Dear Editor,
With the COVID‐19 pandemic, we are facing a changing world. This new coronavirus (SARS‐CoV‐2) poses new challenges to dermatologists too. Some of us are in the field, others are describing skin aspects related to this infection, either directly or indirectly caused (e.g. dermatoses resulting from prolonged contact with personal protective equipment and excessive personal hygiene 1 ). Still, cutaneous manifestations are uncommonly reported and the majority has no clinical or histological pictures. At the end of March, Italian colleagues gave us their first impressions on cutaneous manifestations of COVID‐19 that they found in around 20% of their patients: mainly erythematous rashes, urticaria and chickenpox‐like vesicles, which reminded common viral rashes. 2 A petechial rash resembling Dengue fever was also described as a possible initial presentation of COVID‐19 disease, 3 as well as transient livedo reticularis 4 and acro‐ischaemic lesions (cyanosis, skin bullae, dry gangrene) in seven critically ill patients in Wuhan, China. 5 Chilblain‐like lesions are also being described, especially in young patients with mild infections. 6 , 7 , 8
We describe the case of an 81‐year‐old man admitted for bilateral pneumonia, with a negative initial swab for COVID‐19. Blood tests showed an elevated C‐reactive protein (26.97 mg/dL) and procalcitonin (2.09 ng/mL), leucocytosis (12.8 × 109/L) with neutrophilia (11.45 × 109/L) and lymphopenia (0.74 × 109/L), and elevated D‐dimers (4708 ng/mL). Platelet count and coagulation tests were normal, and the patient did not take antiaggregants or anticoagulants. He started empiric antibiotherapy, and blood cultures were negative. One week later, he developed petechial lesions confined to fingers and toes that progressed in a few days to haemorrhagic bullae and necrotic plaques on the hands and feet (Fig. 1). An echocardiogram showed no signs of endocarditis, and blood tests for other possible causes of acral vasculitic lesions (including serum protein electrophoresis, cryoglobulins, B and C hepatitis and HIV serologies) were normal. A cutaneous biopsy showed partial‐thickness necrosis of the superficial portion of the epidermis and a mild inflammatory infiltrate in the papillary dermis composed predominantly of neutrophils. Red blood cell extravasation and focal infiltration of blood vessel walls by neutrophils were noted, consistent with small‐vessel vasculitis. There were no thrombi, papillary dermal oedema or extension of the infiltrate to the deep dermis (Fig. 2). Even after changing antibiotics and introducing aspirin and rosuvastatin, there was progressive degradation of cutaneous and pulmonary disease, and of the patient’s general condition. A new test for COVID‐19 was positive. The patient died 24 days after admission and 17 days after developing cutaneous lesions.
Figure 1.
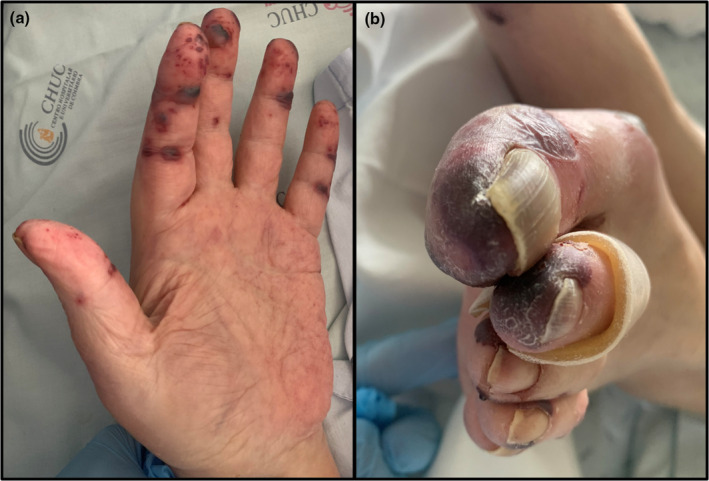
Acro‐ischaemic lesions in a patient infected with COVID‐19. Lesions were mainly purpuric, haemorrhagic bullae and necrotic, affecting fingers (a) and toes (b).
Figure 2.
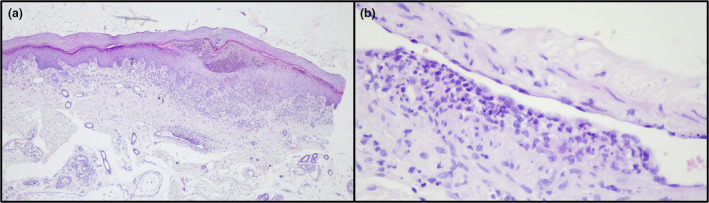
Histological images showing partial‐thickness necrosis of the superficial portion of the epidermis and a mild inflammatory infiltrate in the papillary dermis composed largely by neutrophils (a – H&E 40×). Red blood cell extravasation and focal infiltration of blood vessel walls by neutrophils were also noted, consistent with small‐vessel vasculitis (b – H&E 400×).
Although there is much to discover about SARS‐CoV‐2 and its manifestations, abnormal coagulation results, especially elevated D‐dimers and fibrin degradation products, have been associated with poor prognosis, and disseminated intravascular coagulation (DIC) is common in critically ill COVID‐19 patients. 9 Manalo et al. 4 described transient livedo reticularis (LR) and hypothesized that the microthromboses that manifest in other organs and as DIC in critically ill COVID‐19 patients were the most plausible aetiology for LR and that manifestations could vary from transient LR in milder cases to acrocyanosis in critically ill patients. Findings from minimally invasive autopsies showed degeneration and necrosis of parenchymal cells as well as formation of hyaline thrombi in small vessels in lung and other organs. 8 , 10 In our case, however, we did not find evidence of vascular occlusion but instead a predominantly neutrophilic small‐vessel vasculitis, suggesting that the pathogenesis of the lesions may be different.
To our knowledge, this is the first clinical and histopathological report of COVID‐19 infection‐induced acro‐ischaemic lesions. Similar to other reports, 5 our case also suggests that these acute and ischaemic acral lesions may predict a poor prognosis, in contrast to chilblain lesions that are mostly seen in young and asymptomatic or milder symptomatic patients. 6 , 8
CONFLICTS OF INTEREST
None declared.
ACKNOWLEDGEMENT
A family member of the deceased patient provided consent to the publication of the patient’s case details.
References
- 1. Darlenski R, Tsankov N. Covid‐19 pandemic and the skin – what should dermatologists know? Clin Dermatol 2020; 10.1016/j.clindermatol.2020.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Recalcati S. Cutaneous manifestations in COVID‐ 19: a first perspective. J Eur Acad Dermatol Venereol 2020; 34: 0–1. 10.1111/jdv.16387 [DOI] [PubMed] [Google Scholar]
- 3. Joob B, Wiwanitkit V. COVID‐19 can present with a rash and be mistaken for Dengue. J Am Acad Dermatol 2020; 82: 19–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Manalo IF, Smith MK, Cheeley J, Jacobs R. A dermatologic manifestation of COVID‐19: transient livedo reticularis. J Am Acad Dermatol 2020; 10.1016/j.jaad.2020.04.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zhang Y, Cao W, Xiao M et al. Clinical and coagulation characteristics of 7 patients with critical COVID‐2019 pneumonia and acro‐ischemia. Zhonghua Xue Ye Xue Za Zhi 2020; 41: E006. 10.3760/cma.j.issn.0253-2727.2020.0006 [DOI] [PubMed] [Google Scholar]
- 6. Feoli F, Meiers I, Milone L et al. Coronavirus (COVID‐19) infection‐induced chilblains: a case report with histopathological findings. JAAD Case Rep 2020; 6: 489–492. 10.1016/j.jdcr.2020.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mazzotta F, Troccoli T, Bonifazi E. A new vasculitis at the time of COVID‐19. J Eur Pediatr Dermatol 2020; 4–6. [Google Scholar]
- 8. Alramthan A, Aldaraji W. A case of COVID‐19 presenting in clinical picture resembling chilblains disease. First report from the Middle East. Clin Exp Dermatol 2020; 10.1111/ced.14243 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost 2020; 18: 844–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Yao XH, Li TY, He ZC et al. A pathological report of three COVID‐19 cases by minimally invasive autopsies. Zhonghua Bing Li Xue Za Zhi 2020; 49: E009. [DOI] [PubMed] [Google Scholar]


