Abstract
Objectives
We sought to study the impact of COVID‐19 pandemic on the presentation delay, severity, patterns of care, and reasons for delay among patients with ST‐elevation myocardial infarction (STEMI) in a non‐hot‐spot region.
Background
COVID‐19 pandemic has significantly reduced the activations for STEMI in epicenters like Spain.
Methods
From January 1, 2020, to April 15, 2020, 143 STEMIs were identified across our integrated 18‐hospital system. Pre‐ and post‐COVID‐19 cohorts were based on March 23rd, 2020, whenstay‐at‐home orders were initiated in Ohio. We used presenting heart rate, blood pressure, troponin, new Q‐wave, and left ventricle ejection fraction (LVEF) to assess severity. Duration of intensive care unit stay, total length of stay, door‐to‐balloon (D2B) time, and radial versus femoral access were used to assess patterns of care.
Results
Post‐COVID‐19 presentation was associated with a lower admission LVEF (45 vs. 50%, p = .015), new Q‐wave, and higher initial troponin; however, these did not reach statistical significance. Among post‐COVID‐19 patients, those with >12‐hr delay in presentation 31(%) had a longer average D2B time (88 vs. 53 min, p = .033) and higher peak troponin (58 vs. 8.5 ng/ml, p = .03). Of these, 27% avoided the hospital due to fear of COVID‐19, 18% believed symptoms were COVID‐19 related, and 9% did not want to burden the hospital during the pandemic.
Conclusions
COVID‐19 has remarkably affected STEMI presentation and care. Patients' fear and confusion about symptoms are integral parts of this emerging public health crisis.
Keywords: coronavirus, delayed presentation, door‐to‐balloon, length of stay, troponin
1. INTRODUCTION
Contrary to the anticipated surge in myocardial infarction (MI) related to the novel coronavirus, 1 there have been reports that the COVID‐19 pandemic has significantly reduced the number of activations for ST‐elevation myocardial infarction (STEMI) in a majority of cities with devastating spread of COVID‐19 cases. 2 The mechanism of this decline is unclear. Furthermore, little work has been done to investigate the impact of this pandemic on STEMI in regions, like Northeast Ohio, where numbers of total cases and overall fatality are relatively lower. We sought to examine STEMI presentation delay, severity, and patterns of care before and after the COVID‐19 pandemic in a non‐hot‐spot region. Additionally, we examined specific reasons for the delay in symptom onset to presentation among the post‐COVID‐19 cohort.
2. MATERIALS AND METHODS
2.1. Study population
From January 1, 2020, to April 15, 2020, a total of 143 STEMI subjects were identified across our 18‐hospital system in a non‐hot‐spot region for COVID‐19. Of these, 10 hospitals perform cardiac catheterization, 3 do not perform primary percutaneous coronary intervention (PPCI), 5 have level I cardiac catheterization laboratories that offer both PPCI and open‐heart surgery, and 2 are level II that only offer PPCI.
All study subjects had a combination of ischemic myocardial symptoms and electrocardiographic ST elevation, or its equivalent, in addition to elevated cardiac troponin on initial or subsequent testing. Each patient with STEMI, except one who declined escalation of care, underwent emergent PPCI. Patients were divided into pre‐ and post‐COVID‐19 cohorts based on March 23, 2020, when stay‐at‐home orders and cancellations of non‐essential procedures were initiated in Ohio. The study was approved by the Institutional Review Board. Data were deidentified, and informed consent was waived for all study participants.
2.2. Presentations, patterns of care, and data collection
We hypothesized that due to fear of contracting COVID‐19 or confusion about symptoms, patients with STEMI on or after March 23, 2020, would likely present with longer delays from the onset of symptoms leading to worsened health status at the time of presentation. We used presenting heart rate, blood pressure (BP), troponin, the presence of new Q‐wave on the earliest electrocardiogram, and initial left ventricle ejection fraction (LVEF) to assess the presentation severity between the pre‐ and post‐COVID‐19 cohorts. Duration of intensive care unit (ICU) stay, total length of stay, door‐to‐balloon (D2B) time, and radial versus femoral approach were used to compare patterns of care between these two time periods. All data were collected prospectively and independently by certified chest pain coordinators as part of the National Cardiovascular Data Registry, and were supplemented by detailed retrospective review of all angiograms, electrocardiograms, echocardiograms, laboratory results, and hospital and emergency medical services records. Reasons for delay in presentation for patients in the post‐COVID‐19 cohort were confirmed with telephone calls.
2.3. Statistical analysis
Baseline characteristics and important procedural characteristics, if continuous variables, were compared using t‐test (if parametric variables) or Wilcoxon rank sum test (if nonparametric variables). Categorical variables were presented as percentages and were compared using chi‐square test, unless the frequency was <5, and then Fisher exact test was utilized. Differences in STEMI presentation severity and care pattern metrics between the two groups were examined in the same manner. In addition, presentation severity measures (incidence of late presentation, percentage of new Q‐waves, and average initial troponin and LVEF) were compared between the two cohorts using different cutoffs to define late presentation (>12, >24, >48, and >72 hr). We also examined reasons for delay among late presenting patients with STEMI in the post‐COVID‐19 period. These were divided into four categories; avoidance of the emergency department (ED) due to fear of COVID‐19; belief that the symptoms were COVID‐19 related; desire not to burden the ED given the COVID‐19 pandemic; and reasons that were not COVID‐19 related. In order to examine internal delays due to concerns about COVID‐19, D2B times were compared between the pre‐ and post‐COVID‐19 cohorts and between those who presented with greater and less than a 12‐hr delay in each cohort. All comparisons were two‐sided and statistical significance was determined as p < .05. All analyses were performed using the R statistical software, version 3.6.3 (R Foundation for Statistical Computing, Vienna, Austria).
3. RESULTS
3.1. Baseline characteristics
Compared with pre‐COVID‐19 patients, post‐COVID‐19 patients were older. However, no significant differences in sex, race, comorbidities, baseline cardiac medications, or important STEMI variables (culprit vessel and thrombolysis in myocardial infarction [TIMI] flow) were seen as shown in Table 1.
TABLE 1.
Baseline characteristics of patients with ST‐elevation myocardial infarction pre‐ and post‐COVID‐19
| Characteristics | Pre‐COVID‐19 (n = 108) | Post‐COVID‐19 (n = 35) | p‐value |
|---|---|---|---|
| Demographics and comorbidities | |||
| Age, year | 61.8 ± 12.6 | 66.0 ± 10.0 | .05 |
| Female sex, no. (%) | 36 (33) | 18 (51) | .15 |
| Body‐mass index | 29.3 ± 6.3 | 30.0 ± 6.3 | .59 |
| Race, no. (%) | .62 | ||
| White | 87 (80) | 32 (91) | |
| Black | 14 (13) | 2 (6) | |
| Asian | 1 (1) | 0 (0) | |
| Other | 2 (2) | 0 (0) | |
| Risk factors, no. (%) | |||
| Heart failure | 25 (23) | 11 (31) | .45 |
| Diabetes mellitus | 32 (30) | 14 (40) | .35 |
| Chronic obstructive pulmonary disease | 25 (23) | 10 (28) | .67 |
| Hypertension | 91 (84) | 28 (80) | .74 |
| Smoking status | 76 (70) | 23 (66) | .76 |
| Serum creatinine, mg/dl | 1.3 ± 0.9 | 1.1 ± 0.4 | .07 |
| Fasting total cholesterol, mg/dl | 167.4 ± 46.2 | 187.7 ± 54.7 | .06 |
| Fasting HDL cholesterol, mg/dl | 39.5 ± 11.7 | 42.9 ± 12.4 | .18 |
| Fasting total triglycerides, mg/dl | 146.9 ± 96.9 | 136.7 ± 79.5 | .55 |
| Fasting LDL cholesterol, mg/dl | 99.3 ± 40.6 | 117.5 ± 46.6 | .05 |
| STEMI variables | |||
| Culprit vessel, no. (%) | .15 | ||
| Left main | 1 (1) | 0 (0) | |
| Right coronary | 54 (50) | 9 (25) | |
| Left anterior descending | 32 (30) | 18 (51) | |
| Left circumflex | 8 (8) | 2 (6) | |
| Diagonal | 1 (1) | 0 (0) | |
| Obtuse marginal | 4 (3) | 2 (6) | |
| Posterior descending | 2 (2) | 3 (9) | |
| Posterolateral branch | 5 (4) | 1 (3) | |
| Ramus | 1 (1) | 0 (0) | |
| TIMI grade flow before revascularization, no. (%) | .95 | ||
| 0 | 66 (61) | 21 (64) | |
| 1 | 10 (9) | 3 (9) | |
| 2 | 18 (17) | 6 (18) | |
| 3 | 14 (13) | 3 (9) | |
| TIMI grade flow after revascularization, no. (%) | .21 | ||
| 0 | 4 (4) | 0 (0) | |
| 1 | 0 (0) | 1 (3) | |
| 2 | 3 (3) | 1 (3) | |
| 3 | 101 (93) | 31 (94) |
Note: Post‐COVID era was defined as after March 23, 2020, as this was the first day of mandatory stay‐at‐home order in Ohio.
Abbreviations: HDL, high‐density lipoprotein; LDL, low‐density lipoprotein; TIMI, thrombolysis in myocardial infarction.
3.2. Severity of presentation
Compared with the pre‐COVID‐19 cohort, post‐COVID‐19 patients had a significantly lower initial LVEF (45 [34–50] vs. 50% [40–60], p = .015). Additionally, although not significant, this cohort had a higher average systolic BP, new Q‐waves at presentation, and initial troponin (Table 2). Subgroup analysis using different cutoffs to define late presentation (>12, >24, >48, and >72 hr after symptom onset) found that delayed patients in the post‐COVID‐19 cohort also trended toward more severe presentations compared to those in the pre‐COVID‐19 cohort regardless of which cutoff was used (Figure 1).
TABLE 2.
Severity of presentation between pre‐ and post‐COVID‐19 patients
| Characteristics | Pre‐COVID‐19 (n = 108) | Post‐COVID‐19 (n = 35) | p‐value |
|---|---|---|---|
| Hemodynamics | |||
| Heart rate, beats/min | 78.3 ± 18.0 | 78.6 ± 18.1 | .94 |
| Systolic blood pressure, mmHg | 130.9 ± 21.3 | 138.6 ± 24.7 | .11 |
| Electrocardiogram | |||
| New Q‐wave, no. (%) | 44 (41) | 15 (43) | .98 |
| Echocardiogram | |||
| Ejection fraction, %, median [IQR] | 50 [40–60] | 45 [34–50] | .02 |
| Ejection fraction <40%, no. (%) | 20 (19) | 11 (31) | .17 |
| Blood markers | |||
| Initial troponin I, ng/ml, median [IQR] | 0.13 [0.02–1.0] | 0.27 [0.04–3.9] | .14 |
| Initial troponin I ≥ 0.4 ng/ml, no. (%) | 36 (33) | 16 (46) | .22 |
FIGURE 1.
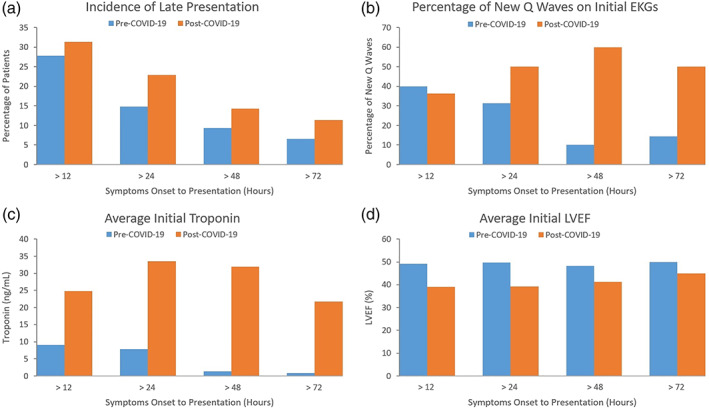
ST‐ elevation myocardial infraction presentation in the pre‐ and post‐COVID‐19 periods. (a) Incidence of late presentation was consistently higher in the post‐COVID‐19 cohort regardless which cutoff was used to define late presentation; similarly, the proportion of patients with (b) new Q‐waves and (c) average initial troponin was consistently higher; and (d) the average initial LVEF was consistently lower [Color figure can be viewed at wileyonlinelibrary.com]
3.3. Reason for delays
Of the 35 patients with STEMI in the post‐COVID‐19 group, 11 presented greater than 12 hr after symptoms onset. Of these, 27% avoided the ED due to fear of COVID‐19, 18% believed symptoms were COVID‐19 related, and 9% did not want to burden the ED given the COVID‐19 pandemic (Table S1). The clinical courses of these 11 patients are depicted in Figure 2.
FIGURE 2.
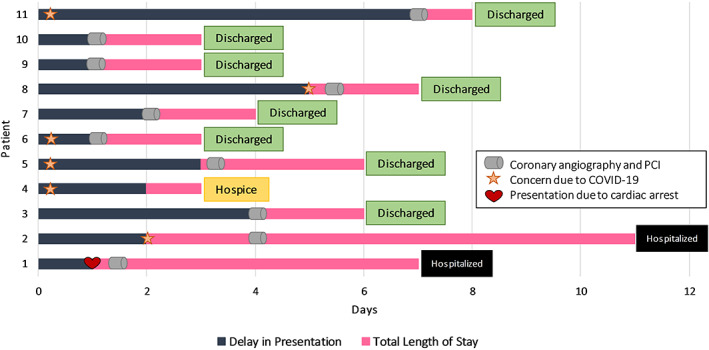
Clinical course of 11 patients with >12 hr delay in the post‐COVID‐19 period. About 50% of patients who presented greater than 12 hr after symptom onset in the post‐COVID‐19 period cited a COVID‐19 related apprehension. Although these patients presented late and with greater severity, they had a shorter average total length‐of‐stay (<3 days) [Color figure can be viewed at wileyonlinelibrary.com]
3.4. D2B times
D2B times were not different between the pre‐ and post‐COVID‐19 cohorts (59 [44–84] vs. 58 [42–102], p = .84) nor between late and nonlate presenters in the pre‐COVID‐19 era. However, in the post‐COVID‐19 cohort, those 11 late‐presenting patients had significantly prolonged D2B times (88 [60–167] vs. 53 min [40–76], p = .033) and peak troponin (58 [9–73] vs. 8.5 ng/ml [4–50], p = .03) compared with those who presented within the first 12 hr (Figure 3). Notably, 18% of these late‐presenting patients experienced a greater than 90‐min D2B time because they were under investigation for COVID‐19.
FIGURE 3.
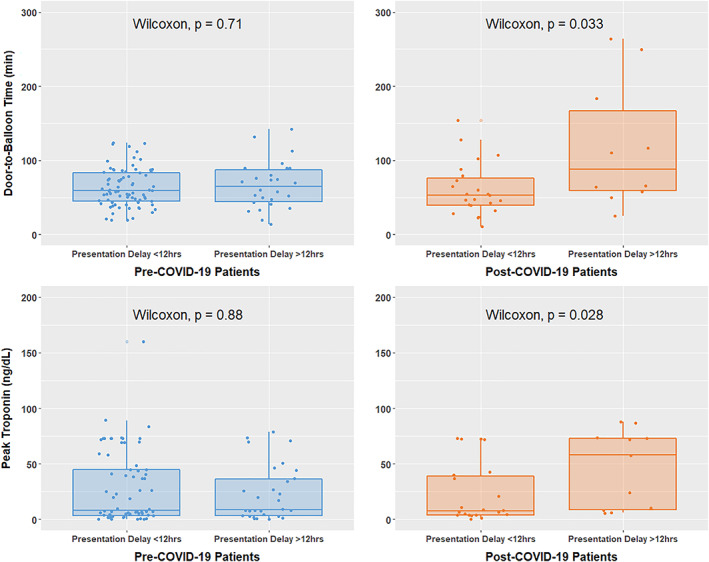
Door‐to‐balloon (D2B) times and peak troponin levels with and without presentation delay in the pre‐ and‐post‐COVID‐19 cohorts. D2B times and peak troponin levels were not different between the pre‐ and post‐COVID‐19 cohorts. However, when comparing patients with and without >12‐hr presentation delay within these two cohorts, we found that (b) the D2B times and (d) peak troponin levels were significantly higher in the patients who presented greater than 12 hr after symptom onset in the post‐COVID‐19 cohort [Color figure can be viewed at wileyonlinelibrary.com]
3.5. Pattern of care
On average, although not significant, STEMI patients in the post‐COVID‐19 period had a shorter ICU duration (1.1 (4.2) vs. 0.4 days (1.5), p = .2) and total length of stay (3.6 (5.9) vs. 2.3 days (1.6), p = .32) (Figure S1). Rates of radial versus femoral approach were 55 and 50% in the pre‐ and post‐COVID cohorts, respectively (p = .8).
4. DISCUSSION
In the studied hospital system, we maintained PPCI for all STEMI patients and did not experience a surge, yet we uncovered untoward consequences of COVID‐19. We found that patients in the post‐COVID‐19 period were more likely to present late and have lower LVEF, higher initial and peak troponin, and new Q‐waves on presentation. More importantly, half of the patients did not seek timely medical help due to COVID‐19‐related apprehensions. Despite late presentation and high‐risk features, post‐COVID‐19 STEMI patients had shorter ICU and hospital length of stay. Collectively, our results confirm a serious public health challenge affecting the cardiovascular care of patients and may have serious short‐ and long‐term consequences even in non‐hot‐spot regions.
A higher proportion of patients in the post‐COVID‐19 period presented with a >12‐hr delay, LVEF <40%, and troponin ≥0.4 ng/ml compared with the pre‐COVID‐19 period. A study of 5,092 STEMI patients treated with PPCI showed that delaying presentation even 4 hr after the onset of symptoms confers a 30% increased risk of mortality. 3 Additionally, Halkin et al showed that patients with a baseline LVEF <40% had a significantly increased likelihood of 1‐year mortality after PPCI. 4 It has also been demonstrated that patients with acute coronary syndromes presenting with an initial troponin ≥0.4 ng/ml have a 3.8‐fold increase in 42‐day mortality. 3 Collectively, our results indicate a delay in seeking medical care with associated worse clinical presentation and confirm a serious public health crisis affecting the cardiovascular care of patients in the United States. 5
Among the patients who presented greater than 12 hr after symptom onset in the post‐COVID‐19 period, about 50% cited fear of COVID‐19 exposure or confusion between COVID‐19 and STEMI symptoms. Our results demonstrate society's fear and the lack of adequate public education regarding symptoms of a heart attack and that of COVID‐19, previously only discussed in anecdotal stories. 6 These heroic, yet disturbing, stories from New York and other epicenters may have played a role in this public fear throughout the United States. Unfortunately, it appears that public trust in the safety of the health care system has been eroded and this needs to be addressed to prevent further adverse outcomes. 6
While the prehospital phase of ischemic duration in STEMI is strongly associated with patient outcomes, 7 , 8 , 9 the in‐hospital phase D2B time is also critically important. 10 , 11 D2B time has been the focus of the American College of Cardiology/American Heart Association guideline for the management of STEMI, as it is an easy to measure metric with strong evidence on its impact on mortality. 12 When comparing D2B times in those with <12 hr vs. >12 hr from symptom onset to presentation in the post‐COVID‐19 period, there was a significant increase in D2B of 33 min for those who already had prolonged prehospital ischemic time (double jeopardy). Further investigation revealed that 40% of those internal delays were related to COVID‐19. This reflects a COVID‐19‐related dysfunction at multiple levels of the STEMI treatment protocol, especially when patients have unclear symptoms or are suspected to have the coronavirus infection. 5
Patients with STEMI in the post COVID‐19 era spent one less day in the hospital with an average LOS of 2.3 days. Two small‐sized randomized trials suggested that early discharge (<3 days) in low‐risk STEMI patients treated with PPCI is safe. 13 , 14 Moreover, Swaminathan et al studied 33,920 elderly STEMI patients from the CathPCI registry and showed that those who had a long hospital stay (>5 days) were more likely to have adverse events. 15 Our results likely reflect physicians' decision to discharge patients early to mitigate the risk of COVID‐19 infection in hospitalized patients with coronary artery disease. The long‐term consequences of this are unknown but may create an opportunity to provide higher value care in the future.
Recently, virtual visits and telemedicine have become common in addressing the COVID‐19 pandemic. 16 While calling 9‐1‐1 is the most appropriate step for patients experiencing a STEMI, creating virtual urgent care visits maybe a viable alternative for patients that remain skeptical, especially when initial symptoms are vague. Furthermore, a broad public health campaign is necessary. While news outlets and media have focused on the gravity of COVID‐19, similar coverage to help educate the public about the safety of EDs and the potentially fatal consequences of acute myocardial infarction is desperately needed.
4.1. Study limitations
Our study has several limitations, especially short‐term follow‐up. However, our results most likely underestimate the impact of COVID‐19 on the long‐term outcomes of STEMI care. Importantly, these data were collected from a region with low COVID‐19 prevalence and may demonstrate trends difference from areas like New York or other epicenters for COVID‐19, although this impact may be larger in COVID‐19 epicenters. 17 Lastly, our sample size is small, but represents a large system with 18 hospitals, 7 of which offer PPCI and cover a large geographic region in Northeast Ohio.
5. CONCLUSION
The current evidence suggests a developing public health crisis within a pandemic. Studies are indicating that patients with acute and chronic conditions suffer major consequences due to multiple factors related to COVID‐19. Some of these, such as unavailability of beds and overloaded EDs in New York or other epicenters, are not easy to address; however, public fears and confusion regarding symptomatology are modifiable. We encourage public health officials, members of the media, and local physician communities to address our patients' fear, provide easily accessible professional opinion through virtual EDs and telemedicine, and once again gain the trust of our patients.
CONFLICT OF INTEREST
The authors declare no potential conflict of interest.
Supporting information
Appendix S1: Supporting Information
ACKNOWLEDGMENTS
The authors are grateful to all nurses, technicians, chest pain coordinators, and physicians for their selfless efforts to care for these patients.
Hammad TA, Parikh M, Tashtish N, et al. Impact of COVID‐19 pandemic on ST‐elevation myocardial infarction in a non‐COVID‐19 epicenter. Catheter Cardiovasc Interv. 2021;97:208–214. 10.1002/ccd.28997
Tarek A. Hammad and Melanie Parik contributed equally to this study.
EDITORIAL COMMENT: Expert Article Analysis for: STEMI and COVID‐19: Unmasking failures and opportunities to enhance future care
Tarek A. Hammad and Melanie Parik contributed equally to this study.
REFERENCES
- 1. Bangalore S, Sharma A, Slotwiner A, et al. ST‐segment elevation in patients with Covid‐19‐a case series. N Engl J Med. 2020. 10.1056/NEJMc2009020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST‐segment elevation cardiac catheterization laboratory activations in the United States during COVID‐19 pandemic. J Am Coll Cardiol. 2020. 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Antman EM, Tanasijevic MJ, Thompson B, et al. Cardiac‐specific troponin I levels to predict the risk of mortality in patients with acute coronary syndromes. N Engl J Med. 1996;335(18):1342‐1349. 10.1056/NEJM199610313351802. [DOI] [PubMed] [Google Scholar]
- 4. Halkin A, Singh M, Nikolsky E, et al. Prediction of mortality after primary percutaneous coronary intervention for acute myocardial infarction: the CADILLAC risk score. J Am Coll Cardiol. 2005;45(9):1397‐1405. 10.1016/j.jacc.2005.01.041. [DOI] [PubMed] [Google Scholar]
- 5. Mahmud E, Dauerman HL, Welt FG, et al. Management of Acute Myocardial Infarction during the COVID‐19 pandemic. Catheter Cardiovasc Interv. 2020;96(2):336‐345. [DOI] [PubMed] [Google Scholar]
- 6. Rosenbaum L. The untold toll‐the pandemic's effects on patients without Covid‐19. N Engl J Med. 2020. 10.1056/NEJMms2009984. [DOI] [PubMed] [Google Scholar]
- 7. Denktas AE, Anderson HV, McCarthy J, Smalling RW. Total ischemic time: the correct focus of attention for optimal ST‐segment elevation myocardial infarction care. JACC Cardiovasc Interv. 2011;4(6):599‐604. 10.1016/j.jcin.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 8. Hannan EL, Zhong Y, Jacobs AK, et al. Effect of onset‐to‐door time and door‐to‐balloon time on mortality in patients undergoing percutaneous coronary interventions for st‐segment elevation myocardial infarction. Am J Cardiol. 2010;106(2):143‐147. 10.1016/j.amjcard.2010.02.029. [DOI] [PubMed] [Google Scholar]
- 9. Cannon CP, Gibson CM, Lambrew CT, et al. Relationship of symptom‐onset‐to‐balloon time and door‐to‐balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. Jama. 2000;283(22):2941‐2947. 10.1001/jama.283.22.2941. [DOI] [PubMed] [Google Scholar]
- 10. Ryota N. Shorter door to balloon time, better long term clinical outcomes in St‐segment elevation myocardial infarction patients Japanese registry of acute myocardial infarction diagnosed by universal definition substudy. J Am Coll Cardiol. 2020;75(11 Supplement 1):14. 10.1016/S0735-1097(20)30641-0.31918829 [DOI] [Google Scholar]
- 11. Tan L‐L, Zheng H, Chow K‐Y, et al. Door‐to‐balloon time correlates better with patients outcomes than symptom‐to‐balloon time. J Am Coll Cardiol. 2016;67(13 Supplement):469. 10.1016/S0735-1097(16)30470-3. [DOI] [Google Scholar]
- 12. O'Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST‐elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. J Am Coll Cardiol. 2013;61(4):e78‐e140. 10.1016/j.jacc.2012.11.019. [DOI] [PubMed] [Google Scholar]
- 13. Melberg T, Jorgensen M, Orn S, Solli T, Edland U, Dickstein K. Safety and health status following early discharge in patients with acute myocardial infarction treated with primary PCI: a randomized trial. Eur J Prev Cardiol. 2015;22(11):1427‐1434. 10.1177/2047487314559276. [DOI] [PubMed] [Google Scholar]
- 14. Kotowycz MA, Cosman TL, Tartaglia C, Afzal R, Syal RP, Natarajan MK. Safety and feasibility of early hospital discharge in ST‐segment elevation myocardial infarction–a prospective and randomized trial in low‐risk primary percutaneous coronary intervention patients (the Safe‐Depart Trial). Am Heart J. 2010;159(1):117 e1‐6. 10.1016/j.ahj.2009.10.024. [DOI] [PubMed] [Google Scholar]
- 15. Swaminathan RV, Rao SV, McCoy LA, et al. Hospital length of stay and clinical outcomes in older STEMI patients after primary PCI: a report from the National Cardiovascular Data Registry. J Am Coll Cardiol. 2015;65(12):1161‐1171. 10.1016/j.jacc.2015.01.028. [DOI] [PubMed] [Google Scholar]
- 16. Hollander JE, Carr BG. Virtually perfect? telemedicine for Covid‐19. N Engl J Med. 2020;382:1679‐1681. 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 17. Rodriguez‐Leor O, Cid‐Alvarez B. STEMI care during COVID‐19: losing sight of the forest for the trees. JACC Case Rep. 2020. 10.1016/j.jaccas.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1: Supporting Information


