Dear Editor,
We read with interest the study by Vrsalovic et al. which examined the prognostic value of high-sensitive (hs) troponin in terms of mortality in patients with COVID-19.1 In patients with COVID-19, cardiac injury is not uncommon and may be attributed to ischemic and non-ischemic causes, including myocardial infarction, coronary microvascular ischemia, cytokine storm, viral myocarditis, stress cardiomyopathy, tachyarrhythmia, or pulmonary embolism.2
Based on the frequency and non-specific nature of abnormal troponin results in COVID-19 patients, the American College of Cardiology, advised clinicians to “measure troponin only if the diagnosis of acute myocardial infarction is being considered on clinical grounds”.3 It has been stressed, however, that troponin is not a test solely for myocardial infarction, but it might also be used as a crucial diagnostic and prognostic tool for risk stratification in COVID-19 patients.1 , 2
Vrsalovic et al. meta-analyzed 3 studies (n = 803), all conducted in China, showing that cardiac injury, defined by an increased hs-troponin value, is associated with an adjusted pooled hazard ratio (HR) of 2.5 (95% confidence intervals [CI] 1.5, 4.1) for death.1 This analysis is important because only studies reporting adjusted HR were included. However, some methodological issues should be considered: (i) two of these studies in this meta-analysis recruited subjects from the same department/hospital within similar time periods, which cannot exclude participants’ overlapping,4 , 5 (ii) one of the studies has not been subjected to peer-review,6 (iii) the evidence appears to be preliminary and emerging.
We performed an updated systematic review using the following algorithm search strategy in PubMed: (“coronavirus 2019” OR “2019-nCoV” OR “SARS-CoV-2” OR “COVID-19”) AND (death OR prognos* OR mortality OR outcome) AND (troponin OR “cardiac injury”) until May 30, 2020. Hand search for eligible articles through the reference list of relevant articles was also performed. Inclusion criteria included full-text articles in English that reported adjusted HR for cardiac injury, defined by increased hs-troponin values, in terms of mortality among patients with COVID-19. In case of studies conducted in the same hospital and the same period, we attempted to clarify overlapping by communicating with the corresponding authors. As the latter was unsuccessful, the study with the largest sample was considered for inclusion. HR and 95% CI values were logarithmically transformed and standard errors were calculated from these values and used in the analysis. Heterogeneity was assessed by the Cochran Q statistic. A p value <0.1 was considered to indicate significant heterogeneity and random-effects model of analysis was used. Meta-analysis was performed using the Stata/ SE 11.2 (Texas) software.
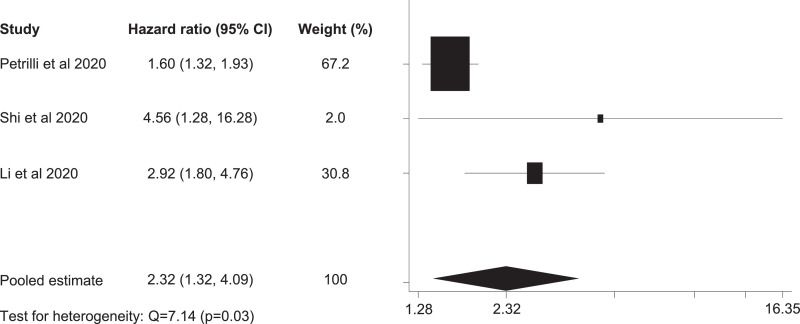
Among 94 articles initially identified, 3 studies fulfilled the inclusion criteria (Table 1 ).7, 8, 9 There was heterogeneity among these studies in defining cardiac injury (Table 1). In one study HR were given for 2 groups of increased troponin versus reference and these were pooled to a study-unique HR. A meta-analysis of these studies (n = 3956) revealed a pooled adjusted HR 2.3 (95% CI 1.3, 4.1) (Fig. 1 ). It is important to mention that adjustment in the models of these studies was performed for several factors, including comorbidities and/or vital signs and laboratory results.
Table 1.
Main characteristics and key results of 3 studies included in meta-analysis.
| Study | City, Country | N | Age (ys), median (IQR) | Cardiac injury definition | Adjusted hazard ratio for mortality (95% CI) |
|---|---|---|---|---|---|
| Petrilli et al.7 | NY, USA | 2737 | 63 (51–74) | Admission troponin I | 1.6 (1.3, 1.9)* |
| >0.1 ng/mL | |||||
| Shi et al.8 | Wuhan, China | 671 | 63 (50–72) | Admission troponin I | 4.6 (1.3, 16.3) |
| >0.026 ng/mL | |||||
| Li et al.9 | Wuhan, China | 548 | 60 (48–69) | Troponin I | 2.9 (1.8, 4.8) |
| >0.0156 ng/mL |
pooled estimate.
Fig. 1.
Forest plot of adjusted hazard ratios for mortality associated with cardiac injury in patients with COVID-19.
Evidence regarding the natural course of the COVID-19 is rapidly evolving, calling for immediate translation into clinical practice during the pandemic. The available data from China and US are preliminary but important. Meta-analysis of the current evidence suggests that cardiac injury defined by elevated hs-troponin has independent adverse prognostic value in COVID-19. Further research is needed to confirm the independent prognostic value of hs-troponin and investigate the pathogenetic mechanisms of cardiac injury in COVID-19 and its impact on mortality. Whether an increased hs-troponin is due to direct cardiac effects of the SARS-CoV-2, or indirect injury induced by the cytokine storm remains unclear. However, physicians should be aware that an increased value of hs-troponin might be useful in risk stratification of COVID-19 patients and should therefore be included in routine assessment.
Declaration of Competing Interest
The authors declare no conflict of interest.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Vrsalovic M., Vrsalovic Presecki A. Cardiac troponins predict mortality in patients with COVID-19: a meta-analysis of adjusted risk estimates. J Infect. 2020;19 doi: 10.1016/j.jinf.2020.05.022. S0163-4453(20)30300-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chapman A.R., Bularga A., Mills N.L. High-sensitivity cardiac troponin can be an ally in the fight against COVID-19. Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.047008. [DOI] [PubMed] [Google Scholar]
- 3.https://www.acc.org/latest-in-cardiology/articles/2020/03/18/15/25/troponin-and-bnp-use-in-covid19. Last accessed May 30, 2020.
- 4.Shi S., Qin M., Shen B., Cai Y., Liu T., Yang F. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan. China. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang L., He W., Yu X., Hu D., Bao M., Liu H. Coronavirus disease 2019 in elderly patients: characteristics and prognostic factors based on 4-week follow-up. J Infect. 2020 doi: 10.1016/j.jinf.2020.03.019. pii: S0163-4453(20)30146-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang F., Yang D., Li J. Myocardial injury is associated with in – hospital mortality of confirmed or suspected COVID - 19 in Wuhan, China: a single center retrospective cohort study. MedRxiv. 2020;17 doi: 10.1101/2020.03.21.20040121. [DOI] [Google Scholar]
- 7.Petrilli C.M., Jones S.A., Yang J., Rajagopalan H., O'Donnell L., Chernyak Y. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 2020;369:m1966. doi: 10.1136/bmj.m1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shi S., Qin M., Cai Y., Liu T., Shen B., Yang F. Characteristics and clinical significance of myocardial injury in patients with severe coronavirus disease 2019. Eur Heart J. 2020 doi: 10.1093/eurheartj/ehaa408. ehaa408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li X., Xu S., Yu M., Wang K., Tao Y., Zhou Y. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol. 2020 doi: 10.1016/j.jaci.2020.04.006. S0091-6749(20)30495-4. [DOI] [PMC free article] [PubMed] [Google Scholar]