allowed safe colorectal surgery, there are several modifications that may have to be considered in view of increasing community transmission and recognition of presymptomatic transmission. One suggestion is that routine bowel preparation may be considered to reduce fecal load during bowel surgery. Secondly, the appropriate PPE in this era needs to be reviewed and perhaps all OR staff should be in N95 respirators for all colorectal procedures until there is more evidence regarding transmission risk during surgery. The difficulty, however, is having the availability of resources and its pragmatic allocation. Thirdly, universal preoperative COVID-19 testing may seem to be intuitively better and replace clinical stratification but the issues of false negatives and limited COVID-19 testing capacity may hamper widespread implementation. We urge the colorectal fraternity to share their workflows and protocols to ensure safe practice among our community amidst this uncertain era.
Table 2.
Recommendations of various professional societies on procedures during the COVID-19 pandemic
| Recommendations regarding Surgical Response to COVID-19 | SAGES and EAES (29 Mar 2020) | Gastroenterology Professional Society Guidance (ASGE, AGA, ACG, AASLD) (31 Mar 2020) | European Society of Gastrointestinal Endoscopy (18 Mar 2020) | Intercollegiate General Surgery Guidance (27 Mar 2020) | American College of Surgeons (24 Mar 2020) |
|---|---|---|---|---|---|
| Endoscopy | All elective cases to be postponed | All elective procedures to be delayed | Strongly consider postponing elective, nonurgent procedures | Only emergency procedures to be performed | NA |
| Patients with time-sensitive diagnosis to proceed with evaluation | No diagnostic work to be done | ||||
| Surgery | All elective cases to be postponed | NA | Largely confined to emergency surgery | Tiered approach for cancer cases | |
| Surgical care limited to those whose needs are imminently life threatening | Stoma formation to be considered rather than anastomosis |
SAGES, society of american gastrointestinal and endoscopic surgeons; EAES, european association of endoscopic surgery; ASGE, american society for gastrointestinal endoscopy; AGA, american gastroenterological association; ACG, american college of gastroenterology; AASLD, american association for the study of liver diseases; NA, not applicable.
REFERENCES
- 1.Baltimore (MD): Johns Hopkins University & Medicine; c2020. John Hopkins Coronavirus Resource Centre [Internet] [cited 2020 Apr 8]. Available from: https://coronavirus.jhu.edu/map.html. [Google Scholar]
- 2.Li R, Pei S, Chen B, Song Y, Zhang T, Yang W, et al. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2) Science. 2020 Mar 16; doi: 10.1126/science.abb3221. [Epub]. pii: eabb3221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Qian G, Yang N, Ma AHY, Wang L, Li G, Chen X, et al. A COVID-19 Transmission within a family cluster by presymptomatic infectors in China. Clin Infect Dis. 2020 Mar 23; doi: 10.1093/cid/ciaa316. [Epub]. pii: ciaa316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tong ZD, Tang A, Li KF, Li P, Wang HL, Yi JP, et al. Potential Presymptomatic Transmission of SARS-CoV-2, Zhejiang Province, China, 2020. Emerg Infect Dis. 2020;26:1052–4. doi: 10.3201/eid2605.200198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wei WE, Li Z, Chiew CJ, Yong SE, Toh MP, Lee VJ. Presymptomatic transmission of SARS-CoV-2 - Singapore, January 23-March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:411–5. doi: 10.15585/mmwr.mm6914e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kimball A, Hatfield KM, Arons M, James A, Taylor J, Spicer K, et al. Asymptomatic and Presymptomatic SARS-CoV-2 Infections in Residents of a Long-Term Care Skilled Nursing Facility - King County, Washington, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69:377–81. doi: 10.15585/mmwr.mm6913e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nishiura H, Kobayashi T, Suzuki A, Jung SM, Hayashi K, Kinoshita R, et al. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19) Int J Infect Dis. 2020 Mar 13; doi: 10.1016/j.ijid.2020.03.020. [Epub]. pii: S1201-9712(20)30139-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goligher J. Colorectal surgery as a specialty. J R Soc Med. 1996;89:601–3. doi: 10.1177/014107689608901101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lisi G, Campanelli M, Spoletini D, Carlini M. The possible impact of COVID-19 on colorectal surgery in Italy. Colorectal Dis. 2020 Mar 30; doi: 10.1111/codi.15054. [Epub]. [DOI] [PubMed] [Google Scholar]
- 10.Gralnek IM, Hassan C, Beilenhoff U, Antonelli G, Ebigbo A, Pellisè M, et al. ESGE and ESGENA Position Statement on gastrointestinal endoscopy and the COVID-19 pandemic. Endoscopy. 2020 Apr 17; doi: 10.1055/a-1155-6229. [Epub]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020 Feb 24; doi: 10.1001/jama.2020.2648. [Epub]. [DOI] [PubMed] [Google Scholar]
- 12.Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H. Evidence for Gastrointestinal Infection of SARS-CoV-2. Gastroenterology. 2020 Mar 3; doi: 10.1053/j.gastro.2020.02.055. [Epub]. pii: S0016-5085(20)30282-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yeo C, Kaushal S, Yeo D. Enteric involvement of coronaviruses: is faecal-oral transmission of SARS-CoV-2 possible? Lancet Gastroenterol Hepatol. 2020;5:335–7. doi: 10.1016/S2468-1253(20)30048-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alp E, Bijl D, Bleichrodt RP, Hansson B, Voss A. Surgical smoke and infection control. J Hosp Infect. 2006;62:1–5. doi: 10.1016/j.jhin.2005.01.014. [DOI] [PubMed] [Google Scholar]
- 15.Choi SH, Kwon TG, Chung SK, Kim TH. Surgical smoke may be a biohazard to surgeons performing laparoscopic surgery. Surg Endosc. 2014;28:2374–80. doi: 10.1007/s00464-014-3472-3. [DOI] [PubMed] [Google Scholar]
- 16.Gu J, Han B, Wang J. COVID-19: Gastrointestinal Manifestations and Potential Fecal-Oral Transmission. Gastroenterology. 2020 Mar 3; doi: 10.1053/j.gastro.2020.02.054. [Epub]. pii: S0016-5085(20)30281-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu Y, Song Y, Hu X, Yan L, Zhu X. Awareness of surgical smoke hazards and enhancement of surgical smoke prevention among the gynecologists. J Cancer. 2019;10:2788–99. doi: 10.7150/jca.31464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention . Atlanta (GA): Centers for Disease Control and Prevention; Infection Control. Guidelines & Guidance Library [Internet] [cited 2020 Apr 8]. Available from: https://www.cdc.gov/infectioncontrol/guidelines/index.html. [Google Scholar]
- 19.Chew MH, Koh FH, Ng KH. A call to arms: a perspective of safe general surgery in Singapore during the COVID-19 pandemic. Singapore Med J. 2020 Apr 3; doi: 10.11622/smedj.2020049. [Epub]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Los Angeles (CA): SAGES; SAGES and EAES Recommendations Regarding Surgical Response to Covid-19 Crisis [Internet] [cited 2020 Apr 8]. Available from: https://www.sages.org/recommendations-surgical-response-covid-19/ [Google Scholar]
- 21.Chicago (IL): American College of Surgeons; c1996-2020. COVID-19 Guidelines for Triage of Colorectal Cancer Patients [Internet] [cited 2020 Apr 8]. Available from: https://www.facs.org/covid-19/clinical-guidance/elective-case/colorectal-cancer. [Google Scholar]
- 22.Downers Grove (IL): American Society for Gastrointestinal Endoscopy; Gastroenterology Professional Society Guidance on endoscopic procedures during the COVID-19 pandemic [Internet] [cited 2020 Apr 8]. Available from: https://www.asge.org/home/advanced-education-training/covid-19-asge-updates-for-members/gastroenterology-professional-society-guidance-on-endoscopic-procedures-during-the-covid-19-pandemic. [Google Scholar]
- 23.Edinburgh (UK): The Royal College of Surgeons of Edinburgh; c2020. Intercollegiate General Surgery Guidance on COVID-19 update [Internet] [cited 2020 Apr 8]. Available from: https://www.rcsed.ac.uk/news-public-affairs/news/2020/march/intercollegiate-general-surgery-guidance-on-covid-19-update. [Google Scholar]


