1. INTRODUCTION
The ongoing coronavirus disease 2019 (COVID‐19) pandemic is having a profound impact on people with dementia. A relevant proportion of COVID‐19–related deaths have probably occurred in patients with dementia. 1 Dramatically high fatality rates have been observed worldwide among residents of long‐term facilities, 2 many of them likely experiencing dementia. In addition, the restrictive measures implemented to tackle the spread of the outbreak still adversely affect patients and their caregivers because they have been asked to isolate from their regular support systems and change their routine. Social distancing and self‐isolation have probably limited the use of those strategies and general rules (e.g., distraction, stimulation, and social interaction) that are routinely adopted to manage some of the dementia symptoms (e.g., neuropsychiatric symptoms) and attenuate the caregiver's burden. 3 The prolonged self‐isolation may have contributed to generate feelings of loneliness, behavioral modifications and disruptions, and acute events (e.g., agitation and delirium) requiring therapeutic changes or even hospitalization. 4 Moreover, the emerging and evolving health needs and priorities of patients and caregivers have not been adequately met. In fact, many scheduled appointments for routine clinical checkups at dedicated services have been canceled and postponed because of the COVID‐19 outbreak.
Thus, we sought to explore whether the clinical conditions of patients with dementia and cognitive disturbances have changed during the pandemic to gain insights on how to rearrange the provision of care in the postemergency phase.
2. METHODS
A telephone survey of a sample of patients attending the Center for Cognitive Disturbances and Dementia, Department of Human Neuroscience, Sapienza University of Rome (Italy), was performed. All consecutive patients performing their last clinical assessment in the 2 months preceding the local introduction of restrictive measures for COVID‐19 (i.e., March 10, 2020) were considered for the present analysis. The survey was conducted by the medical staff from April 9, 2020, to April 15, 2020, as part of standard clinical routine and referred to the first month of lockdown. A standardized set of questions was asked to subjects with mild cognitive deficits or to the caregivers of patients with dementia to assess perceived changes in their clinical conditions that occurred in the previous 30 days. Patients and caregivers (or legal guardians when necessary) had already provided written informed consent for allowing the utilization of the collected data for research purposes (as required by the “Policlinico Umberto I" University Hospital of Rome).
3. RESULTS
A total of 139 subjects (women = 60.4%; median age = 79.0 years) completed the survey (response rate = 85.8%). Among them, 96 (69.1%) were diagnosed with dementia, whereas 43 (30.9%) had milder cognitive disturbances (Table 1). None of the participants had received a laboratory‐confirmed diagnosis of severe acute respiratory syndrome coronavirus 2 infection, and only five of them reported having experienced flu‐like, self‐limiting symptoms. Most of patients (i.e., 66.2%) were reported to have fully adhered to the recommended restrictive measures (e.g., social distancing) and safeguard procedures (e.g., washing hands and wearing masks).
Table 1.
Characteristics of Participants and Reported Clinical Changes
| Variable | Dementia (n = 96) | MCI or SCD (n = 43)a |
|---|---|---|
| Demographics | ||
| Age, y | 80.5 (76.0–85.0) | 73.0 (65.5–77.5) |
| Female sex | 53 (55.2) | 31 (72.1) |
| Survey respondent | ||
| Patient | 2 (2.1) | 40 (93.0) |
| Caregiver | 94 (97.9) | 3 (7.0) |
| Clinical changes | ||
| Cognitive improvement | 1 (1.0) | 2 (4.7) |
| Cognitive worsening | 34 (35.4) | 10 (23.3) |
| Functional improvement | 0 (0.0) | 0 (0.0) |
| Functional decline | 18 (18.8) | 1 (2.3) |
| Improvement of NPSs | 2 (2.1) | 3 (7.0) |
| Worsening of NPSs | 55 (57.3) | 21 (48.8) |
| Changes in pharmacological therapies | ||
| Any therapeutic adjustment | 9 (9.4) | 1 (2.3) |
| New pharmacological treatment | 2 (22.2) | 1 (100) |
| Dosage increase of ongoing therapies | 5 (55.6) | 0 (0.0) |
| Dosage reduction of ongoing therapies | 2 (22.2) | 0 (0.0) |
| Caregiver burden | ||
| Increased caregiver stress | 47 (48.5) | 1 (33.3) |
Note: Data are shown as median (interquartile range) or number (percentage).
Abbreviations: MCI, mild cognitive impairment; NPS, neuropsychiatric symptom; SCD, subjective cognitive decline.
MCI: n = 37; SCD: n = 6.
Overall, a worsening of cognitive symptoms, particularly of memory and orientation abilities, was reported in nearly one‐third of the sample (i.e., 31.7%) (Table 1 and Figure 1). A functional decline was noticed in 19 patients and was mainly described in terms of reduced levels of independence in personal care and housekeeping. More than half of patients (i.e., 54.7%) experienced the worsening or the onset of behavioral disturbances, with agitation/aggression, apathy, and depression representing the most commonly observed manifestations. Such clinical changes were most commonly observed in patients with overt dementia compared with respondents with milder cognitive deficits. Of note, an improvement of cognitive and neuropsychiatric symptoms was described in some cases.
Figure 1.
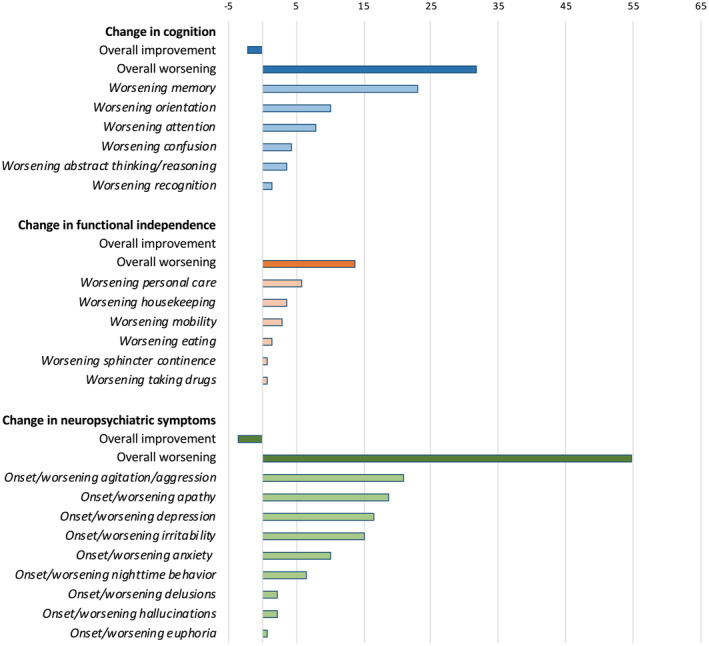
Clinical changes reported in the study population. Data are shown as percentages.
In 7.2% of patients, the observed clinical changes required adjustments of the ongoing pharmacological therapy or the introduction of new treatments (mostly antipsychotics). Half of caregivers (i.e., 49.5%) reported higher levels of stress and exhaustion compared with the previous month.
4. DISCUSSION
These findings, although obtained in a limited study population and based on the perceptions of patients and caregivers, suggest that the COVID‐19 outbreak is indirectly affecting the clinical conditions of people living with dementia and cognitive disturbances. Their multifaceted health needs, largely neglected in the emergency phase of the pandemic, might have silently changed and become even more challenging. Accordingly, caregivers might have been exposed to critical levels of stress because they had to manage, with little external support, complex disturbances.
Special support is urgently needed for patients with dementia and their caregivers during critical events. Dedicated services and facilities, often suspended or reduced in their activities in a period of crisis, must be restored as soon as possible and get organized to deal with the high demand. In the meanwhile, alternative forms of support should be enforced and delivered, taking inspiration from previous promising experiences. 5 Regular contacts, performed by physicians and professional nurses (also with the support of novel technologies), can allow us to monitor the conditions of patients and timely identify urgent situations to prioritize. Self‐help guidance and resources should be disseminated to families and caregivers to improve the at‐home management of patients and attenuate stress. 3
ACKNOWLEDGMENTS
Conflict of Interest
Authors have no competing interest to disclose for the present study.
Marco Canevelli is supported by a research grant of the Italian Ministry of Health (GR‐2016‐02364975) for the project “Dementia in Immigrants and Ethnic Minorities Living in Italy: Clinical‐Epidemiological Aspects and Public Health Perspectives” (ImmiDem). Matteo Cesari has received honoraria for presentations at scientific meetings and/or research funding from Nestlé and Pfizer. He is involved in the coordination of an Innovative Medicines Initiative–funded project (including partners from the European Federation Pharmaceutical Industries and Associates [Sanofi, Novartis, Servier, GSK, and Lilly]).
Author Contributions
Marco Canevelli: study conception and design and writing of the manuscript.
Martina Valletta: data collection and analysis.
Marco Toccaceli Blasi: data collection.
Giulia Remoli: data collection.
Giulia Sarti: data collection.
Filippo Nuti: data collection.
Francesco Sciancalepore: data collection.
Enzo Ruberti: interpretation of data.
Matteo Cesari: interpretation of data and drafting of the manuscript.
Giuseppe Bruno: study conception, interpretation of data, and drafting of the manuscript.
Sponsor's Role
None.
This article was published online on 9 June 2020. An error was subsequently identified in the author degrees. This notice is included in the online and print versions to indicate that both have been corrected on 19 June 2020.
REFERENCES
- 1. SARS‐CoV‐2 Surveillance Group . Istituto Superiore di Sanità. Characteristics of SARS‐CoV‐2 patients dying in Italy. April 29, 2020. 2020. https://www.epicentro.iss.it/en/coronavirus/bollettino/Report-COVID-2019_29_april_2020.pdf. Accessed May 6, 2020.
- 2. McMichael TM, Currie DW, Clark S, et al. Epidemiology of COVID‐19 in a long‐term care facility in King County, Washington. N Engl J Med. 2020;382(21):2005–2011. 10.1056/NEJMoa2005412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Alzheimer Europe . COVID‐19 ‐ living with dementia. https://www.alzheimer-europe.org/Living-with-dementia/COVID-19. Accessed May 7, 2020.
- 4. Wang H, Li T, Barbarino P, et al. Dementia care during COVID‐19. Lancet. 2020;395:1190‐11911. 10.1016/S0140-6736(20)30755-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lucero RJ, Fehlberg EA, Patel AGM, et al. The effects of information and communication technologies on informal caregivers of persons living with dementia: a systematic review. Alzheimers Dement (N Y). 2019;5:1‐12. 10.1016/j.trci.2018.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]


