Introduction
Cardiac resynchronization therapy (CRT) via biventricular pacing provides clinical benefits, but the nonresponse rate remains high. His bundle pacing (HBP), a physiological pacing modality that preserves normal electrical activation of ventricles, is an alternative to conventional CRT.1 Recently, case reports and studies have demonstrated the feasibility and safety of left bundle branch region pacing (LBBP), which can correct left bundle branch block (LBBB) and has a left ventricular (LV) activation pattern similar to HBP.2, 3, 4 We present a case of a CRT-indicated patient in whom both HBP and LBBP were successfully performed. Electrocardiogram (ECG) and echocardiogram of these 2 pacing modalities were evaluated.
Case report
A 78-year-old female patient presented with complete LBBB for 13 years. ECG showed typical LBBB with QRS duration (QRSd) of 168 ms (Figure 1A). In the past 2 years, the patient had symptomatic sinus dysfunction. Echocardiogram documented low left ventricular ejection fraction (LVEF, 44%) and an enlarged LV end-diastolic dimension (54 mm). Her NYHA class was II. Permanent pacing was indicated for this patient and a CRT pacemaker was prescribed in consideration of LBBB and low LVEF.
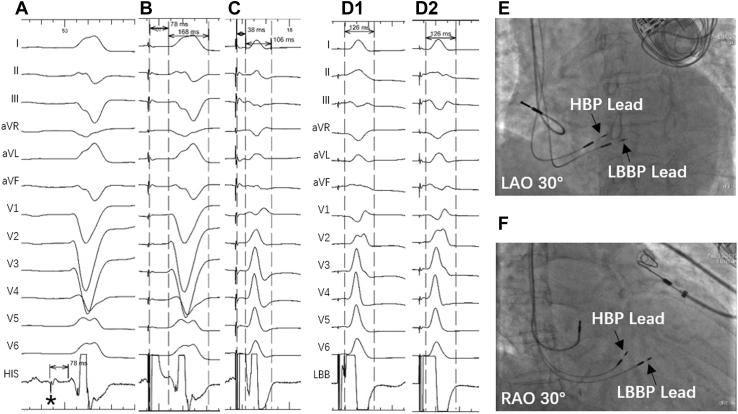
Figure 1.
Selective His bundle pacing (HBP) and left bundle branch pacing (LBBP) during the procedure. A: Intrinsic rhythm with QRS duration (QRSd) of 168 ms; His potential (black star) recorded with HV interval of 78 ms. B: Selective HBP at threshold of 1 V / 0.5 ms with QRSd equal to 168 ms. C: Selective HBP at left bundle branch block (LBBB) correction threshold of 3 V / 0.5 ms with QRSd equal to 106 ms. D: LBBP at different output with constant left ventricular peak activation time and QRSd (D1: LBBP at threshold of 0.6 V / 0.5 ms; D2: LBBP at 5 V / 0.5 ms). E, F: Fluoroscopy image showed the final position of HBP lead and LBBP lead. LAO = left anterior oblique; RAO = right anterior oblique.
Following a failed coronary sinus approach of the LV lead placement, we decided to implement HBP. During the implantation, a fixed-curve sheath (C315HIS, Medtronic Inc, Minneapolis, MN) and a SelectSecure pacing lead (model 3830, 69 cm, Medtronic Inc, Minneapolis, MN) were used. After His bundle potential was recorded (Figure 1A), selective HBP was achieved with a capture threshold of 1 V / 0.5 ms; however, the LBBB correction threshold by HBP was 3 V / 0.5 ms. The paced QRSd was 168 ms at HBP capture threshold (Figure 1B) and 106 ms after LBBB correction by HBP (Figure 1C).
Considering a high acute LBBB correction threshold by HBP and potential increase in HBP capture threshold during follow-up, we performed LBBP with the transventricular septal method.5,6 We moved another set of delivery sheath and pacing lead to the septal location approximately 2 cm below the His bundle region (Figure 1E, F). We then rotated the pacing lead from the right side towards the left side of the interventricular septum while closely monitoring ECG and electrogram during the procedure of lead advancement until LBBP was achieved.6 LBBP with the capture threshold of 0.6 V / 0.5 ms corrected LBBB (Figure 1D1) and yielded the LV peak activation time of 72 ms and QRSd of 126 ms in a pattern of right bundle branch (RBB) conduction delay. The QRSd and LV peak activation time were constant when pacing output was increased to 5 V / 0.5 ms (Figure 1D2). The pacing lead for LBBP was then fixed.
The atrial pacing lead was then implanted and the atrial pacing lead was connected to the atrial port, HBP lead to the LV port, and LBBP lead to the right ventricular (RV) port.
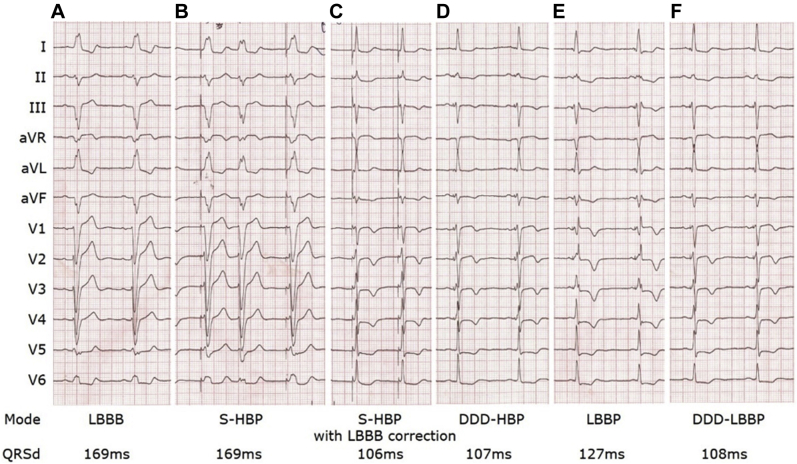
After the implantation, we tested in DDD-RV (LBBP) mode with different sensed atrioventricular (SAV) delay intervals until LBBP synchronized with intrinsic activation to the RV activation to diminish RBB delay. By comparing pacing parameters and QRS morphology between HBP and LBBP (Figure 2), we found that LBBP with optimized SAV delay (DDD-LBBP mode with SAV delay 110 ms) achieved normal QRS pattern (Figure 2E, F) same as during HBP at the LBBB correction threshold of 1.25 V / 0.4 ms (Figure 2B, C, D). The LBBP capture threshold remained stable at 0.5 V / 0.4 ms and the HBP capture threshold at 0.75 V / 0.4 ms. Thus, we finally programmed DDD-RV (LBBP) with SAV interval of 110 ms as permanent pacing mode.
Figure 2.
Comparison of electrocardiogram between selective His bundle pacing (HBP) and left bundle branch pacing (LBBP) after procedure. A: Intrinsic rhythm with QRS duration (QRSd) of 169 ms. B: Selective HBP at threshold of 0.75 V / 0.4 ms with QRSd of 169 ms. C: Selective HBP at left bundle branch block (LBBB) correction threshold of 1.25 V / 0.4 ms with QRSd of 106 ms. D: HBP in DDD mode with sensed atrioventricular (SAV) delay 100 ms, with QRSd of 107 ms. E: LBBP at 0.5 V / 0.4 ms with QRSd of 127 ms and right bundle branch conduction delay pattern. F: LBBP in DDD mode with SAV delay 110 ms, with QRSd of 108 ms.
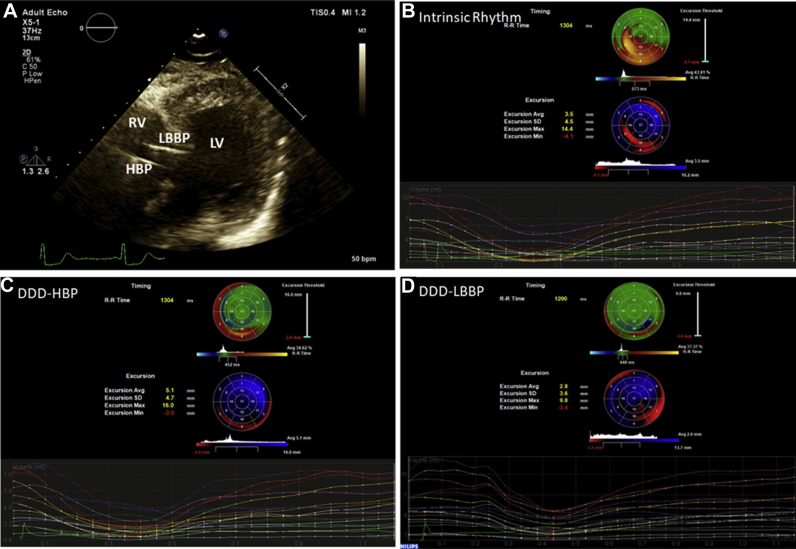
At 3-month follow-up, the cumulative percentage of ventricular pacing was 99.9% during device interrogation. The LBBP capture threshold was 0.75 V / 0.4 ms while the His capture threshold and the LBBB correction threshold by HBP were 1.5 V / 0.4 ms and 1.75 V / 0.4 ms, respectively. The paced QRS morphology was the same as that at implantation. The patient’s cardiac condition was improved with a reduction of NYHA functional class from baseline II to I, a decrease in LV end-diastolic dimension from 54 mm to 47 mm, and an increase in LVEF from 44% to 50%. Parametric imaging of real-time 3-dimensional echocardiography analysis showed 2 bull’s-eye plots of regional timing and excursion, which suggested that significant delayed activation and decreased excursion of inferior and lateral wall of the left ventricle during native rhythm (Figure 3B) were resynchronized by either HBP or LBBP (Figure 3C, D).
Figure 3.
Comparison of 3-dimensional echocardiogram between selective His bundle pacing (HBP) and left bundle branch pacing (LBBP). A: The pacing lead position (the site of LBBP near the sub-endocardium of the left side of the ventricular septum, the HBP site near the tricuspid valve annulus). LV = left ventricle; RV = right ventricle. B–D: Parametric imaging of LV in real-time 3-dimensional echocardiography analysis: B: intrinsic rhythm; C: HBP in DDD mode with sensed atrioventricular (SAV) delay 100 ms; D: LBBP in DDD mode with SAV 110 ms.
Discussion
This case demonstrated that (1) under failed implantation of biventricular pacing for CRT, both HBP and LBBP could be used to correct LBBB, and the LBBB correction threshold was lower for LBBP than for HBP; and (2) the parametric imagine echocardiographic analysis showed cardiac resynchronization by both HBP and LBBP, indicating CRT can be achieved by HBP and LBBP.
According to the theory of longitudinal dissociation, fibers within the His bundle are predestined to the left or right bundle branches and bundle branch block may occur within the His bundle.7 If the HBP lead tip is placed proximal to the LBBB region, a higher pacing output than the capture threshold of HBP is needed to correct LBBB.7,8 Our results of HBP are consistent with this hypothesis; for example, a higher pacing output than the capture threshold was needed for HBP to correct LBBB. Since LBBP at the capture threshold could directly correct LBBB, the pacing tip must be distal to the LBBB region.
This is the first case to compare ECG QRS morphology, pacing parameters, and ventricular resynchronization between HBP and LBBP at implantation and post implantation. The results of the case suggest that both HBP and LBBP can achieve LBBB correction and result in normal QRS and LV resynchronization. HBP, by increasing the pacing output, results in normal QRS morphology in patients with LBBB, while LBBP at a low capture threshold requires additional SAV optimization for offsetting the delay in RV activation during pacing to achieve ventricular resynchronization. Of note, a fixed atrioventricular (AV) delay during LBBP may lead to some degree of delay in pacing the left bundle branch because of dynamic changes in PR interval. For example, an increase in heart rate may lead to the intrinsic RBB conduction ahead of LBBP owing to shortening of the PR interval. Additionally, if a short AV delay is programed to avoid the delay in pacing the left bundle branch, the AV synchronization may be affected. Thus, a new algorithm with a dynamic adjustment of the AV delay for better synchronization between the intrinsic RBB conduction and LBBP is needed. In our current practice, we often fix the SAV delay at a relatively longer value that still yields a short QRSd, usually at 100–120 ms.
We kept both HBP and LBBP in the patient because of concerns of the likelihood of an increase in HBP capture threshold and the lack of long-term clinical results of LBBP. While both HBP and LBBP were successfully performed and showed similar cardiac resynchronization between 2 pacing modalities in this case, potential challenges for achieving these results may exist in elderly patients or patients with valvular heart disease or more diseased myocardium. More clinical investigations and development of new pacing techniques are warranted.
Conclusion
Like HBP, LBBP can achieve LV resynchronization. Both LBBP and HBP can be an alternative to conventional CRT.
Key Teaching Points.
-
•
Cardiac resynchronization can be achieved by either His bundle pacing (HBP) or left bundle branch pacing (LBBP).
-
•
Under failed implantation of coronary sinus lead, HBP or LBBP can be an alternative to conventional cardiac resynchronization therapy via biventricular pacing.
-
•
The pacing output for correcting left bundle branch block is lower for LBBP than for HBP because the site of LBBP bypasses the block while HBP is likely applied proximal to or near the site of the block.
-
•
Right bundle branch conduction delay during LBBP can be offset by sensed atrioventricular delay optimization to fuse ventricular activations deriving from LBBP and intrinsic right bundle branch conduction, leading to a normal electrocardiogram QRS complex.
Acknowledgments
We would like to thank Dr Xiaohong Zhou (Medtronic Inc) for his diligent review of our manuscript.
Footnotes
Funding: Funding was provided by the National Natural Science Foundation of China (Grant/Award Number: 81870260).
References
- 1.Ajijola O.A., Upadhyay G.A., Macias C., Shivkumar K., Tung R. Permanent His-bundle pacing for cardiac resynchronization therapy: Initial feasibility study in lieu of left ventricular lead. Heart Rhythm. 2017;14:1353–1361. doi: 10.1016/j.hrthm.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 2.Chen K., Li Y., Dai Y. Comparison of electrocardiogram characteristics and pacing parameters between left bundle branch pacing and right ventricular pacing in patients receiving pacemaker therapy. Europace. 2019;21:673–680. doi: 10.1093/europace/euy252. [DOI] [PubMed] [Google Scholar]
- 3.Vijayaraman P., Huang W. Atrioventricular block at the distal His bundle: electrophysiological insights from left bundle branch pacing. HeartRhythm Case Rep. 2019;5:233–236. doi: 10.1016/j.hrcr.2019.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang W., Su L., Wu S. A novel pacing strategy with low and stable output: pacing the left bundle branch immediately beyond the conduction block. Can J Cardiol. 2017;33:1736 e1–1736 e3. doi: 10.1016/j.cjca.2017.09.013. [DOI] [PubMed] [Google Scholar]
- 5.Li Y., Chen K., Dai Y. Recovery of complete left bundle branch block following heart failure improvement by left bundle branch pacing in a patient. J Cardiovasc Electrophysiol. 2019:1–4. doi: 10.1111/jce.14034. [DOI] [PubMed] [Google Scholar]
- 6.Li Y., Chen K., Dai Y. Left bundle branch pacing for symptomatic bradycardia: Implant success rate, safety, and pacing characteristics. Heart Rhythm. 2019;16:1758–1765. doi: 10.1016/j.hrthm.2019.05.014. [DOI] [PubMed] [Google Scholar]
- 7.Teng A.E., Massoud L., Ajijola O.A. Physiological mechanisms of QRS narrowing in bundle branch block patients undergoing permanent His bundle pacing. J Electrocardiol. 2016;49:644–648. doi: 10.1016/j.jelectrocard.2016.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Upadhyay G.A., Cherian T., Shatz D.Y. Intracardiac delineation of septal conduction in left bundle branch block patterns. Circulation. 2019;139:1876–1888. doi: 10.1161/CIRCULATIONAHA.118.038648. [DOI] [PubMed] [Google Scholar]