Abstract
Patients with chronic liver disease and patients after solid organ transplantation (SOT) are vulnerable to severe coronavirus disease 2019 (COVID-19). We evaluated fears, attitudes, and opinions associated with COVID-19 in 365 SOT recipients (95% liver, 5% pancreas/kidney), 112 SOT candidates, and 394 immediate household contacts in 2 German transplant centers. Seven (1.5%) patients and 10 (2.5%) controls had contact with confirmed COVID-19 cases. Fear of infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was expressed by 65% of SOT recipients and by 55% of SOT candidates. SOT recipients had higher levels of fear of infection and more often wore personal protective gear than household controls. Female sex, steroid treatment, and using the local newspaper as a primary source of information were independently associated with expressed fear of infection in SOT recipients. Younger age and more recent transplantation correlated with concerns about severe COVID-19 expressed by patients and with concerns about worse medical care expressed by household controls. One third of the patients expressed fear that immunosuppression could worsen COVID-19 but only 15% used the transplantation center as a source of information. These data show that fears associated with the SARS-CoV-2 pandemic are frequently expressed but measures to prevent infection are regularly followed by patients before and after SOT.
KEYWORDS: cirrhosis, clinical research/ practice, infection and infectious agents – viral, liver disease, liver transplantation/ hepatology, outpatient care, patient safety
1. INTRODUCTION
In December 2019, a new form of severe acute respiratory syndrome (SARS) was described in Wuhan, China, and eventually a new coronavirus (SARS-CoV-2) was discovered as the causative pathogen.1 In March 2020, after a worldwide spread, SARS-CoV-2 was announced a global pandemic by the World Health Organization.2 In the following weeks, more than 4.5 million people became infected and more than 300 000 people died following an infection with SARS-CoV-2.3 Governments in different countries have responded with varying levels of social restrictions ranging from bans of assembly to complete lockdowns.4
The coronavirus disease 2019 (COVID-19) presents with cough, fever, myalgia, headache, and can cause respiratory failure with the need for mechanical ventilation, hemodialysis, extracorporeal perfusion techniques, and significant mortality.5 Although the majority of patients present with a mild or even asymptomatic course of the infection,6 patients with obesity and existing cardiovascular and pulmonary comorbidities are reported to be at a higher risk for a severe disease course.7
Patients with chronic liver disease and liver transplant recipients represent vulnerable patient cohorts at increased risk of bacterial, fungal, and viral infection. Although there are reports that patients with nonalcoholic fatty liver disease (NAFLD) are at higher risk for a progressive course of COVID-19,8 until now it remains unclear to what extent chronic liver disease should be considered a risk factor for SARS-CoV-2 infection and complicated courses of COVID-19.9 , 10 Whether medical immunosuppression or preexisting comorbidities contribute to COVID-19-related mortality after liver transplantation is currently a subject of debate.11 , 12 Reflecting on past SARS-CoV and the middle east respiratory syndrome coronavirus (MERS-CoV) outbreaks, there is no conclusive evidence that immunosuppression in patients after solid organ transplantation (SOT) is associated with poor outcome.13 Thus, the reduction of immunosuppression is not recommended in patients with autoimmune liver disease and after liver transplantation.14 , 15
Despite such recommendations, the uncertainty regarding the COVID-19 risk after liver transplantation and on the waiting list is evident from our experience in outpatient clinics. However, to date, there is little known about how the COVID-19 pandemic has affected the behavior and daily lives of patients before and after liver transplantation. Thus, we assessed COVID-19 prevalence/exposure, perception, compliance, and behavior of transplant recipients and candidates on the waiting list in 2 German liver transplant centers in April 2020 using a cross-sectional anonymous survey in patients and their household members.
2. MATERIALS AND METHODS
2.1. Patient recruitment
Patients who underwent liver or pancreas/kidney transplantation or candidates on the waiting list were identified in 2 German transplant centers: Jena University Hospital, Thuringia, and Aachen University Hospital, North-Rhine-Westphalia. A self-report questionnaire was designed and sent to patients by mail between April 14 and April 21, 2020. The study was conducted according to the Declaration of Helsinki. It was approved by the local ethics committees (2020-1733-Reg; EK121/20) and patients provided written informed consent. Only questionnaires returned by April 30, 2020 were considered for analysis.
2.2. Questionnaire
The survey consisted of demographic data (age, sex, educational status, and profession), preexisting medical conditions including transplantation status (year of transplantation, waiting list status), current immunosuppressive therapy after transplantation, flu vaccination status, and smoking status. Participants were asked to select their 2 most important information sources concerning the coronavirus out of 10 options. The participants were asked 12 items about their fears of being infected with SARS-CoV-2 and changes in their behavior using a 5-point Likert scale. They were also surveyed regarding their infection status, adherence to medication, personal protection equipment (eg, face masks covering mouth and nose and gloves in Germany), and contacts with their physician. The participants were asked to have a household member (spouse, next of kin) complete a control questionnaire. For an English translation of the questionnaires see Data S1.
2.3. Statistical analysis
Statistical differences between paired data (for example, patients and controls) were analyzed using the Wilcoxon Signed-Rank test for continuous and ordinal data or the McNemar test for nominal data. Statistical differences between unpaired data (for example, organ transplant candidates and recipients) were assessed using the Mann-Whitney U test for continuous or ordinal data and Fisher’s Exact test for nominal data. Correlations between the baseline characteristics and the items on the 5-item Likert scale were assessed using Spearman’s nonparametric correlation. Statistical analysis was performed using SPSS versions 16 and 26 (IBM Inc, Armonk, NY, USA). Data visualization was performed using Prism 6 (GraphPad Software, LaJolla, CA, USA). P < .05 in 2-sided tests was considered statistically significant. We did not correct for multiple comparisons. Items with missing data were removed from the respective analysis.
3. RESULTS
3.1. Survey participants
The questionnaire was sent out to 948 patients including 725 SOT recipients and 223 patients on the waiting list. Overall, 481 (51%) patients returned the questionnaire on time. After excluding patients who did not specify pre- or posttransplantation state, 365 organ transplant recipients, 112 transplant candidates, and 394 matched household controls were analyzed. Ninety-five percent of patients returning the questionnaire were liver transplant recipients or candidates. The majority of patients were male and the majority of immediate household contacts were female, suggesting that the spouse answered the questionnaire in the majority of controls ( Table 1). In organ transplant recipients, the most frequent liver disease was alcoholic liver disease (ALD) followed by NAFLD and “other or cryptogenic” liver disease comprising “hepatocellular carcinoma” and “cirrhosis of the liver” without further specification of liver disease by the patients. In patients on the waiting list, ALD was the most frequent diagnosis (47 patients, 45%). Comorbidities are provided in Table 1.
TABLE 1.
Subject characteristics
| Organ transplant recipients | Organ transplant candidates on the waiting list | |||
|---|---|---|---|---|
| Patients | Household controls | Patients | Household controls | |
| Total subjects | 365 | 306 | 112 | 88 |
| Age (y) | 62 (53-67) | 59 (50-65)* | 58 (52-64) | 59 (54-66) |
| Male sex (%) | 224/362 (62) | 107/301 (36)* | 75/112 (67) | 30/85 (35)* |
| Highest level of education (%) | n = 352 | n = 293 | n = 109 | n = 86 |
| Secondary school (9 y) | 72 (20) | 58 (20) | 20 (18) | 20 (23) |
| Secondary school (10 y) | 156 (44) | 120 (41) | 59 (54) | 42 (49) |
| High school (12-13 y) | 27 (8) | 41 (11) | 7 (6) | 5 (6) |
| University | 97 (28) | 74 (20) | 23 (21) | 19 (22) |
| Liver disease (%) | n = 326 | n = 306 | n = 105 | n = 88 |
| ALD | 64 (20) | 4 (1) | 47 (45) | 2 (2) |
| NAFLD | 36 (11) | 8 (3) | 11 (10) | 3 (3) |
| HBV | 24 (7) | 4 (1) | 7 (7) | 1 (1) |
| HCV | 13 (4) | 2 (1) | 2 (2) | 0 |
| PBC/PSC | 25 (8) | 0 | 10 (10) | 0 |
| Autoimmune | 11 (3) | 0 | 8 (8) | 0 |
| Hemochromatosis | 11 (3) | 1 (0) | 0 | 0 |
| Wilson’s disease | 2 (1) | 0 | 0 | 0 |
| Other/cryptogenic | 140 (43) | 3 (1) | 20 (19) | 0 |
| Pulmonary comorbidity (%) | n = 364 | n = 306 | n = 112 | n = 88 |
| Asthma | 12 (3) | 17 (6) | 4 (4) | 7 (8) |
| COPD | 19 (5) | 7 (2) | 4 (4) | 2 (2) |
| Other | 13 (4) | 6 (2) | 2 (2) | 0 |
| Cardiovascular comorbidity (%) | n = 364 | n = 306 | n = 112 | n = 88 |
| Coronary heart disease | 26 (7) | 13 (4)* | 3 (3) | 2 (2) |
| Arterial hypertension | 125 (34) | 82 (27) | 29 (26) | 21 (24) |
| Other | 7(2) | 6 (2) | 0 | 7 (8) |
| Diabetes mellitus (%) | n = 364 | n = 306 | n = 112 | n = 88 |
| Type 1 | 25 (7) | 3 (1) | 5 (4) | 4 (5) |
| Type 2 | 100 (27) | 20 (7)* | 34 (30) | 10 (11)* |
| Kidney disease (%) | n = 364 | n = 306 | n = 112 | n = 88 |
| Chronic kidney disease | 96 (26) | 7 (2) | 11 (10) | 1 (1) |
| Polycystic kidney disease | 18 (5) | 2 (1) | 3 (3) | 0 |
| Dialysis | 13 (4) | 0 | 5 (4) | 0 |
| Organ (to be) transplanted (%) | n = 355 | n = 111 | ||
| Liver | 336 (95) | N/A | 106 (95) | N/A |
| Pancreas and kidney | 19 (5) | 5 (5) | ||
| Current smoker (%) | 50/361 (14) | 57/296 (19)* | 20/109 (18) | 16/84 (19) |
| Vaccinated against influenza (%) | 222/364 (61) | 147/297 (49)* | 74/111 (67) | 43/86 (50)* |
| Immunosuppression (%) | n = 359 | |||
| Steroids (%) | 69 (19) | N/A | N/A | N/A |
| Mycophenolate mofetil (%) | 99 (28) | |||
| Calcineurin inhibitors (%) | 306 (85) | |||
| mTOR inhibitors (%) | 78 (22) | |||
| Wearing personal protective gear (gloves/face mask) when leaving the house (%) | 281/360 (78) | 191/299 (64)* | 77/110 (70) | 51/84 (61) |
| Washing hands more frequently than before COVID-19 (%) | 335/362 (93) | 285/296 (96) | 102/110 (93) | 84/85 (99) |
| COVID-19 contact (%) | 7 (2) | 7 (2) | 0 | 3 (4) |
| Infection with SARS-CoV-2 (%) | 1 (0.3) | 0 | 0 | 0 |
Note. Baseline characteristics are depicted as frequencies or medians with interquartiles.
Abbreviations: ALD, alcoholic liver disease; COPD, chronic obstructive pulmonary disease; COVID-19, coronavirus 19; HBV, hepatitis B virus; HCV, hepatitis C virus; mTOR, mammalian target of rapamycin; N/A, not applicable; NAFLD, nonalcoholic fatty liver disease; PBC, primary biliary cirrhosis; PSC, primary sclerosing cholangitis; SARS-CoV-2, severe acute respiratory syndrome coronavirus-2.
P < .05 from Wilcoxon Signed-Rank test or McNemar test comparing patients and their household controls. Total number of responses are indicated for each item.
The median time since transplantation was 6 years (interquartile range 2-9). Eighty-five percent of transplant recipients reported calcineurin inhibitors, 21% mammalian target of rapamycin inhibitors, 28% mycophenolate mofetil, and 19% steroids being part of immunosuppression. Thirty percent received dual immunosuppression and 12% triple immunosuppression.
3.2. Exposure and behavioral changes associated with COVID-19
Seven (1.5%) patients and 10 (2.5%) household controls had contact with confirmed COVID-19 cases. Only 1 liver transplant recipient reported being tested positive for SARS-CoV-2 (Table 1). Seventy-nine percent of the organ transplant recipients and 72% of organ transplant candidates “rather agreed” or “agreed” about the statement that they were leaving the house less frequently than before the COVID-19 pandemic. This was significantly higher than in controls (58% and 59%, respectively) (Table S1). The majority of patients and controls reported wearing gloves and/or face mask when leaving the house, and there were no statistical differences between organ transplant recipients (78%) and patients on the waiting list (70%, P = .10). However, organ transplant recipients used personal protective equipment significantly more frequently than their controls (64%, P = .004). The vast majority of patients and controls reported washing their hands more frequently than before the COVID-19 pandemic, ranging from 93% in organ transplant recipients and patients on the waiting list to 99% in household controls of waiting list patients (Table 1). One liver transplant recipient reported to have unadvisedly reduced immunosuppressive therapy.
3.3. Information, emotions, and attitudes associated with COVID-19
The majority of patients felt informed about COVID-19. About 80% of patients and controls reported to “agree” or “rather agree” in response to the item “I feel sufficiently informed about the Coronavirus Pandemic” without any differences between the groups. In contrast, only about 60% of patients and controls reported being sufficiently informed about the influence of the coronavirus on chronic diseases and transplanted patients (Table S1).
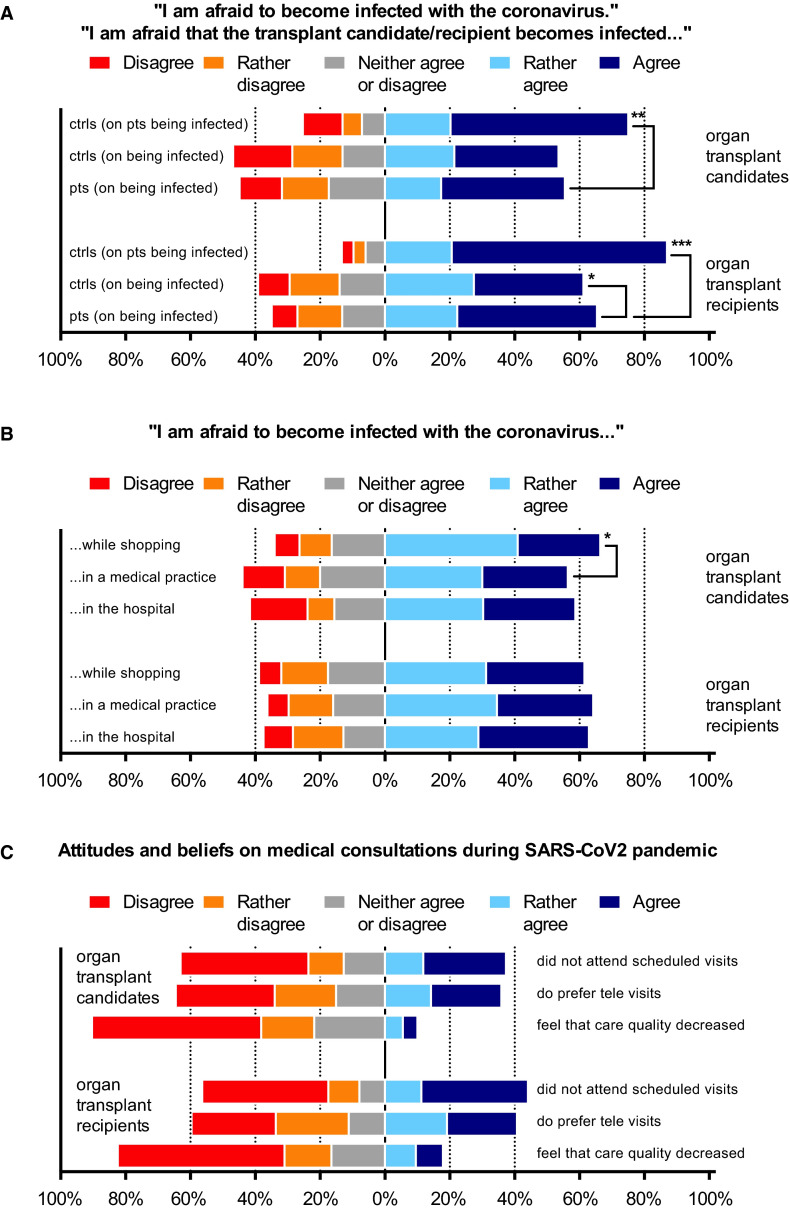
Responding to the item “I am afraid to become infected with the Coronavirus,” SOT recipients reported a significantly greater fear of being infected with SARS-CoV-2 than their household controls ( Figure 1A and Table S1). The fear that the transplant recipient becomes infected with SARS-CoV-2 reported by the household controls (87% “agree” or “rather agree”) was significantly higher than the fear reported by the transplant recipient (65%, P < .001). This pattern was also observed in transplant candidates (56%) and their controls (75%, P = .008, Figure 1A).
FIGURE 1.
Fears, attitudes, and beliefs toward severe acute respiratory syndrome coronary virus 2 infection in organ transplant recipients, candidates on the waiting list, and matched household controls. Panel A shows the responses to the item “I am afraid to become infected with the coronavirus”; panel B the responses to the items “I am afraid to become infected with the coronavirus while shopping,” "...in a medical practice," and "...in the hospital"; and panel C the responses to the items "I did not attend scheduled visits due to the Coronavirus Pandemic," "I would prefer a video or phone consultation to personal consultation at the transplant outpatient clinic," and "I feel the quality of my medical care has decreased because of the Coronavirus Pandemic." Distribution on responses to the respective questionnaire items is shown for patients (pts.) and controls (ctrls.) as indicated. *P < .05, **P < .01, ***P < .001 showing significant differences in the Likert scale distribution as assessed by Wilcoxon’s signed-rank test. For the complete questionnaire items see Table S1
When asked about whether being afraid of becoming infected when visiting different locations, there were no differences between shopping (62% “agree” or “rather agree”), medical offices (64%), and the hospital (63%) in organ transplant recipients. In candidates on the waiting list, the reported fear of a possible infection was highest while shopping (66%) as compared to a medical office (56%) or the hospital (59%). In organ transplant candidates, the difference in Likert scales to the items “I am afraid to become infected in a medical office” and “I am afraid to become infected while shopping” was statistically significant (P = .04) (Figure 1B and Table S1).
Only a minority of patients after organ transplantation (18%) and on the waiting list (10%) agreed with the item “I experience worse medical care than before the COVID-19 pandemic” (Figure 1C).
3.4. Indicators and consequences of fear of COVID-19
A total of 232 (64%) SOT recipients (64%) and 61 (54%) SOT candidates “agreed” or “rather agreed” with the item “I am afraid to become infected with the Coronavirus.” Organ transplant recipients reporting fear were more often female (43% vs 30%, P = .02), more often received steroid therapy (23% vs 12%, P = .01), and more often reported the local newspaper as a primary source of information about the SARS-CoV-2 pandemic (35% vs 24%, P = .03) than transplant recipients not reporting fear (Table S2). Female sex (adjusted odds ratio [OR] 1.73, 95% confidence interval [CI] 1.07-2.81, P = .03), steroid use (OR 2.05, 95% CI 1.07-3.92, P = .03), and using the local newspaper as a primary source of information (OR 1.79, 95% CI 1.09-2.97, P = .03) were independent indicators of fear of being infected with SARS-CoV-2 in multivariable analysis ( Table 2). Age, educational status, underlying liver disease, smoking, and influenza vaccination status did not significantly differ between patients reporting vs not reporting fear of becoming infected with SARS-CoV-2 (Table S2).
TABLE 2.
Indicators of reporteda fear of becoming infected with SARS-CoV-2 in organ transplant recipients
| Univariate logistic regression | Multivariable logistic regressionb | |||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% Confidence interval | P value | Odds ratio | 95% Confidence interval | P value | |
| Female sex | 1.74 | 1.09-2.77 | .02 | 1.73 | 1.07-2.81 | .03 |
| Steroid use | 2.28 | 1.21-4.31 | .01 | 2.05 | 1.07-3.92 | .03 |
| Triple immunosuppression | 2.23 | 1.03-4.80 | .04 | Removed from model | ||
| COVID-19 information from local newspaper | 1.74 | 1.06-2.86 | .03 | 1.79 | 1.07-2.97 | .03 |
Abbreviations: COVID-19, coronavirus 19; SARS-CoV-2, severe acute respiratory syndrome coronavirus-2.
Including the responses “Rather Agree” or “Agree” to the question “I am afraid to become infected with the coronavirus” on a 5-level Likert scale.
Backward elimination.
As a consequence, patients reporting fear of becoming infected with COVID-19 more often used personal protective equipment (85% vs 66%, P < .001) and washed their hands more frequently (95% vs 88%, P = .02). Transplant recipients reporting fear were more likely to skip or postpone scheduled medical visits (52% vs 29%, P < .001) and prefer video or phone consultations (51% vs 21%, P < .001) (Table S2).
3.5. Association of time since transplantation and severity of immunosuppression on attitudes and behavior
In SOT recipients, older age was correlated with higher agreement with the items “I feel sufficiently informed about the Coronavirus Pandemic” and “I feel sufficiently informed about the influence of the Coronavirus on chronic diseases and transplanted patients,” and higher disagreement with the item “I am afraid that my medication could worsen an infection with the Coronavirus” ( Table 3). In contrast, shorter duration since transplantation was associated with higher agreement with the items “I am afraid that my medication could worsen an infection with the Coronavirus,” “I am afraid to become infected while shopping,” and “I leave the house less frequently than my partner/household members.”
TABLE 3.
Correlation of age, transplant duration, and intensity of immunosuppression with attitudes and beliefs towards COVID-19 in organ transplant recipients
| Beliefs and attitudes toward coronavirus 19 | Age of the transplant recipient | Time since transplant | Number of immunosuppressants |
|---|---|---|---|
| “I feel sufficiently informed about the Coronavirus Pandemic” | 0.138* | 0.030 | −0.062 |
| “I feel sufficiently informed about the influence of the Coronavirus on chronic diseases and transplanted patients” | 0.164** | 0.088 | −0.133* |
| “I am afraid to become infected with the Coronavirus” | −0.028 | −0.028 | 0.102 |
| “I am afraid that my medication could worsen an infection with the Coronavirus” | −0.213** | −0.150** | 0.203** |
| “I am afraid to become infected in the hospital” | −0.038 | 0.033 | 0.083 |
| “I am afraid to become infected in a medical practice” | −0.082 | −0.040 | 0.106* |
| “I am afraid to become infected while shopping” | −0.085 | −0.113* | 0.060 |
| “I would prefer a video or phone consultation to personal consultation at the transplant outpatient clinic” | −0.077 | −0.014 | 0.058 |
| “I leave the house less frequently than before the Coronavirus pandemic” | −0.036 | −0.071 | 0.055 |
| “I leave the house less frequently than my partner/household members” | 0.077 | −0.153** | 0.127* |
| “I did not attend scheduled visits due to the Coronavirus Pandemic” | −0.018 | 0.029 | 0.119* |
| “I feel the quality of my medical care has decreased because of the Coronavirus Pandemic” | −0.074 | −0.017 | 0.049 |
| “I am afraid that my diseased partner/household member could receive worse medical care than before” (Household contacts’ response) | −0.233** | −0.141* | 0.101 |
Note. Coefficients from Spearman’s nonparametric correlation with 5-level Likert scales shown.
Abbreviations: COVID-19, coronavirus 19.
*P < .05; **P < .01.
A higher level of immunosuppression, as assessed by the number of immunosuppressant classes used, also correlated with higher agreement with the items “I am afraid that my medication could worsen an infection with the Coronavirus,” “I am afraid to become infected in a medical office,” “I leave the house less frequently than my partner/household members,” and “I did not attend scheduled visits due to the Coronavirus Pandemic” and higher disagreement with the item “I feel sufficiently informed about the influence of the Coronavirus on chronic diseases and transplanted patients” (Table 3).
4. DISCUSSION
While there is an ongoing debate about to what extent patients with liver disease and after liver transplantation are at increased risk of SARS-CoV-2 infection and COVID-19 complications, it is already foreseeable that the SARS-CoV-2 pandemic will have a long-lasting impact on the medical care of patients with liver disease.14 , 16 One of the central emotional responses during a pandemic is fear and even in noninfected households, the pandemic may act as a major stressor facilitating chronic anxiety.17
Here we demonstrate that fears associated with the SARS-CoV-2 pandemic are frequently expressed by liver transplantation recipients and candidates as well as by their household members. Transplant recipients who reported fear of infection adhered to washing hands and wearing face masks and/or gloves when leaving the house. Being afraid of becoming infected with SARS-CoV-2 after transplantation was more frequently reported in female patients and in patients with more intense immunosuppression, that is, steroids or triple immunosuppression. Notably, the fear of infection was not associated with established risk factors for mortality in COVID-19, such as cardiovascular and pulmonary comorbidity and older age.7
Despite reports about higher mortality of COVID-19 in patients after SOT,11 , 12 , 18 , 19 there is no conclusive evidence for a causative role of immunosuppression. As a result, current guidelines recommend continuation of immunosuppressive therapy in transplant patients.14 , 20 Accordingly, only 1 patient in this survey reported a reduction of tacrolimus without consulting a physician. However, the fear that their medication could worsen an infection with SARS-CoV-2 was expressed by one third of patients after transplantation. This fear was highest in younger patients, patients with a shorter time since transplantation, and a more intense immunosuppression in our survey. Notably, such patients were also more likely to report that they do not feel sufficiently informed about the influence of the virus on chronic diseases, emphasizing the need for better communication strategies in these vulnerable patients. Only 15% of patients stated that the transplant center was a relevant source of information about COVID-19. The major given reason was not to impinge on the staff’s time. Therefore, contacting patients directly by sending out information and encouraging them to approach the transplant center with further questions seems advisable.
The fear of becoming infected with SARS-CoV-2 was higher in patients with more intense immunosuppression. A correlation of severity of immunosuppression and fear of infection has been observed in patients with inflammatory bowel disease (P.C. Grunert et al, 2020). Weighing benefits against possible harms resulted in a high adherence to the therapy, because only 1 patient reported a reduction of tacrolimus without consulting a physician.
Another important finding of this study is that patients expressed comparable levels of fear contracting COVID-19 in medical facilities, similar to that of shopping areas. Implementing and communicating measures to ensure that hospitals and medical offices are a low-risk environment for contracting COVID-19 may improve patients’ sense of security. In addition, regular screening of staff and patients may help to detect or prevent outbreaks and identify infected patients early.
In some regions of heavily affected countries, intensive care capacities are overloaded with ventilated patients and therefore capacities for organ donation and transplantation are reduced.21 , 22 In addition, routine consultations are cancelled or postponed, resulting in less frequent contact of patients with the healthcare system. In our survey, 44% of the patients reported postponed clinical visits. This may be underestimating the true frequency given the short period between the begin of the pandemic and conducting the survey. It is likely that the proportion of postponed visits will increase over time. One solution may be healthcare delivery by telehealth in transplant recipients and candidates.23 In our study, transplanted patients who expressed higher fear of becoming infected with SARS-CoV-2 more often reported that they also postponed scheduled visits at the outpatient clinic and expressed their preference for video or telephone visits. While fears and concerns associated with the SARS-CoV-2 pandemic are frequently expressed by SOT recipients and candidates, measures to prevent infection were frequently followed in the vast majority of patients.
Despite the large sample size and the bicenter nature of the survey, there are some limitations. We used 5-point Likert scales as a standard ordinal psychometric measurement of attitudes, beliefs, and opinions. Despite the high response rate, nonresponse bias, acquiescence, and social desirability may result in overestimation of the adherence to preventive measures and underestimation of the reported reduction in immunosuppression. We tried to minimize possible bias (order effect, acquiescence bias, central tendency, and pattern answering) by comparing the results to matched control groups. However, caution is advised when transferring these results to SOT recipients other than liver and pancreas/kidney or patients receiving more intensified immunosuppression. Differences in national health services as well as cultural differences between different populations need to be taken into account when interpreting and generalizing these results.
The current COVID-19 pandemic is a highly dynamic process, and recommendations and regulations change rapidly. As fear is usually highest at the beginning of a new threat, it is likely that the responses underlie dynamic changes as well. The incidence of COVID-19 in Germany is still low; therefore, only a minority of the participants had contact with confirmed cases of COVID-19. Based on the fears and information deficits reported by patients in this survey, transplant centers are advised to intensify communication strategies and consider implementing telehealth in order to provide optimum medical care in liver transplant recipients and patients on the waiting list.
ACKNOWLEDGMENTS
PAR and AS conceived of the study. PAR, FR, SA, and TB recruited patients and collected the data. TB performed statistical analysis. PAR and TB wrote the manuscript. CT, US, and SA gave important intellectual input in data interpretation. All authors read and approved the final version of the manuscript. Funding was not obtained for this study.
DISCLOSURE
The authors of this manuscript have no conflicts of interest to disclose as described by the American Journal of Transplantation.
DATA AVAILABILITY STATEMENT
Data are available from the corresponding authors upon request.
Footnotes
Philipp A. Reuken and Falk Rauchfuss are equally contributing first authors. Tony Bruns and Andreas Stallmach are equally contributing senior authors.
SUPPORTING INFORMATION
Additional supporting information may be found online in the Supporting Information section.
Supplementary Material
REFERENCES
- 1.Zhu NA, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19–-11-march-2020. Accessed April 25, 2020
- 3.COVID-19 Map. Johns Hopkins Coronavirus Resource Center. https://coronavirus.jhu.edu/map.html. Accessed May 3, 2020
- 4.Weible CM, Nohrstedt D, Cairney P, et al. COVID-19 and the policy sciences: initial reactions and perspectives. Policy Sci. 2020;53(2):225. doi: 10.1007/s11077-020-09381-4. Published online April 18, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 7.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ji D, Qin E, Xu J, et al. Non-alcoholic fatty liver diseases in patients with COVID-19: a retrospective study. J Hepatol [published online ahead of print 2020]. 10.1016/j.jhep.2020.03.044 [DOI] [PMC free article] [PubMed]
- 9.Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395(10229):1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang C, Shi L, Wang F-S. Liver injury in COVID-19: management and challenges. Lancet Gastroenterol Hepatol. 2020;5(5):428–430. doi: 10.1016/S2468-1253(20)30057-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bhoori S, Rossi RE, Citterio D, Mazzaferro V. COVID-19 in long-term liver transplant patients: preliminary experience from an Italian transplant centre in Lombardy. Lancet Gastroenterol Hepatol. Published online April 9, 2020. 2020;5(6):532–533. doi: 10.1016/S2468-1253(20)30116-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Webb GJ, Moon AM, Barnes E, Barritt AS, Marjot T. Determining risk factors for mortality in liver transplant patients with COVID-19. Lancet Gastroenterol Hepatol. Published online April 24, 2020. 2020. 10.1016/S2468-1253(20)30125-4. [DOI] [PMC free article] [PubMed]
- 13.D’Antiga L. Coronaviruses and immunosuppressed patients: the facts during the third epidemic. Liver Transpl. [published online ahead of print March 20, 2020]. 26(6):832-834. [DOI] [PubMed]
- 14.Boettler T, Newsome PN, Mondelli MU, et al. Care of patients with liver disease during the COVID-19 pandemic: EASL-ESCMID position paper. JHEP Rep. 2020;2(3):100113. doi: 10.1016/j.jhepr.2020.100113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lleo A, Invernizzi P, Lohse AW, Aghemo A, Carbone M. Highlights for management of patients with autoimmune liver disease during COVID-19 pandemia. J Hepatol. [published online ahead of print April 10, 2020]. 10.1016/j.jhep.2020.04.002. [DOI] [PMC free article] [PubMed]
- 16.Tapper EB, Asrani SK. COVID-19 pandemic will have a long-lasting impact on the quality of cirrhosis care. J Hepatol. [published online ahead of print April 13, 2020]. 10.1016/j.jhep.2020.04.005 [DOI] [PMC free article] [PubMed]
- 17.Bavel JJV, Baicker K, Boggio PS, et al. Using social and behavioural science to support COVID-19 pandemic response. Nat Hum Behav. [published online ahead of print April 30, 2020]. 10.1038/s41562-020-0884-z [DOI] [PubMed]
- 18.Fernández-Ruiz M, Andrés A, Loinaz C, et al. COVID-19 in solid organ transplant recipients: a single-center case series from Spain. Am J Transplant. [published online ahead of print April 16, 2020]. 10.1111/ajt.15929. [DOI] [PMC free article] [PubMed]
- 19.Huang J, Lin H, Wu Y, et al. COVID-19 in posttransplant patients-report of 2 cases. Am J Transplant. [published online ahead of print April 3, 2020]. 10.1111/ajt.15896 [DOI] [PMC free article] [PubMed]
- 20.Fix OK, Hameed B, Fontana RJ, et al. Clinical best practice advice for hepatology and liver transplant providers during the COVID-19 pandemic: AASLD Expert Panel Consensus Statement. Hepatology. [published online ahead of print April 16, 2020]. 10.1002/hep.31281 [DOI] [PMC free article] [PubMed]
- 21.Maggi U, De Carlis L, Yiu D, et al. The impact of the COVID-19 outbreak on Liver Transplantation programmes in Northern Italy. Am J Transplant. [published online ahead of print April 24, 2020]. 10.1111/ajt.15948. [DOI] [PMC free article] [PubMed]
- 22.Boyarsky BJ, Chiang TP-Y, Werbel WA, et al. Early Impact of COVID-19 on transplant center practices and policies in the United States. Am J Transplant. [published online ahead of print April 13, 2020]. 10.1111/ajt.15915 [DOI] [PMC free article] [PubMed]
- 23.John BV, Love E, Dahman B, et al. Use of telehealth expedites evaluation and listing of patients referred for liver transplantation. Clin Gastroenterol Hepatol. [published online ahead of print December 27, 2019]. 10.1016/j.cgh.2019.12.021 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Data Availability Statement
Data are available from the corresponding authors upon request.