To the editor
Since the first report of cutaneous manifestations of the coronavirus disease 2019 (COVID‐19) by Recalcati et al, 1 there has been described five clinical patterns including pseudo‐chilblain lesions, vesicular eruptions, urticarial lesions, livedo and necrosis and maculopapular eruptions. 2 Several clinical reports have been published recently describing these clinical patterns although there is still a lack of information regarding histopathology of maculopapular eruptions.
We designed a retrospective study of patients attended in our department over the course of three weeks. We collected clinical data and pictures, and performed a biopsy when possible. Inclusion criteria were the presence of maculopapular eruptions as the reason for consultation in patients with previously confirmed infection for severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) by nasopharyngeal protein chain reaction (PCR). Exclusion criteria included patients that had taken any new medication in the previous two weeks as well as those who presented other type of lesions.
From a total of 18 initial patients, seven were included in the study. Patients´ information has been summarized in Table 1. Mean age was 66, 57 years (range 57–82 years). All the patients have had pneumonia before the onset of the cutaneous symptoms and consulted after they had been discharged from the hospital. The lesions appeared after a mean time of latency of 27,85 days (range 20–36 days). The clinical presentation and distribution of the lesions were similar in all the cases, being the trunk the most affected area Fig. 1a,b. Mean duration time of the aforementioned lesions after treatment commenced was 10,42 days (range 7–18 days) A second PCR was not performed at the time of the onset cutaneous manifestations and neither serological assays.
Table 1.
Clinical and histological characteristics of patients with maculopapular eruptions
| Case number | Sex | Age (years) | Location | Number of days since onset of | Duration of skin symptoms (days) | Treatment | Histology | |
|---|---|---|---|---|---|---|---|---|
| Symptoms | PCR | |||||||
| 1 | M | 67 | Trunk, proximal upper limbs | 20 | 12 | 18 | None | Mild Superficial perivascular lymphocytic infiltrate |
| 2 | F | 57 | Trunk | 28 | 26 | 9 | Systemic CE | Mild Superficial perivascular lymphocytic infiltrate |
| 3 | F | 82 | Trunk, proximal upper limbs | 32 | 32 | 7 | Systemic CE | – |
| 4 | M | 71 | Trunk, proximal upper limbs | 38 | 31 | 9 | Systemic CE | – |
| 5 | F | 64 | Trunk, proximal upper limbs | 21 | 24 | 9 | Systemic CE | – |
| 6 | F | 62 | Trunk, proximal upper and lower limbs | 20 | 27 | 14 | Systemic CE | Mild superficial perivascular lymphocytic infiltrate, spongiosis |
| 7 | F | 63 | Trunk, proximal upper limbs | 36 | 36 | 7 | Systemic CE | Mild superficial perivascular lymphocytic infiltrate and spongiosis |
CE, Corticoesteroids; F, Female; M, Male.
Figure 1.
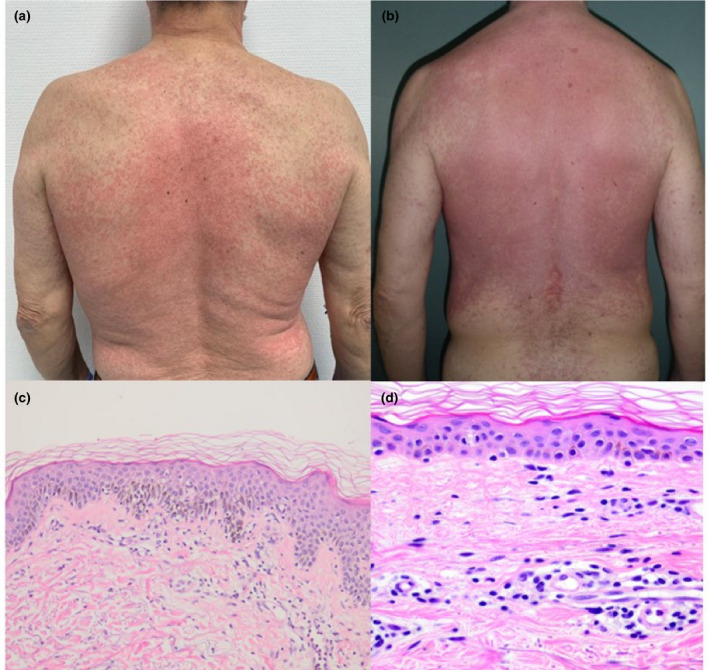
a) Patient 4. Confluent maculopapular exanthem affecting predominantly the trunk and proximal extremities. b) Patient 1. More extensive involvement of the trunk, with areas of unaffected skin. c) HE stain ×20. Mild superficial perivascular lympohcytic infiltrate, spongiosis and interface dermatitis. d) HE ×40. Mild superficial perivascular lymphocytic infiltrate.
Biopsy was performed in four of the cases (57.14%). In all of them a mild superficial perivascular lymphocytic infiltrate was observed Fig. 1c,d.
Jimenez‐Cauhe 3 et al. present a case of maculopapular eruption in a patient infected by SARS‐CoV‐2 and affirms the difficulty of assessing the origin of these reactions and subsequently unable to conclude if they are drug related or induced by the virus itself. Our findings suggest the latter since none of our patients had taken any new medication in the previous fifteen days and all of them showed similar findings in the biopsy.
Another interesting fact is the late time of onset in our patients. In a Spanish study, out of 375 patients with suspected or confirmed COVID19, 176 patients presented maculopapular eruptions. 108 of them appeared at the same time as the respiratory symptoms while only 60 appeared afterwards like in our series. 2 Due to the fast onset of some of the cutaneous manifestations and considering several patients were taking different medications at the time, we suspect some of them to be drug induced reactions. Another possibility is a different response to the viral infection in the cases where the lesions appear with the other symptoms or as a late‐onset cutaneous involvement.
Regarding histopathology, Herrero‐Moyano et al. observed dense neutrophilic infiltrates in 8 patients with late maculopapular eruptions. 4 Seven of them had taken new drugs the previous week, as had 5 of our cases with similar findings, which were excluded from the study. We thought that this might condition a different immune response to viral infection that would justify the heterogeneity of the histological findings.
We conclude these reactions to be late manifestations of COVID19. Furthermore, it would be interesting to perform a SARS‐CoV‐2 PCR and serological test during the onset of these lesions to conclude if these are directly induced by the virus or are a late immune response manifestation.
Acknowledgement
The patients in this manuscript have given written informed consent to the publication of their case details.
Prior presentation: This paper has not been published previously or submitted for publication elsewhere and will not be submitted for publication elsewhere before a decision is reached concerning publication in the JEADV
References
- 1. Recalcati S. Cutaneous manifestations in COVID‐19: a first perspective. J Eur Acad Dermatol Venereol 2020. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 2. Galván‐Casas C, Catalá A, Carretero‐Hernández G et al. Classification of the cutaneous manifestations of COVID‐19: A rapid prospective nationwide consensus study in Spain with 375 cases. Br J Dermatol. 2020. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Jiménez‐Cauhe J, Ortega‐Quijano D, Prieto‐Barrios M, Moreno‐Arrones OM, Fernandez‐Nieto D. Reply to “COVID can present with rash and mistaken for dengue”: Petechial rash in a patient with COVID‐19 infection. J Am Acad Dermatol 2020. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Herrero‐Moyano M, Capusan TM, Andreu‐Barasoain M et al. A clinicopatological study of 8 patients with COVID‐19 pneumonia and a late‐onset exanthema. J Eur Acad Dermatol Venereol 2020. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]


