Abstract
Background:
While gait assessments are recommended to evaluate fall risk in older adults, these often involve walking in a straight line, even though one-third of steps taken throughout the day involve turning. Falls that occur during a turn tend to be more serious than falls that occur during a straight walk, but little is known about how gait variables collected during a turn can predict falls.
Research Question:
How do gait characteristics collected from straight and turning walking phases predict falls in older adults?
Methods:
We prospectively examined the association between six quantitative gait variables measured during normal walking turn and straight walking phases as predictors of incident falls in a community-based sample of older adults (N=253; mean age 78.5; 51% women). Cox regressions adjusted for multiple potential confounders were used to examine the associations.
Results:
Participants had significantly slower stride velocity (57.81 vs 83.26 cm/s), shorter stride length (74.76 vs 101.81 cm,), lower swing (30.1 vs 32.41 %), higher double support (39.79 vs 35.19 %), and more swing (30.09 vs 32.41 %) and stride length variability (31.86 vs 6.35 %) during turns compared with straights. Higher swing percent in both turns (adjusted hazard ratio; HR 0.92, 95% CI 0.87, 0.97) and straights (HR 0.89, 95% CI 0.84, 0.96) was associated with reduced risk of falls. Higher double support percent during both turns (HR 1.04, 95% CI 1.01, 1.07) and straights (HR 1.06, 95% CI 1.02, 1.09) was associated with increased risk of falls. More swing variability during turns (HR 1.03, 95% CI 1.00, 1.06), but not straights, was associated with increased risk of falls.
Significance:
Gait variables collected during turning and walking straight were similar in their predictions of future falls. In the future, clinical research that builds on these findings could improve identification and prevention of falls.
Keywords: Gait, turns, falls
Introduction:
Falls are the most common cause of injuries and one of the leading causes of death, hospitalizations, and disabilities in older adults[1]. Gait abnormalities are consistently recognized as among the strongest risk factors for falls in older adults[2–8]. Discrete gait variables such as slow speed and increased variability have been especially associated with higher risk of falls[9]. Gait assessment is, thus, widely recommended by national organizations [10] and experts to evaluate fall risk in older adults [1–2, 6–7, 20].
Most quantitative or clinical gait protocols involve walking straight on instrumented walkways or over a fixed distance. Thus, turns, pivots, and other weight shifts are not always taken into account in these gait assessments done to assess for falls risk, even though one-third of steps taken throughout the day involve turning while walking[11, 12]. Difficulty turning while walking is an indicator of impaired balance, and could be a major contributor to falls [13]. Furthermore, falls while turning are associated with more injuries than falls during straight walking [14]. However, the question of whether gait variables assessed during turns may improve the ability of gait protocols to predict incident falls has not been established. To address this knowledge gap, we examined and compared the validity of quantitative gait characteristics while turning or walking straight for predicting incident falls in older adults.
Methods:
Participants:
We examined 253 community-residing adults age 65 and over participating in the Central Control for Mobility in Aging (CCMA) study, a gait and mobility study based in the Bronx County, New York, USA [15]. CCMA procedures have been previously reported [15, 16]. In brief, research assistants interviewed potential participants living in lower Westchester County by telephone to assess eligibility and to rule out dementia using established cut-scores on cognitive screening assessments[15]. Individuals who passed the telephone interview and expressed interest in participating in the study were invited to our center where they underwent detailed demographic and medical history intake as well as clinical, gait, and neuropsychological testing[16]. Dementia diagnoses were assigned at consensus case conferences after review of all clinical and neuropsychological data[16]. Exclusion criteria for CCMA included presence of dementia, inability to walk (even with assistance), active neurological or psychiatric disorders severe enough to interfere with study assessments, presence of major visual or hearing loss, and recent or planned surgical procedures restricting walking. All participants provided written informed consents. The Einstein institutional review board approved the study protocol.
Walking protocol:
Quantitative gait assessments were performed on a 4 × 25 foot walkway (Zenometrics, LLC; Peekskill, NY) which was embedded with pressure sensors. The Protokinetics Movement Analysis Software (PKMAS) was used to characterize individual gait variables including stride length (cm), stride length variability (percent of coefficient of variation CV), stride velocity (cm/s), swing phase (percent), swing time variability (CV), and double support phase (percent). Stride velocity as a measure is calculated based on the location and mathematical parameters between sequential footfalls on the pressurized carpet[17]. Swing percent is calculated by an average of the right foot; the percentage over the distance that the participant walked. These variables were chosen based on their strong association with fall risk in our and other studies [5, 9, 18–21]. As previously described with figures [12], participants were instructed to walk on the carpet for three continuous loops. The outline of the walking area was delineated with black tape, and there were no visual indicators on the recording surface to indicate where participants should turn. Each loop consisted of two straight walks and two 180-degree turns, which resulted in a total of six turns and six straight walks for each assessment per individual [12]. Participants always began in the right proximal corner of the mat, walked in the same initial direction, and made wide, counterclockwise turns at the end of the carpet. Turns were defined as “a change in direction while walking” and includes an entry point, curved path, and exit point. The computerized algorithm determines the first footfall entering or exiting a turn by analyzing the changes of footfall angles of the same limb. Next, it defines the turn entry point or exit point as the beginning of the swing phase of the opposite limb [12].
Falls:
Falls were defined as unintentionally coming down to the floor or a lower level not due to a major intrinsic or extrinsic event [4, 21–23]. Participants were interviewed by research assistants using standardized questionnaires about the occurrence of falls at their baseline visit, during annual follow-up clinic visits, and in brief telephone interviews, which occurred every two to four months between the in-person visits (mean time between calls: 2.35 months ± 0.85 months). Standardized fall questionnaires were used to reduce variability between interviewers. In a previous study that used the same methodology for falls assessment [24] we reported high consistencies between participant reports of falls during these bimonthly phone calls, and during their yearly in-person interviews. All reported falls, regardless of whether they occurred when a participant was walking or not, were included in the statistical analyses.
Covariates:
Age, gender, years of education, Global Health Score (GHS), and a history of falls in the previous year were included as covariates in all statistical analyses [25]. The GHS is an internal survey which assigns individuals a comorbidity score (0-10) based on the prevalence of any of the following ten physician diagnosed conditions: angina, arthritis, chronic heart failure, chronic obstructive pulmonary disease, depression, diabetes, hypertension, myocardial infarction, Parkinson’s disease and stroke.
Statistical Analysis:
Baseline characteristics were compared with descriptive statistics, and an independent samples t-test was used to compare fallers and non-fallers on quantitative gait variables during turn and straight walking phases. Gait variables taken from turns and straights were used to separately predict future falls using Cox proportional hazards models. Hazard ratios (HR) with 95% confidence intervals (CI) were computed to predict incident falls based on baseline quantitative gait performance on the five selected parameters. Time scale was follow-up time (years) to incident fall or final contact. All models were adjusted for age, sex, education, GHS, and falls in the previous year. All analyses were conducted using SPSS version 25 (SPSS Inc., Chicago, IL).
Results
The mean age of the participants was 78.59 years and 51% were women. There was a low prevalence of major chronic medical illnesses among our community residing participants, with an average GHS score of 0.94 (Standard Deviation (SD) 0.95). Seventy-seven (30.4%) of participants reported using an assistive device to walk, though none of the participants used their assistive device during the gait assessment for the current study. Of the 253 participants, 50.6% (n = 128) reported at least one fall over the study follow-up. The mean time to incident fall was 1.10 years (SD 0.74); for those without an incident fall mean time to final contact was 2.16 years (SD 0.83).
Table 1 shows that fallers and non-fallers showed significant differences only on swing percent and double support percent. In general, the selected gait variables were worse during turns compared to straight phases for both fallers and non-fallers. When examining the overall group, performance was significantly worse for all of the variables during the turn phase compared to straight (p<0.01; data not shown).
Table 1:
Gait Variables during straight and turn phases at baseline assessment for those who did and did not have an incident fall (n=253)
| Fallers (n=128) | Non-fallers (n=125) | p-value | ||
|---|---|---|---|---|
| Variable | Mean Std. Deviation | Mean Std. Deviation | ||
| Stride Length (cm) | Straight | 101.01 19.21 | 102.62 18.55 | 0.497 |
| Turn | 74.24 17.95 | 75.29 18.09 | 0.645 | |
| Stride Length Variability (CV) | Straight | 6.37 3.12 | 6.29 3.05 | 0.860 |
| Turn | 32.07 7.01 | 31.63 7.69 | 0.638 | |
| Stride Velocity (cm/s) | Straight | 82.27 21.67 | 84.32 19.47 | 0.420 |
| Turn | 57.19 17.02 | 58.44 15.49 | 0.540 | |
| Swing Percent | Straight | 32.08 2.76 | 32.74 2.44 | 0.047* |
| Turn | 29.70 3.69 | 30.50 3.24 | 0.067 | |
| Swing Time Variability | Straight | 7.47 4.52 | 7.09 3.98 | 0.484 |
| Turn | 13.95 7.40 | 13.00 6.02 | 0.483 | |
| Double Support Percent | Straight | 35.79 5.55 | 34.43 4.94 | 0.041* |
| Turn | 40.59 7.43 | 38.98 6.38 | 0.066 |
Table 2 shows that higher swing percent was associated with a reduced risk of incident falls in both straights (p =0.002) and turns (p =0.003), whereas higher swing time variability was associated with increased risk of falls only during turns (p =0.030). More time spent in the double support phase in both straights (p =0.001) and turns (p =0.002) was associated with an increased risk of falls. To graphically present results, we dichotomized swing percent and double support percent by median split. The dichotomized variables during turns and straights were associated with increased risk for falls (Figure 1). In both straight and turn walking phases, stride length, stride length variability and stride velocity were not significant predictors of future falls. Higher swing time time variability during turns was borderline significant after adjustment for reported use of an assistive device in daily life (p=0.057).
Table 2:
Association of quantitative gait variables during straight and turn phases with incident falls.
| Variable | Adjusted* Hazard Ratio (95% Confidence Interval), p-value | |
|---|---|---|
| Straights | Turns | |
| Stride Length (cm) | 0.99 (0.98, 1.00), 0.214 | 0.99 (0.98, 1.00), 0.190 |
| Stride Length Variability (CV) | 1.02 (0.96, 1.01), 0.570 | 1.02 (0.99, 1.01), 0.184 |
| Stride Velocity (cm/s) | 0.99 (0.98, 1.00), 0.212 | 0.99 (0.98, 1.00), 0.193 |
| Swing Percent (%) | 0.89 (0.84, 0.96), 0.002 | 0.92 (0.87, 0.97), 0.003 |
| Swing Percent Variability (CV) | 1.03 (0.99, 1.070), 0.209 | 1.03 (1.00, 1.06), 0.030 |
| Double Support Percent (%) | 1.06 (1.02, 1.09), 0.001 | 1.04 (1.01, 1.07), 0.002 |
CV: Coefficient of Variation
All values adjusted for age, gender, years of education, global health score, and falls in the last year
Figure 1.
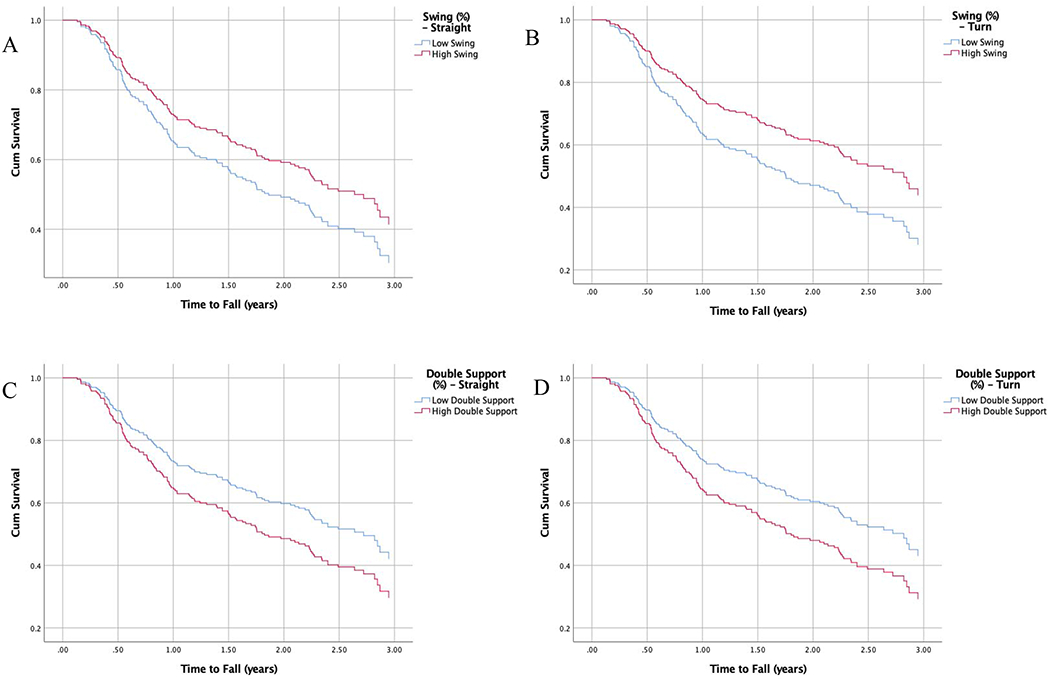
Survival Plots for the Risk of Incident Falls for Swing Percent during Straights (A) and Turns (B) and Double Support Percent during Straights (C) and Turns (D)
Discussion
Our findings demonstrate that turns and straights are similar in their prediction of future falls. Both double support percent and swing percent are strong, significant predictors of future falls, and they predict falls both in straight and turn phases of walks. Swing time variability during turns alone predicted falls.
This finding is generally supported by previous studies. While these studies did not examine measurements collected in the turn phase, swing percent and double support percent during straight walking phases are variables that have been identified as reliable predictors of future falls [9, 26–28]. Previous studies [26, 27] have suggested that fallers may have higher rates of these two variables because they employ a more cautious gait strategy to maintain balance as they walk. Measures of gait variability have also been shown to be predictors of falls [9, 28]; however, the present study found only swing variability during turns to be predictive of future falls. Previous studies have attributed this to unstable gait and poor balance, which may be exacerbated during turns [26]. Differences in predicting for falls may be expected compared to other protocols such as on the spot turns. Gait velocity, which has been widely shown to predict falls [20], did not significantly predict falls in either condition in the current study. We have previously reported that velocity is not always the strongest predictor of falls in comparison to other variables such as swing time, swing time variability and double support[9]. Furthermore, differences in calculating velocity, as well as our healthy community-dwelling sample with low comorbid illnesses, might also contribute to the lack of predictive validity of velocity. While the selected gait variables were different between straight and turn phases, their predictive validity for falls was similar. The overlap in variables associated with falls during the turn and straight phases of walking suggest similar gait generation and control processes might be involved in increasing fall risk in our participants regardless of the walking pattern. Further mechanistic studies are required to address this observation.
Strengths of this study include a well-documented, large sample size with established clinical, gait and fall collection measures and procedures. Within-participant comparisons reduced variability in gait and outcome measure. However, there are also several limitations—the sample included healthy community-residing older adults, and may not be generalizable to those who are institutionalized or have cognitive impairments. Falls were all self-reported through either in-person appointments or structured telephone calls; however, reports were not confirmed through medical records. By excluding participants with dementia and monitoring falls at short intervals through multiple assessments using standardized questionnaires, we aimed to increase reliability of falls reporting, which has been shown to be high in our previous studies [29]. While our sample size was relatively large compared to previous studies [12], we controlled for only the most important fall-related covariates, but it is possible that unmeasured confounding could influence our findings, and this could be tested in larger samples. Finally, our observational study design supports temporal associations of gait abnormalities preceding falls, but does not establish causality.
Conclusions:
While further studies are needed to examine how aspects of the turn phase influence gait and may be causal for falls, this study has promising findings regarding the validity and utility of specific gait variables during turns versus straights as a predictors of falls. Since changing directions and taking turns are large aspects of daily walking patterns, [11, 12] future research could build on these findings to improve identification and prevention of falls.
Highlights:
Turning and straight walking gait variables are similar in their prediction of falls.
Higher swing percent in both phases is associated with a reduced risk of falls.
Higher double support percent in both phases is associated with increased fall risk.
Swing variability during turns only is associated with fall risk.
Acknowledgements:
This study was supported by the National Institute on Aging grants (ROI AG044007 and ROI AG036921) and an intramural grant from the Resnick Gerontology Center, Albert Einstein College of Medicine, Bronx, NY, USA.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of Competing Interest
There were no conflicts of interest with other authors or institution for this study.
References
- [1].Mancini M, Schlueter H, El-Gohary M, Mattek N, Duncan C, Kaye J, et al. , Continuous Monitoring of Turning Mobility and Its Association to Falls and Cognitive Function: A Pilot Study, The journals of gerontology. Series A, Biological sciences and medical sciences 71(8) (2016) 1102–1108. https://www.ncbi.nlm.nih.gov/pubmed/26916339https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5007616/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Campbell AJ, Busby WJ, Robertson MC, Lum CL, Langlois JA, Morgan FC, Disease, impairment, disability and social handicap: a community based study of people aged 70 years and over, Disabil Rehabil 16(2) (1994) 72–9. [DOI] [PubMed] [Google Scholar]
- [3].Montero-Odasso M, Schapira M, Varela C, Pitteri C, Soriano ER, Kaplan R, et al. , Gait velocity in senior people. An easy test for detecting mobility impairment in community elderly, The journal of nutrition, health & aging 8(5) (2004) 340–3. [PubMed] [Google Scholar]
- [4].Tinetti ME, Speechley M, Ginter SF, Risk factors for falls among elderly persons living in the community, The New England journal of medicine 319(26) (1988) 1701–7. https://www.ncbi.nlm.nih.gov/pubmed/3205267. [DOI] [PubMed] [Google Scholar]
- [5].Beauchet O, Annweiler C, Dubost V, Allali G, Kressig RW, Bridenbaugh S, et al. , Stops walking when talking: a predictor of falls in older adults?, European journal of neurology : the official journal of the European Federation of Neurological Societies 16(7) (2009) 786–95. https://www.ncbi.nlm.nih.gov/pubmed/19473368. [DOI] [PubMed] [Google Scholar]
- [6].Verghese J, Wang C, Lipton RB, Holtzer R, Motoric cognitive risk syndrome and the risk of dementia, The journals of gerontology. Series A, Biological sciences and medical sciences 68(4) (2013) 412–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Verghese J, Wang C, Lipton RB, Holtzer R, Xue X, Quantitative gait dysfunction and risk of cognitive decline and dementia, J Neurol Neurosurg Psychiatry 78(9) (2007) 929–35. https://www.ncbi.nlm.nih.gov/pubmed/17237140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Vermeulen J, Neyens JC, van Rossum E, Spreeuwenberg MD, de Witte LP, Predicting ADL disability in community-dwelling elderly people using physical frailty indicators: a systematic review, BMC geriatr 11(1) (2011) 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Verghese J, Holtzer R, Lipton RB, Wang C, Quantitative gait markers and incident fall risk in older adults, The journals of gerontology. Series A, Biological sciences and medical sciences 64(8) (2009) 896–901. https://www.ncbi.nlm.nih.gov/pubmed/19349593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons, J Am Geriatr Soc 59(1) (2011) 148–57. [DOI] [PubMed] [Google Scholar]
- [11].Glaister BC, Bernatz GC, Klute GK, Orendurff MS, Video task analysis of turning during activities of daily living, Gait & posture 25(2) (2007) 289–94. [DOI] [PubMed] [Google Scholar]
- [12].England SE, Verghese J, Mahoney JR, Trantzas C, Holtzer R, Three-level rating of turns while walking, Gait & posture 41(1) (2015) 300–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Thigpen MT, Light KE, Creel GL, Flynn SM, Turning difficulty characteristics of adults aged 65 years or older, Phys Ther 80(12) (2000) 1174–87. [PubMed] [Google Scholar]
- [14].Cummings SR, Nevitt MC, Non-skeletal determinants of fractures: the potential importance of the mechanics of falls. Study of Osteoporotic Fractures Research Group, Osteoporos Int 4 Suppl 1 (1994) 67–70. [DOI] [PubMed] [Google Scholar]
- [15].Lipton RB, Katz MJ, Kuslansky G, Sliwinski MJ, Stewart WF, Verghese J, et al. , Screening for dementia by telephone using the memory impairment screen, Journal of the American Geriatrics Society 51(10) (2003) 1382–1390. <Go to ISI>://WOS:000185535900006. [DOI] [PubMed] [Google Scholar]
- [16].Holtzer R, Verghese J, Wang C, Hall CB, Lipton RB, Within-person across-neuropsychological test variability and incident dementia, JAMA 300(7) (2008) 823–30. https://www.ncbi.nlm.nih.gov/pubmed/18714062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Holtzer R, Yuan J, Verghese J, Mahoney JR, Izzetoglu M, Wang C, Interactions of Subjective and Objective Measures of Fatigue Defined in the Context of Brain Control of Locomotion, The journals of gerontology. Series A, Biological sciences and medical sciences (2016). https://www.ncbi.nlm.nih.gov/pubmed/27567110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Ayers EI, Tow AC, Holtzer R, Verghese J, Walking while talking and falls in aging, Gerontology 60(2) (2014) 108–13. https://www.ncbi.nlm.nih.gov/pubmed/24192342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Luukinen H, Koski K, Laippala P, Kivela SL, Predictors for recurrent falls among the home-dwelling elderly, Scand J Prim Health Care 13(4) (1995) 294–9. [DOI] [PubMed] [Google Scholar]
- [20].Montero-Odasso M, Schapira M, Soriano ER, Varela M, Kaplan R, Camera LA, et al. , Gait velocity as a single predictor of adverse events in healthy seniors aged 75 years and older, Journals of Gerontology Series A-Biological Sciences & Medical Sciences 60(10) (2005) 1304–9. [DOI] [PubMed] [Google Scholar]
- [21].Verghese J, Wang C, Allali G, Holtzer R, Ayers E, Modifiable Risk Factors for New-Onset Slow Gait in Older Adults, Journal of the American Medical Directors Association 17(5) (2016) 421–5. https://www.ncbi.nlm.nih.gov/pubmed/26923472. [DOI] [PubMed] [Google Scholar]
- [22].Gibson MJ, Andres RO, Isaacs B, Radebaugh T, Wormpetersen J, The Prevention of Falls in Later Life - a Report of the Kellogg-International-Work-Group on the Prevention of Falls by the Elderly, Danish Medical Bulletin 34(4) (1987) 1–24. <Go to ISI>://WOS:A1987H254100001. [PubMed] [Google Scholar]
- [23].Cummings SR, Nevitt MC, Kidd S, Forgetting falls. The limited accuracy of recall of falls in the elderly, J Am Geriatr Soc 36(7) (1988) 613–6. https://www.ncbi.nlm.nih.gov/pubmed/3385114. [DOI] [PubMed] [Google Scholar]
- [24].Verghese J, Buschke H, Viola L, Katz M, Hall C, Kuslansky G, et al. , Validity of divided attention tasks in predicting falls in older individuals: a preliminary study, J Am Geriatr Soc 50(9) (2002) 1572–6. https://www.ncbi.nlm.nih.gov/pubmed/12383157. [DOI] [PubMed] [Google Scholar]
- [25].Krishnamurthy M, Verghese J, Gait characteristics in nondisabled community-residing nonagenarians, Arch Phys Med Rehabil 87(4) (2006) 541–5. http://www.ncbi.nlm.nih.gov/pubmed/16571395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Hausdorff JM, Rios DA, Edelberg HK, Gait variability and fall risk in community-living older adults: A 1-year prospective study, Archives of Physical Medicine and Rehabilitation 82(8) (2001) 1050–1056. http://www.sciencedirect.com/science/article/pii/S0003999301632155. [DOI] [PubMed] [Google Scholar]
- [27].Kwon M-S, Kwon Y-R, Park Y-S, Kim J-W, Comparison of gait patterns in elderly fallers and non-fallers, Technol Health Care 26(S1) (2018) 427–436. https://www.ncbi.nlm.nih.gov/pubmed/29758966https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6004957/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Hausdorff JM, Rios DA, Edelberg HK, Gait variability and fall risk in community-living older adults: a 1-year prospective study, Arch Phys Med Rehabil 82(8) (2001) 1050–6. [DOI] [PubMed] [Google Scholar]
- [29].Verghese J, Buschke H, Viola L, Katz M, Hall C, Kuslansky G, et al. , Validity of divided attention tasks in predicting falls in older individuals: a preliminary study.[see comment], Journal of the American Geriatrics Society 50(9) (2002) 1572–6. [DOI] [PubMed] [Google Scholar]


