Abstract
The brachial artery is the most common injured vessel in the upper extremity. Although vascular injury following blunt trauma is rare, it is a condition to be considered because it can easily be overlooked unless the clinician has a high suspicion. In this paper, we present a blunt trauma case with brachial arterial injury, upper extremity ischemia, and the need for urgent management to salvage the limb. A 28-year-old male had a right arm swelling, pain, and paleness accompanied by a weak pulse in the right radial artery and right-hand numbness. Following resuscitation, preoperative Doppler ultrasound revealed to the brachial artery injury. The right brachial artery had an occlusion with a thrombus. In spectral Doppler analysis, there were demonstrated parvus et tardus waveform in the distal arteries. Doppler ultrasound provided crucial information to make an accurate and rapid management decision.
Keywords: Brachial artery injury, Blunt trauma, Color Doppler
Introduction
Traumatic brachial artery injuries include most of the upper limb artery injuries. This is known to be related to the superficial location of the brachial artery. Although most of the upper limb arterial injuries occur as a result of penetrating trauma, blunt trauma is more likely to cause amputation [1]. Although angiography is the best modality known for the evaluation of arterial injuries, color flow (CF) Doppler ultrasound (US) can be used safely and effectively in the diagnosis because of the superficial location of the brachial artery [2]. In this report, we aimed to present the Doppler US findings of the patient who developed brachial artery thrombosis after blunt trauma.
Case report
A 28-year-old male who had no significant previous medical or family history, he was thrown to the ground when he hit the arm of a heavy construction machine during an accident at the workplace. He was referred to our emergency department. At the time of acceptance, he had an open airway, normal breathing with a respiratory rate of 15 breaths/min, was hemodynamically stable with a pulse rate of 90 beats/minutes, and a blood pressure of 128/70 mmHg. Physical examination revealed swelling and tenderness in the right forearm and arm. There was no palpable brachial artery pulses and accompanied by a weak pulse in the right radial artery. The right forearm was cool to the touch and appeared pale than the left forearm. There was numbness and the sensory loss in the fourth and fifth fingers of the right hand. He was referred to the radiology department for upper extremity US.
We then performed an US evaluation (Canon Aplio 500, Otawara, Japan) using a high-frequency linear array transducer (5-11 MHz). The patient was evaluated in a supine position. Upper limb arteries evaluated in axial and longitudinal sections in gray scale, CF and pulsed-wave (PW) modes in proximal to distal parts. We started evaluation the subclavian artery, moving laterally toward the axillary artery. CF and PW Doppler both identified flow through these arteries. B-mode US that revealed 2 hematomas of 5 × 1.5 cm and 3.5 × 1 cm in size with an internal hyperechoic mass in the right biceps muscle. Also, at the origin of the brachial artery, the arterial lumen was filled with thrombus, which extended distally to the level of the antecubital fossa (Fig. 1). Following CF and PW Doppler assessment did not show blood flow in the brachial artery lumen. Then, an attempt was made to image the right ulnar and radial arteries; however, PW Doppler examination of the radial and ulnar arteries revealed slowed systolic upstroke and reduced systolic peak velocity (parvus et tardus pattern), most likely due to the proximal occlusion (Fig. 2). These findings suggested that there was an acute brachial artery occlusion. The patient was taken to the operating room immediately. Surgical exploration revealed the injury to the brachial artery wall. The traumatized artery segment was resected and the reversed great saphenous vein interposition graft was performed.
Fig. 1.
A 28-year-old male with complete hypoechoic thrombosis in the right brachial artery. B-mode gray scale and color flow doppler ultrasound shows intraluminal thrombus (T) and absence of the flow in the brachial artery (BA), also ultrasound images show soft tissue hematoma (H).
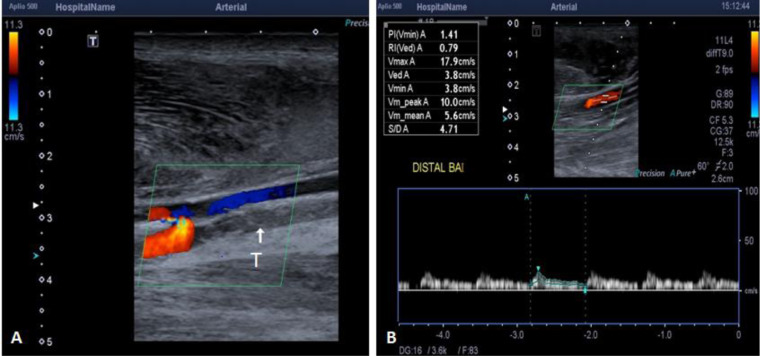
Fig. 2.
(A) Longitudinal view of color flow doppler (CFD) shows intraluminal thrombus (T) and absence of the flow in the brachial artery. (B) Pulsed-waved doppler image shows the blood flow velocity of the distal brachial artery decreased and monophasic flow pattern.
Outcome and follow-up
Of note, there was no significant morbidity such as prolonged swelling of the limb, pain, ischemia, neurologic dysfunction, or amputation, which was graft related in the patient. However mild swelling occurred in the immediate postoperative period in our case, which resolved within ten-days period, and the patient were sent home on a therapeutic dose of enoxaparin for at least 1 month. We did not use aspirin or clopidogrel on the case. No further angiography or imaging was required in this case as our patient had viable limb with a palpable radial pulse at 1-month follow-up.
Discussion
Vascular injuries account for less than 3% of all traumatic pathologies. However, they can result in serious morbidity and amputations. Most of the arterial injuries are penetrating traumas such as gunshot wounds, stabbing, and explosion. While blunt trauma causes solid organ and soft tissue damage, vascular injury is seen less frequently in this group. However, blunt trauma may cause displaced bone fractures and crush injuries that will damage the arterial wall [3].
In many cases, blunt and penetrating trauma causes irregularity in the arterial wall. If the severity of injury increases, findings such as intimal detachment, pseudoaneurysms, or arteriovenous fistula appear, which can cause arterial thrombosis [3,4]. In these types of injuries, rapid and accurate diagnosis is needed to guide the treatment. While conventional angiography is the best method for the diagnosis of trauma-related arterial injuries, noninvasive methods such as computed tomography (CT) and magnetic resonance imaging (MRI) angiography have been used as an alternative in recent years [4]. Compared with MRI, the main disadvantage of CT is that it contains ionizing radiation. CT using intravenous injection of iodinated contrast media reproduces all arterial anatomy within a few minutes. Interpretation of axial, multiplanar reconstructed images, maximum intensity projection, and volume-rendered three-dimensional technique requires approximately 10 minutes. Depiction of arterial reformation and collaterals are better with CT angiography, however, limited to determine the direction of flow. Ionizing radiation, compromised kidney function, and repeatability also limit its use. In our case, no required using CT angiography for arterial injury. Arterial thrombosis was diagnosed using B mode and CF Doppler US images [5].
CF Doppler US, which is another method, is widely used with high sensitivity (95%-97%), and specificity (95%-98%), especially in the evaluation of peripheral arteries. In different studies comparing CF Doppler and CT angiography, the sensitivity and specificity of CF Doppler for detecting arterial damage were 94%-100% and 82.5%-100%, respectively [3]. CF Doppler US has many advantages like portable, no radiation risk, it is also considered to be effective and reliable in the management of treatment without the need for further imaging. Moreover, it is readily available in most clinical settings and is relatively inexpensive. However it is operator dependent. Therefore a combination of operator and interpretative ability are required in answering a specific clinical question, this is what makes US imaging unique [4,6,7].
Additionally, CF Doppler US assessment in the preoperative or endovascular intervention patient provides important information as to the number, extent of stenotic/occlusive lesions and their precise location. It can also be used to mark skin incision sites to reduced contrast MRI or CT use [7].
CF Doppler US should also include the relevant vascular segment and distal of the limb being evaluated. It reliably evaluates arterial flow patterns in normal and abnormal vessels. The normal peripheric arterial waveform consists of three phases, the first phase positive deflection is systolic forward flow, early diastolic flow reversal in the second phase, and the third phase small positive deflection is late diastolic forward flow due to wall recoil, it correlates with wall elasticity. Mild disease results in a biphasic waveform with loss of late diastolic forward flow.
The upper limb artery waveform may convert to a low-resistance form with low pulsatility as a result of the occlusion of more proximal arteries. If the waveform is monophasic, that means that the entire waveform is above the Doppler spectrum baseline. It is characterized by a ''damped/parvus et tardus'' flow pattern, which means that systolic flow acceleration is slowed, peak systolic velocity is reduced, and diastolic flow is increased. This monophasic waveform is appearing at the stenotic site and in the distal artery in cases of severe stenosis with a diameter reduction of more than 50% [7].
In the present case, B-mode US demonstrated complete occlusion with an intraluminal echogenic thrombus of the brachial artery secondary to blunt trauma. Besides, intramuscular and intermuscular soft tissue hematoma accompanied. CF Doppler examination showed the absence of blood flow in the arterial lumen (Fig. 1). In spectral PW Doppler analysis, there were demonstrated monophasic flow pattern and damped flow pattern in the distal arteries. In other words, parvus et tardus waveform in the radial or ulnar arteries are recognized by the decreased in peak systolic velocity and delayed rise. These findings are consistent with the known right brachial artery occlusion (Fig. 2).
Recognition of the parvus et tardus Doppler waveform provides a valuable sign for proximal stenotic disease. Moreover, when reconstitution of flow by collaterals occurs following an arterial occlusion, the parvus et tardus pattern is seen in the distal arteries. This Doppler pattern is also seen distal to sites of arterial occlusion when collateral flow pathways exist [7]. In our case, the parvus et tardus waveform in the distal arteries indicates the flow of blood that passes distally through the collateral vessels.
Compartment hemorrhage or edema can disrupt venous drainage and arterial flow and cause pressure injuries to the nerves [8]. Among the etiologies of ulnar nerve injuries can cause such as compression, blunt trauma, deformities, temporary occlusion of the brachial artery [9]. In this case, improvement of loss sensory in the ulnar nerve distribution after surgery suggests that soft tissue hematoma in the trauma area may have been applied extrinsic compression to the ulnar nerve. The hematoma in the compartment was drained by performing surgery.
Several methods are used in the surgical treatment of arterial injuries. An end-to-end anastomosis is preferred if major collateral vessels can be performed without tension or damage. Otherwise, great saphenous vein interposition graft is the next best choice because it has better patency rates and better infection resistance than synthetic grafts [8]. In this present case, an end-to-end anastomosis was not possible, and the great saphenous vein graft was repaired.
İn conclusion, delayed diagnosis in brachial artery injury due to blunt trauma can cause serious damage such as artery ischemia and nerve compression. However, Doppler US is a noninvasive method that should be used safely in the diagnosis of brachial artery injuries due to its high sensitivity and specificity.
Footnotes
Competing Interests: The authors declare no conflict of interest. The authors alone are responsible for the content and writing of the paper.
Financial Disclosure: This study received no financial support.
Acknowledgments: No acknowledgment is present for the study.
Ethical Standard: Informed consent was obtained from the patient.
Contributor Information
Ismail Gedı Ibrahim, Email: ismaaciilg2@gmail.com.
Mehmet Tahtabasi, Email: mehmet.tahtabasi@sbu.edu.tr.
References
- 1.Dragas M, Davidovic L, Kostic D, Markovic M, Pejkic S, Ille T. Upper extremity arterial injuries: factors influencing treatment outcome. Injury. 2009;40(8):815–819. doi: 10.1016/j.injury.2008.08.012. [DOI] [PubMed] [Google Scholar]
- 2.Grasu BL, Jones CM, Murphy MS. Use of diagnostic modalities for assessing upper extremity vascular pathology. Hand Clin. 2015;31:1Y12. doi: 10.1016/j.hcl.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 3.Montorfano MA, Pla F, Vera L, Cardillo O, Nigra SG, Montorfano LM. Point-of-care ultrasound and Doppler ultrasound evaluation of vascular injuries in penetrating and blunt trauma. Critic Ultras J. 2017;9(1):5. doi: 10.1186/s13089-017-0060-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gaitini D, Razi NB, Ghersin E, Ofer A, Soudack M. Sonographic evaluation of vascular injuries. J Ultrasound Med. 2008;27:95–107. doi: 10.7863/jum.2008.27.1.95. [DOI] [PubMed] [Google Scholar]
- 5.Chidambaram PK, Swaminathan RK, Ganesan P, Mayavan M. Segmental comparison of peripheral arteries by Doppler ultrasound and CT angiography. J Clin Diagnost Res. 2016;10(2):TC12. doi: 10.7860/JCDR/2016/17191.7242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bergstein JM, Blair JF, Edwards J, Wittmann D H, Aprahamian C, Quebbeman E J. Pitfalls in the use of color-flow duplex ultrasound for screening of suspected arterial injuries in penetrated extremities. J Trauma. 1992;33:395–402. doi: 10.1097/00005373-199209000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Gupta P, Lyons S, Hedgire S. Ultrasound imaging of the arterial system. Cardiovasc Diagnosis Ther. 2019;9(Suppl 1):S2. doi: 10.21037/cdt.2019.02.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ergunes K, Yilik L, Ozsoyler I, Kestelli M, Ozbek C, Gurbuz A. Traumatic brachial artery injuries. Texas Heart Inst J. 2006;33(1):31. [PMC free article] [PubMed] [Google Scholar]
- 9.Agarwal A, Chandra A, Jaipal U, Saini N. Imaging in the diagnosis of ulnar nerve pathologies—a neoteric approach. Insights Imaging. 2019;10(1):37. doi: 10.1186/s13244-019-0714-x. [DOI] [PMC free article] [PubMed] [Google Scholar]