Abstract
The current COVID‐19 pandemic has created a global context likely to increase eating disorder (ED) risk and symptoms, decrease factors that protect against EDs, and exacerbate barriers to care. Three pathways exist by which this pandemic may exacerbate ED risk. One, the disruptions to daily routines and constraints to outdoor activities may increase weight and shape concerns, and negatively impact eating, exercise, and sleeping patterns, which may in turn increase ED risk and symptoms. Relatedly, the pandemic and accompanying social restrictions may deprive individuals of social support and adaptive coping strategies, thereby potentially elevating ED risk and symptoms by removing protective factors. Two, increased exposure to ED‐specific or anxiety‐provoking media, as well as increased reliance on video conferencing, may increase ED risk and symptoms. Three, fears of contagion may increase ED symptoms specifically related to health concerns, or by the pursuit of restrictive diets focused on increasing immunity. In addition, elevated rates of stress and negative affect due to the pandemic and social isolation may also contribute to increasing risk. Evaluating and assessing these factors are key to better understanding the impact of the pandemic on ED risk and recovery and to inform resource dissemination and targets.
Keywords: access to care, body image, COVID‐19, eating disorders, media, risk and protective factors
The coronavirus disease 2019 (COVID‐19) pandemic has deeply disrupted daily life across the globe, with profound effects on mental and physical health (Holmes et al., 2020). Accordingly, research on the health effects of the COVID‐19 pandemic has been identified as an important priority (Holmes et al., 2020). Eating disorder (ED) behaviors are likely to be exacerbated by the pandemic through multiple pathways, particularly among vulnerable groups, including those with body image and eating concerns. Thus, the pandemic may precipitate the development of ED behaviors among some and exacerbate existing pathology among others. Here, we outline three pathways with particular relevance for research priorities and call for research examining how the COVID‐19 pandemic and related social disruptions may increase ED risk and symptoms (see Figure 1).
FIGURE 1.
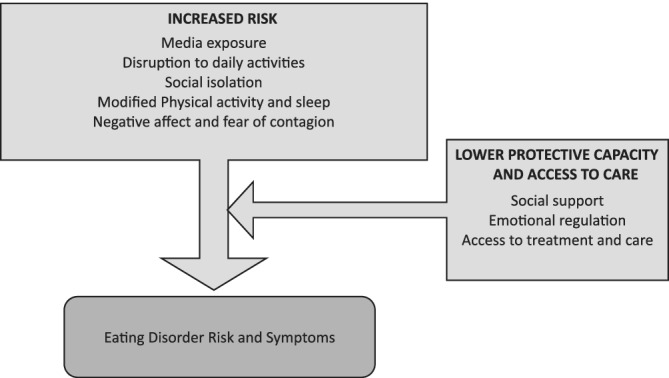
Summary of the pathways through which the COVID‐19 pandemic may increase eating disorder risk and symptoms
1. PATHWAYS FOR EXACERBATION
1.1. Disruptions and restrictions to daily activities and movements
In many countries, the COVID‐19 pandemic has incurred restrictions in daily activities and movements with particularly constraining restrictions in areas of Europe such as Italy and France. For example, work and studying activities have been shifted to the home as much as possible, and all non‐essential travel put on hold. These restrictions have substantial consequences for eating, physical activity, and sleep patterns, each of which may affect or increase the risk of ED behaviors. Regarding eating patterns, the absence of clear routines and markers of time and space, such as mealtimes or separations between home and work areas, may increase risk of ED behaviors by removing structures that were supporting eating plans and, in turn, leading to increased snacking and grazing. Furthermore, for those with families and at risk for EDs, organizing mealtimes several times per day may sharply increase the time spent handling and being around food, which may negatively impact risk for disordered eating behaviors (Heriseanu, Hay, Corbit, & Touyz, 2017). In addition, recommendations to limit activities such as grocery shopping, combined with perceptions of scarcity of certain food products, may heighten attentional focus on food and encourage individuals to stock up on foods more than usual, including snack foods, both of which could increase the likelihood of binge eating (Waters, Hill, & Waller, 2001).
In some contexts, limitations have been placed on physical activity, with individuals allowed outside briefly for physical activity or asked to stay indoors at all times. Such constraints may limit access to regular physical activity, which, in combination with disrupted eating patterns, may lead to heightened shape and weight concerns and disordered eating (Haines, Kleinman, Rifas‐Shiman, Field, & Austin, 2010). Moreover, anxiety related to the pandemic and disrupted routines may negatively impact sleep quality, which is known to increase ED risk (Lombardo, Ballesio, Gasparrini, & Cerolini, 2020; Lombardo, Battagliese, Venezia, & Salvemini, 2015).
Factors that serve to buffer or protect from ED risk have also been negatively impacted by the current COVID‐19 pandemic. Social support has been identified as a global protective and resilience factor during stressful periods, and key to managing and reducing disordered eating (Leonidas & Dos Santos, 2014; Linville, Brown, Sturm, & McDougal, 2012). Worldwide, one of the main strategies to contain and limit the pandemic has been the implementation of social distancing measures and stay‐at‐home orders. Social isolation requirements may constitute a barrier to social support, making individuals more vulnerable to the effects of stressful circumstances. Similarly, other activities that are helpful in terms of emotional regulation (e.g., visiting a therapist, engaging in pleasurable activities) may no longer be accessible to individuals (Cook‐Cottone, 2016), and instead, less adaptive emotional regulation strategies, including emotionally‐induced eating, restrictive eating, or purging behaviors may be relied upon (Lobera, Estébanez, Fernández, Bautista, & Garrido, 2009). Examining the ways in which the COVID‐19 pandemic may increase ED risk and symptoms by negatively affecting protective or buffering factors would be an important contribution. In addition, however, exploring ways in which resilience and protective factors (e.g., removal from stressful social circumstances or decreased daily hassles due to confinement or practice of mind–body activities) may also successfully buffer individuals from ED risk would be another interesting avenue of investigation.
The restrictions placed on movement and disruption to routines may also negatively impact access to care. The COVID‐19 pandemic has the potential to increase need for healthcare services whilst simultaneously reducing capacity for traditional, face‐to‐face treatment options, resulting in greater reliance on telehealth (Davis et al., 2020; Fernández‐Aranda et al., 2020; Gordon & Katzman, 2020; Linardon, Shatte, Tepper, & Fuller‐Tyszkiewicz, 2020; Weissman, Bauer, & Thomas, 2020). These difficulties in access to care may exacerbate existing health inequities, and negatively affect those for whom the pandemic has reduced financial resources (Mulders‐Jones, Mitchison, Girosi, & Hay, 2017; Weissman et al., 2020).
1.2. Media effects
The COVID‐19 pandemic may also be associated with increased risk for ED behaviors relative to media effects in three ways: (a) specific exposure to harmful eating and appearance‐related media, particularly on social media; (b) effects of general media consumption; and (c) the increased use of video‐conferencing while working from home.
Media use, including social media, is associated with increased risk for disordered eating in particular through exposure to thin ideal‐ and diet culture‐related content as well as food advertising (Boswell & Kober, 2016; Levine & Murnen, 2009; Rodgers & Melioli, 2016). The pandemic requirements of social distancing likely increase social media use as a means of communication, which may therefore heighten risk for disordered eating. Furthermore, specific social media trends such as those jokingly referring to weight gain during the period of confinement (“COVID‐19” as a play on words alluding to the “freshman 15”; Elizabeth, 2020), and greater social media attention to home cooking and “pandemic recipes” may create supplemental pressure via greater attention to weight and food that may serve to increase ED risk and symptoms. Although frequency of social media use may vary across cultural contexts, preliminary data on use during the pandemic have shown association with mental health concerns in Asia (Gao et al., 2020; Kantar, 2020; Ni et al., 2020). Exploring how exposure to ED relevant social media, as well as pandemic‐specific social media, is related to ED symptoms and risk would be a fruitful research direction, including cross‐cultural examinations.
Regarding media exposure more broadly, previous research has shown that exposure to media coverage of stressful and traumatic world events was related to increased disordered eating. For example, exposure to media coverage of the 2011 Japanese earthquake was associated with increased dieting but not bulimic type behaviors (Rodgers, Franko, Brunet, Herbert, & Bui, 2012). During the pandemic, much news coverage is devoted to rising numbers of infections and fatalities, health and safety concerns worldwide, and the economic and social impact. As found previously (Rodgers et al., 2012), exposure to such news coverage may similarly increase risk of disordered eating.
In addition to pathways related to media consumption, the increased use of videoconference technologies in the context of “stay at home” orders may also indirectly contribute to risk of ED behaviors by increasing preoccupation around appearance. Body image avoidance is a common feature of body image and eating concerns, and posting self‐images online has been shown to be harmful to body image and mood among young women (Mills, Musto, Williams, & Tiggemann, 2018). It is likely that video conferencing may heighten focus on individuals’ faces and appearance and therefore have similar effects. As this form of communication with family, friends, and in the work setting is likely to continue for some time, examining the effects of “looking in the mirror” repeatedly while talking to others may be an area of interest.
1.3. Emotional distress, and fear of contagion
The COVID‐19 pandemic has resulted in certain eating‐ and food‐specific anxieties (Davis et al., 2020). Thus, fear of contagion from COVID‐19 may lead individuals to experience increased concerns regarding the quality of food or its capacity to be a vehicle of contagion. This may, in turn, increase restrictive eating patterns either through fear of leaving the house to purchase foods or the elimination of certain foods or food groups due to fear of contamination. Disgust responses have been shown to be higher among individuals with ED behaviors and linked to anxiety sensitivity (Anderson et al., 2018; Davey & Chapman, 2009; Harvey, Troop, Treasure, & Murphy, 2002). Although the directionality of these relationships is unclear, combined anxiety and disgust related to fears of contamination might increase ED risk or lead to worsening of existing concerns.
Patterns of disordered eating that are characterized by concerns related to health, rather than weight and shape, have been investigated in the context of orthorexia nervosa, defined by an excessively restrictive eating pattern driven by concerns regarding the quality of food and health concerns (Dunn & Bratman, 2016). Given the capacity for the COVID‐19 pandemic to increase health concerns, and the centrality in orthorexia nervosa of beliefs regarding the usefulness of manipulating diet to promote health, exploring the potential for the COVID‐19 pandemic to increase orthorexia symptomatology specifically would be important.
Relatedly, individuals may adopt restrictive diets believed to have immunity‐related health benefits that may protect them from contracting the coronavirus or minimize its effects (Navaro et al., 2017). While these types of dieting are poorly characterized, they may result in restriction and the elimination of food groups, be accompanied by substantial negative impacts on overall functioning, and lead to increased risk of exposure to the virus due to rigid and specific dietary practices.
In addition to these specific fears created by the COVID‐19 pandemic, the situation has substantially increased general levels of stress and emotional distress (Brooks et al., 2020), which are key risks for disordered eating (Puccio, Fuller‐Tyszkiewicz, Ong, & Krug, 2016), including in the context of traumatic societal events (Harada et al., 2015; Rodgers et al., 2012). Thus, the pandemic may increase risk for key disordered eating patterns, including binge eating and purging, and restrictive, disinhibited, emotional, and external eating patterns. Emotional eating during times of stress, particularly focused on high carbohydrate foods, can often serve as a trigger for binge eating in those with ED or at risk for one (Klatzkin, Gaffney, Cyrus, Bigus, & Brownley, 2018). Importantly, some groups may be more vulnerable to the effects of natural disasters as well as to the present pandemic, in particular people with pre‐existing mental disorders, including EDs (Pfefferbaum & North, 2020).
Worldwide, one of the principal strategies to contain and limit the pandemic has been the implementation of social distancing measures. Beyond the restrictions and limitations to daily activities and movement discussed above, these measures have major, negative psychological impacts (Brooks et al., 2020). Reduced social and physical contact with others may be associated with boredom and frustration, which may in turn increase ED risk and symptoms by increasing emotion‐related eating (Braden, Musher‐Eizenman, Watford, & Emley, 2018). Moreover, social isolation and loneliness, defined as a distressing feeling arising from perceived deficiencies in one's social relationships, that may also result from the social distancing measures may increase negative affect, and negatively impact circadian rhythms and self‐regulation, thereby further increasing ED risk and symptoms (Haines et al., 2010; Lombardo et al., 2015, 2020). Importantly, the psychological impact of social distancing may persist for several months (Brooks et al., 2020), and therefore considering both the immediate and also delayed and longer‐term effects is an additional important focus (Reynolds et al., 2008).
2. CONCLUSIONS
In sum, the current COVID‐19 pandemic has created a situation across the globe likely to increase ED risk and symptoms through multiple pathways and to decrease protective factors and elevate barriers to care. Here we propose pathways and mechanisms that may account for the effects of the pandemic on EDs and we join the call for international researchers in the field to come together to collaboratively generate empirical data to test these potential relationships (Touyz, Lacey, & Hay, 2020). Evaluating and assessing these factors, including across different cultural settings, are key to better understanding the impact of the pandemic on ED risk and recovery and to inform resource dissemination and targets. Identifying high‐risk groups, such as those with pre‐existing disorders or histories of EDs, or youth, due to their increased media consumption and the higher risk of ED onset during this period, will be critical. Incorporating COVID‐related questions in existing longitudinal or cohort disordered eating studies (Eik‐Nes, Austin, Blashill, Murray, & Calzo, 2018; Micali et al., 2017; Pearson et al., 2017; Weissman & Rosselli, 2017) and new studies with population‐representative samples for comparison against existing norms may provide best evidence for disordered eating‐related impacts of COVID‐19.
CONFLICT OF INTEREST
The authors have no conflicts of interest to disclose.
Rodgers RF, Lombardo C, Cerolini S, et al. The impact of the COVID‐19 pandemic on eating disorder risk and symptoms. Int J Eat Disord. 2020;53:1166–1170. 10.1002/eat.23318
Action Editor: Ruth Weissman
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
REFERENCES
- Anderson, L. M. , Reilly, E. E. , Thomas, J. J. , Eddy, K. T. , Franko, D. L. , Hormes, J. M. , & Anderson, D. A. (2018). Associations among fear, disgust, and eating pathology in undergraduate men and women. Appetite, 125, 445–453. 10.1016/j.appet.2018.02.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boswell, R. G. , & Kober, H. (2016). Food cue reactivity and craving predict eating and weight gain: A meta‐analytic review. Obesity Reviews, 17(2), 159–177. 10.1111/obr.12354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braden, A. , Musher‐Eizenman, D. , Watford, T. , & Emley, E. (2018). Eating when depressed, anxious, bored, or happy: Are emotional eating types associated with unique psychological and physical health correlates? Appetite, 125, 410–417. 10.1016/j.appet.2018.02.022 [DOI] [PubMed] [Google Scholar]
- Brooks, S. K. , Webster, R. K. , Smith, L. E. , Woodland, L. , Wessely, S. , Greenberg, N. , & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet, 395, 912–920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook‐Cottone, C. (2016). Embodied self‐regulation and mindful self‐care in the prevention of eating disorders. Eating Disorders, 24(1), 98–105. 10.1080/10640266.2015.1118954 [DOI] [PubMed] [Google Scholar]
- Davey, G. C. , & Chapman, L. (2009). Disgust and eating disorder symptomatology in a non‐clinical population: The role of trait anxiety and anxiety sensitivity. Clinical Psychology and Psychotherapy: An International Journal of Theory and Practice, 16(4), 268–275. 10.1002/cpp.623 [DOI] [PubMed] [Google Scholar]
- Davis, C. , Chong, N. K. , Oh, J. Y. , Baeg, A. , Rajasegaran, K. , & Elaine Chew, C. S. (2020). Caring for children and adolescents with eating disorders in the current COVID‐19 pandemic: A Singapore perspective. Journal of Adolescent Health. 10.1016/j.jadohealth.2020.03.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn, T. M. , & Bratman, S. (2016). On orthorexia nervosa: A review of the literature and proposed diagnostic criteria. Eating Behaviors, 21, 11–17. 10.1016/j.eatbeh.2015.12.006 [DOI] [PubMed] [Google Scholar]
- Eik‐Nes, T. T. , Austin, S. B. , Blashill, A. J. , Murray, S. B. , & Calzo, J. P. (2018). Prospective health associations of drive for muscularity in young adult males. International Journal of Eating Disorders, 51(10), 1185–1193. 10.1002/eat.22943 [DOI] [PubMed] [Google Scholar]
- Elizabeth, D. (2020). Can I socially distance myself from these terrible jokes about gaining weight while quarantined? Allure. Retrieved from https://www.allure.com/story/covid-19-weight-gain-jokes-eating-disorders
- Fernández‐Aranda, F. , Casas, M. , Claes, L. , Bryan, D. C. , Favaro, A. , Granero, R. , … Menchón, J. M. (2020). COVID‐19 and implications for eating disorders. European Eating Disorders Review, 28(3), 239–245. 10.1002/erv.2738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao, J. , Zheng, P. , Jia, Y. , Chen, H. , Mao, Y. , Chen, S. , … Dai, J. (2020). Mental health problems and social media exposure during COVID‐19 outbreak. PLoS One, 15(4), e0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon, C. M. , & Katzman, D. K. (2020). Lessons learned in caring for adolescents with eating disorders: The Singapore experience. Journal of Adolescent Health. 10.1016/j.jadohealth.2020.03.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haines, J. , Kleinman, K. P. , Rifas‐Shiman, S. L. , Field, A. E. , & Austin, S. B. (2010). Examination of shared risk and protective factors for overweight and disordered eating among adolescents. Archives of Pediatrics and Adolescent Medicine, 164(4), 336–343. 10.1001/archpediatrics.2010.19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harada, N. , Shigemura, J. , Tanichi, M. , Kawaida, K. , Takahashi, S. , & Yasukata, F. (2015). Mental health and psychological impacts from the 2011 Great East Japan earthquake disaster: A systematic literature review. Disaster and Military Medicine, 1(1), 17. 10.1186/s40696-015-0008-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey, T. , Troop, N. A. , Treasure, J. L. , & Murphy, T. (2002). Fear, disgust, and abnormal eating attitudes: A preliminary study. International Journal of Eating Disorders, 32(2), 213–218. 10.1002/eat.10069 [DOI] [PubMed] [Google Scholar]
- Heriseanu, A. I. , Hay, P. , Corbit, L. , & Touyz, S. (2017). Grazing in adults with obesity and eating disorders: A systematic review of associated clinical features and meta‐analysis of prevalence. Clinical Psychology Review, 58, 16–32. 10.1016/j.cpr.2017.09.004 [DOI] [PubMed] [Google Scholar]
- Holmes, E. A. , O'Connor, R. C. , Perry, V. H. , Tracey, I. , Wessely, S. , Arseneault, L. , … Bullmore, E. (2020). Multidisciplinary research priorities for the COVID‐19 pandemic: A call for action for mental health science. The Lancet Psychiatry. 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kantar . (2020). COVID‐19 Barometer: Consumer attitudes, media habits and expectations. Retrieved from https://www.kantar.com/Inspiration/Coronavirus/COVID-19-Barometer-Consumer-attitudes-media-habits-and-expectations
- Klatzkin, R. R. , Gaffney, S. , Cyrus, K. , Bigus, E. , & Brownley, K. A. (2018). Stress‐induced eating in women with binge‐eating disorder and obesity. Biological Psychology, 131, 96–106. 10.1016/j.biopsycho.2016.11.002 [DOI] [PubMed] [Google Scholar]
- Leonidas, C. , & Dos Santos, M. A. (2014). Social support networks and eating disorders: An integrative review of the literature. Neuropsychiatric Disease and Treatment, 10, 915–927. 10.2147/NDT.S60735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine, M. P. , & Murnen, S. K. (2009). “Everybody knows that mass media are/are not [pick one] a cause of eating disorders”: A critical review of evidence for a causal link between media, negative body image, and disordered eating in females. Journal of Social and Clinical Psychology, 28(1), 9–42. 10.1521/jscp.2009.28.1.9 [DOI] [Google Scholar]
- Linardon, J. , Shatte, A. , Tepper, H. , & Fuller‐Tyszkiewicz, M. (2020). A survey study of attitudes toward, and preferences for, e‐therapy interventions for eating disorder psychopathology. International Journal of Eating Disorders. 10.1002/eat.23268 [DOI] [PubMed] [Google Scholar]
- Linville, D. , Brown, T. , Sturm, K. , & McDougal, T. (2012). Eating disorders and social support: Perspectives of recovered individuals. Eating Disorders, 20(3), 216–231. 10.1080/10640266.2012.668480 [DOI] [PubMed] [Google Scholar]
- Lobera, I. J. , Estébanez, S. , Fernández, M. S. , Bautista, E. Á. , & Garrido, O. (2009). Coping strategies in eating disorders. European Eating Disorders Review: The Professional Journal of the Eating Disorders Association, 17(3), 220–226. 10.1002/erv.920 [DOI] [PubMed] [Google Scholar]
- Lombardo, C. , Ballesio, A. , Gasparrini, G. , & Cerolini, S. (2020). Effects of acute and chronic sleep deprivation on eating behaviour. Clinical Psychologist, 24, 64–72. 10.1111/cp.12189 [DOI] [Google Scholar]
- Lombardo, C. , Battagliese, G. , Venezia, C. , & Salvemini, V. (2015). Persistence of poor sleep predicts the severity of the clinical condition after 6 months of standard treatment in patients with eating disorders. Eating Behaviors, 18, 16–19. 10.1016/j.eatbeh.2015.03.003 [DOI] [PubMed] [Google Scholar]
- Micali, N. , Martini, M. G. , Thomas, J. J. , Eddy, K. T. , Kothari, R. , Russell, E. , … Treasure, J. (2017). Lifetime and 12‐month prevalence of eating disorders amongst women in mid‐life: A population‐based study of diagnoses and risk factors. BMC Medicine, 15(1), 12. 10.1186/s12916-016-0766-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills, J. S. , Musto, S. , Williams, L. , & Tiggemann, M. (2018). “Selfie” harm: Effects on mood and body image in young women. Body Image, 27, 86–92. 10.1016/j.bodyim.2018.08.007 [DOI] [PubMed] [Google Scholar]
- Mulders‐Jones, B. , Mitchison, D. , Girosi, F. , & Hay, P. (2017). Socioeconomic correlates of eating disorder symptoms in an Australian population‐based sample. PLoS One, 12(1), e0170603. 10.1371/journal.pone.0170603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Navaro, D. A. , Raz, O. , Gabriel, S. , Shriqui, V. K. , Gonen, E. , & Boaz, M. (2017). Functional foods in fad diets: A review. Functional Foods in Health and Disease, 7(9), 702–715. 10.31989/ffhd.v7i9.346 [DOI] [Google Scholar]
- Ni, M. Y. , Yang, L. , Leung, C. M. , Li, N. , Yao, X. I. , Wang, Y. , … Liao, Q. (2020). Mental health, risk factors, and social media use during the COVID‐19 epidemic and cordon sanitaire among the community and health professionals in Wuhan, China. JMIR Public Health and Surveillance, 7, e19009. 10.2196/19009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson, C. M. , Miller, J. , Ackard, D. M. , Loth, K. A. , Wall, M. M. , Haynos, A. F. , & Neumark‐Sztainer, D. (2017). Stability and change in patterns of eating disorder symptoms from adolescence to young adulthood. International Journal of Eating Disorders, 50(7), 748–757. 10.1002/eat.22692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum, B. , & North, C. S. (2020). Mental health and the COVID‐19 pandemic. New England Journal of Medicine. 10.1056/NEJMp2008017 [DOI] [PubMed] [Google Scholar]
- Puccio, F. , Fuller‐Tyszkiewicz, M. , Ong, D. , & Krug, I. (2016). A systematic review and meta‐analysis on the longitudinal relationship between eating pathology and depression. International Journal of Eating Disorders, 49(5), 439–454. 10.1002/eat.22506 [DOI] [PubMed] [Google Scholar]
- Reynolds, D. L. , Garay, J. R. , Deamond, S. L. , Moran, M. K. , Gold, W. , & Styra, R. (2008). Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiology and Infection, 136(7), 997–1007. 10.1017/S0950268807009156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers, R. F. , Franko, D. L. , Brunet, A. , Herbert, C. F. , & Bui, E. (2012). Disordered eating following exposure to television and internet coverage of the March 2011 Japan earthquake. International Journal of Eating Disorders, 45(7), 845–849. 10.1002/eat.22031 [DOI] [PubMed] [Google Scholar]
- Rodgers, R. F. , & Melioli, T. (2016). The relationship between body image concerns, eating disorders and internet use, part I: A review of empirical support. Adolescent Research Review, 1(2), 95–119. 10.1007/s40894-015-0016-6 [DOI] [Google Scholar]
- Touyz, S. , Lacey, H. , & Hay, P. (2020). Eating disorders in the time of COVID‐19. Journal of Eating Disorders, 8, 19. 10.1186/s40337-020-00295-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters, A. , Hill, A. , & Waller, G. (2001). Internal and external antecedents of binge eating episodes in a group of women with bulimia nervosa. International Journal of Eating Disorders, 29(1), 17–22. [DOI] [PubMed] [Google Scholar]
- Weissman, R. S. , Bauer, S. , & Thomas, J. J. (2020). Access to evidence‐based care for eating disorders during the COVID‐19 crisis. International Journal of Eating Disorders, 53, 369–376. 10.1002/eat.23279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman, R. S. , & Rosselli, F. (2017). Reducing the burden of suffering from eating disorders: Unmet treatment needs, cost of illness, and the quest for cost‐effectiveness. Behaviour Research and Therapy, 88, 49–64. 10.1016/j.brat.2016.09.00 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.


