Editor
In the context of the ongoing COVID-19 pandemic, the field of surgical oncology demands careful crisis management considering the overall importance of timely treatment1,2. Based on an online survey (Google Forms; Google LLC, Mountain View, California, USA) conducted among university-affiliated surgical departments throughout Europe, we offer a multicentre perspective on the instantaneous performance of gastrointestinal (GI) and hepatopancreatobiliary (HPB) tumour surgery. Ninety-five surgeons from 79 surgical departments in 20 European countries completed the survey. The survey revealed an alarming status quo. Some 59 per cent of participants stated that the COVID-19 pandemic is having a strong or very strong impact on ongoing treatment of their patients (Fig. 1a).
Fig. 1.
Impact of the COVID-19 pandemic
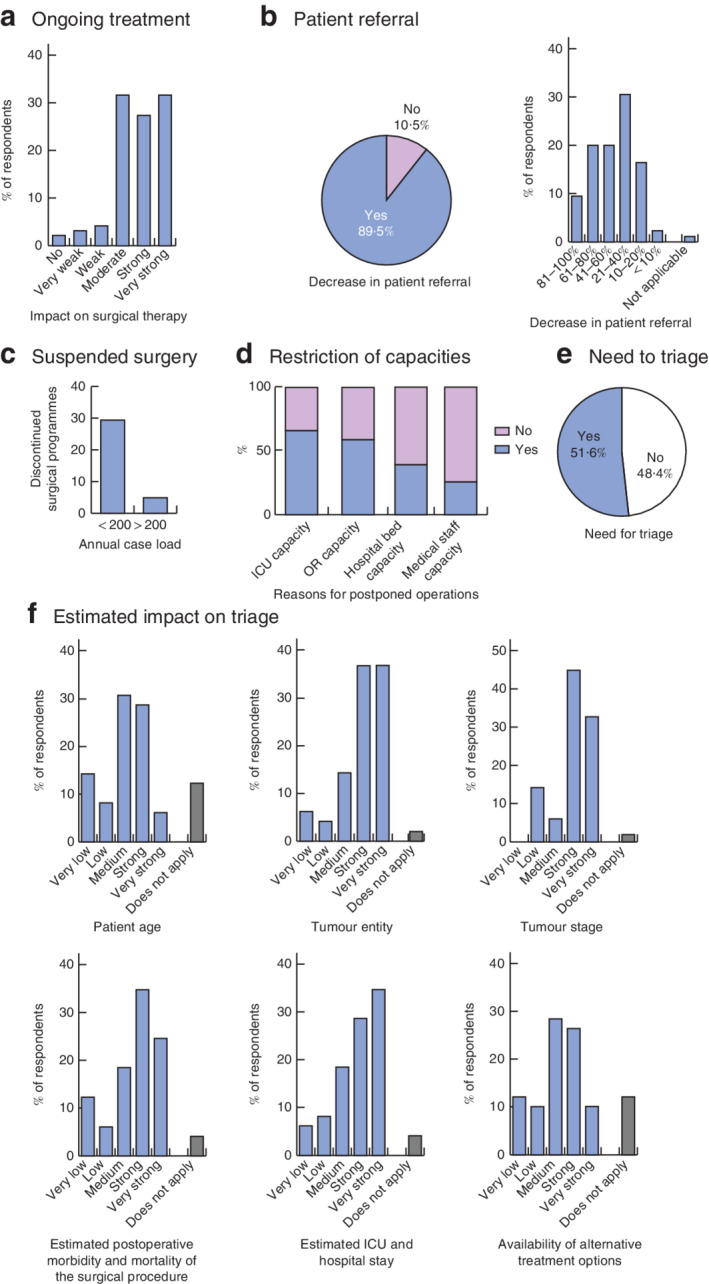
a Ongoing treatment. b Patient referral. c Suspended gastrointestinal (GI) and hepatopancreatobiliary (HPB) surgical programmes, depending on performance size of the participating departments. d Attributed relevance of individual factors on restriction of capacities. e Need to triage surgical procedures. f Estimated degree of impact of individual factors on triage. OR, operating room. c, P = 0·008.
A decrease in patient referral since onset of the viral outbreak was observed by 90 per cent of respondents. Twenty-nine per cent reported a decrease of more than 60 per cent compared to the pre-pandemic standard (Fig. 1b). In addition to a re-evaluation of hospital capacities, the excessive workload of general practitioners, the role of the media and general recommendations to avoid person-to-person contact, including medical appointments, have to be reconsidered3. It can be assumed that telemedical options are not offered sufficiently (only 12 per cent of respondents reported telemedical options for all outpatient appointments)4. Moreover, almost one-third reported that multidisciplinary tumour boards have been discontinued. Preoperative consultations and diagnostics have been postponed in 61 per cent of participants' centres, with an estimated delay of more than 1 month reported by 55 per cent.
Some 39 per cent of surgeons reported that surgical procedures for malignant HPB and GI tumours have been postponed, with 67 per cent estimating the postponement to be above 4 weeks. HPB and GI surgery has been discontinued temporarily according to 10 per cent of respondents, with a higher rate of complete suspension for smaller departments performing 200 or fewer procedures annually (P = 0·008) (Fig. 1c). The most prominent limiting factors reported were restrictions in intensive care bed and operating room capacity. Less frequently, hospital bed, surgical or nursing staff capacities were reported as limiting (Fig. 1d); 52 per cent of surgeons confirmed the need to triage surgical procedures (Fig. 1e). Factors influencing triage and their weighting are detailed in Fig. 1f. Thirty-nine per cent of participants noted that non-surgical approaches might be favoured over surgical resection.
Reduced availability of postsurgical diagnostics and adjuvant treatment was reported by many respondents. This underlines the importance of interdisciplinary crisis management. Fifty-one per cent reported that clinical trials were discontinued at least partly. The overall impact of the COVID-19 pandemic on basic or translational research was rated as strong or very strong by 71 per cent of respondents. Some 58 per cent of respondents described the overall impact of the COVID-19 pandemic on the treatment of GI and HPB tumour patients as either compromising or strongly compromising with a possible or expected negative effect on patient survival.
This survey reveals the devastating effects of the COVD-19 pandemic on oncological surgery in Europe and may serve as an impulse for a critical re-evaluation and reasonable calibration of capacity allocation with regards to the high therapeutic value of surgical oncology, especially in GI and HPB tumour patients5.
Supplementary Material
Appendix S1: Supporting Information
Acknowledgements
NFN and KHH contributed equally as first authors. MS and JP contributed equally as senior authors.
Contributor Information
COVID-19 Surgical Oncology Collaboration Group:
Mohammad Abu Hilal, Luca Aldrighetti, Roland Andersson, Vereczkei András, Andreas Andreou, İlker Murat Arer, Ali Emre Atıcı, Attila Szijártó, Ahmet Ayav, Hüseyin Onur Aydın, Detlev Bartsch, Andrea Belli, Claude Bertrand, Maximilian Bockhorn, Martin Bolli, Zdrinko Brekalo, Christiane Bruns, Ruben Ciria, Ahmet Coker, Roland Croner, Andre d'Hoore, Nicolas Demartines, Ekin Demir, Arvin Dibra, Osman Nuri Dilek, Ahmet Dogrul, Mikhail Efanov, Ela Ekmekcigil, Sefa Ergün, Marco Farsi, Stefan Fichtner-Feigl, Åsmund Fretland, Helmut Friess, Geerard Beets, Beat Gloor, Ines Gockel, Ali Kağan Gökakın, Concepción Gomez i Gavara, Stephan Gretschel, Christina Hackl, Andreas Hecker, Stefan Heinrich, Tobias Huber, Cem Ibis, Jakob R Izbicki, Christoph Kahlert, Carsten Kamphues, Selin Kapan, Geert Kazemier, Joerg Kleeff, Christian Klink, Wolfram Knoefel, Maciej Kosieradzki, Rainer Kube, Stefan Löb, Lars Maagaard Andersen, Hanno Matthaei, Jens Mittler, Mehmet Haluk Morgul, David Moszkowicz, Nermin Musanovic, Felix Nickel, Magnus Nilsson, Dietmar Öfner, Taner Oruğ, Andreas Pascher, Patrick Pessaux, Michail Radionov, Michael Raraty, Christoph Reissfelder, Rami Rhaiem, Fernando Rotellar, Fernando Rotellar, Miroslav Ryska, Santiago López-Ben, Kaya Saribeyoglu, Clemens Schafmayer, Moritz Schmelzle, Thomas Schmidt, Martin Schneider, Markus Schoenberg, Wenzel Schöning, Daniel Seehofer, Recep Erçin Sönmez, Olivier Soubrane, Daniel Stange, Benjamin Strücker, Amir Tursunovic, Acar Tüzüner, Florian Vondran, Georg Weber, Ulrich Wellner, Pinar Yazici, Cumhur Yeğen, and Sinan Yol
Reference
- 1. Spinelli A, Pellino G. COVID-19 pandemic: perspectives on an unfolding crisis. Br J Surg 2020; 10.1002/bjs.11627 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ives J, Huxtable R. Surgical ethics during a pandemic: moving into the unknown? Br J Surg 2020; 10.1002/bjs.11638 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 3. Di Marzo F, Sartelli M, Cennamo R, Toccafondi G, Coccolini F, La Torre Get al. Recommendations for general surgery activities in a pandemic scenario (SARS-CoV-2). Br J Surg 2020; 10.1002/bjs.11652 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Vogler SA, Lightner AL. Rethinking how we care for our patients in a time of social distancing. Br J Surg 2020; 10.1002/bjs.11636 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mayol J, Fernandez PC. Elective surgery after the pandemic: waves beyond the horizon. Br J Surg 2020; 10.1002/bjs.11688 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1: Supporting Information


