Abstract
In the face of a novel infectious disease, changing our collective behaviour is critical to saving lives. One determinant of risk perception and risk behaviour that is often overlooked is the degree to which we share psychological group membership with others. We outline, and summarize supporting evidence for, a theoretical model that articulates the role of shared group membership in attenuating health risk perception and increasing health risk behaviour. We emphasize the importance of attending to these processes in the context of the ongoing response to COVID‐19 and conclude with three recommendations for how group processes can be harnessed to improve this response.
Keywords: health risk perception, risk taking, behaviour change, group processes, trust
Background
As COVID‐19 infection rates soar around the world, public health advice from epidemiologists, medical professionals, and political leaders is that the most powerful weapon we possess to combat its spread is to change our behaviours. Indeed, the measures that governments have imposed – from closing bars to closing borders, from stopping mass gatherings to shutting down entire countries – all represent attempts to ensure widespread behaviour change. These broad evidence‐based measures have been effective in helping to slow, and ultimately halt, the spread of infectious diseases such as SARS in the past (Wilder‐Smith & Freedman, 2020), and have helped attenuate the spread of COVID‐19 (Anderson, Heesterbeek, Klinkenberg, & Hollingsworth, 2020). However, individuals engage in dozens of micro‐level behaviours every day that lead to infectious diseases being passed from one person to another. These behaviours – gathering in close proximity, shaking hands, sharing drinks, choosing to visit one’s ageing parents – are harder to prevent through broad policies, yet critically determine whether containment efforts succeed.
Extant approaches to modelling the transmission of infectious diseases typically draw on economic models (e.g., game theory) and seek to predict the rate and distribution of disease spread through a population (for a review of such models that incorporate some psychological variables, see Weston, Hauck, & Amlot, 2018). Such models necessarily simplify human interaction. For instance, they assume that contact between individuals is random (called homogeneous mixing), such that transmission is just as likely between two strangers as between a husband and a wife (Keeling, 2005). There is also no consensus about the degree to which such models can accurately capture preventative behaviour (e.g., physical distancing; Mao & Yang, 2012). Criticism of these approaches led to the development of alternatives that are network‐based and assume interaction between fewer actors. Interestingly, these network‐based models show more diverse patterns of epidemic spread. For instance, in more clustered networks, there is a faster drop‐off in the initial transmission rate but a longer persistence of susceptible individuals in the population (Keeling, 2005). Nevertheless, network models are limited by the degree to which they accurately reflect key features of real social networks (Aparicio & Pascual, 2007).
We argue that both the modelling of infectious disease and the public health response seeking to alter risk behaviour would be improved through greater consideration of the social psychology of the people in the networks that we seek to model, and whose behaviours leaders seek to change. In particular, we contend that peoples’ engagement (or not) in behaviours that contribute to the spread of infectious disease is fundamentally shaped by their group memberships, most particularly by those groups which hold psychological meaning to them – their social identities (see Tajfel & Turner, 1979; Turner, Hogg, Oakes, Reicher, & Wetherell, 1987). We build on this fundamental proposition by outlining – and providing evidence that speaks to – a social identity model of health risk taking, in which we specify some of the key processes through which social identities shape health risk behaviours (see also Cruwys, Greenaway et al., 2020). At a time when the implications of such behaviours have rarely been more critical, we argue that being cognizant of these processes is paramount.
A social identity model of health risk taking
According to the social identity approach (Tajfel & Turner, 1979; Turner et al., 1987), people categorize themselves in terms of both their personal identity (i.e., as a unique individual) and their various social identities (i.e., as a member of social groups that hold value and meaning to them). In line with this, several thousand empirical studies have demonstrated that subjectively defining oneself in terms of a particular group membership affects thoughts, attitudes, perception, and behaviour (see Haslam, 2014).
Through their capacity to transform psychology and behaviour, group processes fundamentally structure our perception of safety versus vulnerability. Central to our model (see Figure 1) is the proposition that potential threats arising from ingroup members – particularly those with whom we share a strong social identity – will be perceived as less risky, and inspire greater risk taking behaviour, than potential threats arising from outgroup members. In our model, we also articulate two key processes through which we hypothesize that shared group membership affects risk: (a) via increased trust, and (b) via lowered disgust. In the sections that follow, we summarize key evidence for our model.
Figure 1.
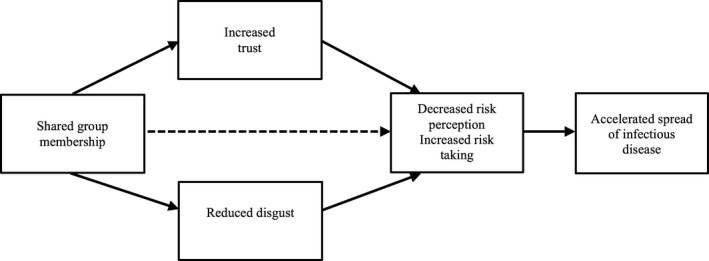
A social identity model of health risk taking. This conceptual framework summarizes key pathways through which social identities shape risk perception and engagement in risk behaviours that contribute to the spread of infectious disease. Adapted from Cruwys, Greenaway, et al. (2020).
Importantly, although this model focuses on the ways in which group processes can undermine the containment of infectious diseases such as COVID‐19, we note that group processes also have a key role to play in an effective response. For instance, greater group identification is associated with increased conformity to group norms (e.g., see Neighbors et al., 2010; Stevens, Rees, & Polman, 2019). For instance, depending on one’s referent group, normative influence may prompt a person to get vaccinated (Falomir‐Pichastor, Toscani, & Despointes, 2009), but could also prompt them to attend a rally protesting social distancing (Ferris, Radke, Walter, & Crimston, 2019). Although norms are non‐focal in the model we present here, we briefly return to the importance of normative influence in the Implications section below.
The importance of group memberships in disease risk
There is a long history of research examining the predictors of risk taking, with good evidence that various biological factors (e.g., hormones such as testosterone; Mehta, Welker, Zilioli, & Carré, 2015), individual factors (e.g., personality traits such as impulsivity; Adan, Forero, & Navarro, 2017), and social factors (e.g., maladaptive social norms; Brady, Iwamoto, Grivel, Kaya, & Clinton, 2016) are associated with a greater likelihood of engaging in risky behaviour. There is also good evidence that people choose to engage (or not engage) in behaviours that pose a risk to their health (e.g., dangerous dieting, wearing sunscreen) because of concerns related to the way they will be perceived by others (e.g., see Leary, Tchividjian, & Kraxberger, 1994). It is likely that these factors are also relevant predictors of peoples’ engagement in behaviours that confer the risk of disease contagion to themselves and others.
Although important, these factors are not the focus of the present article. Rather, our interest centres on the role of shared group membership as a determinant of risk perception and behaviour. That is, a person may well be more likely to take the risk of shaking hands with another person during a pandemic if they are more impulsive, or if this is behaviour they, or people around them, normally engage in. However, we argue that they are also more likely to engage in this behaviour if they perceive the other person to be a fellow ingroup member with whom they share a valued social identity (e.g., as a member of their work or religious group). As a corollary to this, we also propose that people more readily recognize the risk posed by strangers or outgroup members, and take appropriate precautions (or in some cases, engage in inappropriate racism and discrimination; Zhai & Du, 2020, see also Greenaway & Cruwys, 2019).
This critical role of shared identity has been under‐recognized in public health messaging that seeks to change individual behaviour. It is also a particularly insidious contributor to health risk behaviour because people may not even recognize the risk to begin with. That is, the danger posed by shared group membership is that people do not even perceive a risk in the first place because ingroup members are considered ‘safe’ – paving the way for risky behaviour to occur when one’s guard is down. For example, speaking to the role of shared group membership as a predictor of disease risk perception, Hult Khazaie and Khan (2019) found that mass gatherings attendees felt less vulnerable to disease when they felt a strong sense of shared identity with fellow attendees. Loersch and Bartholow (2011) found that participants perceived beer consumption to be less dangerous when they were presented with beer cans that featured the colours of their university, rather than standard beer cans. Regarding risk behaviour, in a sample of 128 military and police officers, Firing and Ladberg (2012) found that shared identity with fellow officers significantly predicted the likelihood of participants taking the risk of jumping into a freezing ocean. Indeed, shared identity was a stronger predictor of risk taking than the personal characteristics of the participants.
Most recently, across eight studies, Cruwys, Greenaway et al. (2020) found consistent evidence for a direct causal link between shared group membership and risk perception and behaviour, including in the context of disease. For instance, in an experiment utilizing the minimal group paradigm (i.e., with groups created at random based on arbitrary criteria), a confederate ostensibly had a cold, and left used tissues in a shared workspace. Participants rated the health risk as greater when the confederate was an outgroup member compared to when they were an ingroup member. Another study explored health risk behaviour among 149 attendees at a controversial art festival. People who strongly identified with fellow attendees stayed for longer at a performance that posed a potential health risk (because it involved dismembering an animal carcass in close proximity to attendees; see Figure 2). In a further experiment, participants were asked to imagine shaking hands with a colleague and later noticing the colleague had a rash on their hand. Participants perceived this to be less risky when their colleague was a member of their political party, rather than an opposing political party. There was evidence that these effects were not attributable to other plausible mechanisms, such as a generalized bias towards ingroup members (i.e., ingroup favouritism). Ingroup favouritism did not mediate the effect of shared group membership on risk perception, and this relationship remained significant when ingroup favouritism was included as a covariate.
Figure 2.

People attended art events that posed a health risk for longer when they identified with fellow attendees (Cruwys, Greenaway et al., 2020). This is consistent with experimental evidence that suggests that we perceive health risks to be lower when they arise from ingroup, rather than outgroup, members. Note: Image of 150.Action supplied by Hermann Nitsch/Dark Mofo. [Colour figure can be viewed at wileyonlinelibrary.com]
The mediating role of trust
A key mechanism through which we propose that shared group membership affects risk perception and behaviour is trust. A robust link has been established between shared group membership and trust, with much of this research using economic investment game paradigms. This research has found that participants are more likely to trust ingroup members to distribute monetary outcomes fairly (Platow, Hoar, Reid, Harley, & Morrison, 2012; Tanis & Postmes, 2005), even when group membership is based on arbitrary criteria (Güth, Levati, & Ploner, 2008).
Trust has primarily been studied as an adaptive cognition that facilitates effective social functioning (Brewer, 2008) – for instance, by enhancing cooperation (Gilson, 2003), and allowing for more effective communication (Longstaff & Yang, 2008). However, trust is also closely linked to risk taking – a relationship that has also been indicated in controlled economic investment game contexts, where evidence suggests participants are more willing to risk gambling money during interactions with more trustworthy game partners (Fetchenhauer & Dunning, 2012; see also Cruwys, Stevens, et al., 2020). The link between trust and health‐related risk taking is supported by evidence from diverse contexts. For instance, ethnographic studies on needle sharing indicate that this behaviour primarily occurs within close social networks and represents an expression of trust (Feldman & Biernacki, 1988). Similarly, research in interpersonal contexts has found trust in one’s sexual partner to be negatively associated with condom use (e.g., see Brady, Tschann, Ellen, & Flores, 2009; see also Flood, 2003). Applied to infectious disease, the capacity for trust to attenuate risk perception and risk avoidant behaviour has implications for contagion spread, because it may lead people to engage in behaviours they should avoid (e.g., shaking hands).
In line with this, recent research has demonstrated the full mediational pathway of shared group membership on health risk perception and behaviour via trust (Cruwys, Greenaway et al., 2020). For example, in a study involving almost 1400 attendees of a school leaving festival, those who identified more strongly with their fellow attendees also trusted them more and, in turn, perceived activities such as accepting a drink from them as less risky. A more fine‐grained analysis suggests that a specific form of trust drives this effect. In two further studies in the context of health and financial risk taking, integrity‐based trust consistently mediated the effect of shared group membership on risk perception and behaviour (Cruwys, Greenaway et al., 2020). This suggests that people tend to believe ingroup members pose less risk than outgroup members primarily because they assume ingroup members will behave in principled ways. In the context of COVID‐19, this means that people may be more likely to assume that ingroup members are strictly adhering to good hygiene practices and are thus less likely to be carrying the disease.
The mediating role of disgust
The second pathway through which we propose that shared group membership can affect health risk is via disgust. Disgust can have substantial benefits in the context of disease contagion. This is because it represents part of the body’s behavioural immune system (Schaller & Park, 2011) – ‘a collection of psychological mechanisms that enables individuals to detect pathogens in their environment and motivate behaviours that prevent these pathogens from entering the body’ (van Leeuwen & Petersen, 2018, p.226). A specific role that disgust plays in mitigating risk is to help distance people from others who could contaminate them (van Leeuwen & Petersen, 2018). Research suggests that peoples’ disgust response can even increase during periods when they are particularly vulnerable to infectious disease (e.g., the first trimester of pregnancy; Fessler, Eng, & Navarrete, 2005).
Disgust also appears to be attenuated by shared group membership. In an early demonstration of the impact of social relationships on disgust, Case et al. (2006) found evidence across two studies that people are less disgusted by the smell of, and by changing, their own children’s nappies compared to those of other children. Relatedly, experimental and questionnaire‐based research indicates that people feel more comfortable being close to, and in a shared environment with, ingroup (rather than outgroup) members (Novelli, Drury, & Reicher, 2010; Steffens, Slade, Stevens, Haslam, & Rees, 2019). These findings align with the evolutionary perspective that we are ‘hard‐wired’ to avoid, or at least be more cautious of, outgroup members because they are more likely to carry pathogens that we (ingroup members) are not immune to (e.g., see Faulkner, Schaller, Park, & Duncan, 2004). However, recent research suggests that these findings may be due to an ingroup attenuation effect on disgust, at least as much as an outgroup accentuation effect.
Research by Reicher et al. (2016) speaks directly to the role of ingroup relations in attenuating disgust. In their first study, these researchers found that university students rated a sweaty t‐shirt bearing the emblem of a different university as less disgusting after their identity as a university student (broadly) had been made salient (making the owner of the t‐shirt an ingroup member) compared to (a) when their identity as a member of their own university had been made salient (making the owner of the t‐shirt an outgroup member), or (b) when their personal identity had been made salient. In their second study, participants’ disgust response – operationalized as the time they took to walk to a bottle of hand sanitizer after touching a sweaty t‐shirt – was lower when the t‐shirt bore the emblem of their university, compared to both (a) when it bore the emblem of a rival university and (b) when the t‐shirt was plain. Importantly, in both studies there was little difference in disgust ratings between the outgroup and personal identity conditions, suggesting that perceiving that someone is an outgroup member may not increase disgust towards them, so much as perceiving someone as an ingroup member decreases disgust towards them. In the COVID‐19 context, this might mean that people experience an attenuated disgust reaction in situations that pose a risk for disease transmission (e.g., sharing food) specifically when the other people involved are perceived to be ingroup members.
Implications for the COVID‐19 response
Our response to this emergency cannot afford to ignore social psychological factors that contribute to risk perception and risk behaviour. From the evidence reviewed above indicating that ingroup members pose a particular risk of transmitting infectious disease, we thus abstract three specific recommendations for the COVID‐19 response (see Table 1).
Table 1.
Recommendations for how to implement social identity principles in the COVID‐19 response
| Recommendation 1 | Statistical modelling of virus spread should weight ingroup members (or close contacts, as a proxy) as posing greater risk for transmission. |
| Recommendation 2 | Public health messages should explicitly highlight the risk associated with being in physical contact with those we care the most about. |
| Recommendation 3 | Public health messages should frame lack of physical contact as an expression of care. |
First, we propose that modelling of disease spread should weight interactions such that ingroup members both (a) interact more often and (b) have a higher risk of transmission with each interaction. Although it may not be practical to model the psychological perception of shared group membership in such models, network models typically include close contacts, which are an acceptable proxy for these purposes. Second, we propose that the elevated risk posed by ingroup members should be recognized in public health messaging, such that this explicitly highlights the risks associated with being in physical contact with others that we care the most about, and the need to be equally vigilant in the way we interact with these people as we are with strangers. Along these lines, we recognize that most people will find it easier to grasp the risk posed by a handshake with a stranger than by a hug with a relative. Thus, third and finally, we propose that public health messages should explicitly challenge this, and frame a lack of physical contact as an expression of care (i.e., show solidarity with your loved ones by keeping your distance).
More broadly, we urge political and health care leaders to work with, rather than against, group processes in their messaging. Indeed, we note that several group processes that are beyond the scope of this article (e.g., normative influence, leadership, and strategies for building solidarity) have a critical role to play in optimizing the COVID‐19 response. While people may find it difficult to perceive the risk of COVID‐19 arising from those closest to them, they are also most motivated to protect their loved ones. Indeed, research indicates that if people perceive that failing to modify their behaviour will result in harm for others, or that modifying their behaviours may improve the health of others, then this positively influences their decisions to engage in protective behaviours such as vaccinations (e.g., see Christini, Shutt, & Byers, 2007). Initial investigations in the context of COVID‐19 support the idea that messages focusing on collective responsibility to loved ones increases compliance with public health directives (Everett, Colombatto, Chituc, Brady, & Crockett, 2020; Jordan, Yoeli, & Rand, 2020).
Conclusion
Through their capacity to shape our perceptions of who we are, social identities structure our cognitive (trust) and emotional (disgust) reactions towards others. Because of this, our evaluation of risk versus safety is inextricably tied to our group memberships. These processes are not, of course, limited to COVID‐19. Indeed, prior research has suggested that our perceptions of, and engagement in, many kinds of risk (financial, physical safety) are also structured by shared group membership (Blois & Ryan, 2013; Cruwys, Greenaway et al., 2020). However, in the absence of biomedical solutions to COVID‐19 (e.g., vaccines), it is vital that we harness all the tools at our disposal in the fight against its deadly spread. We argue that applying our understanding of the social determinants of health risk perception and health risk behaviour is one such tool.
Conflicts of interest
All authors declare no conflict of interest.
Author contribution
Tegan Cruwys, PhD (Conceptualization; Funding acquisition; Project administration; Supervision; Writing – original draft; Writing – review & editing) Mark Stevens (Data curation; Validation; Writing – review & editing) Katharine H Greenaway (Conceptualization; Validation; Writing – review & editing).
Acknowledgements
This research was supported by Australian Research Council Discovery Early Career Research Award to the first author (DE160100592).
Data availability statement
Data sharing is not applicable to this article as no new data were created or analysed in this study.
References
- Adan, A. , Forero, D. A. , & Navarro, J. F. (2017). Personality traits related to binge drinking: A systematic review. Frontiers in Psychiatry, 8, 134. 10.3389/fpsyt.2017.00134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson, R. M. , Heesterbeek, H. , Klinkenberg, D. , & Hollingsworth, T. D. (2020). How will country‐based mitigation measures influence the course of the COVID‐19 epidemic? The Lancet, 395, 931–934. 10.1016/S0140-6736(20)30567-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aparicio, J. P. , & Pascual, M. (2007). Building epidemiological models from R0: An implicit treatment of transmission in networks. Proceedings of the Royal Society B: Biological Sciences, 274, 505–512. 10.1098/rspb.2006.0057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blois, K. , & Ryan, A. (2013). Affinity fraud and trust within financial markets. Journal of Financial Crime, 20, 186–202. 10.1108/13590791311322364 [DOI] [Google Scholar]
- Brady, J. , Iwamoto, D. K. , Grivel, M. , Kaya, A. , & Clinton, L. (2016). A systematic review of the salient role of feminine norms on substance use among women. Addictive Behaviors, 62, 83–90. 10.1016/j.addbeh.2016.06.005 [DOI] [PubMed] [Google Scholar]
- Brady, S. S. , Tschann, J. M. , Ellen, J. M. , & Flores, E. (2009). Infidelity, trust, and condom use among Latino youth in dating relationships. Sexually Transmitted Diseases, 36, 227–231. 10.1097/OLQ.0b013e3181901cba [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer, M. B. (2008). Depersonalized trust and ingroup cooperation. In Krueger J. I. (Ed.), Rationality and social responsibility: Essays in honor of Robyn Mason Dawes. Modern pioneers in psychological science: An APS‐Psychology Press series (pp. 215–32). New York, NY: Psychology Press. [Google Scholar]
- Case, T. I. , Repacholi, B. M. , & Stevenson, R. J. (2006). My baby doesn't smell as bad as yours: The plasticity of disgust. Evolution and Human Behavior, 27, 357–365. 10.1016/j.evolhumbehav.2006.03.003 [DOI] [Google Scholar]
- Christini, A. , Shutt, K. , & Byers, K. (2007). Influenza vaccination rates and motivators among healthcare worker groups. Infection Control & Hospital Epidemiology, 28, 171–177. 10.1086/511796 [DOI] [PubMed] [Google Scholar]
- Cruwys, T. , Greenaway, K. , Ferris, L. J. , Rathbone, J. , Saeri, A. K. , Williams, E. , Parker, S. L. , Change, M. X. L. , Croft, N. , Bingley, W. , & Grace, L. (2020). When trust goes wrong: A social identity model of risk taking. Journal of Personality and Social Psychology. 10.1037/pspi0000243 [DOI] [PubMed] [Google Scholar]
- Cruwys, T. , Stevens, M. , Platow, M. J. , Drury, J. , Williams, E. , Kelly, A. J. , & Weekes, M. (2020). Risk‐taking that signals trust increases social identification. Social Psychology. 10.1027/1864-9335/a000417 [DOI] [Google Scholar]
- Everett, J. A. C. , Colombatto, C. , Chituc, V. , Brady, W. J. , & Crockett, M. (2020). The effectiveness of moral messages on public health behavioral intentions during the COVID‐19 pandemic. 10.31234/osf.io/9yqs8. [DOI]
- Falomir‐Pichastor, J. M. , Toscani, L. , & Despointes, S. H. (2009). Determinants of flu vaccination among nurses: The effects of group identification and professional responsibility. Applied Psychology: An International Review, 58(1), 42–58. [Google Scholar]
- Faulkner, J. , Schaller, M. , Park, J. H. , & Duncan, L. A. (2004). Evolved disease‐avoidance mechanisms and contemporary xenophobic attitudes. Group Processes & Intergroup Relations, 7, 333–353. 10.1177/1368430204046142 [DOI] [Google Scholar]
- Feldman, H. W. , & Biernacki, P. (1988). The ethnography of needle sharing among intravenous drug users and implications for public policies and intervention strategies. In Battjes R. J. & Pickens R. W. (Eds.), Needle sharing among intravenous drug abusers: National and international perspectives (pp. 28–39). Rockville, MD: National Institute on Drug Abuse. [PubMed] [Google Scholar]
- Ferris, L. J. , Radke, H. R. M. , Walter, Z. C. , & Crimston, C. R. (2019). Divide and conquer? Identity, threat, and moral justification of violence at the G20. Australian Journal of Psychology. 10.1111/ajpy.12249 [DOI] [Google Scholar]
- Fessler, D. M. T. , Eng, S. J. , & Navarrete, C. D. (2005). Elevated disgust sensitivity in the first trimester of pregnancy. Evolution and Human Behavior, 26, 344–351. 10.1016/j.evolhumbehav.2004.12.001 [DOI] [Google Scholar]
- Fetchenhauer, D. , & Dunning, D. (2012). Betrayal aversion versus principled trustfulness—How to explain risk avoidance and risky choices in trust games. Journal of Economic Behavior & Organization, 81, 534–541. 10.1016/j.jebo.2011.07.017 [DOI] [Google Scholar]
- Firing, K. , & Laberg, K. C. (2012). Personal characteristics and social identity as predictors of risk taking among military officers: An empirical study. International Journal of Management, 29, 86–98. [Google Scholar]
- Flood, M. (2003). Lust, trust and latex: Why young heterosexual men do not use condoms. Culture, Health & Sexuality, 5, 353–369. 10.1080/1369105011000028273 [DOI] [Google Scholar]
- Gilson, L. (2003). Trust and the development of health care as a social institution. Social Science & Medicine, 56, 1453–1468. 10.1016/S0277-9536(02)00142-9 [DOI] [PubMed] [Google Scholar]
- Greenaway, K. H. , & Cruwys, T. (2019). The source model of group threat: Responding to internal and external threats. American Psychologist, 74, 218–231. 10.1037/amp0000321 [DOI] [PubMed] [Google Scholar]
- Güth, W. , Levati, M. V. , & Ploner, M. (2008). Social identity and trust – An experimental investigation. Journal of Socio‐Economics, 37, 1293–1308. 10.1016/j.socec.2006.12.080 [DOI] [Google Scholar]
- Haslam, S. A. (2014). Making good theory practical: Five lessons for an Applied Social Identity Approach to challenges of organizational, health, and clinical psychology. British Journal of Social Psychology, 53, 1–20. 10.1111/bjso.12061 [DOI] [PubMed] [Google Scholar]
- Hult Khazaie, D. , & Khan, S. S. (2019). Shared social identification in mass gatherings lowers health risk perceptions via lowered disgust. British Journal of Social Psychology. 10.1111/bjso.12362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordan, J. , Yoeli, E. , & Rand, D. G. (2020). Don’t get it or don’t spread it? Comparing self‐interested versus prosocially framed COVID‐19 prevention messaging. 10.31234/osf.io/yuq7x. [DOI] [PMC free article] [PubMed]
- Keeling, M. (2005). The implications of network structure for epidemic dynamics. Theoretical Population Biology, 67, 1–8. 10.1016/j.tpb.2004.08.002 [DOI] [PubMed] [Google Scholar]
- Leary, M. R. , Tchividjian, L. R. , & Kraxberger, B. E. (1994). Self‐presentation can be hazardous to your health: Impression management and health risk. Health Psychology, 13, 461–470. 10.1037/0278-6133.13.6.461 [DOI] [PubMed] [Google Scholar]
- Loersch, C. , & Bartholow, B. D. (2011). The color of safety: Ingroup associated colors make beer safer. Journal of Experimental Social Psychology, 47(1), 190–194. 10.1088/1367-2630/15/1/015008.Fluid [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longstaff, P. H. , & Yang, S. U. (2008). Communication management and trust: their role in building resilience to “surprises” such as natural disasters, pandemic flu, and terrorism. Ecology and Society, 13, 3. [Google Scholar]
- Mao, L. , & Yang, Y. (2012). Coupling infectious diseases, human preventive behavior, and networks ‐ A conceptual framework for epidemic modeling. Social Science and Medicine, 74, 167–175. 10.1016/j.socscimed.2011.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta, P. H. , Welker, K. M. , Zilioli, S. , & Carré, J. M. (2015). Testosterone and cortisol jointly modulate risk‐taking. Psychoneuroendocrinology, 56, 88–99. 10.1016/j.psyneuen.2015.02.023 [DOI] [PubMed] [Google Scholar]
- Neighbors, C. , LaBrie, J. W. , Hummer, J. F. , Lewis, M. A. , Lee, C. M. , Desai, S. , … Larimer, M. E. (2010). Group identification as a moderator of the relationship between perceived social norms and alcohol consumption. Psychology of Addictive Behaviors, 24, 522–528. 10.1037/a0019944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novelli, D. , Drury, J. , & Reicher, S. (2010). Come together: Two studies concerning the impact of group relations on personal space. British Journal of Social Psychology, 49, 223–236. 10.1348/014466609X449377 [DOI] [PubMed] [Google Scholar]
- Platow, M. J. , Foddy, M. , Yamagishi, T. , Lim, L. , & Chow, A. (2012). Two experimental tests of trust in in‐group strangers: The moderating role of common knowledge of group membership. European Journal of Social Psychology, 42, 30–35. 10.1002/ejsp.852 [DOI] [Google Scholar]
- Reicher, S. D. , Templeton, A. , Neville, F. , Ferrari, L. , & Drury, J. (2016). Core disgust is attenuated by ingroup relations. Proceedings of the National Academy of Sciences USA, 113, 2631–2635. 10.1073/pnas.1517027113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaller, M. , & Park, J. H. (2011). The behavioral immune system (and why it matters). Current Directions in Psychological Science, 20, 99–103. 10.1177/0963721411402596 [DOI] [Google Scholar]
- Steffens, N. K. , Slade, E. L. , Stevens, M. , Haslam, S. A. , & Rees, T. (2019). Putting the ‘we’ into workout: The association of identity leadership with exercise class attendance and effort, and the mediating role of group identification and comfort. Psychology of Sport and Exercise, 45, 101544. 10.1016/j.psychsport.2019.101544 [DOI] [Google Scholar]
- Stevens, M. , Rees, T. , & Polman, R. (2019). Social identification, exercise participation, and positive exercise experiences: Evidence from parkrun. Journal of Sports Sciences, 37, 221–228. 10.1080/02640414.2018.1489360 [DOI] [PubMed] [Google Scholar]
- Tajfel, H. , & Turner, J. C. (1979). An integrative theory of intergroup conflict. In Austin W. G. & Worehel S. (Eds.), The social psychology of intergroup relations (pp. 33–47). Monterey, CA: Brooks/Cole. [Google Scholar]
- Tanis, M. , & Postmes, T. (2005). A social identity approach to trust: Interpersonal perception, group membership and trusting behaviour. European Journal of Social Psychology, 35, 413–424. 10.1002/ejsp.256 [DOI] [Google Scholar]
- Turner, J. C. , Hogg, M. A. , Oakes, P. J. , Reicher, S. D. , & Wetherell, M. S. (1987). Rediscovering the social group: A self‐categorization theory. Oxford, UK: Blackwell. [Google Scholar]
- van Leeuwen, F. , & Petersen, M. B. (2018). The behavioral immune system is designed to avoid infected individuals, not outgroups. Evolution and Human Behavior, 39, 226–34. 10.1016/j.evolhumbehav.2017.12.003 [DOI] [Google Scholar]
- Weston, D. , Hauck, K. , & Amlôt, R. (2018). Infection prevention behaviour and infectious disease modelling: a review of the literature and recommendations for the future. BMC Public Health, 18, 336. 10.1186/s12889-018-5223-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilder‐Smith, A. , & Freedman, D. O. (2020). Isolation, quarantine, social distancing and community containment: Pivotal role for old‐style public health measures in the novel coronavirus (2019‐nCoV) outbreak. Journal of Travel Medicine, 27, taaa020. 10.1093/jtm/taaa020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhai, Y. , & Du, X. (2020). Mental health care for international Chinese students affected by the COVID‐19 outbreak. The Lancet Psychiatry, 7, e22. 10.1016/S2215-0366(20)30089-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analysed in this study.


