Abstract
Objectives
The coronavirus disease 2019 (COVID‐19) pandemic has led to widespread disruptions in the clinical education of medical students. In managing students’ return to the clinical setting, medical schools face the challenge of balancing education, service and risk considerations. To compound this challenge, medical students may prefer not to re‐enter during a period of great uncertainty, leading to substantive downstream sequelae on individual, institutional and national levels. Understanding students’ views on resuming clinical experiences, therefore, is an important consideration. The purpose of this study was to assess medical students’ preference for re‐entering the clinical setting during the COVID‐19 pandemic and to explore personal and environmental characteristics associated with that preference.
Methods
We conducted an electronic survey of currently enrolled medical students at the Duke‐NUS Medical School, less than a month into the COVID‐19 pandemic. Survey items were aligned with a conceptual framework related to medical students’ preference for returning to the clinical setting. The framework consisted of three domains: (a) non‐modifiable demographic information; (b) factors thought to be modifiable through the course of medical education, including burnout, tolerance for ambiguity, motivation and professionalism, and (c) students’ perception of COVID‐19 infection risk to self.
Results
Approximately one‐third (n=63) of 179 students preferred not to return to the clinical setting. Results of a multivariable analysis indicated that compared to this group, the two‐thirds (n=116) of students favouring return showed evidence of greater autonomous (or internal) motivation, a greater sense of professional responsibility and a lower self‐perception of harbouring risk to patients.
Conclusions
Students’ preference on returning to the clinical environment stems from the interplay of several key factors, and is substantively associated with perceptions of professional responsibility and their own potential risk to the health care system. Mindfully considering and addressing these issues may help medical schools in their preparation for returning students to the clinical setting.
Short abstract
As medical schools worldwide decide when students should return to clinical settings to continue their training, Compton et al. explore factors that predict student preferences.
1. INTRODUCTION
The Republic of Singapore identified its first case of the novel coronavirus diesease 2019 (COVID‐19) on 23 January 2020. 1 The arrival of COVID‐19 in the densely populated city‐state resulted in a swift and proactive response by Singapore's Ministry of Health, which elevated its Disease Outbreak Response System Condition (DORSCON) to ‘Orange,’ the third highest of the four DORSCON categories, on 7 February 2020. As a result, all clinical activities for medical students were paused and students’ permission to enter health care institutions suspended. The following month saw COVID‐19 become a pandemic, 2 with more countries suspending medical student clinical activities. 3 , 4 , 5
A few weeks into the COVID‐19 pandemic, the debate over whether to reintegrate medical students into a strained learning environment rages on a wide scale. 3 , 4 , 5 , 6 , 7 , 8 , 9 The rationale for suspending clinical activities during infectious disease outbreaks are manifold, requiring a balance of individual, systemic and societal considerations. These include priorities to help ‘flatten the curve,’ limit involvement in clinical care areas to ‘essential’ staff, conserve personal protective equipment (PPE), reduce exposure risk of medical students, and consider the burden of clinician educators in meeting education goals in the face of overwhelmingly increased clinical demands. 5 , 6 Some posit that as students are not health care professionals, they should not be expected to share the same exposure risks and responsibilities. This could be compounded by students’ limited clinical knowledge and capability, whereas an ill‐timed re‐entry could potentially give rise to psychological concerns, moral distress and even legal liabilities. 10 Yet others contend that clinical experiences during such times enable opportunities for learning, service, and inculcation of professional responsibilities of health care workers. 8 , 9
The challenging and multifactorial decision to resume clinical education necessitates each locality, based on its context, to conduct a risk‐benefit analysis. An important element of such an analysis is knowledge of the preference of students themselves regarding resumption of their clinical education. This information is currently lacking, representing a critical gap for medical educators, particularly pertaining to students who may prefer not to resume clinical experiences. On an individual level, such a preference may provide useful insight into a student's resilience, burnout, tolerance for uncertain situations, sense of professional identity, motivation for learning, and awareness and assessment of disease risk. From the medical school perspective, this may reflect a shortcoming of an educational programme to appropriately support students in these areas. However, it may also provide an opportunity for the school to better understand and strengthen its support of students as they continue to develop their professional identity, as well as bolstering its transparent and frequent communication of contingency plans, institutional resources and risk mitigation measures during periods of uncertainty and risk.
The ongoing COVID‐19 pandemic provides a unique opportunity to address this critical gap in an authentic real‐time setting. Therefore, the purpose of this study was to assess the prevalence of medical students’ preference for re‐entering the clinical environment during an infectious disease pandemic, and to explore personal and environmental characteristics associated with that preference. We hypothesised that students with stronger autonomous (internal) motivation or a self‐determined regulatory style for learning, higher sense of professional identity and lower perception of COVID‐19 infection risk to self, would prefer to return to the clinical learning environment.
2. METHODS
2.1. Study design
We conducted this study using survey methodology between 1 April and 8 April 2020 with approval from the National University of Singapore Institutional Review Board (IRB Reference Code: S‐20‐102).
2.2. Conceptual framework
We hypothesised a conceptual framework (Figure 1) to elucidate medical students’ preference for returning to the clinical setting during the COVID‐19 pandemic, based on four domains: (a) non‐modifiable demographic information; (b) factors thought to be modifiable through the course of medical education and therefore within the remit of medical educators, including burnout, tolerance for ambiguity, motivation and professionalism; (c) students’ perception of personal vulnerability and COVID‐19 risk to self, and (d) acknowledgement of the multifactorial nature of these decisions, including institutional influences outside the scope of this study. The conceptual framework thus formed the roadmap by which we selected the survey items.
FIGURE 1.
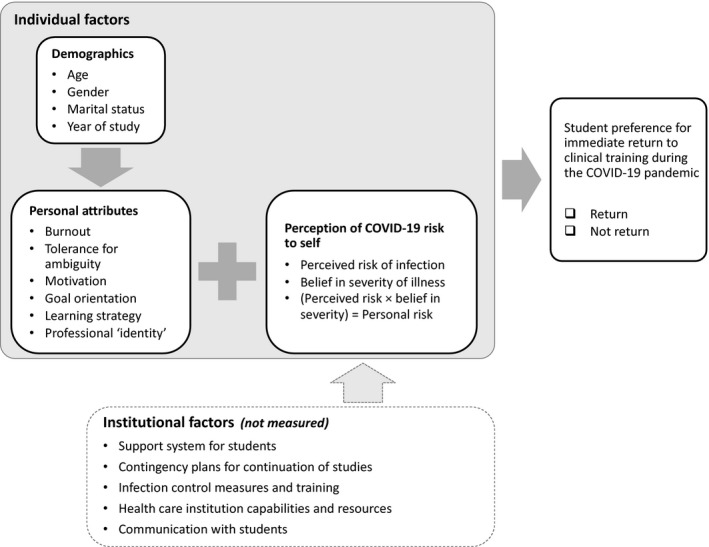
Conceptual model to elucidate medical students’ preference for returning to the clinical environment during the first month of the COVID‐19 pandemic
2.3. Participants and setting
Eligible participants were all medical students enrolled at the Duke‐NUS Medical School, which is an allopathic, graduate‐entry medical school located in the Republic of Singapore and a partnership between the Duke University School of Medicine (Durham, North Carolina) and the National University of Singapore. The curriculum structure allows for some early clinical experiences in the first year as well as predominantly focusing on pre‐clinical sciences, intensive clinical education in the second and fourth years, and a mix of research or scholarly activities and clinical education in the third year.
2.4. Historical context and timeline of communication
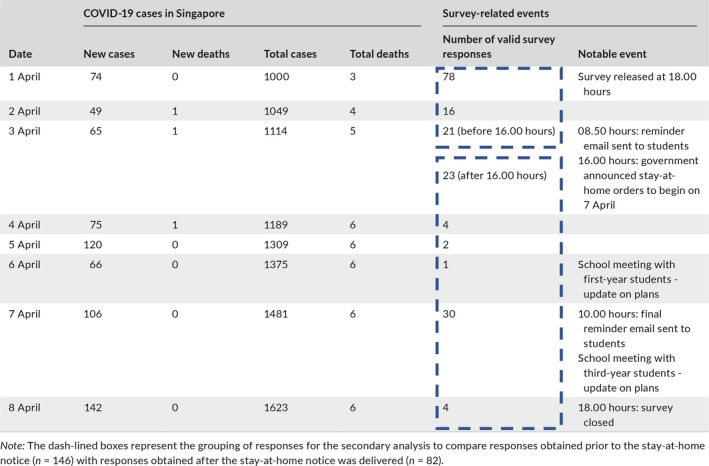
The dynamic COVID‐19 situation set in motion adaptive measures nationally and institutionally. To account for how those changes may have impacted student perceptions, we logged the historical events during the period of data collection, as shown in Table 1.
TABLE 1.
Historical context of data collection period
2.5. Measures and survey development
We developed an anonymous online questionnaire to assess each domain within the conceptual framework (Figure 1), using the following tools: (i) the Oldenburg Burnout Inventory for Medical Students Scale 11 to measure the domains of exhaustion and disengagement; (ii) the Tolerance for Ambiguity Scale 12 to assess ability to cope with situations of uncertainty; (iii) a Modified Treatment Self‐Regulation Questionnaire (TSRQ) 13 to measure the degree to which motivation is intrinsic (autonomous), extrinsic (controlled) or absent (amotivation); (iv) the Modified Archer's Health Promotions Motivation Survey (MAHPMS) 14 to examine students’ learning goal orientation (‘mastery’ orientation, with a focus on developing in‐depth understanding in order to move closer towards expertise or ‘mastery’; ‘performance’ orientation, whereby a student has an eye on perceived favourable recognition for his or her competence; and ‘avoidance’ of learning altogether, as a means to evade the perception of incompetence), as well as metacognitive versus non‐metacognitive learning strategies, the former promoting learning through reflection on experiences rather than reliance of rote memorisation, signifying confidence in one's ability to succeed when learning 14 , 15 ; (v) an author‐developed measure of professionalism related to the COVID‐19 pandemic, and (vi) the perception of COVID‐19 risk to self, as the likelihood of becoming infected upon resuming clinical work and incurring critical risk to life, as guided by the theory of planned behaviour. 16
2.6. Survey dissemination
We sent an email invitation to all eligible students, with a participation information sheet and a link to complete the self‐administered questionnaire. We followed this with two reminder emails during the week to request participation from eligible students who had not yet completed the survey.
2.7. Data analysis
To assess medical students’ preference for re‐entering the clinical setting during an infectious disease pandemic, and to explore personal and environmental characteristics associated with that preference, we first determined a point estimate and associated 95% confidence intervals (CIs) for the number of students who would prefer to re‐enter the clinical setting at that time. We subsequently identified potential factors associated with students’ preference by comparing categorical variables (eg, demographic data) and continuous variables (eg, tolerance for ambiguity) between groups of students who voiced a preference to return or not return to the clinical setting, using chi‐squared independent samples t tests, or Wilcoxon rank sums tests as appropriate. We retained associated factors with a p‐value less than 0.10 for a multivariable analysis to determine the explanatory contribution of those variables in terms of students’ preference to not return, using binary logistic regression with a backward conditional stepwise entry method. All analyses were conducted using SPSS statistical package Version 26 (IBM Corp., Armonk, NY, USA).
3. RESULTS
There are 262 enrolled medical students in the Duke‐NUS Medical School. Having initially received 228 anonymous survey responses, we carefully reviewed each for a minimally acceptable level of completion, requiring the respondent's year of study and his or her preference for returning to the clinical setting. This was done to achieve the first specific aim of assessing the prevalence of medical students’ preferences for re‐entering the clinical setting. This process removed 38 responses. Next, we examined each response for evidence of uniqueness, to minimise the risk that a single student submitted multiple responses. We identified cases of duplication based on internet protocol addresses, postal codes, browser types and device types matches, all of which were recorded on the survey platform. Through this process, we removed 11 cases due to a suspicion of multiple responses. In these cases, we chose the most complete, or the most recent entry if both were of similar levels of completion. Thus, the overall number of valid cases was 179, yielding a response rate of 68.3% for this survey.
As shown in Table 2, of the 179 valid respondents, 116 (64.8%; 95% CI, 60.9% to 68.8%) expressed a preference to return to the clinical setting if given the option. To further assess the robustness of this point estimate, we conducted a best‐case and worst‐case analysis to account for the possibility of a response bias of all non‐respondents preferring to return or not return, yielding a potential range of 55.7% to 80.0%. The preference to return varied by year of study, with students in their second year (ie, the first clinical clerkship year in our curriculum) being the least likely to prefer to return.
TABLE 2.
Overall respondent demographics and comparisons between preference to return or not return
|
Overall Mean rating ± SD (n = 179) |
Student preferences | P‐value | ||
|---|---|---|---|---|
| Return | Not return | |||
| Mean rating ± SD (n = 116) | Mean rating ± SD (n = 63) | |||
| Gender, n (%) | ||||
| Male | 81 (45.3) | 56 (69.1) | 25 (30.9) | .270 |
| Female | 98 (54.7) | 60 (61.2) | 38 (38.8) | |
| Year of study, n (%) | ||||
| Year 1 | 52 (29.1) | 35 (67.3) | 17 (32.7) | |
| Year 2 | 47 (26.3) | 22 (46.8) | 25 (53.2) | .015 |
| Year 3 | 31 (17.3) | 21 (67.7) | 10 (32.3) | |
| Year 4 | 49 (27.4) | 38 (77.6) | 11 (22.4) | |
| Age | 27.8 (3.1) | 28.2 (3.2) | 27.2 (2.8) | .046 |
| Marital status, n (%) | ||||
| Married | 32 (18.2) | 22 (68.8) | 10 (31.3) | .553 |
| Not married | 144 (81.8) | 91 (63.2) | 53 (36.8) | |
| Have children, n (%) | ||||
| Yes | 12 (6.8) | 9 (75.0) | 3 (25.0) | .419 |
| No | 164 (93.2) | 104 (63.4) | 60 (36.6) | |
| Citizenship, n (%) | ||||
| Singaporean | 126 (71.6) | 81 (64.3) | 45 (35.7) | .528 |
| Singapore Permanent Resident (SG) permanent resident | 13 (7.4) | 10 (76.9) | 3 (23.1) | |
| Other | 37 (21.0) | 22 (59.5) | 15 (40.5) | |
| Lives with at least 1 parent, n (%) | ||||
| Yes | 113 (63.8) | 75 (66.4) | 38 (33.6) | .468 |
| No | 64 (36.2) | 39 (60.9) | 25 (39.1) | |
All percentages are displayed as valid percentages (where non‐responders are not included in denominator).
Abbreviation: SD, standard deviation.
We computed a ‘personal risk’ score for each student by taking the product of his or her rating of perceived risk of infection (to self) and belief in the severity of associated illness. 16 We found that students who preferred to not return had a significantly higher perception of their personal risk (P < .001).
Aligned with the conceptual framework, we compared responses based on return or not return, in terms of ratings on items related to burnout, tolerance for ambiguity, motivation, learning goal‐orientation, learning strategies and professional identity. As shown in Table 3, students who preferred to not return displayed significantly lower ratings on professional identity, and conversely, higher ratings on items related to concern over causing harm to patients or the health care system. Although respondents did not differ on measures of burnout or tolerance for ambiguity, there were two subdomains where student responses notably differed: (a) autonomous motivation, and (b) metacognitive learning strategy.
TABLE 3.
Personal attributes and risk perception of respondents based on preference to return or not return
| Modifiable variables | Student preferences | P‐value | |
|---|---|---|---|
| Return | Not return | ||
| Mean rating ± SD (n = 116) | Mean rating ± SD (n = 63) | ||
| Oldenburg Burnout Inventory for Medical Students | |||
| Exhaustion | 14.05 (2.1) | 14.45 (1.9) | .227 |
| Disengagement | 13.58 (2.2) | 13.73 (2.4) | .692 |
| Tolerance for ambiguity a | 26.39 (5.8) | 26.54 (5.2) | .874 |
| Modified Treatment Self‐Regulation Questionnaire (TSRQ) | |||
| Autonomous motivation | 29.88 (4.1) | 23.1 (5.3) | <.001 |
| Controlled motivation | 15.00 (5.8) | 13.53 (5.9) | .129 |
| Amotivation | 6.52 (2.9) | 7.20 (3.1) | .173 |
| Health Professions Motivation Survey | |||
| Goal orientation | |||
| Mastery | 4.18 (0.4) | 4.02 (0.3) | .005 |
| Performance | 3.69 (0.5) | 3.74 (0.6) | .446 |
| Alienation | 2.65 (0.6) | 2.79 (0.6) | .161 |
| Learning strategy | |||
| Metacognitive | 3.57 (0.5) | 3.40 (0.5) | .052 |
| Non‐metacognitive | 2.63 (0.4) | 2.63 (0.4) | .905 |
| Professionalism | |||
| Reasons to return b | |||
| Returning to the clinical setting during DORSCON code orange is important to me because … | |||
| It is part of my professional responsibility | 3.38 (0.6) | 2.61 (0.7) | <.001 |
| It is a chance to help provide care to patients | 3.32 (0.6) | 2.63 (0.7) | <.001 |
| I want to be responsive to the needs of patients | 3.35 (0.5) | 2.77 (0.7) | <.001 |
| It is a chance for me to improve my clinical capacity | 3.56 (0.5) | 2.71 (0.8) | <.001 |
| I am part of the team, therefore I should be there | 3.14 (0.7) | 2.38 (0.7) | <.001 |
| It is part of my social responsibility to help the most vulnerable when needed | 3.41 (0.5) | 2.72 (0.7) | <.001 |
| It is part of my moral obligation | 3.30 (0.6) | 2.67 (0.7) | <.001 |
| Reasons to not return b | |||
| I should not return to the clinical setting during DORSCON code orange because … | |||
| I don't want to be a drain on clinicians' time | 2.89 (0.7) | 3.42 (0.7) | <.001 |
| I don't want to be a possible vector of infection | 2.89 (0.8) | 3.56 (0.6) | <.001 |
| I want to reduce possible risks to patients as I am not trained | 2.82 (0.8) | 3.56 (0.6) | <.001 |
| Perception of COVID‐19 risk to self | ||||
|---|---|---|---|---|
|
Overall Mean rating ± SD (n = 179) |
Mean rating ± SD (n = 116) | Mean rating ± SD (n = 63) | P‐value | |
| Perceived risk of infection | ||||
| If you were to return to the clinical setting right now, how likely do you believe it would be for you to become infected by COVID‐19? b | 2.84 (0.7) | 2.69 (0.7) | 3.13 (0.7) | <.001 |
| Belief in severity of illness | ||||
| If you were to become infected by COVID‐19, how likely do you believe that it would result in a critical risk to your life? b | 2.64 (0.7) | 2.54 (0.7) | 2.82 (0.8) | .006 |
| Computed ‘personal risk’ score = perceived risk of infection × belief in severity of illness | 7.7 (3.5) | 7.0 (3.1) | 9.1 (3.8) | <.001 |
Higher scores are correlated with higher tolerance for ambiguity.
Measured on a scale of 1 = strongly disagree to 4 = strongly agree; means are shown for ease of interpretation, however P‐values were obtained from non‐parametric tests.
Abbreviations: DORSCON, Disease Outbreak Response System Condition; SD, standard deviation.
We entered all variables that differed between response groups at the P < .10 level into a multivariable logistic regression model, in order to identify the subset of variables most explanatory for differentiating students by return or not return preference. As shown in Table 4, the final multivariable model consisted of three variables, two of which were related to professionalism and one related to autonomous motivation. The final model fit of the data yielded an area under the receiver operating curve of 90.5%.
TABLE 4.
Binary logistic regression for explaining preference not to return to clinical setting
| B | Standard error (SE) | Wald | df | P‐value | Odds ratio (95% CI) | |
|---|---|---|---|---|---|---|
| Final model | ||||||
| Constant | 5.513 | 2.082 | 7.011 | 1 | .008 | 247.93 |
| It is part of my professional responsibility | −1.252 | 0.453 | 7.652 | 1 | .006 | 0.286 (0.118; 0.694) |
| I want to reduce possible risks to a patient as I am not trained | 1.232 | 0.369 | 11.122 | 1 | .001 | 3.428 (1.662; 7.071) |
| Autonomous motivation | −0.236 | 0.066 | 12.951 | 1 | <.001 | 0.790 (0.694; 0.898) |
Variables entered at Step 1: year of study; age; personal risk score; ‘It is part of my professional responsibility’; ‘It is a chance to help provide care to patients’; ‘I want to be responsive to the needs of patients’; ‘It is a chance for me to improve my clinical capacity’; ‘I am part of the team, therefore I should be there’; ‘It is part of my social responsibility to help the most vulnerable when needed’; ‘It is part of my moral obligation’; ‘I don't want to be a drain on clinicians’ time’; ‘I don't want to be a possible vector of infection’; ‘I want to reduce possible risks to patients as I am not trained’; (Modified Treatment Self‐Regulation Questionnaire) autonomous motivation; (Modified Archer's Health Promotions Motivation Survey) mastery goal‐orientation. Abbreviations: CI, confidence interval; df, degrees of freedom.
We conducted additional analyses to assess the impact of historical factors during the data collection period. Of note, approximately 46 hours after the initiation of data collection, the Singapore government announced a nationwide ‘Circuit Breaker’ plan with enhanced social distancing and stay‐at‐home measures. We hypothesised at the time of the announcement that this historical event would negatively impact the students’ preference to return. Therefore, we analysed the responses received before the announcement (n = 116) and after (n = 63), but found no evidence to suggest that the preference to return was impacted by the announcement (before = 65.5%; after = 61.9%; P = .630).
4. DISCUSSION
This study was conducted less than a month following the World Health Organization's declaration of the COVID‐19 pandemic, during rapidly evolving conditions where clinical education was paused in many locations globally. Under these conditions, we found that overall, approximately one‐third (n=63) of our students preferred not to return to the clinical education setting. Compared to this group, the two‐thirds (n=116) of students favouring return showed higher scores for autonomous (or internal) motivation and sense of professional responsibility, and a lower self‐perception of harbouring risk to patients. Based on these three variables, we were able to accurately predict responses relating to return or not return preferences, suggesting that beyond statistical significance, these variables were substantively related to the preference. To our knowledge, this is the first report examining this issue.
Students’ preference to return or not return can be viewed through different lenses. Students who preferred to not return appear concerned about introducing possible risks to patients, as they are ‘not trained.’ The return cohort did not consider this as much of a prohibitive factor to resuming clinical experiences, perhaps because this group's perceived level of personal risk was also lower than that of the not return group. Perceived risk, however, may be based on many factors, including, but not limited to, knowledge of the disease or consideration of personal underlying medical issues such as diabetes or asthma. Thus, it is unclear if students’ personal risk assessment is based on an accurate understanding of COVID‐19 or of their personal health.
Students in the return group also scored significantly higher in their response to the rationale ‘It is part of my professional responsibility.’ This is consistent with students’ desire to be held to the high ethical standards of medical professionals 17 and to be part of the medical team. 8 Developing clinical capabilities 6 and forming professional identity are closely intertwined with effective supervision, role modelling and reflective learning, 5 essential factors, which at present are being balanced against wider societal needs. Understanding student responses under these conditions may identify a nuanced relationship between his or her perceptions of self‐risk as a marker for severity of disease of patients, and by extension, the appropriateness of adding potential risk into the health care system, such as by having medical students return to a taxed clinical setting. We did not find any difference between the two groups with respect to burnout or tolerance for ambiguity, and ruled out these variables from having influenced students’ stated preference.
When analysing motivation as a self‐regulatory factor critical to learning, it was unsurprising to find a higher autonomous or intrinsic motivation in the return preference group, indicating a higher degree of a self‐determined regulatory style for learning. We additionally examined students’ goal orientation (mastery, performance or avoidance) as a reflection of their driving mechanism for learning. The higher mastery goal orientation (over performance or alienation) amongst the student population as a whole, is consistent with that amongst other health professions learners. 14 When analysing students’ learning strategies, we found a higher trend towards metacognitive strategies in the return group, although the difference compared to the not return cohort was not statistically significant (P = .052).
4.1. Limitations
Although the results of this study identify information for medical schools to consider, we recognise the limitations of this study. This is a single‐institution study with demographic and cultural features that may not be generalisable to other populations. Further, as a quantitative survey approach, we were limited in our ability to deeply explore the rationale behind students’ responses, which may be more complex than the general domains that we incorporated into our conceptual framework. Future qualitative research in this area could better elucidate the impact of the COVID‐19 pandemic on medical students’ professional identity formation.
Based on our findings, we posit that even in the absence of student choice, medical education programmes can use students’ input to positively influence modifiable factors in order to bolster their support and preparation of students’ return to the clinical setting. These may include steps to promote students’ professional identity formation through reflective opportunities, inculcate autonomous motivation by emphasising not short‐term gains such as performance in examinations but long‐term efforts and outcomes, real‐life examples of which abound on the frontlines, and prioritise student understanding of risk mitigation and infection control measures, including PPE training. We acknowledge that this may not have been as significant an issue for our population, where PPE is not in short supply, as compared to the situation across many settings globally where the lack of PPE availability may prohibit the return of students to the clinical setting.
5. CONCLUSIONS
Medical schools and health care institutions face the challenge of balancing education, service and risk considerations for students in the clinical environment, often with limited information. Knowledge of student perceptions and preferences adds an additional perspective to help guide deliberations under exceptional and evolving circumstances.
AUTHOR CONTRIBUTIONS
SC conceived and designed the study, acquired and analysed data, drafted the manuscript and tables, and approved the final version of the manuscript. SS‐Y conceived and designed the study, drafted the manuscript and figures, and approved the final version of the manuscript. FR conceived and designed the study, acquired and analysed data, drafted the manuscript and approved the final version of the manuscript. LKRK conceived and designed the study, drafted the manuscript and approved the final version of the manuscript. All authors (SC, SS‐Y, FR and LKRK) are accountable for all aspects of the work.
CONFLICTS OF INTEREST
The authors have no competing interests regarding this paper or the topic of this paper.
ETHICAL APPROVAL
This project was approved by the National University of Singapore Institutional Review Board (IRB Reference Code: S‐20‐102).
ACKNOWLEDGEMENTS
None.
Compton S, Sarraf-Yazdi S, Rustandy F, Krishna LKR. Medical students’ preference for returning to the clinical setting during the COVID‐19 pandemic. Med Educ. 2020;54:943–950. 10.1111/medu.14268
REFERENCES
- 1. Wong JEL, Leo YS, Tan CC. COVID‐19 in Singapore ‐ current experience. JAMA. 2020;323(13):1243‐1244. [DOI] [PubMed] [Google Scholar]
- 2. World Health Organization (WHO) . Coronavirus disease (COVID‐19) outbreak: statements, press and ministerial briefings. [WHO website]. http://www.euro.who.int/en/health‐topics/health‐emergencies/coronavirus‐covid‐19/statements. Accessed April 10, 2020
- 3. Whelan A, Prescott J, Young G, Catanese VM, McKinney R. COVID‐19: Updated guidance for medical students' roles in direct patient care. [AAMC website]. April 14, 2020. https://www.aamc.org/news‐insights/press‐releases/updated‐guidance‐medical‐students‐participation‐direct‐patient‐care‐during‐coronavirus‐covid‐19. April 14, 2020. Accessed April 15, 2020
- 4. Australian Medical Students' Association (AMSA) . AMSA COVID‐19 response. [AMSA website]. https://www.amsa.org.au/amsa‐covid‐19‐response. Accessed April 10, 2020
- 5. Rose S. Medical student education in the time of COVID‐19. JAMA. 2020;323(21):2131‐2132. [DOI] [PubMed] [Google Scholar]
- 6. Ferrel MN, Ryan JJ. The impact of COVID‐19 on medical education. Cureus. 2020;12(3):e7492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bauchner H, Sharfstein J. A bold response to the COVID‐19 pandemic: medical students, national service, and public health. JAMA. 2020;323(18):1790‐1791. [DOI] [PubMed] [Google Scholar]
- 8. Brodar C. Should medical students continue clinical rotations during the COVID‐19 pandemic? [in‐Training website]. March 17, 2020. https://in‐training.org/should‐medical‐students‐continue‐clinical‐rotations‐during‐a‐pandemic‐19371. Published March 17, 2020. Accessed April 15, 2020
- 9. Chema A. The professional obligations of medical students in COVID‐19 responses. [Bioethics.net website]. March 23, 2020. http://www.bioethics.net/2020/03/the‐professional‐obligations‐of‐medical‐students‐in‐covid‐19‐responses/. Published March 23, 2020. Accessed April 15, 2020
- 10. Adams JG, Walls RM. Supporting the health care workforce during the COVID‐19 global epidemic. JAMA. 2020;323(15):1439. [DOI] [PubMed] [Google Scholar]
- 11. Demerouti E, Bakker AB, Nachreiner F, Schaufeli WB. Burnout inventory for medical students. The job demands‐resources model of burnout. J Appl Psychol. 2001;86(3):499‐512. [PubMed] [Google Scholar]
- 12. Geller G, Tambor ES, Chase GA, Holtzman NA. Measuring physicians’ tolerance for ambiguity and its relationship to their reported practices regarding genetic testing. Med Care. 1993;31(11):989‐1001. [DOI] [PubMed] [Google Scholar]
- 13. Levesque CS, Williams GC, Elliot D, Pickering MA, Bodenhamer B, Finley PJ. Validating the theoretical structure of the Treatment Self‐Regulation Questionnaire (TSRQ) across three different health behaviors. Health Educ Res. 2007;22(5):691‐702. [DOI] [PubMed] [Google Scholar]
- 14. Perrot L, Deloney L. An instrument to measure health professional motivation ‐ description and review. MedEdPORTAL. 2013;9:9406. [Google Scholar]
- 15. Perrot L, Deloney LA, Hastings JK, Savell S, Savidge M. Measuring student motivation in health professions' colleges. Adv Health Sci Educ Theory Pract. 2001;6(3):193‐203. [DOI] [PubMed] [Google Scholar]
- 16. Francis J, Eccles MP, Johnston M, et al. Constructing Questionnaires Based on the Theory of Planned Behaviour: A Manual for Health Services Researchers. Newcastle upon Tyne, UK: Centre for Health Services Research, University of Newcastle upon Tyne; 2004. [Google Scholar]
- 17. Zuger A, Miles SH. Physicians, AIDS, and occupational risk: historic traditions and ethical obligations. JAMA. 1987;258(14):1924‐1928. [PubMed] [Google Scholar]


