Abstract
Objective:
Recent years have witnessed growing interest in the role of the social environment in the development and outcomes of schizophrenia. We investigated whether neighborhood characteristics are associated with two important prognostic factors in early-course psychosis, age at onset of psychosis (AOP) and duration of untreated psychosis (DUP).
Methods:
Data were collected from patients admitted to the hospital for first-episode schizophrenia-spectrum disorder. We collected data on perceived neighborhood disorder (NDS) during childhood/adolescence and extracted data on 13 neighborhood characteristics from the American Community Survey based upon individual addresses. Four neighborhood-level factors were derived from factor analysis. Multiple logistic regression analyses assessed the association between specific neighborhood characteristics and the two prognostic factors (earlier AOP and longer DUP) in early-course psychosis.
Results:
143 participants had valid addresses geo-coded. Neighborhood-level Residential Instability was associated with an earlier AOP (OR=1.760; p=0.022) even after controlling for known risk factors (OR=2.026; p=0.020) and also after controlling for individual-level residential instability (OR=1.917; p=0.037). The General Socioeconomic Status neighborhood factor (OR=1.119; p=0.019) and perceived neighborhood disorder (OR=1.075; p=0.005) were associated with a longer DUP. But only perceived neighborhood disorder (OR=1.215; p=0.062) remained significant, and General Socioeconomic Status was close to significance (OR=1.215; p=0.062), after controlling for individual-level predictors and socioeconomic status.
Conclusions:
This study found evidence that neighborhood-level characteristics (in this case, residential instability) may be associated with earlier AOP, and perceptions of neighborhood disorder is associated with a longer treatment delay. Socioenvironmental factors should be more consistently considered going forward in research on early psychotic disorders.
Keywords: Age at onset, Census tract, Duration of untreated psychosis, Neighborhood, Psychosis, Schizophrenia
1. Introduction
Neighborhood characteristics are known to be important social determinants of health, influencing a wide range of outcomes related to chronic physical illnesses such as obesity and diabetes (Ludwig et al., 2011). Growing evidence suggests that neighborhood characteristics influence the rates and outcomes of mental illnesses as well, including schizophrenia (Eaton et al., 2019; Heinz et al., 2013; Kirkbride et al., 2014). Though sparsely studied in the United States, this association was first explored more than 80 years ago when Faris and Dunham (1939) demonstrated an association between high rates of schizophrenia and city zones in Chicago characterized by social disorder or lack of cohesion. They argued that those who resided in disorganized communities found it difficult to foster and maintain positive affiliations with local institutions, neighbors, and family members, thus increasing these residents’ sense of social isolation, which was deemed significant to the onset and course of mental illnesses (Faris, R. E. L., & Dunham, 1939). Some recent research suggests that neighborhood characteristics may influence rates of schizophrenia. Specifically, more population-dense areas and areas with lower socioeconomic status may have higher incidence rates of psychosis (Heinz et al., 2013; Kirkbride et al., 2014; Richardson et al., 2018). In addition, a few studies have assessed neighborhood variation in relation to prognostic factors and positive symptoms (Kirkbride et al., 2010; Newbury et al., 2016). However, in the United States, there has been a dearth of research to characterize the relationship between specific neighborhood factors and key manifestations of schizophrenia and related psychotic disorders.
An earlier age at onset of psychosis (AOP) and longer duration of untreated psychosis (DUP) are two important factors associated with poorer prognosis for schizophrenia (e.g., greater symptom severity, longer time to and likelihood of remission). Known risk factors for earlier AOP, one of the most commonly examined predictors of outcomes in schizophrenia (Clemmensen et al., 2012; Hafner et al., 1998; Immonen et al., 2017), include family history of psychosis (Suvisaari et al., 1998), male gender (Gureje, 1991; Hafner et al., 1998), and earlier age at initiation and more rapid escalation of premorbid cannabis use (Arseneault et al., 2002; Compton et al., 2009b; Kelley et al., 2016; McGrath et al., 2010; Stefanis et al., 2013; Zammit et al., 2002). Longer DUP is associated with poorer response to treatment, more frequent relapses, and poorer long-term symptom and functioning outcomes (Marshall et al., 2005; Perkins et al., 2005). Conversely, early detection of and intervention for psychosis considerably improves outcomes (Burns, 2013). Risk factors for longer DUP include chronic or insidious mode of onset of psychosis (Compton et al., 2008; Larsen et al., 1996; Morgan et al., 2006), history of incarceration (Broussard et al., 2013), and possibly cannabis use (Broussard et al., 2013; Burns, 2012).
Given the significance of AOP and DUP to the prognosis of schizophrenia, identifying other modifiable risk factors shaping them could ultimately inform means of improving outcomes. Exploring whether neighborhood characteristics in adolescence affect AOP and DUP could have a public health impact by leading to population-level interventions to influence the rate and course of psychotic disorders (and at the same time, many other illnesses and health outcomes).
To further explore the relationship between neighborhood characteristics and prognostic factors in early-course psychotic disorders, this analysis investigated the following questions: (1) Which neighborhood-level characteristics (both subjectively rated and objectively obtained), if any, are associated with AOP and DUP? (2) Do any potential effects of neighborhood-level characteristics on these prognostic factors remain after controlling for known risk factors for AOP and DUP? (3) Do the potential effects of neighborhood-level characteristics on these prognostic factors remain after controlling for individual-level sociodemographic characteristics? This study builds on the well-established link of urbanicity and neighborhood adversity with psychosis by examining the association of several neighborhood characteristics with AOP and DUP.
There have only been two studies investigating the relationship between neighborhood characteristics and DUP, in Southeast London and South Dublin (Kirkbride et al., 2010; O’Donoghue et al., 2016), which found conflicting results. While one study did not find variability in DUP across neighborhoods in Southeast London (Kirkbride et al., 2010), another reported that the least socially fragmented neighborhoods in South Dublin had very short DUPs (O’Donoghue et al., 2016). This is the first study in the United States, to our knowledge, to study the relationship between neighborhood characteristics and two prognostic factors: AOP and DUP. As such, we made no a priori hypotheses regarding the relationships between specific neighborhood characteristics and AOP or DUP. Based on prior literature examining the relationship between neighborhood characteristics and other health outcomes in the United States (Alegría et al., 2014; Krieger et al., 2002; Silver et al., 2002), we employed both objective (i.e., those obtained from census-tract data) and subjective (based on self-reported perceptions) measures of neighborhood characteristics to explore possible associations with AOP and DUP.
2. Methods
2.1. Subjects
The data were part of a project designed primarily to investigate the associations between premorbid cannabis use and AOP. This project included patients admitted to the hospital for a first episode of a schizophrenia-spectrum disorder; they were referred by clinicians in three inpatient psychiatric units in Atlanta, Georgia and three in Washington, D.C., based on the clinical diagnosis. The eligible age range for the study was 18 to 30 years. The Structured Clinical Interview for DSM-IV Axis I Disorders was used to make research diagnoses, using all available information, including in-depth interviews with participants. Among 713 subjects referred as potentially eligible or approached due to likely being eligible, a total of 247 were enrolled from August 2008 to June 2013. This study included only a subset of these participants (143) for whom we had data on their addresses during their adolescence. The study was approved by the Georgia Department of Human Resources IRB, the Grady Health System Research Oversight Committee, and the Emory University Institutional Review Board (IRB).
2.2. Instruments
Sociodemographic and clinical variables were obtained from informant/family member collateral, interview-based measures, and chart review. The data obtained was part of a larger clinical research assessment using a structured interview. Many sociodemographic and clinical variables were assessed, such as current and past addresses, individual-level residential instability (operationalized as the number of times one moved between ages 12 and 18), family history of psychosis, history of incarceration, mode of onset of psychosis, history of cannabis use, AOP, and DUP.
Mode of onset of psychosis was derived from a consensus-based best estimate process, using all available information (Compton et al., 2008). This variable was first classified into five types (Jablensky A, Sartorius N, Ernberg G, 1992) and then grouped into acute, subacute, and chronic. The Lifetime Substance Use Recall (LSUR) instrument is an interviewer-administered questionnaire, used to assess age at first cannabis use (Ramsay et al., 2011).
Individual-level general socioeconomic status (SES) was important to this study not only as an individual-level control variable, but also because prior research has shown that those with lower SES are more likely to present with a longer DUP (Peralta et al., 2005). This variable was created by averaging the z-scores of five variables: the patient’s highest level of education, the patient’s mother’s and the patient’s father’s highest level of education, and reverse-coded Hollingshead Redlich Index Scores for the mother and the father, which is an indicator of the highest occupational level ranging from 1 (high executives and major professions) to 9 (chronically jobless).
2.3. AOP and DUP
AOP and DUP were determined using the Symptom Onset in Schizophrenia (SOS) inventory (Perkins et al., 2000). The earliest date of onset of either hallucinations or delusions or both was determined by team consensus following a thorough review of all available information, including the patient’s in-depth, semi-structured SOS interview, as well as informants’ SOS interviews and the medical chart. DUP was operationalized as duration in weeks from the date of onset of either hallucinations or delusions (whichever came first) or both, based on criteria provided in the SOS. The end-point of the DUP measure was the date of hospital admission. This standardized approach to utilizing the SOS to determine AOP and DUP through consensus-based best-estimate methods has been described in prior reports (Compton et al., 2011, 2009a, 2009b, 2008). AOP and DUP were both dichotomized into earlier AOP and longer DUP variables, respectively, because the distribution for both AOP and DUP were highly skewed. As such, earlier AOP was defined as less than the third quartile of AOP (23 years), which was assigned a value of 1 while age greater or equal to 23 years was assigned a value of 0. Longer DUP was defined as greater than the third quartile of DUP (108 weeks), which was assigned a value of 1 while DUP less than or equal to 108 weeks was assigned a value of 0.
2.4. Neighborhood Disorder Scale
The Neighborhood Disorder Scale (NDS) was adapted to assess experiences with neighborhood-level social disorder during adolescence (Ross and Mirowsky, 1999). This scale, which is known to have good reliability and validity, contains 15 statements that were used to query participants about the neighborhood where they lived the longest between ages 12 and 18 years. Participants were asked to rate 15 statements on a scale of 1 (strongly disagree) to 4 (strongly agree). Examples of statements include the following: “There was a lot of graffiti in my neighborhood;” “My neighborhood was noisy;” “There was too much drug use in my neighborhood;” “There was a lot of crime in my neighborhood.”
2.5. Neighborhood-Level Variables
For this study, the selection of specific neighborhood characteristics was guided by prior neighborhood-based theory and research (Alegría et al., 2014; Krieger et al., 2002; Sampson and Groves, 1989; Shaw, C., & McKay, 1942; Silver et al., 2002). We accessed neighborhood characteristics using census tract-level data, designed to represent area-level properties in terms of living conditions, economic status, and population. Prior neighborhood-related health research showed that census tracts represent a valid level of area-based analysis (Krieger et al., 2002). Data were extracted from the 2006 to 2010 American Community Survey 5-year estimates and linked to addresses where individual lived during adolescence. See Figure 1 for a map of the census tracts in greater Atlanta, Georgia included in this study. This map was generated using factfinder.census.gov. Based on prior neighborhood-related health research, we selected the following 13 neighborhood characteristics: percentage of households with income greater than or equal to $75,000 in 2010 inflation-adjusted dollars (High Household Income); percentage of residents employed in arts occupations, science, business, and/or management among civilians employed and 16 years and over (White Collar Occupation); percentage of owner-occupied housing (Owner-Occupied); percentage of residents who are high school graduates or higher (High School); percentage of female-headed households with no husband present and family with own children under 18 years (Single Mother); percentage of families whose income in the past 12 months is below the federal poverty level (Poverty); percentage of Hispanic or Latino ethnicity (Hispanic/Latino); percentage of Black or African American race (Black/African American); percentage of births outside the United States (Foreign); percentage of residents unemployed among civilian labor force population 16 years and over (Unemployed); percentage of residents with cash public assistance income (Public Assistance); percentage living in a different house in the United States or living abroad within the past year (Residential Instability); and percentage value of houses less than $500,000 among owner-occupied units (Low Household Value).
Figure 1. Map of Census Tracts in Greater Atlanta, Georgia.
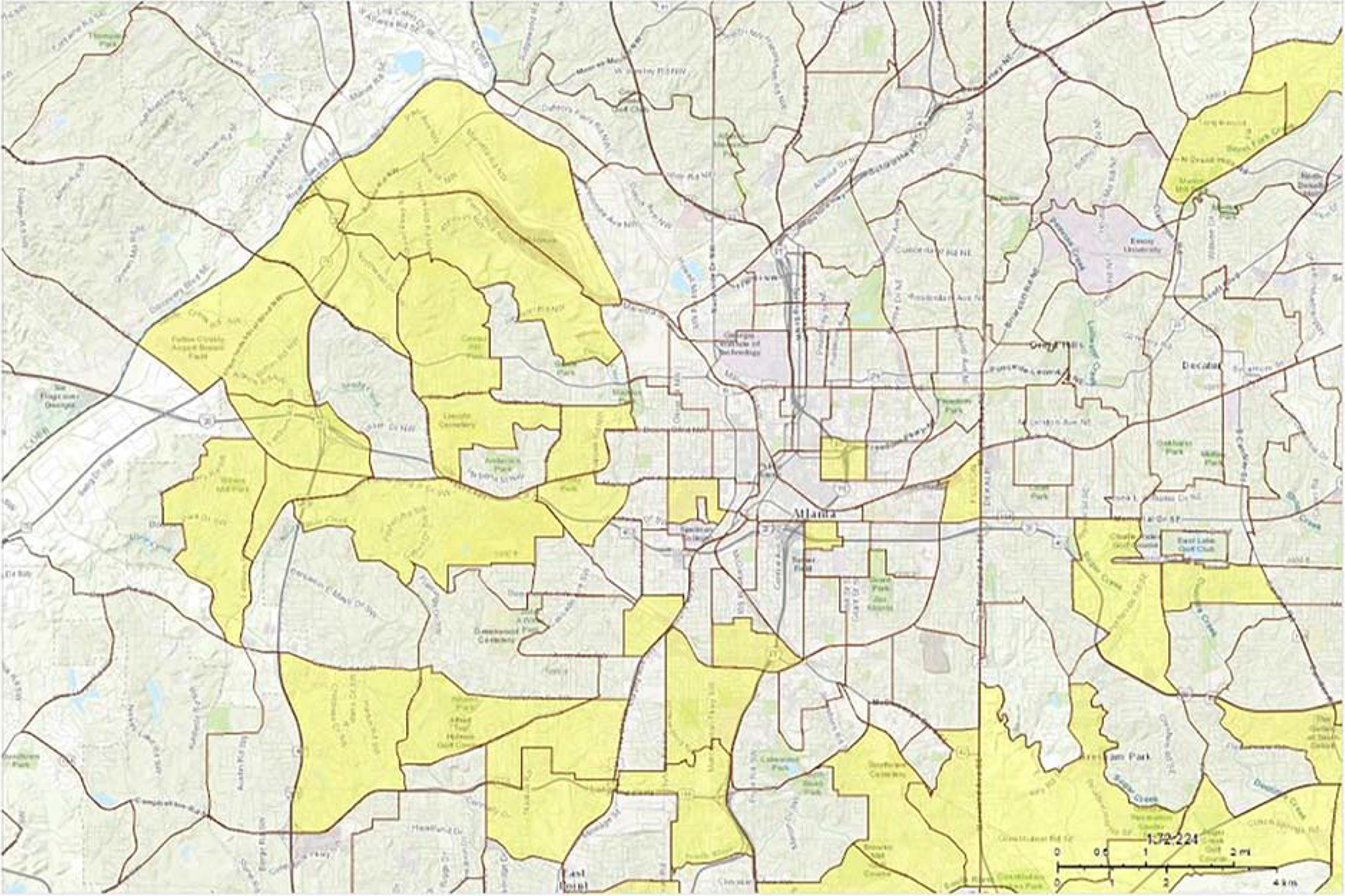
Note: Census Tracts are outlined in brown. Yellow highlighted census tracts represent those included in the present analysis (where one or more participants lived during adolescence).
Prior studies have shown an association between urbanicity and incidence of schizophrenia. The Census Bureau defines urban areas to be “a densely settled core of census tracts and/or census blocks that meet minimum population density requirements.” In this study, we considered using population density as one of our neighborhood-level factors; however, there was insufficient variability in population density in our sample because (1) our sample size was relatively small and (2) most participants lived in the metropolitan Atlanta area.
2.6. Data Analyses
We first calculated the correlation between the 13 census-tract derived neighborhood characteristics. After reverse scoring the variables with negative weights—denoted (reverse), we conducted a factor analysis to identify the neighborhood-level variables that were highly correlated with each other. For variables with loadings of ≥ 0.40 on more than one factors, we assigned the variable to the factor on which it loaded the strongest. We applied this convention in order to have factors with unique (non-overlapping) items and minimize inter-correlations.
Logistic regression was chosen because the distributions of the dependent variables were highly skewed and thus the variables were dichotomized. The first analysis shows bivariate associations between earlier AOP / longer DUP and the following nine variables: five neighborhood variables (including census-tract-derived factors and NDS), three known predictors of earlier AOP (age at first cannabis use, male gender, and family history of schizophrenia) or longer DUP (mode of onset of psychosis, history of incarceration, and age at first cannabis use), and an individual-level variable related to neighborhood-level variables that were ultimately significantly associated with the dependent variables.
To maximally understand the findings in this exploratory analyses, eight logistic regression models were carried out, with earlier AOP (Models A to D) and longer DUP (Models E to H) as the dependent variables. Models A/E include the five neighborhood variables (census-tract-derived factors and NDS) together, and then Models B/F show results of a stepwise backward elimination until all remaining variables are statistically significant. Models C/G then keep those significant variables and control for three known predictors of earlier AOP and longer DUP, and then Models D/H also control for an individual-level variable related to the neighborhood-level variable that was significantly associated with dependent variable. The IBM SPSS 18.0.0 statistical software package was used for all analyses.
3. Results
3.1. Sample Characteristics
SCID-determined diagnoses among the 143 participants included: schizophrenia (78, 54.6%), schizophreniform disorder (21, 14.7%), psychotic disorder not otherwise specified (25, 17.5%), schizoaffective disorder (14, 9.8%), delusional disorder (3, 2.1%), and brief psychotic disorder (2, 1.4%). The median age of participants was 22 years. The median years of school completed was 12. Most participants were African American (86.0%). The percentage of participants with a history of cannabis use was 86.0%. Some 67.1% were unemployed in the month prior to hospitalization. The median AOP and DUP were 21 years and 20 weeks, respectively. Sociodemographic and clinical characteristics of the sample are summarized in Table 1.
Table 1.
Demographic and Clinical Characteristics (n=143)
| Continuous Variables | Median | Interquartile Range |
|---|---|---|
| Age | 22 | (20–24) |
| Age at Onset of Psychosis | 21 | (19–23) |
| Duration of Untreated Psychosis (in weeks) | 20 | (4.75–108) |
| NDS Total | 34 | (29–42) |
| Years of School Completed | 12 | (11–13) |
| Residential Instability (number of moves from ages 12 to 18) | 1.5 | (1–2) |
| Age at First Cannabis Use | 15 | (13–17) |
| Hollingshead Redlich Index Score (Mother) | 4 | (2–6) |
| Hollingshead Redlich Index Score (Father) | 4 | (0–6) |
| Categorial Variables | n | % |
| Schizophrenia-Spectrum | ||
| Psychotic Disorder NOS | 25 | 17.5 |
| Schizophreniform Disorder | 21 | 14.7 |
| Schizophrenia | 78 | 54.6 |
| Schizoaffective Disorder | 14 | 9.8 |
| Bipolar Disorder with Psychotic Features | 3 | 2.1 |
| Brief Psychotic Disorder | 2 | 1.4 |
| Ethnicity/Race | ||
| Hispanic or Latino | 6 | 4.2 |
| African American | 123 | 86.0 |
| Caucasian | 9 | 6.3 |
| Other | 11 | 7.7 |
| Gender, Male | 103 | 72.0 |
| Marital Status, Single and Never Married | 130 | 90.9 |
| Unemployed in the Month Prior to Hospitalization | 96 | 67.1 |
| Family History of Schizophrenia | 22 | 15.4 |
| History of Incarceration | 76 | 53.1 |
| Living Below the Federal Poverty Level | 43 | 30.1 |
| Mode of Onset of Psychosis | ||
| Acute | 41 | 28.7 |
| Subacute | 16 | 11.2 |
| Chronic | 37 | 25.9 |
| History of Cannabis Use | 123 | 86.0 |
3.2. Exploratory Factor Analysis
The four factors produced by the factor analysis were as follows: Factor 1, General Socioeconomic Status, which included: High Household Income, White Collar Occupation, Owner-Occupied, High School, Single Mother (reverse), and Poverty (reverse); Factor 2, Race/Ethnicity/Unemployment, which included: Hispanic/Latino (reverse), Black/African American, Foreign (reverse), Unemployed, and Public Assistance; Factor 3, Residential Instability, which included only Residential Instability; and Factor 4, Low Household Value, which included only Low Household Value. Factor loadings (after Varimax rotation) from the exploratory factor analysis are shown in Table 2.
Table 2.
Factor Loadings from an Exploratory Factor Analysis of 13 Census-Tract Neighborhood Characteristics
| Factor | ||||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| High Household Income | .90 | −.15 | −.21 | −.21 |
| White Collar Occupation | .85 | .08 | −.06 | −.38 |
| Owner-Occupied | .82 | −.15 | −.34 | .43 |
| High School | .82 | .11 | .09 | .04 |
| Poverty (reverse) | .71 | −.23 | −.19 | −.08 |
| Single Mother (reverse) | .51 | −.48 | −.11 | −.12 |
| Hispanic/Latino (reverse) | .21 | .68 | −.08 | .11 |
| Black/African American | −.44 | .63 | <−.01 | .32 |
| Foreign (reverse) | .12 | .56 | −.01 | .43 |
| Public Assistance | −.20 | .42 | .01 | −.16 |
| Unemployed | −.38 | .40 | .12 | .32 |
| Residential Instability | −.17 | −.07 | .97 | .18 |
| Low Household Value | −.16 | .14 | .17 | .54 |
3.3. Earlier Age at Onset of Psychosis: Logistic Regression Models
Results of bivariate analysis and logistic regression models pertaining to earlier AOP—including the odds ratio (OR), 95% confidence intervals (CI), p-values, and adjusted Nagelkerke R2 of each model—are shown in Table 3. Bivariate analysis shows that neighborhood-level residential instability was significantly associated with earlier AOP (OR=1.760, 95% CI=1.085–2.856, p=0.022). When all five neighborhood-level factors were entered into the model, none of the factors were statistically significant (Model A), and after stepwise backward elimination, only neighborhood-level residential instability remained as significant (Model B) Neighborhood-level residential instability remained significantly associated with earlier AOP even after controlling for known risk factors for earlier AOP, including age at first cannabis use, male gender, and family history of schizophrenia (Model C) and also after controlling for individual-level residential instability (Model D; OR=1.917, 95% CI=1.040–3.535, p=0.037).
Table 3.
Logistic Regression Models for Earlier Age at Onset of Psychosis (AOP)
| Variables | Bivariate | Model A Multiple logistic regression model | Model B Regression model after stepwise backward elimination | Model C Controlling for known risk factors for AOP | Model D Controlling for individual-level residential instability | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | |
| F1 - General SES | 0.968 | 0.895–1.049 | 0.429 | 1.008 | 0.908–1.119 | 0.879 | |||||||||
| F2 - Race/ethnicity/unemployment | 1.020 | 0.904–1.151 | 0.745 | 1.031 | 0.886–1.200 | 0.691 | |||||||||
| F3 - Residential instability | 1.760 | 1.085–2.856 | 0.022 | 1.797 | 0.994–3.246 | 0.052 | 1.760 | 1.085–2.856 | 0.022 | 2.026 | 1.117–3.676 | 0.020 | 1.917 | 1.040–3.535 | 0.037 |
| F4 - Low household value | 1.462 | 0.983–2.175 | 0.061 | 1.168 | 0.721–1.892 | 0.529 | |||||||||
| NDS | 0.988 | 0.947–1.031 | 0.583 | 0.982 | 0.936–1.029 | 0.438 | |||||||||
| Age at first cannabis use | 0.941 | 0.786–1.127 | 0.509 | 0.957 | 0.780–1.174 | 0.673 | 0.981 | 0.797–1.209 | 0.860 | ||||||
| Male gender | 2.114 | 0.891–5.018 | 0.090 | 1.753 | 0.562–5.473 | 0.334 | 2.252 | 0.680–7.465 | 0.184 | ||||||
| Family history of psychosis | 1.111 | 0.369–3.346 | 0.851 | 0.583 | 0.164–2.077 | 0.406 | 0.572 | 0.157–2.088 | 0.398 | ||||||
| Individual-level residential instability | 1.346 | 0.830–2.184 | 0.228 | 1.587 | 0.810–3.111 | 0.178 | |||||||||
| *Nagelkerke R2 | 8.8% | 6.7% | 12.1% | 16.2% | |||||||||||
Note: OR represents Odds Ratio; CI = Confidence Interval;
Nagelkerke’s pseudo R2 reflects the model fit
3.4. Longer Duration of Untreated Psychosis: Logistic Regression Models
Results of bivariate analysis and logistic regression models for longer DUP are shown in Table 4. Bivariate analysis shows that NDS was positively associated with longer DUP. When all five neighborhood-level variables were entered into logistic model, both neighborhood-level General Socioeconomic Status (OR=1.174, 95% CI=1.041–1.323, p=0.009) and NDS (OR=1.090, 95% CI=1.032–1.151, p=0.002) were significantly associated with longer DUP (Model E); both of these variables remained significant after stepwise backward elimination (Model F). NDS (OR=1.146, 95% CI=1.032–1.273, p=0.011) remained significantly associated with longer DUP and neighborhood-level General Socioeconomic Status (OR=1.215, 95% CI=0.990–1.491, p=0.062) was very close to significance even after controlling for known predictors of longer DUP including mode of onset of psychosis, history of incarcerations, and age at first cannabis use (Model G), and also controlling for individual-level general socioeconomic status (Model H).
Table 4.
Logistic Regression Models for Longer Duration of Untreated Psychosis (DUP)
| Variables | Bivariate | Model E Multiple logistic regression model | Model F Regression model after stepwise backward elimination | Model G Controlling for known risk factors for DUP | Model H Controlling for individual-level general SES | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | |
| F1 - General SES | 1.058 | 0.976–1.147 | 0.170 | 1.174 | 1.041–1.323 | 0.009 | 1.119 | 1.019–1.230 | 0.019 | 1.164 | 0.973–1.391 | 0.097 | 1.215 | 0.990–1.491 | 0.062 |
| F2 - Race/ethnicity/unemployment | 0.981 | 0.867–1.110 | 0.762 | 0.972 | 0.827–1.144 | 0.735 | |||||||||
| F3 - Residential instability | 0.976 | 0.641–1.487 | 0.911 | 1.060 | 0.637–1.763 | 0.824 | |||||||||
| F4 - Low household value | 1.025 | 0.660–1.591 | 0.913 | 2.024 | 0.879–4.661 | 0.098 | |||||||||
| NDS | 1.053 | 1.007–1.101 | 0.023 | 1.090 | 1.032–1.151 | 0.002 | 1.075 | 1.023–1.131 | 0.005 | 1.132 | 1.027–1.248 | 0.012 | 1.146 | 1.032–1.273 | 0.011 |
| Mode of onset | 2.529 | 1.398–4.577 | 0.002 | 3.219 | 1.346–7.699 | 0.009 | 3.345 | 1.362–8.217 | 0.008 | ||||||
| History of incarcerations | 1.159 | 0.508–2.644 | 0.727 | 0.760 | 0.169–3.424 | 0.721 | 0.461 | 0.070–3.037 | 0.421 | ||||||
| Age at first cannabis use | 0.803 | 0.670–0.963 | 0.018 | 0.860 | 0.639–1.159 | 0.322 | 0.869 | 0.639–1.182 | 0.372 | ||||||
| Individual-level general SES | 0.921 | 0.492–1.722 | 0.796 | 0.553 | 0.168–1.817 | 0.329 | |||||||||
| *Nagelkerke R2 | 19.3% | 13.9% | 43.1% | 44.7% | |||||||||||
Note: OR represents Odds Ratio; CI = Confidence Interval;
Nagelkerke’s pseudo R2 reflects the model fit
4. Discussion
This study found that neighborhood-level characteristics affect important prognostic factors in early psychosis, specifically AOP and DUP. Even when controlling for known predictors of earlier AOP—and when controlling for individual-level residential instability—greater census-tract-level residential instability was associated with an earlier AOP. We also found that perceived/subjective neighborhood disorder as measured by the NDS was associated with a longer DUP and census-tract-level socioeconomic status was close to being significantly associated with DUP.
An effect of neighborhood residential instability on rates of psychosis has been reported before. Previous investigators found that neighborhood residential instability was associated with higher rates of schizophrenia, even after controlling for individual-level characteristics (Silver et al., 2002). It is possible that high levels of residential instability undermine social integration in neighborhoods, making it more difficult for individuals in these neighborhoods to sustain supportive social contacts with others, thereby increasing the risk that those who are predisposed to a mental disorder will manifest symptoms (Silver et al., 2002). Sampson and Groves showed that neighborhood residential instability and disadvantage each decrease local friendship ties through constraining individual friendship choices, leading to disruption to social support and in social integration (Sampson and Groves, 1989). Along these lines, one study showed that adverse neighborhood conditions such as low social cohesion, high neighborhood disorder, and crime victimization explained the relationship between urban upbringing and psychotic experiences in adolescents (J. Newbury et al., 2017).
Other studies, mainly conducted in Europe, have found that urbanicity, increased social fragmentation, living in a low ‘ethnic density’ area (with few people from the corresponding ethnic group), increased residential instability, and being a second-generation migrant were consistently associated with increased incidence of psychosis (Kirkbride et al., 2014, 2012; March et al., 2008; Price et al., 2018; Schofield et al., 2018; Sundquist et al., 2004; Vassos et al., 2012). Although this study investigated only prognostic factors rather than incidence of psychosis, it is possible that the same neighborhood-level risk factors are also causal risk factors that would increase incidence.
Just as how urbanicity or individual-level migration have been hypothesized to be related to the experience of social fragmentation (Zammit et al., 2010), living in an area in which the majority of people in the community are residentially unstable may also contribute to increased social stress. This stress has been shown to be associated with more dopamine dysregulation and may contribute to earlier AOP (Selten et al., 2013). Future research should examine mechanisms that may further elucidate the relationship between residential instability and AOP, especially given the importance of AOP as a long-term prognostic indicator.
We also found that higher neighborhood-level General Socioeconomic Status, and high perceived neighborhood disorder (higher NDS scores) were associated with longer DUP. The association between NDS and DUP has been previously documented in this sample (Broussard et al., 2013), but not in analyses including census-tract-level measures of neighborhood factors. The fact that we replicated the association between DUP and NDS, even when including “objective” measures of neighborhood and even while controlling for known risk factors including mode of onset, emphasizes the potential importance of the association between perceived neighborhood disorder and DUP. Prior research has shown that adolescents who perceived higher levels of neighborhood disorder were significantly more likely to have psychotic experiences, even after controlling for objective measures of crime and disorder, neighborhood- and family-level socioeconomic status (J. B. Newbury et al., 2017). The connection between greater perceived neighborhood disorder and longer DUP could be explained in multiple ways.
First, those who scored higher on NDS may be living in neighborhoods with lower access to mental health and social support service and/or weaker informal support networks. However, this lower access and weaker social support aspect of their neighborhood was not captured by our neighborhood-level variables. Although this may be a possible explanation, it is less likely as previous research also showed no correlation between objective measures of neighborhood characteristics and DUP. Second, those with a longer DUP may have more severe negative symptoms (Perkins et al., 2005), leading them to being isolated and to perhaps having feelings of loneliness, which has been shown to correlate with higher perceptions of neighborhood disorder (Matthews et al., 2019). That is, more lonely individuals perceive worse neighborhood conditions, even though objective measures are not associated with loneliness; this could suggest that lonely individuals (or those with longer DUP) are more fearful of their neighborhoods and are therefore less likely to seek help. Since DUP is an important prognostic factor for early psychosis, and reducing DUP is a key public health priority, the relationships between neighborhood conditions and DUP should be further explored. One notable difference in our study sample in comparison with other pertinent studies, mainly done in Europe, is that our sample had a longer DUP. Most participants in this study were recruited from public-sector hospitals that mainly serve those with no insurance or with State provided insurance (Medicaid) only. In our context, being uninsured or underinsured is associated with demographic characteristics such as race, and clinical characteristics, such as a high prevalence of substance abuse. Previous studies in this population have shown that lack of insurance and substance abuse are predictive of longer treatment delay (Compton et al., 2011); these factors may be quite different in samples from European countries that show a shorter DUP.
There are several limitations of this study. First, the sample’s narrow sociodemographic and clinical characteristics may limit generalizability of these findings to other first-episode samples. Furthermore, the sample included only those patients with psychosis presenting to six hospitals, most of which were public-sector facilities; as such, patients presenting to other settings (e.g., private psychiatric hospitals, outpatient clinics) were not included, which impacts generalizability. However, this study sample’s demographics and clinical characteristics were relatively homogeneous which improves the internal validity of the results. Second, due to the small study sample, we were unable to conduct a multi-level analysis. Thus, we were not able to further investigate the interaction between participants’ and their neighborhoods’ characteristics on prognostic factors of first episode psychosis. Third, only a subset of patients (those remembering their address and for whom the address could be validating by geo-coding) were included in this analysis; the potential for a bias cannot be excluded.
Finally, the parent study was not designed to test the relationships between neighborhood factors and early psychosis outcomes (i.e., this was a secondary analysis), and as a result, both the variables and power to explore effects were limited. With regard to potential mediators, it is possible that people living in residentially unstable and socially disordered neighborhoods are exposed to stressful life events more frequently and have less access to adequate social supports. These socially structured life experiences, in turn, are expected to increase the risk of psychological distress. However, we did not measure life stress or social support, and as such were unable to test their relationship to AOP and DUP in these analyses. In addition to incorporating individual-level mediating variables, future research on the relationships between neighborhood-level characteristics and prognostic factors in early psychosis should incorporate additional area-level data. This would enable a better understanding of the dynamic relationships between population-level structural characteristics and the prognosis of schizophrenia, which would potentially highlight opportunities for public health interventions that might ultimately improve outcomes for individuals with schizophrenia.
Funding:
This research was supported by grants K23 MH067589 and R01 MH081011 from the National Institute of Mental Health (NIMH).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Alegría M, Molina KM, Chen C-N, 2014. Neighborhood Characteristics and Differential Risk for Depressive and Anxiety Disorders Across Racial/Ethnic Groups in the United States. Depress. Anxiety 31, 27–37. 10.1002/da.22197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arseneault L, Cannon M, Poulton R, Murray R, Caspi A, Moffitt TE, 2002. Cannabis use in adolescence and risk for adult psychosis: longitudinal prospective study. BMJ 325, 1212–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broussard B, Kelley ME, Wan CR, Cristofaro SL, Crisafio A, Haggard PJ, Myers NL, Reed T, Compton MT, 2013. Demographic, socio-environmental, and substance-related predictors of duration of untreated psychosis (DUP). Schizophr. Res 148, 93–8. 10.1016/j.schres.2013.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns JK, 2013. Pathways from cannabis to psychosis: a review of the evidence. Front. psychiatry 4, 128 10.3389/fpsyt.2013.00128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns JK, 2012. Cannabis use and duration of untreated psychosis: a systematic review and meta-analysis. Curr. Pharm. Des 18, 5093–104. [DOI] [PubMed] [Google Scholar]
- Clemmensen L, Vernal DL, Steinhausen H-C, 2012. A systematic review of the long-term outcome of early onset schizophrenia. BMC Psychiatry 12, 150 10.1186/1471-244X-12-150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton MT, Chien VH, Leiner AS, Goulding SM, Weiss PS, 2008. Mode of onset of psychosis and family involvement in help-seeking as determinants of duration of untreated psychosis. Soc. Psychiatry Psychiatr. Epidemiol 43, 975–982. 10.1007/s00127-008-0397-y [DOI] [PubMed] [Google Scholar]
- Compton MT, Gordon TL, Goulding SM, Esterberg ML, Carter T, Leiner AS, Weiss PS, Druss BG, Walker EF, Kaslow NJ, 2011. Patient-Level Predictors and Clinical Correlates of Duration of Untreated Psychosis Among Hospitalized First-Episode Patients. J. Clin. Psychiatry 72, 225–232. 10.4088/JCP.09m05704yel [DOI] [PubMed] [Google Scholar]
- Compton MT, Goulding SM, Gordon TL, Weiss PS, Kaslow NJ, 2009a. Family-level predictors and correlates of the duration of untreated psychosis in African American first-episode patients. Schizophr. Res 115, 338–345. 10.1016/j.schres.2009.09.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton MT, Ramsay CE, Shim RS, Goulding SM, Gordon TL, Weiss PS, Druss BG, 2009b. Health Services Determinants of the Duration of Untreated Psychosis Among African-American First-Episode Patients. Psychiatr. Serv 60, 1489–1494. 10.1176/ps.2009.60.11.1489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton S, Harrap B, Downey L, Thien K, Bowtell M, Bardell-Williams M, Ratheesh A, McGorry P, O’Donoghue B, 2019. Incidence of treated first episode psychosis from an Australian early intervention service and its association with neighbourhood characteristics. Schizophr. Res 209, 206–211. 10.1016/j.schres.2019.04.017 [DOI] [PubMed] [Google Scholar]
- Faris REL, & Dunham HW, 1939. Mental disorders in urban areas: an ecological study of schizophrenia and other psychoses. The University Chicago Press, Chicago/London. [Google Scholar]
- Gureje O, 1991. Gender and schizophrenia: age at onset and sociodemographic attributes. Acta Psychiatr. Scand 83, 402–405. 10.1111/j.1600-0447.1991.tb05564.x [DOI] [PubMed] [Google Scholar]
- Hafner H, an der Heiden W, Behrens S, Gattaz WF, Hambrecht M, Loffler W, Maurer K, Munk-Jorgensen P, Nowotny B, Riecher-Rossler A, Stein A, 1998. Causes and Consequences of the Gender Difference in Age at Onset of Schizophrenia. Schizophr. Bull 24, 99–113. 10.1093/oxfordjournals.schbul.a033317 [DOI] [PubMed] [Google Scholar]
- Heinz A, Deserno L, Reininghaus U, 2013. Urbanicity, social adversity and psychosis. World Psychiatry 12, 187–97. 10.1002/wps.20056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Immonen J, Jääskeläinen E, Korpela H, Miettunen J, 2017. Age at onset and the outcomes of schizophrenia: A systematic review and meta-analysis. Early Interv. Psychiatry 11, 453–460. 10.1111/eip.12412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jablensky A, Sartorius N, Ernberg G, et al. , 1992. Chapter 2. Sociodemographic, clinical and diagnostic description of the study population., Psychol Med. [Google Scholar]
- Kelley ME, Wan CR, Broussard B, Crisafio A, Cristofaro S, Johnson S, Reed TA, Amar P, Kaslow NJ, Walker EF, Compton MT, 2016. Marijuana use in the immediate 5-year premorbid period is associated with increased risk of onset of schizophrenia and related psychotic disorders. Schizophr. Res 171, 62–67. 10.1016/j.schres.2016.01.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkbride JB, Errazuriz A, Croudace TJ, Morgan C, Jackson D, Boydell J, Murray RM, Jones PB, 2012. Incidence of Schizophrenia and Other Psychoses in England, 1950–2009: A Systematic Review and Meta-Analyses. PLoS One 7, e31660 10.1371/journal.pone.0031660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkbride JB, Jones PB, Ullrich S, Coid JW, 2014. Social Deprivation, Inequality, and the Neighborhood-Level Incidence of Psychotic Syndromes in East London. Schizophr. Bull 40, 169–180. 10.1093/schbul/sbs151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkbride JB, Lunn DJ, Morgan C, Lappin JM, Dazzan P, Morgan K, Fearon P, Murray RM, Jones PB, 2010. Examining evidence for neighbourhood variation in the duration of untreated psychosis. Health Place 16, 219–25. 10.1016/j.healthplace.2009.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Chen JT, Waterman PD, Soobader M-J, Subramanian SV, Carson R, 2002. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter?: the Public Health Disparities Geocoding Project. Am. J. Epidemiol 156, 471–82. [DOI] [PubMed] [Google Scholar]
- Larsen TK, McGlashan TH, Moe LC, 1996. First-episode Schizophrenia: I. Early Course Parameters. Schizophr. Bull 22, 241–256. 10.1093/schbul/22.2.241 [DOI] [PubMed] [Google Scholar]
- Ludwig J, Sanbonmatsu L, Gennetian L, Adam E, Duncan GJ, Katz LF, Kessler RC, Kling JR, Lindau ST, Whitaker RC, McDade TW, 2011. Neighborhoods, obesity, and diabetes--a randomized social experiment. N. Engl. J. Med 365, 1509–19. 10.1056/NEJMsa1103216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- March D, Hatch SL, Morgan C, Kirkbride JB, Bresnahan M, Fearon P, Susser E, 2008. Psychosis and Place. Epidemiol. Rev 30, 84–100. 10.1093/epirev/mxn006 [DOI] [PubMed] [Google Scholar]
- Marshall M, Lewis S, Lockwood A, Drake R, Jones P, Croudace T, 2005. Association Between Duration of Untreated Psychosis and Outcome in Cohorts of First-Episode Patients. Arch. Gen. Psychiatry 62, 975 10.1001/archpsyc.62.9.975 [DOI] [PubMed] [Google Scholar]
- Matthews T, Odgers CL, Danese A, Fisher HL, Newbury JB, Caspi A, Moffitt TE, Arseneault L, 2019. Loneliness and Neighborhood Characteristics: A Multi-Informant, Nationally Representative Study of Young Adults. Psychol. Sci 30, 765–775. 10.1177/0956797619836102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGrath J, Welham J, Scott J, Varghese D, Degenhardt L, Hayatbakhsh MR, Alati R, Williams GM, Bor W, Najman JM, 2010. Association Between Cannabis Use and Psychosis-Related Outcomes Using Sibling Pair Analysis in a Cohort of Young Adults . Arch. Gen. Psychiatry 67, 440 10.1001/archgenpsychiatry.2010.6 [DOI] [PubMed] [Google Scholar]
- Morgan C, Abdul-Al R, Lappin JM, Jones P, Fearon P, Leese M, Croudace T, Morgan K, Dazzan P, Craig T, Leff J, Murray R, AESOP Study Group, 2006. Clinical and social determinants of duration of untreated psychosis in the AESOP first-episode psychosis study. Br. J. Psychiatry 189, 446–52. 10.1192/bjp.bp.106.021303 [DOI] [PubMed] [Google Scholar]
- Newbury J, Arseneault L, Caspi A, Moffitt TE, Odgers CL, Fisher HL, 2017. Cumulative Effects of Neighborhood Social Adversity and Personal Crime Victimization on Adolescent Psychotic Experiences. Schizophr. Bull 10.1093/schbul/sbx060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newbury J, Arseneault L, Caspi A, Moffitt TE, Odgers CL, Fisher HL, 2016. Why Are Children in Urban Neighborhoods at Increased Risk for Psychotic Symptoms? Findings From a UK Longitudinal Cohort Study. Schizophr. Bull 42, 1372–1383. 10.1093/schbul/sbw052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newbury JB, Arseneault L, Caspi A, Moffitt TE, Odgers CL, Baldwin JR, Zavos HMS, Fisher HL, 2017. In the eye of the beholder: Perceptions of neighborhood adversity and psychotic experiences in adolescence. Dev. Psychopathol 29, 1823–1837. 10.1017/S0954579417001420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Donoghue B, Lyne JP, Renwick L, Lane A, Madigan K, Staines A, O’Callaghan E, Clarke M, 2016. Neighbourhood characteristics and the incidence of first-episode psychosis and duration of untreated psychosis. Psychol. Med 46, 1367–78. 10.1017/S003329171500286X [DOI] [PubMed] [Google Scholar]
- Peralta V, Cuesta MJ, Martinez-Larrea A, Serrano JF, Langarica M, 2005. Duration of untreated psychotic illness. Soc. Psychiatry Psychiatr. Epidemiol 40, 345–349. 10.1007/s00127-005-0905-2 [DOI] [PubMed] [Google Scholar]
- Perkins DO, Gu H, Boteva K, Lieberman JA, 2005. Relationship Between Duration of Untreated Psychosis and Outcome in First-Episode Schizophrenia: A Critical Review and Meta-Analysis. Am. J. Psychiatry 162, 1785–1804. 10.1176/appi.ajp.162.10.1785 [DOI] [PubMed] [Google Scholar]
- Perkins DO, Leserman J, Jarskog LF, Graham K, Kazmer J, Lieberman JA, 2000. Characterizing and dating the onset of symptoms in psychotic illness: the Symptom Onset in Schizophrenia (SOS) inventory. Schizophr. Res 44, 1–10. [DOI] [PubMed] [Google Scholar]
- Price C, Dalman C, Zammit S, Kirkbride JB, 2018. Association of Residential Mobility Over the Life Course With Nonaffective Psychosis in 1.4 Million Young People in Sweden. JAMA psychiatry 75, 1128–1136. 10.1001/jamapsychiatry.2018.2233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramsay CE, Abedi GR, Marson JD, Compton MT, 2011. Overview and initial validation of two detailed, multidimensional, retrospective measures of substance use: The Lifetime Substance Use Recall (LSUR) and Longitudinal Substance Use Recall for 12 Weeks (LSUR-12) Instruments. J. Psychiatr. Res 45, 83–91. 10.1016/j.jpsychires.2010.04.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson L, Hameed Y, Perez J, Jones PB, Kirkbride JB, 2018. Association of Environment With the Risk of Developing Psychotic Disorders in Rural Populations. JAMA Psychiatry 75, 75 10.1001/jamapsychiatry.2017.3582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross CE, Mirowsky J, 1999. Disorder and Decay. Urban Aff. Rev 34, 412–432. 10.1177/107808749903400304 [DOI] [Google Scholar]
- Sampson RJ, Groves WB, 1989. Community Structure and Crime: Testing Social-Disorganization Theory. Am. J. Sociol 94, 774–802. 10.2307/2780858 [DOI] [Google Scholar]
- Schofield P, Thygesen M, Das-Munshi J, Becares L, Cantor-Graae E, Agerbo E, Pedersen C, 2018. Neighbourhood ethnic density and psychosis - Is there a difference according to generation? Schizophr. Res 195, 501–505. 10.1016/j.schres.2017.09.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selten J-P, van der Ven E, Rutten BPF, Cantor-Graae E, 2013. The social defeat hypothesis of schizophrenia: an update. Schizophr. Bull 39, 1180–6. 10.1093/schbul/sbt134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw C, & McKay H, 1942. Juvenile delinquency and urban areas, University of Chicago Press; Chicago. [Google Scholar]
- Silver E, Mulvey EP, Swanson JW, 2002. Neighborhood structural characteristics and mental disorder: Faris and Dunham revisited. Soc. Sci. Med 55, 1457–70. [DOI] [PubMed] [Google Scholar]
- Stefanis NC, Dragovic M, Power BD, Jablensky A, Castle D, Morgan VA, 2013. Age at Initiation of Cannabis Use Predicts Age at Onset of Psychosis: The 7- to 8-Year Trend. Schizophr. Bull 39, 251–254. 10.1093/schbul/sbs188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundquist K, Frank G, Sundquist J, 2004. Urbanisation and incidence of psychosis and depression: follow-up study of 4.4 million women and men in Sweden. Br. J. Psychiatry 184, 293–8. [DOI] [PubMed] [Google Scholar]
- Suvisaari JM, Haukka J, Tanskanen A, Lönnqvist JK, 1998. Age at onset and outcome in schizophrenia are related to the degree of familial loading. Br. J. Psychiatry 173, 494–500. [DOI] [PubMed] [Google Scholar]
- Vassos E, Pedersen CB, Murray RM, Collier DA, Lewis CM, 2012. Meta-Analysis of the Association of Urbanicity With Schizophrenia. Schizophr. Bull 38, 1118–1123. 10.1093/schbul/sbs096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zammit S, Allebeck P, Andreasson S, Lundberg I, Lewis G, 2002. Self reported cannabis use as a risk factor for schizophrenia in Swedish conscripts of 1969: historical cohort study. BMJ 325, 1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zammit S, Lewis G, Rasbash J, Dalman C, Gustafsson J, Allebeck P, 2010. Individuals, schools, and neighborhood: a multilevel longitudinal study of variation in incidence of psychotic disorders. Arch. Gen. Psychiatry 67, 914–22. 10.1001/archgenpsychiatry.2010.101 [DOI] [PubMed] [Google Scholar]


