Abstract
Aim
Novel coronavirus infection (COVID‐19) was confirmed in Wuhan, China in December 2019, and the COVID‐19 pandemic has spread around the world. However, no clinical studies on the impact of the COVID‐19 pandemic on emergency medical service (EMS) systems have been carried out.
Methods
This was a retrospective study with a study period from 1 January 2020 to 14 April 2020. We included the patients transported by ambulance for acute diseases and traffic accidents in Osaka city, Japan. The main outcome of this study was the difficulty in hospital acceptance. We calculated the rate of difficulty of hospital acceptance for each month for acute diseases and traffic accidents.
Results
Between 1 January and 14 April 2020, 36,981 patients were transported to hospitals by ambulance for acute diseases and 3,096 patients for traffic accidents. There was no difference in the proportion of the difficulty in hospital acceptance due to traffic accidents between 2019 and 2020, but there was an increase in the proportion of the difficulty in hospital acceptance due to acute disease after the 13th week (25–31 March) of 2020 compared to that of 2019. The odds ratio in April was 2.17 (95% confidence interval, 1.84–2.58) for acute disease.
Conclusion
We assessed the impact of the COVID‐19 pandemic on the EMS system in Osaka City, Japan and found that, since April 2020, the EMS system in Osaka City has been facing difficulty in terms of hospital acceptance of patients transported to hospital for acute diseases.
Keywords: COVID‐19, emergency medical service, novel coronavirus, pandemic
Novel coronavirus infection (COVID‐19) was confirmed in Wuhan, China in December 2019, and the COVID‐19 pandemic has spread around the world. However, no clinical studies on the impact of the COVID‐19 pandemic on emergency medical service (EMS) systems have been carried out. In this study, the EMS system in Osaka City faced difficulty in terms of hospital acceptance of patients transported to hospital for acute diseases from April 2020.
Introduction
Novel coronavirus infection (COVID‐19) was confirmed in Wuhan, China in December 2019, and the epidemic of COVID‐19 has spread not only in China but now throughout the world. 1 In Japan, the number of patients infected with COVID‐19 exceeded 10,000 on 18 April 2020, and is still increasing. 2 The characteristic chief complaints of COVID‐19 are common to those of the common cold or influenza such as fever, cough, sore throat, and general malaise, and some patients with COVID‐19 are asymptomatic. 3
As the number of patients infected with COVID‐19 has increased worldwide, the global health system is on the verge of total collapse. It is evident that the COVID‐19 pandemic is putting health‐care systems such as intensive care and emergency medicine divisions at particular risk. As the health‐care system in Japan is under universal coverage, the emergency medical service (EMS) system, such as the ambulance service, is also fully operated by the public sector. Presently, to our knowledge, no clinical studies on the impact of the COVID‐19 pandemic on the EMS system have been carried out anywhere in the world.
The Osaka Municipal Fire Department (OMFD) has been collecting records of ambulance dispatches in Osaka ity, Japan, a metropolitan community with approximately 2.6 million residents as of 2015 and over 200,000 ambulance dispatches every year. Since the first case of COVID‐19 occurred in Osaka on 29 January 2020, 4 the number of patients infected with COVID‐19 in Osaka Prefecture has increased to 1075 as of 18 April 2020; a state of emergency was declared by the Japanese government for Osaka Prefecture on 7 April 2020. 5 The aim of this study was to assess the impact of the COVID‐19 pandemic on the EMS system in Osaka city, Japan.
Methods
Study design and setting
This study was a retrospective, descriptive study with a study period from 1 January 2020 to 17 April 2020. Osaka City, the largest metropolitan community in western Japan, covers an area of 222 km2. The OMFD has been recording the reason for ambulance calls into 13 categories, which include acute disease, gynecological disease, fire accident, water accident, natural disaster, traffic accident, industrial accident, disease and injury due to sports, asphyxia, gas poisoning, assault, self‐inflicted injury, and other injury. 6 To assess the influence of the COVID‐19 pandemic on the EMS system, we focused on the patients transported by ambulance for acute disease in Osaka City because suspected cases of COVID‐19 infection should be treated as ambulance calls for acute disease. In addition, we also included the patients transported by ambulance for traffic accidents to determine the influence of the COVID‐19 pandemic as urgent cases. This study excluded patients who were not transported to a hospital. The ambulance records in Osaka City are considered administrative records, and the requirement of obtaining patients’ informed consent was waived because the data were anonymous. This study was approved by the Ethics Committee of Osaka University Graduate School of Medicine (Suita, Japan). This manuscript was written based on the STROBE statement to assess the reporting of cohort and cross‐sectional studies. 7
Emergency medical service system and hospitals in Osaka City, Japan
The EMS system is basically the same as that used in other areas of Japan, as previously described. 8 Briefly, it is operated exclusively by the OMFD and is activated by calling 1‐1‐9. The EMS personnel at the scene select the appropriate medical institutions near the scene that are best able to treat emergency patients according to the medical urgency or patient symptoms. The OMFD had 25 fire stations (79 ambulances) and one dispatch center in 2018. Usually, each ambulance has a crew of three emergency providers, including at least one emergency lifesaving technician who is a highly trained prehospital emergency care provider authorized to use an automated external defibrillator, to insert an i.v. line and administer adrenaline, and to provide advanced airway management. 9 In Osaka City, there were 184 hospitals (32,645 beds) in 2015. 10 Among them, 99 hospitals, including six critical care centers, were designated to accept life‐threatening emergency patients from ambulances. In Osaka City, emergency dispatchers do not make phone calls to hospitals to confirm acceptance; only ambulance crews at the scene select appropriate hospitals, including critical care centers, for the emergency patients.
Data collection and quality control
Data were uniformly collected using specific data collection forms and included the reason for ambulance call, location of the accident, the time of day and day of the week, and tools used. 6 The detailed situation and patient information were recorded in text form. These data were completed by EMS personnel and then transferred to the information center in the OMFD. The data sheet is supposed to be returned to the relevant EMS personnel for them to correct if it was incomplete. However, in the present study, we used the preliminary data that had not been fed back to the EMS personnel due to the urgency of this situation.
Outcomes
The main outcome of this study was the difficulty in obtaining hospital acceptance for transfer of a patient. According to the guideline of the Fire and Disaster Management Agency, we defined the cases for which ambulance crews needed to make five or more phone calls to hospitals before obtaining hospital acceptance as difficult cases. 6 The secondary outcome was the case in which the time interval from arrival at the scene to departure from the scene was longer than 60 min.
Data analysis
We calculated the numbers of patients transported by ambulance due to acute disease and traffic accidents per week from 1 January 1 to 14 April 2020. For comparison purposes, the numbers of patients transported by ambulance for the same reasons per week from 1 January to 15 April 2019 were also collected. In addition, we used a linear regression analysis to assess the trends in the number of patients transported by ambulances in 2019 and 2020. Next, we calculated the rate of difficulty of hospital acceptance of patients for each month for acute disease and traffic accidents and then calculated the crude odds ratio (OR) for each month for the difficulty of hospital acceptance and 95% confidence interval (CI) with January as the reference. In addition, we calculated the incidence of cases that took more than 60 min from EMS arrival at the scene to departure, and the crude OR and 95% CI with January as the reference were also calculated. All statistical analyses were undertaken using the spss statistical package version 26.0 J (IBM, Armonk, NY, USA). All tests were two‐tailed, and P‐values <0.05 were considered statistically significant.
Results
Between 1 January and 14 April 2020, 36,981 patients were transported to hospitals by ambulances for acute diseases and 3,096 patients were transported to hospitals for traffic accidents in Osaka City, Japan. For comparison, between 1 January and 15 April 2019, 41,095 patients and 3,367 patients were transported to hospitals, respectively.
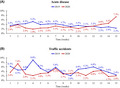
Figure 1 shows the number of patients transported due to acute disease and traffic accidents per week for each year. Compared to 2019, the number of patients transported due to acute disease was lower after the 10th week of 2020. Similarly, the number of those transported due to traffic accidents was lower after the 14th week of 2020. In acute disease cases, the regression coefficient was −67.5 (95% CI, −88.6 to −46.3, P for trend <0.001) in 2019 and −77.5 (95% CI, −96.0 to −58.8, P for trend < 0.001) in 2020. In traffic accident cases, it was 5.8 (95% CI, 1.7 to 9.8, P for trend = 0.009) in 2019 and −1.9 (95% CI, −6.5 to −2.7, P for trend = 0.389) in 2020.
Fig. 1.
Number of patients in Osaka City, Japan, transported to hospital by ambulance due to acute disease and traffic accidents per week in 2019 and 2020.
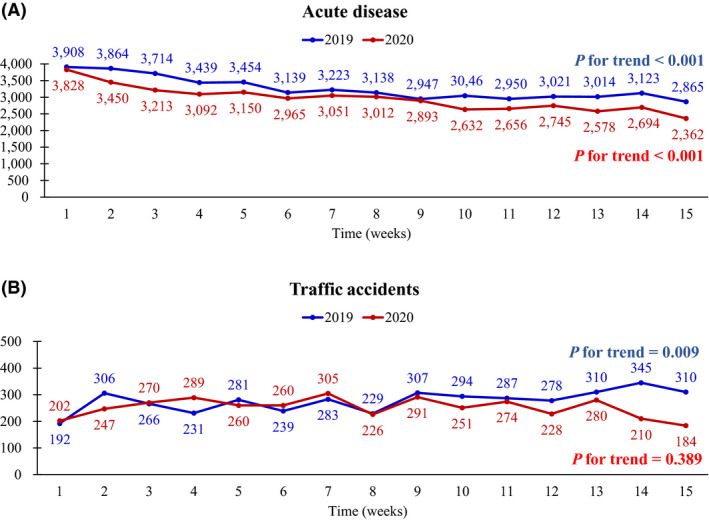
Figure 2 shows the proportion of difficulty in hospital acceptance among patients who were transported to the hospitals by ambulance due to acute disease and traffic accidents. There was no difference in the proportion of difficulty in hospital acceptance due to traffic accidents between 2019 and 2020, but there was an increase in the proportion of difficulty in hospital acceptance due to acute disease after the 13th week in 2020 compared with that in 2019. The OR in April was 2.17 (95% CI, 1.84–2.58) for acute disease, whereas there was no significant difference for traffic accidents compared to January (Table 1).
Fig. 2.
Proportion of difficulty in hospital acceptance in Osaka City, Japan, among patients who were transported by ambulance due to acute disease and traffic accidents in 2019 and 2020.
Table 1.
Proportion of difficulty in hospital acceptance among patients in Osaka City, Japan, transported by ambulance for acute disease or traffic accidents for each month of the study (January–April 2019 and 2020)
| Causes | Month | n/N | (%) | OR (95% CI) | P‐value | |
|---|---|---|---|---|---|---|
| Acute disease | 1 | 349/12,661 | (2.8) | Ref. | ||
| 2 | 285/10,448 | (2.7) | 0.99 (0.84–1.16) | 0.894 | ||
| 3 | 297/9,824 | (3.0) | 1.10 (0.94–1.29) | 0.235 | ||
| 4 | 235/4,048 | (5.8) | 2.17 (1.84–2.58) | <0.001 | ||
| Traffic accidents | 1 | 32/920 | (3.5) | Ref. | ||
| 2 | 35/886 | (4.0) | 1.14 (0.7–1.86) | 0.596 | ||
| 3 | 33/962 | (3.4) | 0.99 (0.6–1.62) | 0.955 | ||
| 4 | 6/328 | (1.8) | 0.52 (0.21–1.25) | 0.142 | ||
CI, confidence interval; OR, odds ratio; Ref., reference.
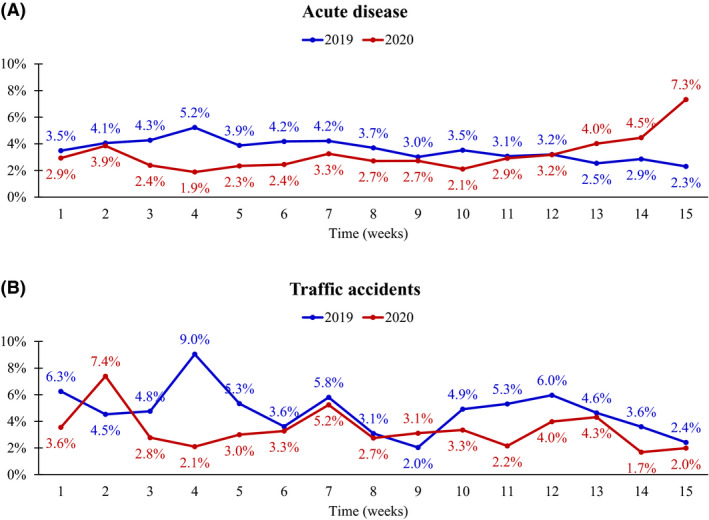
Figure 3 shows the proportion of patients transported for acute disease and traffic accidents whose time period from EMS arrival at the scene to departure from the scene was longer than 60 min. There was no difference between 2019 and 2020 for traffic accidents, but there was an increase in the proportion of difficulty in hospital acceptance among transported patients for acute disease after the 13th week in 2020 compared to that in 2019. The crude OR in April was 2.81 (95% CI, 2.14–3.68) for acute disease, whereas there was no difference in each month for traffic accidents (Table 2).
Fig. 3.
Proportion of patients in Osaka City, Japan, transported to hospital for acute disease and traffic accidents whose time period from emergency medical service arrival at the scene to departure from the scene was >60 min in 2019 and 2020.
Table 2.
Proportion of patients in Osaka City, Japan, whose time period from emergency medical service arrival at the scene to departure from the scene was >60 min, grouped by month of study (January–April 2019 and 2020)
| Cause | Month | n/N | (%) | OR (95% CI) | P‐value |
|---|---|---|---|---|---|
| Acute disease | 1 | 114/12,661 | (0.9) | Ref. | |
| 2 | 98/10,448 | (0.9) | 1.04 (0.8–1.37) | 0.766 | |
| 3 | 105/9,837 | (1.1) | 1.19 (0.91–1.55) | 0.206 | |
| 4 | 101/4,058 | (2.5) | 2.81 (2.14–3.68) | <0.001 | |
| Traffic accidents | 1 | 8/920 | (0.9) | Ref. | |
| 2 | 3/886 | (0.3) | 0.39 (0.1–1.47) | 0.162 | |
| 3 | 9/963 | (0.9) | 1.08 (0.41–2.8) | 0.882 | |
| 4 | 0/329 | (0.0) | n.a. |
CI, confidence interval; n.a., not available; OR, odds ratio; Ref., reference.
Discussion
In this study, there was a decrease in the number of patients transported by ambulance after the ninth week in 2020 compared to the same period in 2019 (Fig. 1). In the patients transported by ambulance due to acute disease, the proportion of difficulty in hospital acceptance of patients increased from the 12th week and increased significantly from April. In contrast, there was no difference in the proportion of difficulty in hospital acceptance among patients transported by ambulance due to traffic accidents. This is the first study, to our knowledge, to show the impact of the COVID‐19 pandemic on an EMS system and could contribute to the development of various countermeasures taken by the EMS system in the coming weeks of the COVID‐19 pandemic and also for future epidemics of infectious diseases.
The number of patients transported by ambulance after the ninth week of 2020 was lower than the same period in 2019. According to the statistics from the Fire and Disaster Management Agency, the number of patients transported by ambulance in Japan has been increasing for the past 10 years, 11 and that in Osaka City has been increasing for the past 5 consecutive years. 12 Two factors might have played a role in the results of our analysis. First, ambulance calls in Japan are a public service, and anyone can request an ambulance for free. As a result, it was reported that 48.6% of the patients transported to hospitals were patients with minor illnesses who could be returned home from the emergency department. 11 As the COVID‐19 pandemic has grown, there have been campaigns around the world to thank health‐care providers for their service. 13 A similar campaign in Japan 14 might have resulted in increased public concern for emergency medical care providers, and less urgent patients might have been discouraged from using ambulances. Second, the route of transmission of COVID‐19 is thought to be direct contact or through aerosolized droplets, 15 so some patients might have considered the risk of contracting COVID‐19 through contact with a patient with COVID‐19 if they were taken to hospital. It is unclear whether these reactions in the EMS system are seen only in Japan or are similar around the world. Thus, it will be necessary to compare the impact of the COVID‐19 pandemic on the EMS system in other countries.
The proportion of difficulty in hospital acceptance among patients transported by ambulance due to acute disease increased significantly in April. The chief complaints of COVID‐19 are similar to those of a common cold and flu. In April 2020, a simple diagnostic kit for COVID‐19 such as that for influenza was not available. Therefore, when ambulances transported patients with symptoms such as fever and cough, there was a concentration of requests to transport patients to certain hospitals that were well‐equipped facilities with infection control measures, and that might have affected patient transport by ambulance. In addition, we cannot deny the possibility that some hospitals that usually receive emergency patients transported by ambulance could have turned down patients suspected of having COVID‐19 due to inadequate infection control measures against the COVID‐19 virus.
However, there was no increase in the proportion of difficulty in hospital acceptance of urgent cases such as traffic accidents. In Osaka City, the majority of severe patients with COVID‐19 requiring intensive care, such as ventilators and extracorporeal membrane oxygenation, were treated at critical care centers. These critical care centers in Japan mainly treat severe patients such those injured in traffic accidents, those with sepsis, and those suffering out‐of‐hospital cardiac arrest. Although the prevalence of COVID‐19 has hindered hospital acceptance among transported patients by ambulance due to acute disease compared to 2019, most medical institutions still had the capacity to accommodate patients with high urgency such as traffic accidents. It will be necessary to continue to monitor how these conditions change with the evolution of the COVID‐19 pandemic.
Limitations
There are several limitations in this study. First, because we emphasized the rapidity and short timeframe of this study, we analyzed preliminary data. Therefore, the present data could differ slightly from the official statistical data that will be published later, in which incorrect data are corrected. Second, because we analyzed ambulance records in this study, the final diagnosis and prognosis in hospital were unknown. Therefore, it is unclear whether patients with highly urgent conditions, such as acute myocardial infarction or stroke, were actually affected by transport difficulties. Because Osaka Prefecture has been operating a population‐based registry for patients transported by ambulance (ORION), which records the final diagnosis and prognosis in hospital, 16 in the future, we will use the ORION data to analyze the impact of the COVID‐19 pandemic on the EMS system. Finally, this study was a retrospective, observational study, and there could be some unknown confounding factors due to the study type.
Conclusion
We assessed the impact of the COVID‐19 pandemic on the EMS system in Osaka City, Japan. Since April 2020, the EMS system in Osaka City has faced difficulty in terms of hospital acceptance of patients transported for acute disease by ambulance.
Funding information
No funding information provided.
Disclosure
Approval of the research protocol: The protocol was approved by the Ethics Committee of Osaka University as the corresponding institution.
Informed consent: The requirement for informed consent of the patients was waived.
Registry and the registration no. of the study/trial: This study was not registered.
Animal studies: N/A.
Conflict of interest: None.
Acknowledgements
The authors are greatly indebted to all of the EMS personnel working in the Osaka Municipal Fire Department. We thank our colleagues from Osaka University Center of Medical Data Science and Advanced Clinical Epidemiology Investigator’s Research Project for providing their insight and expertise for our research.
References
- 1. Lai CC, Wang CY, Wang YH et al Global epidemiology of coronavirus disease 2019 (COVID‐19): disease incidence, daily cumulative index, mortality, and their association with country healthcare resources and economic status. Int. J.. Antimicrob. Agents. 2020; 55: 105946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ministry of Health, Labour and Welfare . The statistics of patients with COVID‐19. https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000121431_00086.html. Accessed on 28 April 2020. (in Japanese).
- 3. Huang C, Wang Y, Li X et al Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020; 395: 497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Osaka Prefectural Government . The statistics of patients with COVID‐19 in Osaka Prefecture. https://covid19‐osaka.info/. Accessed on 28 April 2020. (in Japanese).
- 5. Prime Minister’s Office of Japan . Headquarters for Novel Coronavirus Infection Control (27th meeting). https://www.kantei.go.jp/jp/98_abe/actions/202004/07corona.html. Accessed on 28 April 2020. (in Japanese).
- 6. Katayama Y, Kitamura T, Kiyohara K et al Factors associated with the difficulty in hospital acceptance at the scene by emergency medical service personnel: a population‐based study in Osaka City, Japan. BMJ Open. 2016; 6: e013849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Von Elm E, Altman DG, Egger M et al The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J. Clin. Epidemiol. 2008; 61: 344–9. [DOI] [PubMed] [Google Scholar]
- 8. Irisawa T, Iwami T, Kitamura T et al An association between systolic blood pressure and stroke among patients with impaired consciousness in out‐of‐hospital emergency settings. BMC Emerg. Med. 2013; 13: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kajino K, Kitamura T, Iwami T et al Impact of the number of on‐scene emergency life‐saving technicians and outcomes from out‐of‐hospital cardiac arrest in Osaka City. Resuscitation. 2014; 85: 59–64. [DOI] [PubMed] [Google Scholar]
- 10. Ministry of Health, Labour and Welfare . Medical faculty survey in 2015. https://www.mhlw.go.jp/toukei/saikin/hw/iryosd/15/dl/gaikyo.pdf. Accessed on 28 April 2020. (in Japanese).
- 11. The Fire and Disaster Management Agency . White book on Emergency system in Japan. 2018. https://www.fdma.go.jp/publication/hakusho/h30/chapter2/section4/38607.html. Accessed on 28 April 2020. (in Japanese). [Google Scholar]
- 12. Osaka Municipal Fire Department . The annual report of ambulance dispatch in 2018. https://www.city.osaka.lg.jp/shobo/page/0000491144.html. Accessed on 28 April 2020. (in Japanese).
- 13. BBC . Coronavirus Clap for Our Carers. https://www.bbc.co.uk/programmes/m000h5r6. Accessed on 28 April 2020.
- 14. Osaka Prefectural Government . Novel coronavirus rescue fund in Osaka Prefecture. http://www.pref.osaka.lg.jp/kenisomu/coronakikin/index.html. Accessed on 28 April 2020. (in Japanese).
- 15. Gupta MK, Lipner SR. Personal protective equipment recommendations based on COVID‐19 route of transmission. J Am Acad Dermatol. 2020; 83: e45–e46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Okamoto J, Katayama Y, Kitamura T, et al Profile of the ORION (Osaka emergency information Research Intelligent Operation Network system) between 2015 and 2016 in Osaka, Japan; a population‐based registry of emergency patients with both ambulance and in‐hospital records. Acute Med Surg. 2019; 6: 12–24. [DOI] [PMC free article] [PubMed] [Google Scholar]


