Highlights
-
•
49% of 543 survey participants worked full-time from home during the COVID-19 pandemic.
-
•
Perceived productivity was lower, with associated feelings of guilt.
-
•
Anxiety and depressive symptoms were higher than normative values in Europe.
-
•
Anxiety symptoms were negatively correlated with the number of years in research.
-
•
Mental health symptoms were lower in participants with institutional health support.
Keywords: COVID-19, Isolation, Mental health, HADS, Research
Abstract
Introduction
With the COVID-19 pandemic, individuals have been forced to follow strict social isolation guidelines. While crucial to control the pandemic, isolation might have a significant impact on productivity and mental health. Especially for researchers working in healthcare, the current situation is complex. We therefore carried out a survey amongst researchers in the field of radiation oncology to gain insights on the impact of social isolation and working from home and to guide future work.
Materials and methods
An online survey was conducted between March 27th and April 5th, 2020. The first part contained 14 questions intended to capture an overview of the specific aspects related to research while in isolation. The second (optional) part of the questionnaire was the validated Hospital Anxiety and Depression Scale (HADS), a self-reported measure used to assess levels of anxiety and depressive symptoms.
Results
From 543 survey participants, 48.8% reported to work full-time from home. The impact on perceived productivity, with 71.2% of participants feeling less productive, caused 58% of participants to feel some level of guilt.
Compared to normative data, relatively high levels of anxiety and depressive symptoms were recorded for the 335 participants who filled out the HADS questionnaire. Group comparisons found the presence of a supportive institutional program as the sole factor of statistical significance in both anxiety and depressive symptom levels. People having to work full-time on location showed higher depressive symptom levels than those working from home. Anxiety scores were negatively correlated with the number of research years.
Conclusion
Results of the survey showed there is a non-negligible impact on both productivity and mental health. As the radiation oncology research community was forced to work from home during the COVID-19 pandemic, lessons can be learned to face future adverse situations but also to improve work-life balance in general.
1. Introduction
With the outbreak and spread of the Severe Acute Respiratory Syndrome CoronaVirus 2 (SARS-CoV-2), the virus responsible for Coronavirus disease 2019 (COVID-19), an unprecedented scenario took hold of every aspect of our life.
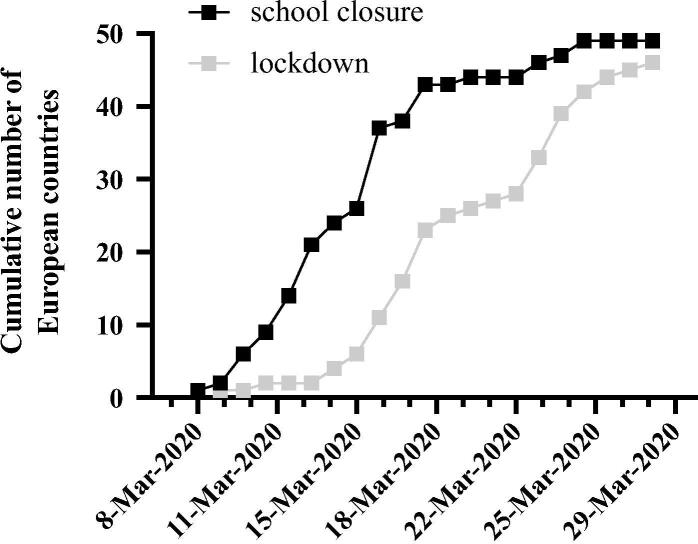
The World Health Organisation (WHO) designated COVID-19 as a public health emergency on January 30th, 2020 and as a pandemic on March 11th [1], [2]. Two days earlier, on March 9th, the Italian government declared the entire country in ‘lockdown’, restricting its citizens to home-confinement and closing its borders and airports to all non-essential travel [3]. Soon, other European countries followed with a partial or full lockdown (Fig. 1). Most countries, including those who refrained from lockdown, imposed strict social distancing and isolation guidelines requiring people to work from home whenever possible. Often, this was installed from one day to another with citizens having to adapt in a matter of hours.
Fig. 1.
Cumulative number of European countries implementing COVID-19 related measures over a time span between March 8th and 29th. Dates indicate the moment measures were implemented. School closure is defined as a nationwide closure of either (pre-)elementary school, high school or university. Lockdown is defined as home-confinement, closing the borders or airports to all non-essential travel. Survey results were gathered from the 29th of March to the 5th of April 2020.
In early March, the WHO emphasized the need to “stop, contain, control, delay and reduce the impact of this virus at every opportunity” [4]. While the control of the pandemic and the safety and continuity of healthcare programs are primary concerns, it is also important to minimize the indirect impact on people forced to work from home. Isolation, while crucial to keep the spread of SARS-CoV-2 under control, can have a significant impact on physical and mental health [5]. In a large systematic review, it was found that across the general population, actual and perceived isolation is as strongly associated with increased risk for early mortality as smoking [6].
As academia is already associated with high pressure and expectations on productivity, the isolation measures might have a non-negligible impact on researchers, who often rely on time-limited funding or have to deliver scientific output under strict deadlines [7]. Technological developments have facilitated remote working for most researchers. However, having it imposed as the main or sole mode of work at short notice may have a negative impact on productivity and mental health, as the creativity of research benefits from interactions between group members and with collaborators in other institutes or in the industry. Researchers with university affiliations might have seen their teaching workload increase as classes had to suddenly be transferred to online formats. Laboratory researchers might have lost access to their labs especially if these were located in COVID-hospitals [8]. Gathering patient data, e.g. for clinical trials, became more difficult if not impossible. Researchers with clinical training might have become fully occupied with clinical duties or even be transferred to other services to directly treat COVID-19 patients. This might have also hindered research continuity for those remaining at home, as interaction with colleagues still involved in patient care has to be avoided. Especially for researchers working in healthcare, the current situation is complex. While some studies found traumatization to be higher in the public than in healthcare personnel involved in treating patients infected with COVID-19, other studies report direct contact with COVID-19 as a predictive factor for increased psychological distress [9], [10], [11], [12], [13].
Radiation oncology is a highly interdisciplinary field, with researchers having various backgrounds such as radiobiology, medical physics, computer science and/or clinical studies. Therefore, it is difficult to predict the impact of the COVID-19 pandemic and related measures on their mental health and we hypothesise that the very different personal circumstances may result in different effects and coping mechanisms. In particular, we hypothesized that three groups experienced substantial negative impact of the current pandemic on their mental health: a) researchers in training, such as PhD students with strict deadlines, b) those still involved in clinical duties confronted with the crisis situation in healthcare, and c) those completely isolated at home.
We therefore carried out a survey amongst researchers in the field of radiation oncology, including a validated anxiety and depressive symptoms test, with the aim to assess the impact of social isolation and working from home on mental health and to identify possible high-risk groups to guide future work in mitigating this impact.
2. Materials and methods
An online survey was disseminated amongst researchers in the field of radiation oncology between March 27th and April 5th, 2020 (see supplementary material). Participants were invited via email using the European SocieTy for Radiotherapy and Oncology (ESTRO) membership database (3850 recipients), social media, national radiation oncology societies and their young member working groups and personal networks. The survey platform restricted survey participation to one per device, limiting the chance of multiple participations per person.
The questionnaire was anonymous and consisted of two parts. The first part contained 14 questions intended to capture an overview of the specific aspects related to research while in isolation. Aspects such as family duties, caring for oneself or loved ones affected by the disease or other aspects that affect the general population in a similar manner were not specifically surveyed but participants could include this in free-text responses. The second (optional) part of the questionnaire was the Hospital Anxiety and Depression Scale (HADS) [14], [15]. The HADS is a self-reported measure used to assess psychological distress in both clinical and non-clinical populations. It includes 14 items representing two subscales: anxiety (HADS-A) and depression (HADS-D). Each subscale consists of 7 items rated on a 0–3 scale, with the total score ranging from 0 to 21. For both scales, a score of 8 or more suggests a clinically significant level of depressive/anxiety symptoms. The HADS has shown good concurrent validity, test–retest reliability, and internal consistency (Cronbach’s alphas ranging from 0.82 to 0.90) [16].
Statistical analyses of the survey results were carried out with the Statistical Package for Social Science, version 26.0 (IBM SPSS Statistics for Windows, Armonk, NY, USA). Indices of asymmetry and kurtosis were used to test for normality of the data. Values for asymmetry and kurtosis between –1 and + 1 were considered acceptable to prove normal univariate distribution. Comparisons between the different group variables on anxiety/depression scores were performed by means of a t-tests or one-way Analysis of Variance (ANOVA), as appropriate. The effect size was determined by calculating Cohen’s d or partial eta-squared (η2). Spearman’s rank-order correlations were run to evaluate the possible relationships between ordinal variables extracted from the first part of the survey and the HADS scores.
Additional comparisons were performed to investigate the possible presence of group differences, considering only those participants who scored above the clinical significance cut-off point (≥8). A p-value < 0.05 was considered statistically significant.
3. Results
From the survey, 543 participants were identified as researchers working in the field of radiation oncology with varying levels of experience, field of research and additional duties besides research (Table A1). At the time of answering the survey, participants were working in 45 different countries of which the large majority (85.7%) was located in Europe (Table A2). Most of the participants worked from home full-time (48.8%) or part-time (26.5%) while 24.7% worked full-time on location (hospital, laboratory or office). Many participants made use of digital communication to stay in contact with either family and friends (76.3%) or colleagues (68.4%), while 4% of participants replied to have little or no contact with anyone.
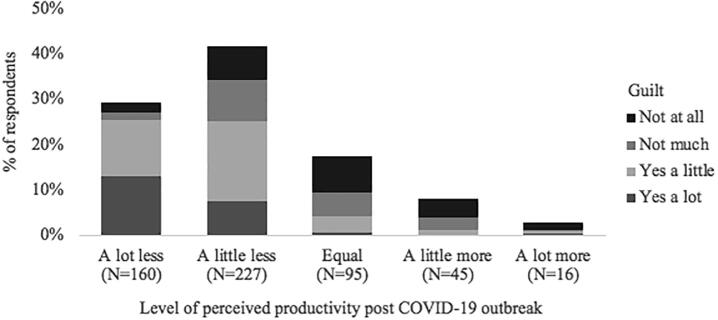
The survey showed that the outbreak of COVID-19 had an impact on perceived productivity, with 71.2% of participants feeling either a lot or a little less productive than pre-pandemic, while 11.2% responded that they felt a little or a lot more productive. The feeling of guilt associated with the participants’ perceived change in productivity is illustrated in Fig. 2, with a little or a lot of guilt being more abundant when productivity declined.
Fig. 2.
Level of perceived productivity (Q8) compared to pre-COVID-19 outbreak, together with the participants’ feeling of guilt around productivity (Q9).
Participants were asked which measures they took to cope with isolation and if these measures helped. Exercise at home and online social interactions with friends/family or with colleagues were the most popular answers, especially among participants who said the measures helped a lot (Fig. 3). Other measures entered by participants in a free-text field included creative and artistic hobbies, reading, films, video games, music and cooking (5.3% of all the participants) or spending time with family (4.4%). Although not explicitly asked, five participants (1%) wrote that they had more time with family in the current situation. Outdoor activities, meditation, yoga, relaxation and self-care as well as housework/gardening were also entered by participants. Only 5% of the participants said these measures did not help.
Fig. 3.
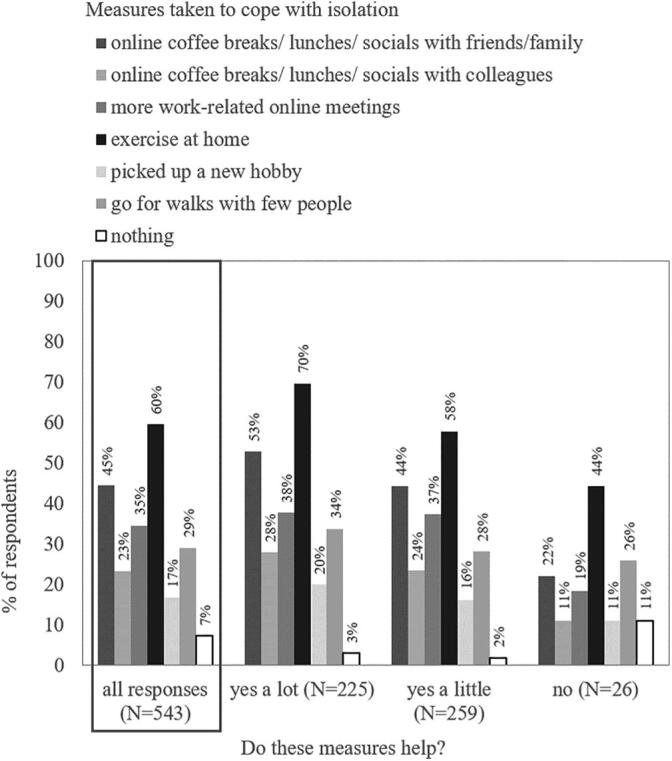
Percentage of participants who take certain measures to cope with isolation (Q13) overall and grouped by effect (Q14). (33 participants did not grade the effect of the measures).
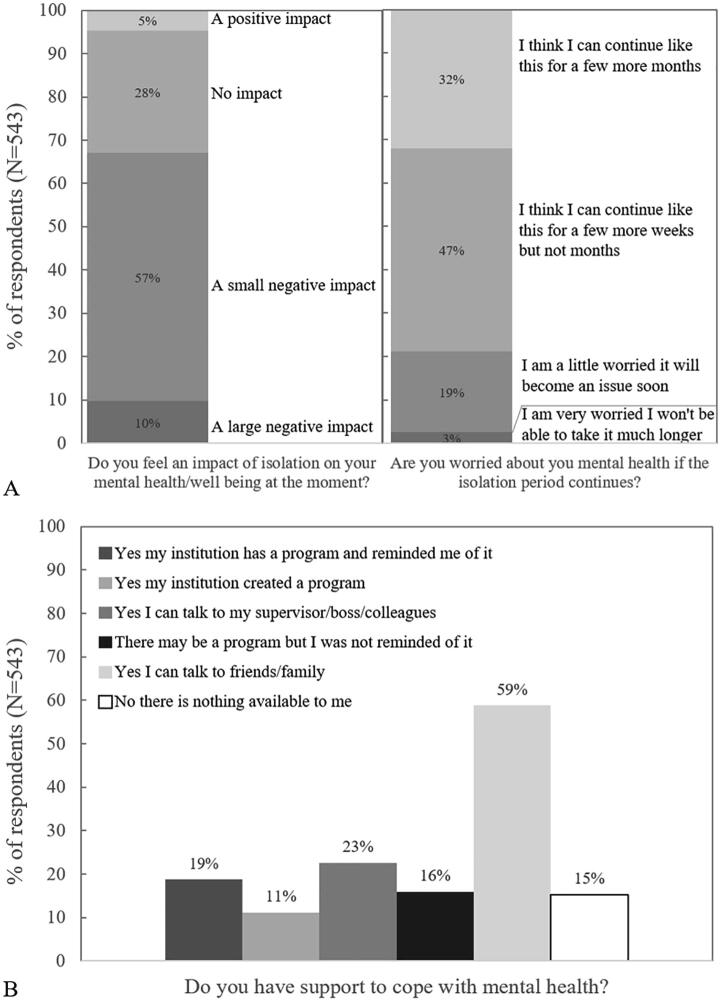
Despite the measures, over half of the participants (67%) declared that they felt isolation had a negative impact on their mental health while 5% said it had a positive one. Further, 21% of participants were worried it would become an issue soon or very soon while only 32% said they thought they could continue in isolation for a few more months or longer (Fig. 4A). A majority of participants said they could talk to friends and family to cope with mental health issues. Institutional programs existed or were recently created for 19% and 11% of participants respectively. However, 15% of the participants said there was no form of mental health support available to them within their institutes (Fig. 4B).
Fig. 4.
Self-assessed impact of isolation on mental health (top) and available means to cope with mental health problems (bottom).
Of the 543 participants, 335 (61.7%) completed the HADS questionnaire (part 2) of the survey. All variables included in the analyses were normally distributed according to the criteria mentioned earlier (kurtosis values ranging from −0.829 to + 0.508; asymmetry values ranging from + 0.128 to + 0.957). The Cronbach’s alpha values in our sample were α = 0.84 (HADS-A) and α = 0.78 (HADS-D). A detailed overview of the statistical analysis results can be found in Appendix A.
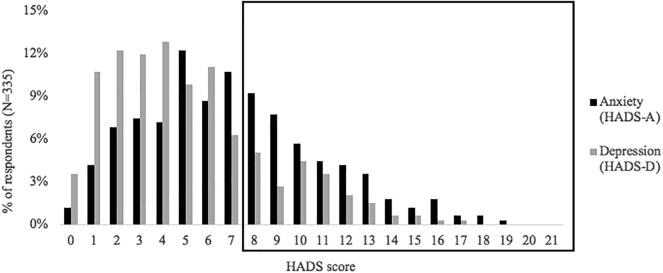
From a descriptive point of view, 41% and 21% of participants reported a clinically relevant level of anxiety symptoms (HADS-A ≥ 8) and depressive symptoms (HADS-D ≥ 8), respectively (Fig. 5). Overall, participants reported higher levels of anxiety symptoms than depressive symptoms (HADS-A vs. HADS-D, mean ± SD: 7.02 ± 3.90 vs. 5.02 ± 3.46, p < .001).
Fig. 5.
Distribution of HADS-A and HADS-D scores of all 335 participants. Scores for participants with a clinically significant level of depression/anxiety symptoms (HADS score ≥ 8) are in the black box.
Group comparisons on both HADS-A and HADS-D scores to identify possible high-risk groups or causes for increased anxiety and/or depressive symptoms are summarized in Table 1. As ANOVA showed no significant difference between part-time and full-time work from home, the two groups work at home (part- or full-time) and work on location (full-time) were compared using t-test. Regarding group comparisons on both the levels of anxiety and depressive symptoms, a univariate ANOVA showed the presence of significant differences between participants who had support from institution programs vs. participants who had support from colleagues/family/friends vs. participants who had no support at all (HADS-A: mean ± SD: 6.30 ± 3.85 vs. 7.12 ± 3.82 vs. 7.81 ± 4.03; p = .038, HADS-D: mean ± SD: 4.29 ± 3.02 vs. 4.80 ± 3. 32 vs. 6.56 ± 4.06; p < .001). Particularly, post-hoc tests revealed a statistically significant difference between people who received support from institution programs and people who had no support. Regarding group differences on depressive symptom scores only, results of t-tests showed the presence of significant differences between participants who have virtual or non-virtual contacts with colleagues/friends/family vs. no contact at all (mean ± SD: 4.97 ± 3.42 vs. 7.57 ± 4.39; p = .049), and between participants who work on location vs. from home (mean ± SD: 5.94 ± 4.23 vs. 4.75 ± 3.14; p = .024). For all other group comparisons, no significant differences were detected on either the HADS-A or HADS-D scores (Appendix A).
Table 1.
Group comparisons for HADS-A and HADS-D.
| Number (%) | HADS-Amean ± SD | p | HADS-Dmean ± SD | p | |
|---|---|---|---|---|---|
| PhD students | 79 (23.6) | 7.32 ± 4.51 | 0.490 | 5.04 ± 3.80 | 0.967 |
| Other professionals | 256 (76.4) | 6.93 ± 3.70 | 5.02 ± 3.35 | ||
| In training* | 119 (35.5) | 7.47 ± 4.25 | 0.134 | 5.31 ± 3.97 | 0.292 |
| Not in training | 216 (64.5) | 6.77 ± 3.68 | 4.87 ± 3.14 | ||
| Clinical duties | 162 (48.4) | 6.88 ± 3.61 | 0.513 | 5.24 ± 3.63 | 0.267 |
| No clinical duties | 173 (51.6) | 7.16 ± 4.16 | 4.82 ± 3.28 | ||
| Work at home† | 257 (76.7) | 7.50 ± 4.15 | 0.216 | 4.75 ± 3.14 | 0.024 |
| Work at office | 78 (23.3) | 6.88 ± 3.82 | 5.94 ± 4.23 | ||
| Support | |||||
| from institution | 101 (30.1) | 6.30 ± 3.85 | 0.038 | 4.29 ± 3.02 | <0.001 |
| from family/friends only | 162 (48.4) | 7.12 ± 3.82 | 4.80 ± 3. 32 | ||
| no support | 72 (21.5) | 7.81 ± 4.03 | 6.56 ± 4.06 | ||
| Virtual / non-virtual contact | 328 (97.9) | 7.02 ± 3.92 | 0.934 | 4.97 ± 3.42 | 0.049 |
| No contact | 7 (2.1) | 7.14 ± 2.97 | 7.57 ± 4.39 | ||
| Coping measures | 311 (92.8) | 7.06 ± 3.90 | 0.498 | 5.00 ± 3.34 | 0.707 |
| No coping measures | 24 (7.2) | 6.50 ± 3.96 | 5.38 ± 4.79 |
*MSc students + PhD students + MD residents + MD or Medical Physicist in training. †full-time + part-time at home. Results in bold indicate a statistically significant difference.
Based on Spearman’s rank-order correlation analysis, results showed the presence of significant and negative associations between anxiety symptoms and years of research experience (rs(3 3 3) = -0.148, p = .007), and between anxiety/depressive symptoms and the perceived productivity levels after COVID-19 outbreak (HADS-A: rs(3 3 3) = -0.112, p = .40; HADS-D: rs(3 3 3) = -0.235, p < .001). Significant positive correlations were found, instead, between anxiety/depressive symptoms and the feeling of guilt about current productivity levels (HADS-A: rs(3 3 3) = 0.312, p < .001; HADS-D: rs(3 3 3) = 0.334, p < .001), the negativity of the self-perceived impact of isolation on mental health (HADS-A: rs(3 3 3) = 0.384, p < .001; HADS-D: rs(3 3 3) = 0.411, p < .001) and the worry about mental health in case of prolonged isolation (HADS-A: rs(3 3 3) = 0.402, p < .001; HADS-D: rs(3 3 3) = 0.441, p < .001).
Next, we considered only participants who presented with a clinically significant level of anxiety or depressive symptoms (HADS-A/D ≥ 8). Regarding anxiety symptoms, results of t-tests showed the presence of significant differences on the HADS-A scores between PhD students (n = 35) vs. other professionals (n = 103) (mean ± SD: 11.57 ± 2.79 vs. 10.53 ± 2.56; p = .045). As far as depressive symptoms are concerned, results of t-tests showed the presence of significant differences on the HADS-D scores between participants who are in training (n = 31) vs. not in training (n = 40) (mean ± SD: 11.03 ± 2.36 vs. 9.93 ± 1.81; p = .029), and between participants who have virtual or non-virtual contacts with colleagues/friends/family (n = 69) vs. no contact at all (n = 2) (mean ± SD: 10.32 ± 2.08 vs. 13.50 ± 2.12; p = .036). For all other group comparisons, no significant differences were detected on either the HADS-A or HADS-D scores (p-values > 0.05).
4. Discussion
A survey among researchers in the field of radiation oncology was carried out during one of the early weeks of the COVID-19 pandemic, when isolation measures had been installed for a maximum of 3 weeks, depending on the country. At the time of data collection, the total duration of the lockdown measures was unknown in most countries but expected to last for several months. The survey gathered a total of 543, of which 335 filled-in the included HADS questionnaire. The aim was to gain insight into the impact of the current COVID-19 pandemic and isolation measures on productivity and mental health in this population. We hypothesized that three groups may experience substantial negative impact of the current pandemic on their mental health: a) researchers in training, such as PhD students with strict deadlines, b) those still involved in clinical duties confronted with the crisis situation in healthcare, and c) those completely isolated at home.
Several European studies have gathered normative HADS data which can be used as a benchmark. Mean normative anxiety scores range from 3.9 to 6.4, with most studies reporting higher anxiety in women. Mean normative depressive symptom scores are more homogeneous, ranging between 3.0 and 3.7, with a maximum of 4.0 reported by a Swedish study and several studies reporting a positive trend between depressive symptoms and age [17], [18], [19]. Compared to these normative data, relatively high levels of anxiety and depressive symptoms were recorded in the present study, with mean ± SD scores over all participants of 7.02 ± 3.90 for anxiety and 5.02 ± 3.46 for depressive symptoms. Furthermore, a significant number of individuals reported a clinically relevant level of anxiety (41%) and of depressive (21%) symptoms. A limitation is that participants were not asked about gender or age and so stratification based on these factors was not possible. Another limitation is the lack of assessment of pre-existing mental or somatic health issues in the studied population prior to the COVID-19 pandemic and no baseline levels for the pre-pandemic period were recoded for similar populations. Therefore, the higher levels of anxiety and depressive symptoms in our sample may be due to several factors other than the pandemic. Nevertheless, the majority of participants (67%) reported feeling a negative impact of isolation on their mental health, which was correlated with the HADS scores; while 22% indicated to be a little or very worried about their mental health in case of prolonged isolation. This points to the interpretation that the pandemic had an effect on the level of anxiety and depression in our population.
Our results also indicate that the current unprecedented circumstances have a significant impact on perceived productivity, with most participants (71.1%) feeling less productive. Moreover, this change in perceived productivity causes more than half the participants (58%) to feel some level of guilt. Both these indirect consequences of the current pandemic were found to be associated with the participants’ levels of anxiety (HADS-A) and depressive symptoms (HADS-D). Based on these findings, (academic) institutions are encouraged to acknowledge human limitations in a time of crisis and support the mental health of their researchers. The presence of a supportive institutional program was found to be the sole factor of statistical significance in both anxiety and depressive symptom levels, and so creating such a program and/or reminding researchers of its existence may help reduce the risk of anxiety and depressive disorders among researchers. Early intervention measures should be taken to alleviate the psychological issues and avoid long-term consequences such as burn-out [20].
Generally speaking, whenever trying to specifically address the potential sources of anxiety and fear, it is more important and valuable to focus on addressing the specific concerns, rather than teaching generic approaches to manage stress reduction or enhance resilience [13]. It is considered useful to investigate what people are concerned about, what type of message and indication they feel they need from their leaders, and which could be other tangible sources of support of which they believe they could mostly take advantage. As the field of radiation oncology is highly interdisciplinary, concerns and helpful support are likely to be quite diverse and require further investigation.
Significantly higher depressive symptom levels were observed in participants who are still required to work full-time on location compared to those working full- or part-time from home, indicating that isolation is likely not the main contributor to increased depressive symptom levels. With a mean HADS-D score of 5.94 ± 4.23, participants required to work full-time on location are well above reported normative values for depressive symptoms (range: 3–4). Several factors could serve as an explanation such as fear of contamination, fear of contaminating family members or a high exposure to critically ill patients, though clinical duties were no indicator for increased anxiety nor depressive symptoms. The exact ratio of time spent working at home vs. on location was not requested. This encourages additional investigation in the relationship between the ratio of time spent working at home vs on location and HADS scores. It is important to observe that one of the mechanisms by which isolation may have an impact on the psychological aspects of an individual is through the role of loneliness as a mediator. This has been demonstrated, for example, in older adults, where the effect of social isolation on cognitive function decline was found to be influenced by the indirect effect of loneliness [21]. This means that, even if constrained within a context of isolation, if a person can maintain social relations and cope with feelings of loneliness, this can potentially mitigate the impact on mental health. In this sense, technology can be very helpful to help researchers feel connected despite isolation [22].
Despite the generally negative impact of isolation on mental health, 5% of respondents said that isolation had a positive impact on their mental health. Notably, some participants noted having more time to spend with their family or for self-care. More time at home instead of commuting and the additional flexibility may positively balance the effects of isolation [23]. Working from home is also likely beneficial for people having a toxic professional environment [24]. Just over 20% of the respondents to the Nature PhD survey reported experiencing harassment and discrimination at the workplace [8]. In circumstances other than a global pandemic, allowing more flexibility and remote working may help bridge the gender gap, especially for early-career researcher [25].
Several group comparisons on both HADS-A and HADS-D scores were performed in this study to identify possible high-risk groups based on our hypothesis. Obtaining a PhD or a higher education degree is a once-in-a-lifetime experience and achievement and although it can be a very rewarding experience, PhD students experience particularly high levels of psychological distress, including depressive and anxiety symptoms. In fact, over a third of the participants to the Nature 2019 PhD survey have sought help for depression and anxiety, and only 26% of them were satisfied with the help received from their institutions [8]. In our study, the overall levels of anxiety and depressive symptoms were not statistically different for PhD students and non-PhD students or in-training members vs non-in-training members. However, the years of research experience was found to be correlated with anxiety and when considering only participants with a clinically significant level of anxiety or depressive symptoms, indications were found that the severity of the symptoms was higher in PhD students (anxiety score) or in-training participants (depression score) compared to non-PhD students or non-in-training participants, respectively. Given the small number of participants in this sub-analysis compared to the overall prevalence analysis, these results should be interpreted with caution and confirmed in a larger cohort.
The work conducted in this study was an initial impact assessment of the current pandemic and isolation regulations on the productivity and mental health of researchers working in radiation oncology. 543 invitees responded to the survey in the relatively short timeframe of one week, representing a snapshot of a very dynamic situation that followed different time courses per country. The number of respondents (5 4 3) can be compared to the ESTRO membership database (3850 members), however, other channels were used to promote the survey as well. The survey was only addressed to individuals involved in research. Other possible reasons for not responding include not having the time to respond possibly due to COVID-19 related circumstances, or not seeing its relevance. This could have created a nonresponse bias in the reported results in this manuscript which should be considered when interpreting the results. However, we believe that our sample nonetheless provides important insights into how the radiation oncology research community was affected by the pandemic. A focus group will further investigate the possible underlying causes or consequences of the present results and what constitutes helpful support from institutions. We believe that both this survey and further analysis are relevant for a number of future scenario’s, including global (epidemic) situations but also those which may occur on a smaller or even a personal level such as medium to long-term caring duties or illness, where a researcher or group of researchers has to work from home.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
We would like to thank ESTRO for logistic support and dissemination of the survey, and the participants for taking the time to fill out the questionnaires. We would also like to thank Piotr Krawczyk, MD for his assistance and valuable comments.
Marianne Aznar acknowledges support from Cancer Research UK (grant no C8225/A21133), the Cancer Research UK RadNet Manchester [C1994/A28701] and the NIHR Manchester Biomedical Research Centre. Marianne Aznar is a member of the European Society for Radiotherapy & Oncology (ESTRO) Physics Committee.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ctro.2020.06.006.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.World Health Organization . World Health Organization; 2020. Novel Coronavirus (2019-nCoV): situation report, 10. https://apps.who.int/iris/handle/10665/330775. [Google Scholar]
- 2.World Health Organization . World Health Organization; 2020. Coronavirus disease 2019 (COVID-19): situation report, 51. https://apps.who.int/iris/handle/10665/331475. [Google Scholar]
- 3.Remuzzi A., Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020;395(10231):1225–1228. doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. WHO statement on cases of COVID-19 surpassing 100 000. 2020. https://www.who.int/news-room/detail/07-03-2020-who-statement-on-cases-of-covid-19-surpassing-100-000.
- 5.Rajkumar RP. COVID-19 and mental health: A review of existing literature. Asian J. Psychiatr 2020; 52.n doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed]
- 6.Holt-Lunstad J., Smith T., Baker M. Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspect Psychol Sci. 2015;10(2):227–237. doi: 10.1177/1745691614568352. [DOI] [PubMed] [Google Scholar]
- 7.Woolston C. PhDs: the tortuous truth. Nature. 2019;575(7782):403–406. doi: 10.1038/d41586-019-03459-7. [DOI] [PubMed] [Google Scholar]
- 8.Bardelli A. Coronavirus lockdown: What I learnt when I shut my cancer lab in 48 hours. Nature. 2020 doi: 10.1038/d41586-020-00826-7. [DOI] [PubMed] [Google Scholar]
- 9.Li Z., Ge J., Yang M. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in Covid-19 control. Brain Behav Immun. 2020 doi: 10.1016/j.bbi.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang WR., Wang K., Yin L., et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom 2020; 1-9. doi: https://doi.org/10.1159/000507639. [DOI] [PMC free article] [PubMed]
- 11.Neto MLR., Almeida HG., Esmeraldo JDA., et al. When health professionals look death in the eye: the mental health of professionals who deal daily with the 2019 coronavirus outbreak. Psychiatry Res 2020; 112972. doi: 10.1016/j.psychres.2020.112972. [DOI] [PMC free article] [PubMed]
- 12.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open 2020; 3(3):e203976-e203976. doi:10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed]
- 13.Shanafelt T., Ripp J., Trockel M. Understanding and Addressing Sources of Anxiety Among Health Care Professionals During the COVID-19 Pandemic. JAMA. 2020 doi: 10.1001/jama.2020.5893. [DOI] [PubMed] [Google Scholar]
- 14.Brennan C., Worrall-Davies A., McMillan D. The hospital anxiety and depression scale: a diagnostic meta-analysis of case-finding ability. J Psychosom Res. 2010;69:371–378. doi: 10.1016/j.jpsychores.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 15.Zigmond A.S., Snaith R.P. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 16.Bjelland I., Dahl A.A., Haug T.T., Neckelmann D. The validity of the hospital anxiety and depression scale. An updated literature review. J Psychosom Res. 2002;52:69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 17.Crawford J.R., Henry J.D., Crombie C., Taylor E.P. Normative data for the HADS from a large non-clinical sample. Br J Clin Psychol. 2010;40(4):429–434. doi: 10.1348/014466501163904. [DOI] [PubMed] [Google Scholar]
- 18.Breeman S., Cotton S., Fielding S., Jones G.T. Normative data for the Hospital Anxiety and Depression Scale. Qual Life Res. 2015;24(2):391–398. doi: 10.1007/s11136-014-0763-z. [DOI] [PubMed] [Google Scholar]
- 19.Hinz A., Brähler E. Normative values for the hospital anxiety and depression scale (HADS) in the general German population. J Psychosom Res. 2011;71(2):74–78. doi: 10.1016/j.jpsychores.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 20.Brooks S.K., Webster R.K., Smith L.E. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yang R., Wang H., Edelman L.S. Loneliness as a mediator of the impact of social isolation on cognitive functioning of Chinese older adults. Age Ageing. 2020 doi: 10.1093/ageing/afaa020. [DOI] [PubMed] [Google Scholar]
- 22.Sharma A. Finding community during a pandemic. Science. 2020;368(6487):206. doi: 10.1126/science.368.6487.206. [DOI] [PubMed] [Google Scholar]
- 23.Shepherd-Banigan M., Bell J.F., Basu A. Workplace stress and working from home influence depressive symptoms among employed women with young children. Int J Behav Med. 2016;23(1):102–111. doi: 10.1007/s12529-015-9482-2. [DOI] [PubMed] [Google Scholar]
- 24.Unicef. Social stigma associated with the coronavirus disease (COVID-19). 2020. https://www.unicef.org/documents/social-stigma-associated-coronavirus-disease-covid-19.
- 25.McCarthy H. Working at home: The key to gender equality? British Academy Review 2018; (BAR). 33.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.