Abstract
The epidemiological burden of COVID‐19 is a healthcare challenge throughout the world, not only in terms of testing the limits of medical capacities, but also as an enigma considering preventive strategies and methods. The upper respiratory tract mucosa is the first line of defense, as a physical barrier, as well as through multiple innate and adaptive immune mechanisms which are crucial for efficient antiviral responses. Identifying methods able to reduce or prevent colonization, viral adhesion, and promote virus shedding on mucous membranes or have the ability to inactivate pathogens and thus reduce virus dose and/or increase immune response would be essential in the management of COVID‐19 outbreak and help in flattening the curve. We review the effects of propolis, an old remedy with proven antiviral properties, as a possible low‐cost inhibitor of SARS‐CoV‐2 in the oropharyngeal niche, prophylaxis, or adjuvant therapy.
Keywords: COVID‐19, prevention, propolis, quercetin, SARS‐CoV‐2
1. INTRODUCTION
The severe acute respiratory syndrome (SARS) coronavirus 2 (SARS‐CoV‐2) responsible for coronavirus disease 19 (COVID‐19) is the seventh member of the coronavirus family that infects human beings after SARS coronavirus and Middle East respiratory syndrome (MERS) coronavirus. 1 Compared with the abovementioned strains, this novel virus has high transmissibility and infectivity and poses great challenge to prevent viral transmission and infection. 2 Human‐to‐human transmission occurs through indirect or direct contact with mucous membranes of the mouth, eyes, or nose. 3 The upper respiratory tract mucosa is the first line of defense, not only as a physical barrier but also through multiple innate and adaptive immune mechanisms which are crucial for efficient antiviral responses.
Viral colonization of the nasopharyngeal niche is a dynamic and complex interplay among microflora, pathogens, host, and interference by environmental factors. 4 Considering the mode of transmission and pathogenesis, effective oral hygiene may be beneficial to decrease the risk of transmission. In addition, gargling is deemed to bring about favorable effects through removal of oral/pharyngeal protease which helps viral replication. 5 Several gargles/mouthwashes have been suggested for the reduction of viral load in the oral cavity: 0.2% chlorhexidine, 1% povidone iodine, 1.5% hydrogen peroxide, or 0.05% hypochlorous acid, essential oils, tap water, and propolis. 6 , 7 Unfortunately, evidence about the effectiveness of these products in prevention of respiratory viral infections is scarce.
2. PROPOLIS: ANCIENT REMEDY
Propolis (bee glue) is a complex resinous mixture produced by honeybees (Apis mellifera) used by humans since ancient times for its medicinal properties. Substances collected from various plants are mixed with the β‐glycosidase enzyme of the honey bee saliva, digested, and added to beeswax to form the final product. Propolis has an important role in hive construction as a waterproof resin; however, it also acts as a barrier to yeasts and molds, bacteria, and viruses.
Propolis is a highly complex mixture, containing over 300 chemical moieties, a number of which have documented beneficial health outcomes. The main constituents of propolis include resins, waxes, essential oils, and pollen, as well as various organic compounds, among which are phenolic compounds, flavonoids, terpenes, esters, aromatic aldehydes and alcohols, and several specific antioxidant compounds including beta‐carotene, caffeic acid, and kaempferol. A new compound isolated from Brazilian green propolis, 3,5‐diprenyl‐4‐hydroxycinnamic acid (artepillin C), may be a key immunomodulatory compound. 7
The biochemical composition of propolis is highly variable, and this variety is significantly affected by the geographical origin, climate, water availability, and other environmental factors. It is widely recognized, for example, that propolis from temperate climatic zones are rich in flavonoids, phenolic acids, and their esters, while propolis from tropical regions are rich in prenylated benzophenones, diterpenes, and flavonoids. 7 , 8 That being said, all types of propolis possess antimicrobial, anti‐neoplastic, anti‐inflammatory, antioxidant, hepatoprotective, cariostatic, and immunostimulatory activity. 8
3. ANTIVIRAL ACTIVITY OF PROPOLIS
The natural variety of propolis has traditionally been an obstacle in research and a standardizing medical use. 7 It also cannot be used as raw material (Figure 1), and it must be purified by extraction with solvents.
FIGURE 1.
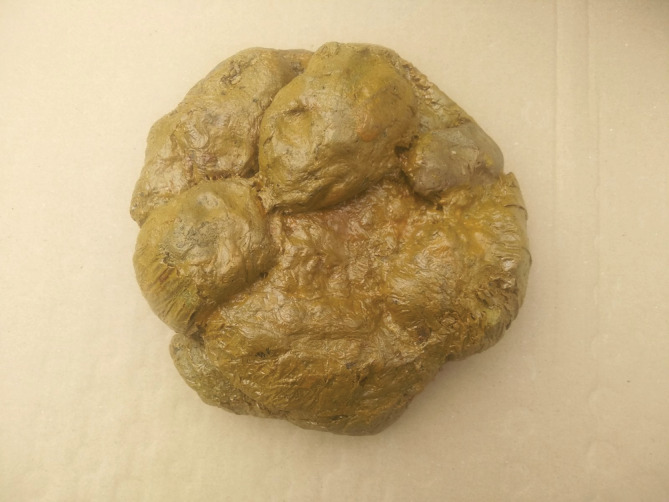
Raw propolis cannot be used, and it must be purified by extraction with solvents, to remove the inert material, and preserve the polyphenolic fraction
Be it alcoholic or aqueous, propolis extracts from temperate climate have been shown to possess a potent and broad‐spectrum antiviral activity against a diverse panel of viruses such as HSV‐1, HSV‐2, Influenza virus type A and B, Parainfluenza virus, Adenovirus, HIV, infectious bursal disease virus, and avian reovirus, Newcastle virus disease, bovine rotavirus, pseudorabies virus, feline calicivirus, canine adenovirus type 2, and bovine viral diarrhea virus. 7 , 8 , 9 , 10 , 11
A 5% alcoholic propolis solution given intranasally 2 h before infection completely inhibited influenza virus proliferation in experimental animals. The preparation had no effect when given to mice already infected. 12
Flavonoids extracted from the resin (kaempferol, acacetin, quercetin, galangin, and chrysine) have been reported to be cytotoxic in variable doses. For example, 3‐methyl‐but‐2‐enyl caffeate, a compound extracted and characterized from poplar has been shown to inhibit DNA synthesis of HSV 1 ex‐vivo. Isopentyl ferulate has shown activity against influenza virus A1 Honey Kong (H3N2) ex‐vivo. Proposed mechanisms of antiviral activity include inhibition of virus entry into the cells, and disruption of the viral replication machinery. 9 , 10 In addition to its effect on virus multiplication, propolis was also found to exert a virucidal action on the enveloped viruses. 10
4. PROPOLIS AND CORONAVIRUS
The studies evaluating the effect of propolis on coronaviruses are scarce. Debiaggi et al. 13 investigated the in vitro effect of five propolis flavonoids on several DNA and RNA viruses including coronavirus, employing the technique of viral plaque reduction. Acacetin and galangin had no effect on either the infectivity or replication of any of the viruses studied. Chrysine and kaempferol, were highly active in inhibiting the replications.
SARS researchers have been paying particular attention to quercetin, a flavonol found in propolis, due to the fact that quercetin in conjunction with vitamin C has been found to be an effective aminopeptidase inhibitor. 14 Quercetin and its derivatives inhibit in vitro, the SARS‐CoV‐1 and MERS‐CoV main protease. Quercetin also modulates the cellular unfolded protein response (UPR). As coronaviruses can utilize the UPR to complete their entire replication cycle, quercetin may have anti‐coronavirus effects through its modulation of this pathway. 15
A promising pharmacological approach for treatment of COVID‐19 is targeting the downstream effectors, such as p21‐activated kinases (PAKs). Caffeic acid phenethyl ester (CAPE), one of the most important constituents of propolis, has shown the property to down‐regulate RAC (a signaling protein found in human cells), therefore acting as a RAC/CDC42‐activated kinase 1 (PAK1) blocker. These data support the idea that CAPE can be useful as an agent to stop or inhibit coronavirus‐induced fibrosis in the lungs. 16
Although propolis belongs to the safest natural remedies, on rare occasions, adverse effects of propolis or its constituents are to be expected, especially allergic reactions. Therefore, when used in prevention or treatment of COVID‐19, hypersensitivity reactions should be taken into account. 8
5. CONCLUSION
Viruses causing respiratory diseases invade their host via the nasopharyngeal, oropharyngeal, or tracheal mucosa. At present, there are no specific antiviral drugs or vaccines against SARS‐CoV2 infection for potential therapy of humans. Identifying methods able to reduce or prevent colonization, viral adhesion, and promote virus shedding on mucous membranes or have the ability to inactivate pathogens and thus reduce virus dose and/or increase immune response would be essential in the management of COVID‐19 outbreak. Therefore, we suggest that propolis (or its constituents) may represent a low‐cost treatment option that may act as potential inhibitors of SARS‐CoV‐2 in the oropharyngeal niche.
Propolis should be explored as a prophylaxis in high‐risk groups, such as individuals in close contact with infected patients. Further studies should be conducted for the validation of these compounds using in vitro and in vivo models. These studies must thoroughly characterize the biological activities and underlying mechanisms of action and isolating the most beneficial compounds, mainly those related to antiviral properties.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Bachevski D, Damevska K, Simeonovski V, Dimova M. Back to the basics: Propolis and COVID‐19. Dermatologic Therapy. 2020;33:e13780. 10.1111/dth.13780
REFERENCES
- 1. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727‐733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Liu Y, Gayle AA, Wilder‐Smith A, Rocklöv J. The reproductive number of COVID‐19 is higher compared to SARS coronavirus. J Travel Med. 2020;27(2):taaa021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Docea AO, Tsatsakis A, Albulescu D, et al. A new threat from an old enemy: re‐emergence of coronavirus (review). Int J Mol Med. 2020;45(6):1631‐1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Vareille M, Kieninger E, Edwards MR, Regamey N. The airway epithelium: soldier in the fight against respiratory viruses. Clin Microbiol Rev. 2011;24(1):210‐229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kitamura T, Satomura K, Kawamura T, Great Cold Investigators‐I , et al. Can we prevent influenza‐like illnesses by gargling? Intern Med. 2007;46:1623‐1624. [DOI] [PubMed] [Google Scholar]
- 6. Eggers M, Koburger‐Janssen T, Eickmann M, Zorn J. In vitro bactericidal and virucidal efficacy of povidone‐iodine gargle/mouthwash against respiratory and oral tract pathogens. Infect Dis Ther. 2018;7(2):249‐259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pascoal AX, Feás T, Dias LG, Estevinho LM. The role of honey and propolis in the treatment of infected wounds. In: Kon K, Rai M, eds. Microbiology for Surgical Infections: Diagnosis, Prognosis and Treatment. Burlington: Elsevier; 2014:221‐234. [Google Scholar]
- 8. Kurek‐Górecka A, Górecki M, Rzepecka‐Stojko A, Balwierz R, Stojko J. Bee products in dermatology and skin care. Molecules. 2020;25(3):556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. González‐Búrquez MJ, González‐Díaz FR, García‐Tovar CG, et al. Comparison between in vitro antiviral effect of Mexican propolis and three commercial flavonoids against canine distemper virus. Evid Based Complement Alternat Med. 2018;2018:7092416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Amoros M, Simões CM, Girre L, Sauvager F, Cormier M. Synergistic effect of flavones and flavonols against herpes simplex virus type 1 in cell culture. Comparison with the antiviral activity of propolis. J Nat Prod. 1992;55(12):1732‐1740. [DOI] [PubMed] [Google Scholar]
- 11. Anjum SI, Ullah A, Khan KA, et al. Composition and functional properties of propolis (bee glue): a review. Saudi J Biol Sci. 2019;26(7):1695‐1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Shevchenko LF, Chasovodtseva OA, Peschanskii AN. Inhibiting activity of própolis on the influenza virus. Chem Abstr. 1972;82:11. [Google Scholar]
- 13. Debiaggi M, Tateo F, Pagani L, Luini M, Romero E. Effects of propolis flavonoids on virus infectivity and replication. Microbiologica. 1990;13(3):207‐213. [PubMed] [Google Scholar]
- 14. Syed S, Saleem A. Severe acute respiratory syndrome epidemiology and control. Lab Med. 2004;35(2):112‐116. [Google Scholar]
- 15. Polansky H, Lori G. Coronavirus disease 2019 (COVID‐19): first indication of efficacy of Gene‐Eden‐VIR/Novirin in SARS‐CoV‐2 infection. Int J Antimicrob Agents. 2020;55(6):105971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Maruta H, He H. PAK1‐blockers: potential therapeutics against COVID‐19. Med Drug Discov. 2020;6:100039. [DOI] [PMC free article] [PubMed] [Google Scholar]


