Dear Editor,
Coronavirus (SARS‐CoV‐2; COVID‐19) has dramatically spread throughout the world despite extraordinarily restricted measures performed by all countries. Global cases of COVID‐19 have passed the 4.5 million checkpoint, and Russia is currently ranked the second most infected nation in the world with 252 245 confirmed cases and 2305 deaths. Approximately 65% of patients are under the age of 65 and less than 6% are children. 1
People are infected either by contact with a contagious person or by touching contaminated surfaces. Infection may be asymptomatic or show different clinical alterations including acute respiratory symptoms, pneumonia, and multiple organ failure. 2 Due to their stronger immune system, compared to adults, children tend to have lower incidence and milder forms of COVID‐19 and generally recover within 1 to 2 weeks. As stated by Shen et al, it appears that the main clinical symptoms in children are fever, dry cough, fatigue, sometimes respiratory, or gastrointestinal symptoms. 3
Dr Recalcati made the first report on cutaneous manifestations in COVID‐19 nearly a month ago, 4 and since then, several authors have also noticed COVID‐19‐associated skin rash in adults. 5 , 6 , 7 , 8 , 9 According to them, skin symptoms may include erythematous rash, localized or widespread urticaria, chicken pox‐like lesions, vascular lesions, and dengue‐like rash. The trunk and the limbs are reported to be the most commonly involved sites. However, the data on COVID‐19‐associated skin disorders in children are scarce.
We observed that a 12‐year‐old girl who was confined to her home in Moscow due to COVID‐19 self‐isolation in mid‐April had a fever of 38.2°C for 2 consecutive days. No clinical symptoms of any bacterial or viral infection were noted except for fatigue and headache. On the second day of fever, the PCR COVID‐19 test was positive. The general blood test was normal except for elevated C‐reactive protein level and erythrocyte sedimentation rate. Chest CT scan revealed no pulmonary changes. The patient was most likely infected by her COVID‐positive mother, who is a nurse looking after many COVID‐19 patients. The treatment was unspecific and consisted of paracetamol. On the third day of illness, the fever dramatically ceased and the skin rash appeared. On examination, we noted purpuric eruptions and erythematous macula rashes of 3 to 4 mm size mainly on the upper eyelids, above the eyebrows and in temporal region (Figure 1). Besides that, her tongue was slightly swollen and irritated with pronounced lingual papillae (Figure 2). The described eruptions were asymptomatic and completely disappeared within 3 days without treatment.
FIGURE 1.
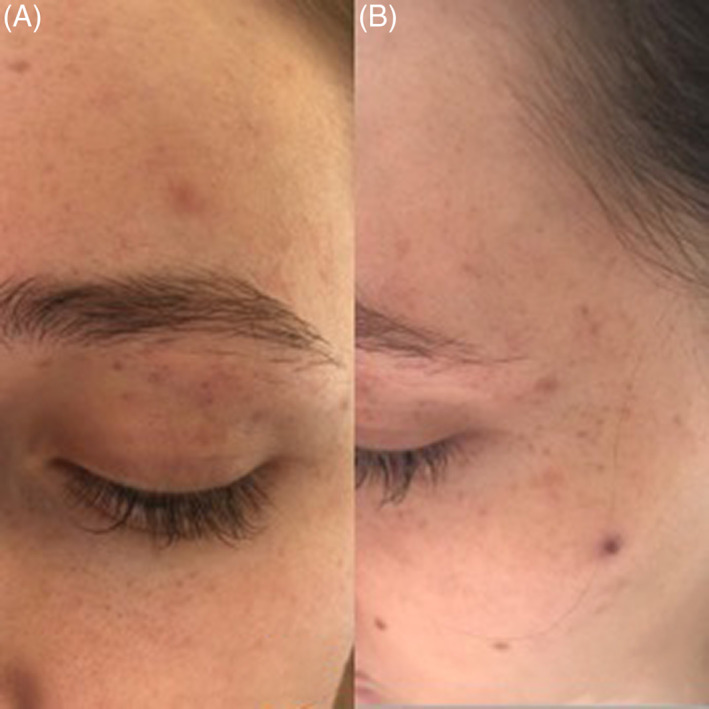
Erythematous macules and purpuric eruptions on the upper eyelids, above the eyebrows, A, and in temporal region, B
FIGURE 2.

Swollen tongue with fur and pronounced lingual papillae
Our observation confirms the idea that the COVID‐19 infectious syndrome not infrequently includes different types of skin rashes and as seen in this first description with a rare involvement of the oral mucous membranes. Along with fever and fatigue, these eruptions may be considered as the only clinical manifestation of these particular COVID‐19 infections in children. This could be due to CD8 hyperexpression, which participates in antiviral immunity. 10
We think it is important to monitor the skin not only in adults but also in children who can transmit this virus asymptomatically. In the case of any skin alterations, we would strongly recommend that a nasopharyngeal and oropharyngeal swab is performed to confirm the possible COVID‐19 diagnosis and in this way break the chain of transmission immediately.
CONFLICT OF INTEREST
The authors declare no potential conflict of interest.
ACKNOWLEDGMENT
The patients in this manuscript have given written informed consent to the publication of their case details.
REFERENCES
- 1. JHU . 2020. COVID‐19 Map—Johns Hopkins Coronavirus Resource Center. https://coronavirus.jhu.edu/map.html. Accessed May 16, 2020.
- 2. Cheng ZJ, Shan J. 2019 Novel coronavirus: where we are and what we know. Infection. 2020;48(2):155‐163. 10.1007/s15010-020-01401-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Shen K‐L, Yang Y‐H, Jiang R‐M, Wang T‐Y, Zhao D‐C, Jiang Y. Updated diagnosis, treatment and prevention of COVID‐19 in children: experts' consensus statement (condensed version of the second edition). World J Pediatr. 2020;16(3):232–239. 10.1007/s12519-020-00362-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Recalcati S. Cutaneous manifestations in COVID‐19: a first perspective. J Eur Acad Dermatol Venereol. 2020;34(5):212–213. 10.1111/jdv.16387. [DOI] [PubMed] [Google Scholar]
- 5. Suchonwanit P, Leerunyakul K, Kositkuljorn C. Cutaneous manifestations in COVID‐19: lessons learned from current evidence. J Am Acad Dermatol. 2020;83(1):57–60. 10.1016/j.jaad.2020.04.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tammaro A, Adebanjo G, Parisella F, Pezzuto A, Rello J. Cutaneous manifestations in COVID‐19: the experiences of Barcelona and Rome. J Eur Acad Dermatol Venereol. 2020. 10.1111/jdv.16530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. van Damme C, Berlingin E, Saussez S, Accaputo O. Acute urticaria with pyrexia as the first manifestations of a COVID‐19 infection. J Eur Acad Dermatol Venereol. 2020. 10.1111/jdv.16523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Joob B, Wiwanitkit V. COVID‐19 can present with a rash and be mistaken for dengue. J Am Acad Dermatol. 2020;82(5):e177. 10.1016/j.jaad.2020.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wollina U, Karadağ AS, Rowland‐Payne C, Chiriac A, Lotti T. Cutaneous signs in COVID‐19 patients: a review. Dermatol Ther. 2020. 10.1111/dth.13549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ruggiero A, Attinà G, Chiaretti A. Additional hypotheses about why COVID‐19 is milder in children than adults. Acta Paediatr. 2020;109(8):1690. 10.1111/apa.15328. [DOI] [PMC free article] [PubMed] [Google Scholar]


